Abstract
This study aims to investigate clinical effects of protruding after percutaneous vertebral plasty (PKP holds) for treatment of chronic painful osteoporotic vertebral compression fractures (CPOVCFs), and assess its safety and effectiveness. One hundred and eighteen CPOVCFs patients were included, and analyzed and followed up therapeutic effects of PKP holds. All of these patients were divided into NIVC (73 cases) and IVC (45 cases) group. Comparing operation time, bone cement perfusion, pain intensity modulus visual grading scoring, Oswestry disability index, fracture fanterior relative height, local convex Angle, and surgical complications between the two groups. There were no significant differences between two groups for operation time of PKP holds (P>0.05). Amount of bone cement injection in IVC groups was significantly higher compared to NIVC group (P<0.05). Pain intensity visual modulus ratings and Oswestry disability index were significantly improved in both groups after surgery and postoperative follow-up period compared to pre-operation (P<0.05). Fracture fanterior margin relative height and local convex angle were also significantly improved (P<0.05). Fracture fanterior margin relative height was also significantly improved for IVC compared to NIVC group (P<0.05). There were no differences for bone cement leakage rate and adjacent segment fracture between two groups (P>0.05). But there was a case of bone cement loose, which needs to be treated for further step. In conclusion, PKP holds is a kind of effective and safe method for the IVC and NIVC patients. Especially for the IVC patients, PKP holds can significantly improve the fracture fanterior margin relative height.
Keywords: Protruding after percutaneous vertebral plasty, osteoporosis, vertebral fracture, vertebral body fracture, treatment effect
Introduction
The incidence of Osteoporotic vertebral compression fractures (osteoporotic vertebral compression will fractures, OVCFs) increased year by year. Although this disease with a benign development process, about 30% of patients with bad outcomes with the conservative treatment. Always the patients suffer from many symptoms, including worse healing fractures, chronic low back pain, which affect the quality of life seriously. Due to the fracture end pseudarthrosis formation, vertebral body collapse, increase of the protruding after spinal deformity, which may damage the spinal cord [1,2].
Many studies showed that the protruding after percutaneous vertebral plasty (percutaneous kyphoplasty, PKP holds) is a very important method for the treatment of chronic painful osteoporotic vertebral compression fractures (chronic painful OVCEs, CPOVCFs) [1-3]. According to the imaging examination, CPOVCFs can be divided into a vertebral body fracture (intravertebral cleft, IVC) and no vertebral body fracture (none intravertebral cleft, NIVC) [8-10]. For the treatment of IVC or NIVC the operation details and clinical effect may be inconsistent for PKP holds. However, there are seldom studies targeting the effects of PKP holds on the treatment of different types of CPOVCFs.
We employed the PKP holds to treat the IVC and NIVC CPOVDFs patients, specified the therapeutic details, and assess the clinical effects and safe for this method.
Materials and methods
Subjects
This study included 118 single segmental CPOVCFs patients from October, 2008 to October 2013. The patients were divided into two groups according to the imaging examination, including NIVC group (73 cases) and IVC (45 cases).
This study was approved by the ethics committee of Shandong Provincial Qianfoshan Hospital. All of the patients have been gave their consents, and approved this study.
Clinical diagnosis
Patients complained with chronic low back pain, and change posture can aggravate the pain, the pain was relief when lying position. Physical examination illustrated the Local kyphosis of spine, tenderness and taps pain in vertebral spine, and no radiation pain.
Imaging diagnosis
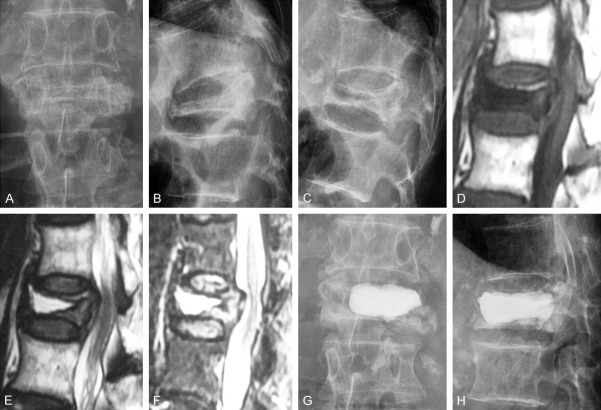
According to the imaging findings, the patients were divided into NIVC group and IVC group. The X-ray and CT results indicated that of the spine after partial protrusion deformity, vertebral osteoporosis, vertebral body fracture wedge, flat shape or double concave change; MRI in vertebral body fracture T1WI low signal, high T2WI signal, STIR high signal. IVC groups: X ray film and CT examination, besides NIVC group performance, vertebral body cracks; MRI in vertebral body fracture fluid accumulation) or vacuum) [11,12] (Figure 1).
