Abstract
Background and aims: Endoscopic Interventional Treatment is of little trauma and less complications in the treatment of esophageal tumor and leads to faster recovery and fewer days of hospitalization. This study was aimed to investigate the safety and efficacy of endoscopic interventional therapy for huge esophageal tumor arising in the muscularis propria. Methods: The patient was treated by submucosal tunneling endoscopic resection (STER). Results: The huge esophageal tumor was resected completely by STER technique, with little trauma and less complications. The size of the resected tumor was 5.5×3.5×3.0 cm. Conclusion: Submucosal tunneling endoscopic resection is a safe and efficient technique for treating Huge Esophageal Tumor originating from muscularis propria layer.
Keywords: Huge esophageal tumor, muscularis propria, submucosal tunneling endoscopic resection
Introduction
In recent years, with the improvement of endoscopic diagnosis and widespread of endoscopic ultrasonography, more and more esophageal muscularis propria tumors are detected. Although most of the tumors were benign tumors, a series of serious problems such as malignancy, bleeding, obstruction and important organs oppression can occur with the growing of the tumor. Furthermore, it is possible that the benign ones may mutate into malignant [1]. Most patients have strong demand to remove the tumor because of psychological stress. So it is still required early removal. As the esophageal tumors arising in the muscularis propria are in deep level, the traditional therapy for these tumors is traditional open surgery and laparoscopic surgery, which is traumatic, expensive and difficult to accept for the patients. Endoscopic therapy improved significantly currently, especially the invention of STER technology used by Chinese scholars in 2010 on the base of Peroral Endoscopic Myotomy (POEM) [2]. Esophageal mucosal tumor was first operated by STER in Shanghai Zhongshan Hosptal in September, 2010 [3]. Esophageal tumor arising in the muscularis propria was first operated by STER technology in Shandong Provincial Hospital affiliated to Shandong University in 2th November, 2011. The tumor of this case diagnosed esophageal tumor arising in the muscularis propria by EUS resected by STER was the biggest one.
Material and methods
Patient
A 30-year-old female was admitted with dysphagia for 3 months and found esophageal submucosal tumor for 1 month. On admission, physical examination revealed no discomfort. The esophageal submucosal tumor was 30~35 cm from the incisors with gastroscopy. The tumor size was 5×3 cm with smooth surface (Figure 1A). An oval hypoechoic mass originated in the esophageal muscularis propria by endoscopic ultrasonography (EUS) (Figure 1B).
Figure 1.
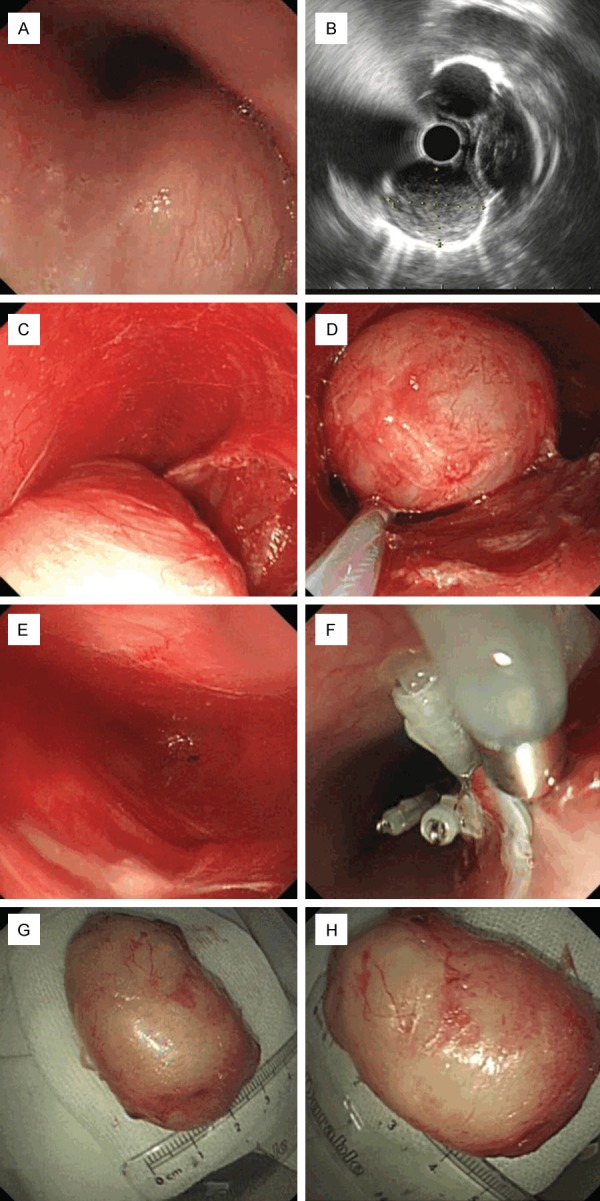
A: Submucosal bump at the esophagus. B: An oval hypoechoic mass originated in the esophagus muscularis propria by EUS. The edge of the tumor was clear with hypoechoic halo ring. C: The tumor was from the tumor bed after separated with the surrounding tissue. D: The tumor was drawing upstream by snare trap along the tunnel. E: No bleeding inside the tumor bed and the tunnel. F: Seal the mucosal incision with titanium clips. G and H: The size of the tumor.
