Abstract
Hamartoma of soft tissue in the extremity is uncommon. We report a 36-year-old female patient with neurofibromatosis type 1 (NF-1). She had had a gradually increased mass in her right forearm and wrist for ten years. The mass increased suddenly after the trauma. As a result, she felt pain and progressive numbness of forearm and hand. Her radial and median nerves were compressed by the mass. We resected the tumor and released the compression of nerves. After the surgery, the patient gained neural functional recovery. Two years after surgery, she had no tumor recurrence. We discuss its clinical diagnosis, radiological features, MRI findings, pathophysiology, and treatment. Background: Hamartoma consists of multiple tissue elements. It can develop a bony disorder, rupture the blood vessels and create altered hemodynamics. NF-1 is caused by the mutation of a gene on chromosome 17 that is responsible for the control of cell division. It is also known as von Recklinghausen’s disease. No case of the radial and median nerves that are compressed by the forearm hamartoma in NF-1 has been described in the literature before.
Keywords: Hamartoma, nerve compression, neurofibromatosis type 1
Case presentation
A 36-year-old female patient presented with gradually increased mass in her right forearm and wrist for ten years. She felt no pain and numbness of her hand, and reported no history of trauma. She was diagnosed with “hemangioma” via ultrasound in other hospital. At that time, she was not suggested to do the surgery. The day before she was in hospital, she had her forearm hit when moving the weights. As a result, the mass of the forearm increased rapidly and she felt pain and progressive numbness of forearm and hand. The mass was located on the radial palmar of the right wrist, and a large café-au-lait spot covered the lesion. Due to the exhibited multiple café-au-lait spots throughout the patient’s body and her family history, we diagnosed her as NF type 1 (Figure 1). The mass was soft and its margin was not well-defined. Her wrist deformed ulnar deviation. Neurologic examination showed impaired function of sensory deficit. Electromyography (EMG) showed that the conduction velocity of radial and median nerves decreased. Laboratory studies showed the counting of white blood cells and neutrophile granulocyte increased, the tumor biological markers were normal. Radiographs (Figure 2) showed a large soft-tissue mass in the patient’s forearm and wrist, and trapezium, scaphoi distal radius were destructed. Magnetic resonance imaging (MRI) (Figure 3) showed as follows. In T1-weighted images the mass showed isointense to muscle signal intensity; in T2-weighted images, the mass showed hyperintense to muscle signal intensity, it was about 9.2×3.9 cm in size. Due to the slow development of mass, we diagnosed this case as a benign tumor. While, biopsy procedure cannot be performed in order to avoid wound contamination. CT angiography showed that a large soft-tissue mass within the wads of blood vessels was not well defined. The main purpose of the operation was based on the excursion of tumor and releasing the compression of nerves. The excision of the mass in the forearm, resection of transverse carpal ligament and decompression of nerves were performed under the general anesthesia. During the operation, we found that the mass without well-defined margin was large in size, which was 9×6×1.5 cm. It developed abnormally with partial blood vessels, adhered severely with radial artery and radial nerve, and entered carpal tunnel to compress the median nerve (Figure 4). After the tumor removal, we designed local skin flaps, and primary skin closure was achieved. Frozen section and histologic findings revealed that it was hamartoma of soft tissue, consisting of nerve sheath cells, endothelial cells, mononuclear cells, chemokines, collagen and vessels. Immunohistochemistry shows: CD34 positive, S-100 protein positive, SMA negative. Micrograph showed proliferation of nerve fibers apparently, some of which grew among the cutaneous appendages. There were multiple irregular enlarged thick-walled vessels in the tissues, which accompanied the formation of hematoma. (hematoxylin-eosin stain, original magnification_400) (Figure 5).
Figure 1.
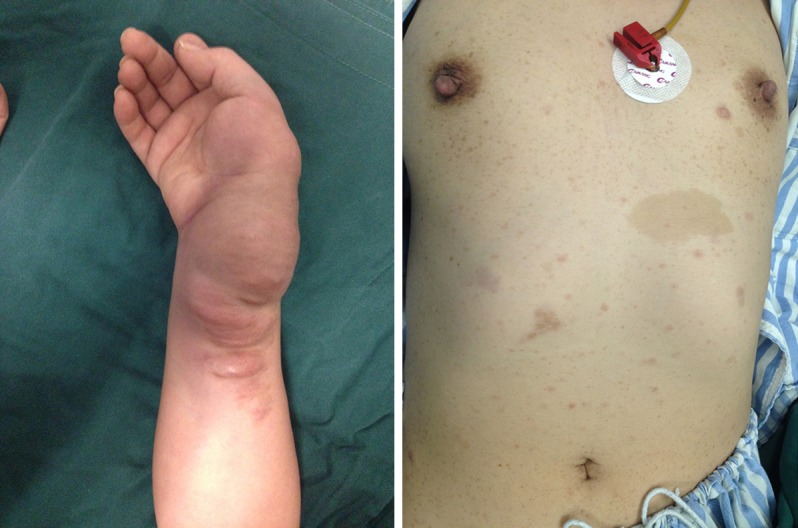
Pre-operation photograph, showing a large-sized mass in right forearm and wrist and multiple café-au-lait spots throughout the patient’s body.