Figure 1.
Imaging pictures of a 95 years old male OVCFs patient with IVC who had taken PKP treatment at L1. X-ray shows good vertebral height reduction and PMMA filling after PKP. A. Anteroposterior position preoperative. B. Lateral scan when body bends. C. Lateral scan when body extends. D. MRI view of T1WI. E. MRI view of T2WI. F. MRI view of STIR. G. Anteroposterior position postoperative. H. Lateral scan postoperative.
Include and exclude standards
Inclusion criteria: (1) Determination of dual-energy X-ray absorptiometry (dexa) in patients with lumbar 1~l4 vertebral bone mineral density, the T value is less than 2.5 SD. (2) After bed rest, support, painkillers such as conservative treatment in February, the pain still exist and serious. (3) MRI performance for high T2WI and STIR signals, or see liquid accumulation drafts, vacuum). (4) Taps pain location and imaging findings consistent.
Exclusion criteria: (1) Caused by spinal tumors, infections such as vertebral pathological fracture. (2) Combined nerve injury patient. (3) Memory, treatment and follow-up of compliance.
PKP holds surgery and treatment process
Patients prone position, abdominal dangling and maintain stretch thoracic lumbar segment, 2.0% lidocaine local infiltration anesthesia, c-shaped arm fluoroscopy monitoring work with casing under the needle through the pedicle of puncture, usually on the left side of the 9-10 o’clock, 2-3 o’clock position on the right side into the needle, needle point reached after pedicle, vertebral body around the inner edge, pull out the needle, establish working channel. NIVC group: after using solid enlarge pulp, fanterior 1/3 fracture in a balloon, a balloon expansion will collapse of vertebral body up reset; IVC groups: negative pressure suction first vertebral fracture contents [13], with a balloon expansion reset. The basic restore vertebral body height or balloon expansion contact edge vertebral body bone cortex, stop expansion, remove the balloon. Under the perspective to pass through the work in wire drawing stage bone cement casing injection fracture vertebral body, such as side piercing filled with bone cement did not diffuse to the vertebral body center line, line of lateral pedicle puncture filled in. Intraoperative closely monitoring vital signs and unwell feeling, pay attention to the feeling of lower limbs, activity. Stay in bed for eight hours postoperatively, waist circumference of bed recovery activities. Postoperative give fight osteoporosis treatment, 2~7 days after discharge.
Clinical effect assessment
Record the operation time, bone cement perfusion in every PKP holds operation. Assessment the visual analogue scale (VAS), Oswestry dysfunctional index (ODI) of the patients at preoperative and postoperative follow-up time to determine the clinical curative effect and recovery.
Imaging evaluation
X ray film was employed to monitor the fracture fanterior margin relative height, local convex Angle and the status of leakage of bone cement at postoperation and the follow-up periods.
Fanterior edge relative height = wounded vertebral height/average height of the up and down wounded vertebral height × 100%.
Statistical analysis
All data were presented as mean ± S.D, and analyzed using Student’s t-test and one-way ANOVA analysis to determine the levels of significance. A P value less than 0.05 or 0.01 was considered statistically significant. Statistical analysis was done with SPSS/Win19.0 software (SPSS Inc., Chicago, IL).
Results
General results
In all of the 118 CPOVCFs patients, 73 examples distribute in the NIVC group, and 45 samples distribute in IVC group. The fractures distribute in the range of T7 to L5 (and mainly distribute in T11-L2 thoracic lumbar segment). There were no significant differences for the patients’ age, gender, involving segment, pain, bone mineral density, length of hospital stay, and follow-up time between the two groups (Table 1).
Table 1.