The patient was given conventional CT scan before operation to have an understanding of anatomy structures around the tumor, particularly pay attention to the arteries around the tumor and the tumor protruding into the cavity. The written informed consent was signed by the patient, who had been told possible procedure-related benefits and risks (including possible complications and corresponding managements), as well as the alternative treatment options. According to the location and size of the lesion, we think that the best treatment was STER.
Methods
The patient was performed endoscopy first to observe the tumor size, color, shape, texture, activity, relationship with the surrounding tissues, and so on. Routine endoscopic ultrasonography examination was done before STRE to confirm that the tumor originated from the muscularis propria.
Materials
The patient was treated with STER under general anesthesia in the operating room. Intravenous antibiotics were used to prevent infection half an hour before surgery. Second-generation cephalosporin was the first choice. If the patient was allergic to cephalosporins, nitromidazole, such as tinidazole, can be applied two hours before surgery. The operation was performed using a single-channel endoscope (GIF-Q260J, Olympus) and/or a dual-channel endoscope (GIF-2TQ260M, Olympus). Other equipment and accessories included VIO 200s high frequency electric cutting device (ERBE), APC 300 Argon plasma coagulation (ERBE), an endoscopic carbon dioxide regulation unit (Co., Ltd, JSQB-PI), an endoscopic flushing (Olympus), a transparent cap (NM-200L-0521, Olympus), an injection needle (SD-230U-20, Olympus), an insulated-tip knife (KD-611L, IT2, Olympus), Double helix snare (HX-610-135L, Olympus), a hot biopsy forceps (FD-410LR, Olympus).
The procedures of STER
The patient was treated with Submucosal Tunnelling Endoscopic Resection (STER): 1. Mark the esophageal lesions after rinsing with saline and inject Glycerol fructose indigo carmine on esophageal mucosa 6 cm from the tumor (24 cm from the incisors). Make a longitudinal incision in the mucous membrane layer to the submucosa to establish the submucosal tunnel top (Figure 1C). 2. Establish the submucosal tunnel (Figure 1D) and downward gradually to expose the tumor completely and separate the tumor with the surrounding tissue (Figure 1E). 3. The tumor resected was sent for pathological analysis. Stanch bleeding inside the submucosal tunnel and close the mucosal incision with hemostatic clips (Figure 1F). Pathological diagnosis: No pneumothorax, mediastinal emphysema, delayed bleeding, esophageal leak, mediastinum or pleural infection and other complications occur after treatment with STER. Gastrointestinal decompression for 3 days after surgery and began eating at the first four day. The patient was discharged at the 7th day.
Histology and immunohistochemistry
The samples were fixed in 4% formalin and embedded in paraffin. Sections were cut and stained with hematoxylin & eosin (H&E). In order to confirm the tissue sources, the immunohistochemical staining was performed. The antibodies applied are including S-100, CD34, CD117, Dog-1, SMA and Ki67. The patient was observed for 48 hours, treated with proton pump inhibitor and parenteral nutrition support. Antibiotics were continued for 48 h after STER.