Figure 2.

Radiographs of pre-operation showing a large soft-tissue mass in patient’s forearm and wrsit, and trapezium, scaphoi distal radius were destructed.
Figure 3.
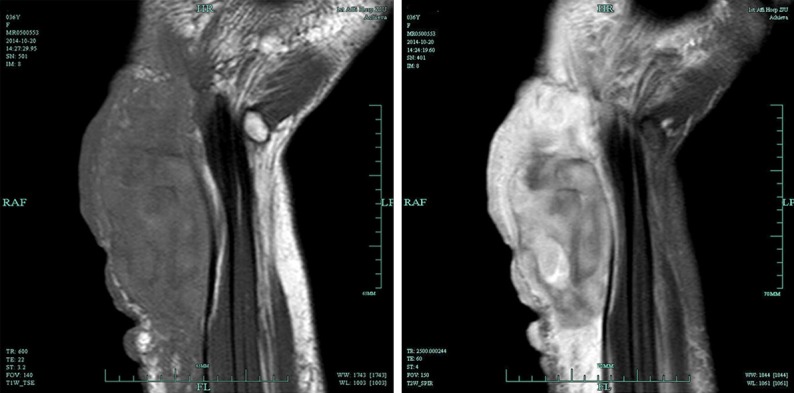
MRI of pre-operation showing in T1-weighted images the mass showed isointense to muscle signal intensity; in T2-weighted images, the mass showed hyperintense to muscle signal intensity.
Figure 4.

The photograph during the operation, showing the released median nerve and radialis nerve which were entrapped by the masses. The mass entered carpal tunnel.
Figure 5.
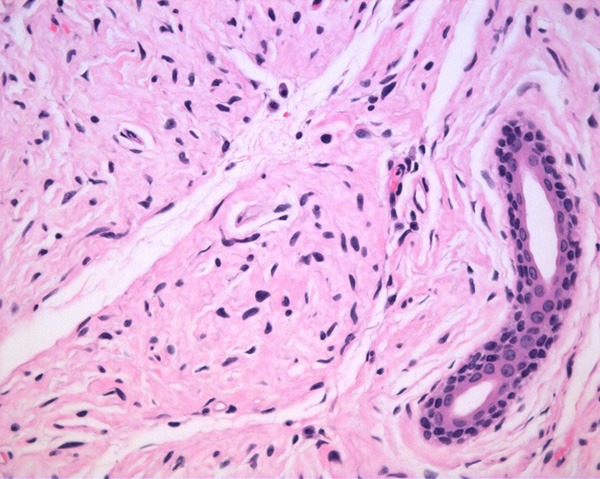
Pathological photograph, showing hamartoma of soft tissue, consisting of nerve sheath cells, endothelial cells, mononuclear cells, chemokines, collagen and vessels. CD34 positive, S-100 protein positive (hematoxylin-eosin stain, original magnification_400).
One week after the surgery, the patient was allowed to perform rehabilitation exercise. The patient had taken methylcobalamin tablets for half a year (0.5 mg every 8 h; Eisai Co, Ltd Japan). One month after the surgery, the sense of numbness decreased, and her wrist range of motion recovered to the level before her injury. In order to correct the patient’s deformity of ulnar deviation in the wrist, we chose functional rehabilitation with wrist brace. Three months after the surgery, electromyography showed the recovery of normal nerve conduction velocity. Two years after the surgery, MRI presented no tumor recurrence and she had no symptom of nerve compression syndromes.