Clinical characteristics of patients
| Characteristic parameters | NIVC group (n = 73) | IVC group (n = 45) |
|---|---|---|
| Age (year) | 69.1 ± 6.8 | 70.6 ± 6.5 |
| Gender ratio (F:M) | 44:29 | 26:19 |
| Spinal level of OVFC-no (%) | ||
| T7-T10 | 4 (5) | 3 (7) |
| T11 | 9 (12) | 4 (9) |
| T12 | 19 (26) | 16 (36) |
| L1 | 22 (30) | 11 (24) |
| L2 | 13 (18) | 6 (13) |
| L3-L5 | 6 (9) | 5 (11) |
| Duration from OVFC to PKP (week) | 15.2 ± 6.4 | 16.7 ± 8.5 |
| Bone density (-) | 3.44 ± 0.37 | 3.53 ± 0.44 |
| Operation time (min) | 35.7 ± 6.9 | 34.4 ± 5.9 |
| Amount of bone cement injected (ml)* | 4.0 ± 0.9 | 5.5 ± 1.2 |
| Length of Stay (day) | 4.6 ± 1.3 | 5.1 ± 2.4 |
| Duration of follow-up (month) | 18.9 ± 9.4 | 19.4 ± 10.2 |
P<0.05 for the comparison between the two groups.
PKP holds the treatment process
All of the patients in two groups underwent a safe operation, and no blood vessel damage, nerve damage, and pulmonary embolism were occurred in the operation.
For the operating time of PKP holds, 35.7 ± 6.9 min for the NIVC group, 34.4 ± 5.9 min for the IVC group. There were significant differences for the operation time between the two groups (P>0.05).
For the bone cement perfusion measure, 4.0 ± 0.9 ml in NIVC group, and 5.5 ± 1.2 ml in IVC group. There were significant differences for the bone cement perfusion measure between the two groups (P<0.05) (Table 1).
Clinical effect assessment
VAS (Figure 2): After the operation, the back pain was significantly reduced at post-operation compared to the pre-operation (P<0.05). Also, the VAS scores were significantly improved at the post-operation compared to the pre-operation (P<0.5). However, there were not significant differences between the two groups both at post-operation and pre-operation (P>0.05).
Figure 2.
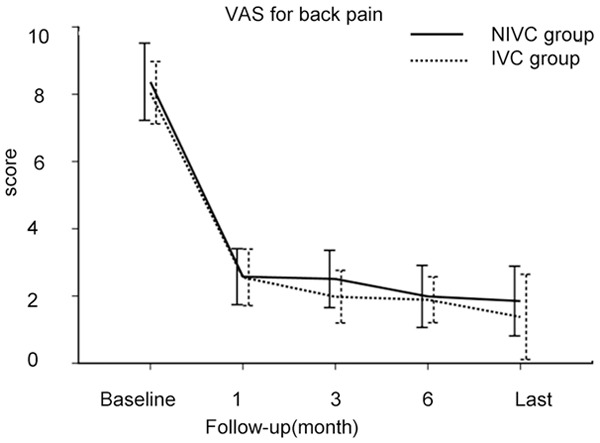
VAS for back pain before PKP and during the period of follow-up between the two groups.
ODI score (Figure 3): Both of the active functions and the ODI scores were improved at the post-operation compared to the post-operation (P<0.05). However, there were not significant differences between the two groups both at post-operation and pre-operation (P>0.05).
Figure 3.
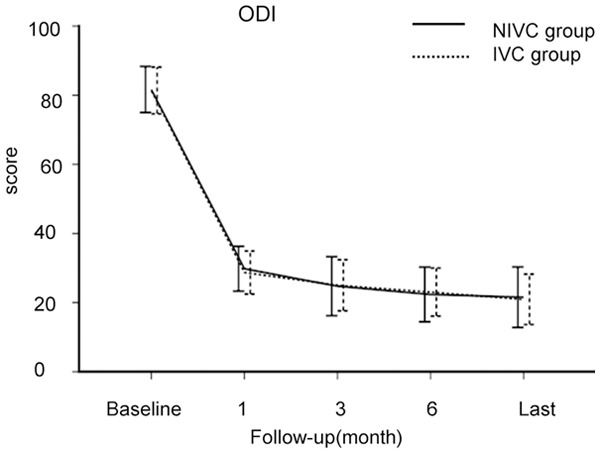
ODI before PKP and during the period of follow-up between the two groups.