Discussion
NF-1, which is also known as von Recklinghausen’s disease, with an estimated prevalence of approximately one case per 3000 in the general population [1,2]. It affects male and female subjects equally in all races [3]. NF-1 has an autosomal dominant pattern of inheritance that is linked to a defect on chromosome 17, with approximately 50% of cases arising as new somatic mutations [4]. The neurofibroma most commonly present as skin lesions as isolated soft papules or nodules arising in any cutaneous site. Hamartoma consists of multiple tissue elements, such as ectodermal and mesodermal components [5]. Its progression can lead to a bony disorder, rupture the blood vessels and create altered hemodynamics. Among the patients who are diagnosed with NF-1, it is difficult to tell the differences between hamartoma and neurofibroma so as that it is also difficult to make a correct diagnosis. Pathological diagnosis can help. Hamartoma can completely release the compression of nerves relative to neurofibroma. Neurofibroma is a localized discrete mass of benign nerve sheath tumor in the peripheral nervous system. Neurofibroma is mostly considered as a benign tumor condition; however malignant transformation has been reported in two percent of patients with NF1 [6-8]. The aim of the operation is mainly to avoid haemorrhage [9]. The patient, who had been misdiagnosed with hemangioma, accepted passive intervention, which resulted in the mass increased at the later stage and entered carpal tunnel to compress the median nerve. Hamartoma requires a surgical resection that is as extensive as possible to reduce the recurrence. It was not feasible to widely excise the lesion, as it has no distinct capsule and it could be separated from adjacent structures difficultly. It often involves the muscles and subcutaneous tissue simultaneously and typically surrounded the neurovascular structures. In our case, the patient’s emergency decompression of nerves symptom resulted from the rupture of tumor and hemorrhage, so the main purpose of the operation is based on releasing nerves and excising the tumor as much as possible. After releasing the compression of nerve entrapment, the patient can achieve rapidly and completely recovery. However, without finding the compression of nerve entrapment, delayed diagnosis and treatment may cause the bad outcomes.
Conclusion
Among the patients who are diagnosed with NF-1, it is difficult to diagnosis between hamartoma and neurofibroma. It needs pathological diagnosis. Early diagnosis and treatment are essential to maintain function and avoid neuropathy. It is also important to perform the individualized treatment plan for the special cases.
Acknowledgements
First and foremost, I would like to show my deepest gratitude to my colleagues Dr Qiang Chen, Dr Hui Shen, who have provided me with valuable assist in every stage of writing this paper. Meanwhile, I also appreciate Zhejiang Medicine and Hygiene Research Program for sponsoring our research (the grant number 2015KYA100). Last but not least, I’d like to thank all my friends, especially my lovely wife for her encouragement and support.
Disclosure of conflict of interest
None.
References
- 1.Katz BH, Quencer RM. Hamartomatous spinal cord lesion in neurofibromatosis. AJNR Am J Neuroradiol. 1989;10:S101. [PMC free article] [PubMed] [Google Scholar]
- 2.Ferner RE, Gutmann DH. International consensus statement on malignant peripheral nerve sheath tumors in neurofibromatosis. Cancer Res. 2002;62:1573–1577. [PubMed] [Google Scholar]
- 3.Coakley D, Atlas MD. Diffuse neurofibroma obstructing the external auditory meatus. J Laryngol Otol. 1997;111:145–147. doi: 10.1017/s0022215100136680. [DOI] [PubMed] [Google Scholar]
- 4.Egelhoff JC, Bates DJ, Ross JS, Rothner AD, Cohen BH. Spinal MR findings in neurofibromatosis types 1 and 2. AJNR Am J Neuroradiol. 1992;13:1071–1077. [PMC free article] [PubMed] [Google Scholar]
- 5.Kimura T, Miyazawa H, Aoyagi T, Ackerman AB. Folliculosebaceous cystic hamartoma. A distinctive malformation of the skin. Am J Dermatopathol. 1991;13:213–220. [PubMed] [Google Scholar]
- 6.Voutsinas S, Wynne-Davies R. The infrequency of malignant disease in diaphyseal aclasis and neurofibromatosis. J Med Genet. 1983;20:345–349. doi: 10.1136/jmg.20.5.345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Korf BR. Malignancy in neurofibromatosis type 1. Oncologist. 2000;5:477–485. doi: 10.1634/theoncologist.5-6-477. [DOI] [PubMed] [Google Scholar]
- 8.Varan A, Sen H, Aydin B, Yalcin B, Kutluk T, Akyuz C. Neurofibromatosis type 1 and malignancy in childhood. Clin Genet. 2015 doi: 10.1111/cge.12625. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 9.Baek SH, Kim JH, Kim JS, Han SB, Cho JS, Yoon YH, Kim L. Recurrent massive subcutaneous hemorrhage in neurofibromatosis type 1: a case report. J Korean Med Sci. 2007;22:728–730. doi: 10.3346/jkms.2007.22.4.728. [DOI] [PMC free article] [PubMed] [Google Scholar]