Imaging results
There were no significant differences for the fanterior edge after relative height and local convex Angle at the pre-operation (P>0.05).
Fanterior edge relative height (Table 2): The fanterior edge relative height was significantly increased at post-operation compared to the pre-operation (P<0.05). Meanwhile, the therapeutic effects of IVC group were better compared to the NIVC group (P<0.05).
Table 2.
Comparison of relative vertebral anterior height of preoperative, 3 day after cement augmentation and the time of last follow-up
| Preoperative | 3 days postoperative | The last follow-up | |
|---|---|---|---|
| NIVC (%) | 62.9 ± 7.9 | 75.1 ± 7.5* | 73.1 ± 8.4* |
| IVC (%) | 55.5 ± 13.6 | 77.5 ± 7.2*,# | 75.3 ± 12.1*,# |
Compared with the preoperative group, P<0.05.
P<0.05 for the comparison between the NIVC and IVC group.
Local convex Angle (Table 3): The local convex angles were significantly decreased at post-operation compared to the pre-operation (P<0.05).
Table 3.
Comparison of kyphotic angle of preoperative, 3 day after cement augmentation and the time of last follow-up
| Preoperative | 3 days postoperative | The last follow-up | |
|---|---|---|---|
| NIVC (%) | 22.5 ± 4.2 | 12.5 ± 2.9* | 13.6 ± 2.5* |
| IVC (%) | 24.6 ± 4.4 | 13.2 ± 2.6* | 13.4 ± 4.1* |
Compared with the preoperative group, P<0.05.
Complications
There were 7 case (9.6%) with bone cement leakage in NIVC group, and 5 cases (11.1%) in IVC group (no significant difference, P>0.05). All the bone cement leakage patients without the complications of nerve damage, pulmonary embolism, and etc.
During follow-up period, there were 12 cases (16 adjacent segment vertebral compression fractures) in NIVC group, and 8 cases (11 adjacent segment vertebral compression fractures) in IVC group.
Discussion
Our research shows that PKP holds CPOVCFs patients treated effectively, restore vertebral body height, quickly relieve pain, and improve the quality of life. CPOVCFs MRI manifestation of patients with vertebral body, T2WI and STIR high signal or fluid accumulation), vacuum sign, suggest fracture is failed to heal and vertebral instability [8]. This is the important reason for the lower back in older people with chronic pain, conservative treatment the effect not beautiful. Therefore, for patients with CPOVCFs, most scholars advocate surgery, surgery effect is good [14-20].
We found that, compared to the NIVC vertebral fracture, PKP holds can significantly improve the IVC fracture of vertebral body height, significantly reduce the spine after partial protrusion deformity. IVC fractures, the vertebral body bone cortex discontinuous ahead, vertebral body height change with position and change often, this is good for surgery to restore vertebral body height in the process of [21]. Past research has shown that PKP holds the intraoperative factors including position [22] is beneficial to fracture, fracture type and amount of bone cement injection [23,24]. For this type of fracture, we was hyperextension by patient position, open the application of balloon and high-pressure injection of bone cement with high viscosity larger doses to complete a good reset. Our research shows that: group IVC of bone cement injection quantity is more, the degree of vertebral body fracture reduction is bigger also. More bone cement perfusion protrusion deformity after reduction, improved the spinal sagittal balance [25]. For the NIVC vertebral fracture, due to the continuous edge vertebral body bone, the reset ability weakened [18]. But also the scholar thinks, PKP holds also can obviously recover NIVC height. WU [3], studied 92 patients with subacute OVCFs, found after PKP holds the convex Angle improved after IVC group 9.14 degrees, vertebral compression reduction by 20.09%, while NIVC group was 8.76 degrees Fahrenheit and 20.23%, respectively. After in vertebral body bone cement solidification, the fracture piece together, achieve the purpose of stable fractures [26], quickly relieve patients’ pain symptoms.
In the treatment of CPOVCFs, complications of bone cement leakage happen quite often, reported as high as 41.5% [10]. Fortunately, most of the bone cement leakage rarely causes serious symptoms [26]. Vertebral body patients with IVC PKP holds the treatment, the higher rates of bone cement permeability to the adjacent intervertebral disc [3,27], at the same time, also should be alert to leakage of bone cement to the spinal canal, lest cause spinal cord compression [10]. Our bone cement leakage rate was 10.2%, lower than document report. We adopt the method is: on preoperative imaging evaluation, vertebral body bone edge defect, if any, is adopted by several times with bone cement injection method, with a small amount of bone cement block bone edge defect first, after waiting for bone cement solidification and large dose injection of bone cement with high viscosity. Intraoperative still needs strict imaging monitoring, such as found that leakage of bone cement began, is slow or stop the injections.
In the process of follow-up, there were 16.9% patients with adjacent segment fracture, the majority of patients have a willingness to accept surgery again. The study found that the happening of the adjacent segment fracture with low serum 25(OH)D levels and low BMD, low BMI, and intradiscal cement leakage on 28 to 30. Civelek [31] suggest vertebral body filled with bone cement, as far as possible after correction convex deformity, and restore the spinal sagittal balance, in order to reduce the adjacent segment fracture. Some scholars reported IVC line after PKP holds treatment, job responsibility disease may also be compressed again [32]. We have not seen this kind of circumstance, but follow-up is rare to find one bone cement loose shift, and destroyed the upper vertebral body, need operation treatment. This complication is a reminder that we need to adopt some methods to improve bone cement and bone anchor close degree.
In conclusion, PKP holds is the presence or absence of the IVC CPOVCFs, which is a safe and effective treatment method. For patients with IVC, PKP holds can significantly improve the fracture of vertebral body height, significantly reduce the spine after partial protrusion deformity.
Acknowledgements
This study was granted by the pharmaceutical and health care in shandong province science and technology development plan project (Grant No. 2013 ws0140); The ministry of health, medical and health science and technology development program (Grant No. W2012ZT35).
Disclosure of conflict of interest
None.
References
- 1.Hoshino M, Nakamura H, Terai H, Tsujio T, Nabeta M, Namikawa T, Matsumura A, Suzuki A, Takayama K, Takaoka K. Factors affecting neurological deficits and intractable back pain in patients with insufficient bone union following osteoporotic vertebral fracture. Eur Spine J. 2009;18:1279–1286. doi: 10.1007/s00586-009-1041-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ito Y, Hasegawa Y, Toda K, Nakahara S. Pathogenesis and diagnosis of delayed vertebral collapse resulting from osteoporotic spinal fracture. Spine J. 2002;2:101–106. doi: 10.1016/s1529-9430(01)00165-6. [DOI] [PubMed] [Google Scholar]
- 3.Wu AM, Lin ZK, Ni WF, Chi YL, Xu HZ, Wang XY, Huang QS. The existence of intravertebral cleft impact on outcomes of nonacute osteoporotic vertebral compression fractures patients treated by percutaneous kyphoplasty: a comparative study. J Spinal Disord Tech. 2014;27:E88–93. doi: 10.1097/BSD.0b013e31829142bf. [DOI] [PubMed] [Google Scholar]
- 4.Yang H, Wang G, Liu J, Ebraheim NA, Niu G, Hiltner L, Lee AH, Tang T. Balloon kyphoplasty in the treatment of osteoporotic vertebral compression fracture nonunion. Orthopedics. 2010;33:24. doi: 10.3928/01477447-20091124-28. [DOI] [PubMed] [Google Scholar]
- 5.Chen B, Fan S, Zhao F. Percutaneous balloon kyphoplasty of osteoporotic vertebral compression fractures with intravertebral cleft. Indian J Orthop. 2014;48:53–59. doi: 10.4103/0019-5413.125498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Edidin AA, Ong KL, Lau E, Kurtz SM. Life expectancy following diagnosis of a vertebral compression fracture. Osteoporos Int. 2013;24:451–458. doi: 10.1007/s00198-012-1965-2. [DOI] [PubMed] [Google Scholar]
- 7.Wang G, Yang H, Chen K. Osteoporotic vertebral compression fractures with an intravertebral cleft treated by percutaneous balloon kyphoplasty. J Bone Joint Surg Br. 2010;92:1553–1557. doi: 10.1302/0301-620X.92B11.24671. [DOI] [PubMed] [Google Scholar]
- 8.Kawaguchi S, Horigome K, Yajima H, Oda T, Kii Y, Ida K, Yoshimoto M, Iba K, Takebayashi T, Yamashita T. Symptomatic relevance of intravertebral cleft in patients with osteoporotic vertebral fracture. J Neurosurg Spine. 2010;13:267–275. doi: 10.3171/2010.3.SPINE09364. [DOI] [PubMed] [Google Scholar]
- 9.Movsky Y, Anekstein Y, Shalmon E, Peer A. Vacuum clefts of the vertebral bodies. AJNR Am J Neuroradiol. 2005;26:1634–1640. [PMC free article] [PubMed] [Google Scholar]
- 10.Wang C, Fan S, Liu J, Suyou L, Shan Z, Zhao F. Basivertebral foramen could be connected with intravertebral cleft: a potential risk factor of cement leakage in percutaneous kyphoplasty. Spine J. 2014;14:1551–1558. doi: 10.1016/j.spinee.2013.09.025. [DOI] [PubMed] [Google Scholar]
- 11.Hasegawa K, Homma T, Uchiyama S, Takahashi H. Vertebral pseudarthrosis in the osteoporotic spine. Spine. 1998;23:2201–2206. doi: 10.1097/00007632-199810150-00011. [DOI] [PubMed] [Google Scholar]
- 12.Ryu CW, Han H, Lee YM, Lim MK. The intravertebral cleft in benign vertebral compression fracture: the diagnostic performance of non-enhanced MRI and fat-suppressed contrast-enhanced MRI. Br J Radiol. 2009;82:976–981. doi: 10.1259/bjr/57527063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Koike Y, Takizawa K, Ogawa Y, Fujikawa A, Yoshimatsu M, Nakajima Y. Percutaneous vertebroplasty for vertebral compression fractures with intravertebral cleft: cement injection under vacuum aspiration. J Vasc Interv Radiol. 2011;22:1721–1726. doi: 10.1016/j.jvir.2011.08.021. [DOI] [PubMed] [Google Scholar]
- 14.Nakano M, Kawaquchi Y, Kimura T, Hirano N. Transpedicular vertebroplasty after intravertebral cavity formation versus conservative treatment for osteoporotic burst fractures. Spine J. 2014;14:39–48. doi: 10.1016/j.spinee.2013.03.016. [DOI] [PubMed] [Google Scholar]
- 15.Patil S, Rawall S, Singh D, Mohan K, Nagad P, Shial B, Pawar U, Nene A. Surgical patterns in osteoporotic vertebral compression fractures. Eur Spine J. 2013;22:883–891. doi: 10.1007/s00586-012-2508-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nakamae T, Fujimoto Y, Yamada K, Takata H, Shimbo T, Tsuchida Y. Percutaneous vertebroplasty for osteoporotic vertebral compression fracture with intravertebral cleft associated with delayed neurologic deficit. Eur Spine J. 2013;22:1624–1632. doi: 10.1007/s00586-013-2686-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nieuwenhuijse MJ, van Erkel AR, Dijkstra PD. Percutaneous vertebroplasty for subacute and chronic painful osteoporotic vertebral compression fractures can safely be undertaken in the first year after the onset of symptoms. J Bone Joint Surg Br. 2012;94:815–820. doi: 10.1302/0301-620X.94B6.28368. [DOI] [PubMed] [Google Scholar]
- 18.Sun G, Jin P, Li M, Liu XW, Li FD. Height restoration and wedge angle correction effects of percutaneous vertebroplasty: association with intraosseous clefts. Eur Radiol. 2011;21:2597–2603. doi: 10.1007/s00330-011-2218-z. [DOI] [PubMed] [Google Scholar]
- 19.Saito F, Takahashi K, Tanaka S, Torio T, Iizuka H, Wei C, Oda H. Effects of vertebroplasty for delayed-onset paraplegia caused by vertebral pseudarthrosis. J Orthop Sci. 2011;16:673–681. doi: 10.1007/s00776-011-0155-y. [DOI] [PubMed] [Google Scholar]
- 20.Lee SH, Kim ES, Eoh W. Cement augmented anterior reconstruction with short posterior instrumentation: a less invasive surgical option for Kummell’s disease with cord compression. J Clin Neurosci. 2011;18:509–514. doi: 10.1016/j.jocn.2010.07.139. [DOI] [PubMed] [Google Scholar]
- 21.Yokoyama K, Yamada M, Tanaka H, Ito Y, Hirano M, Kuroiwa T. In not only vertebroplasty but also kyphoplasty, the resolution of vertebral deformities depends on vertebral mobility. AJNR Am J Neuroradiol. 2013;34:1474–1478. doi: 10.3174/ajnr.A3424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cho JH, Shin SI, Lee JH, Yeom JS, Chang BS, Lee CK. Usefulness of prone cross-table lateral radiographs in vertebral compression fractures. Clin Orthop Surg. 2013;5:195–201. doi: 10.4055/cios.2013.5.3.195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Xu C, Liu HX, Xu HZ. Analysis of related factors on the deformity correction of balloon kyphoplasty. AJNR Am J Neuroradiol. 2014;35:202–206. doi: 10.3174/ajnr.A3617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Krüger A, Noriega D, Figiel J, Dorschel C, Ruchholtz S, Oberkircher L. Height restoration and maintenance after treating unstable osteoporotic vertebral compression fractures by cement augmentation is dependent on the cement volume used. Clin Biomech (Bristol, Avon) 2013;28:725–730. doi: 10.1016/j.clinbiomech.2013.06.007. [DOI] [PubMed] [Google Scholar]
- 25.Yokoyama K, Kawanishi M, Yamada M, Tanaka H, Ito Y, Hirano M, Kuroiwa T. Validity of intervertebral bone cement infusion for painful vertebral compression fractures based on the presence of vertebral mobility. AJNR Am J Neuroradiol. 2013;34:228–232. doi: 10.3174/ajnr.A3160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pedicelli A, Lozupone E, Gatto A, Gulino P, D’Argento F, Capozzi A, Colosimo C. Vertebra plana: reappraisal of a contraindication to percutaneous vertebroplasty. Eur J Radiol. 2013;82:2303–2308. doi: 10.1016/j.ejrad.2013.08.042. [DOI] [PubMed] [Google Scholar]
- 27.Nieuwenhuijse MJ, Van Erkel AR, Dijkstra PD. Cement leakage in percutaneous vertebroplasty for osteoporotic vertebral compression fractures: identification of risk factors. Spine J. 2011;11:839–848. doi: 10.1016/j.spinee.2011.07.027. [DOI] [PubMed] [Google Scholar]
- 28.Zhang Z, Fan J, Ding Q, Wu M, Yin G. Risk factors for new osteoporotic vertebral compression fractures after vertebroplasty: a systematic review and meta-analysis. J Spinal Disord Tech. 2013;26:E150–157. doi: 10.1097/BSD.0b013e31827412a5. [DOI] [PubMed] [Google Scholar]
- 29.Martinez-Ferrer A, Blasco J, Carrasco JL, Macho JM, Román LS, López A, Monegal A, Guañabens N, Peris P. Risk factors for the development of vertebral fractures after percutaneous vertebroplasty. J Bone Miner Res. 2013;28:1821–1829. doi: 10.1002/jbmr.1899. [DOI] [PubMed] [Google Scholar]
- 30.Wang YT, Wu XT, Chen H, Wang C, Mao ZB. Adjacent-level-symptomatic fracture after percutaneous vertebral augmentation of osteoporotic vertebral compression fracture: a retrospective analysis. J Orthop Sci. 2014;19:868–876. doi: 10.1007/s00776-014-0610-7. [DOI] [PubMed] [Google Scholar]
- 31.Civelek E, Cansever T, Yilmaz C, Kabatas S, Gülşen S, Aydemir F, Altιnörs N, Caner H. The retrospective analysis of the effect of balloon kyphoplasty to the adjacent-segment fracture in 171 patients. J Spinal Disord Tech. 2014;27:98–104. doi: 10.1097/bsd.0b013e31824e9b98. [DOI] [PubMed] [Google Scholar]
- 32.Kim YY, Rhyu KW. Recompression of vertebral body after balloon kyphoplasty for osteoporotic vertebral compression fracture. Eur Spine J. 2010;19:1907–1912. doi: 10.1007/s00586-010-1479-6. [DOI] [PMC free article] [PubMed] [Google Scholar]