Postoperative follow-up
We suggested that the patient to reexamine endoscopy 3, 6, and 12 months after surgery and to observe the wound healing and to observe whether there is residual or recurrent. During the follow-up period of 12 months, wound healing was satisfied, and no residual or recurrent lesions were found.
Results
Endoscopy findings
The patient being performed by endoscopy had submucosal bump with oval appearance. The mass had smooth mucosa, without ulcers or bleedings. The diameter of the lesion is 5.5 cm by EUS examination. The mass originated from the esophageal muscularis propria, shown as oval hypoechoic appearance, with clear boundary and hypoechoic halo ring. The size of the resected tumor was 5.5×3.5×3.0 cm (Figure 1G, 1H).
Endoscopic treatment outcomes
The patient was performed STER therapy successfully. Operation time lasted about 45 minutes. The wound was closed with titanium clips completely. The lesion was removed thoroughly, with less bleeding and no perforation.
Postoperative status and follow-up
No late bleeding, inflammation or infection occurred after surgery. The wound healed well at the third-month, the six-month, and the one-year follow-ups. No recurrence was found during follow-up.
Pathological results
Esophageal leiomyoma is mainly composed of bland spindle cells and shows low or moderate cellularity. The cells have eosinophilic, fibrillary and clumped cytoplasm, which are scattered in the lymphoid-rich stroma (Figure 2A). High magnification showing nodules of spindle cells with oval elongated nuclei (Figure 2B). Immunohistochemical stains were negative for S-100 (Figure 3A), CD-34 (Figure 3B), c-Kit (CD117) (Figure 3C) and DOG-1 (Figure 3D) markers, but positive for smooth muscle actin (SMA) (Figure 3E) and Ki-67 (Figure 3F) markers. The Ki-67 labeling index was not high (up to 1%) (Figure 3F). Based on these histologic and immunohistochemical features, our patient was diagnosed as leiomyoma of esophagus.
Figure 2.
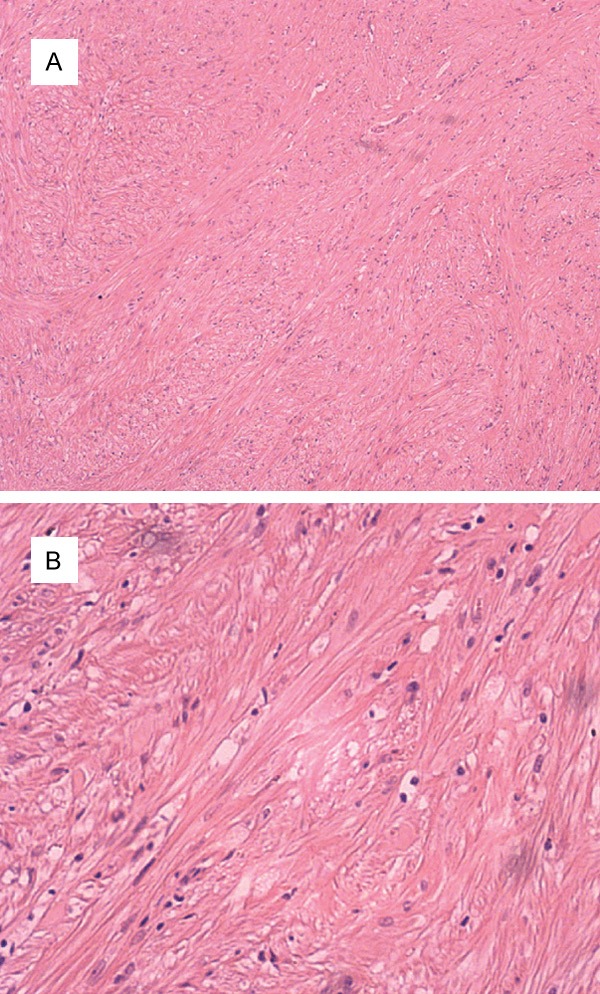
A: The cells have eosinophilic, fibrillary and clumped cytoplasm, which are scattered in the lymphoid-rich stroma (×100 magnification microscope). B: High magnification showing fasciles of spindle smooth cells with moderate nuclei (×400 magnification microscope).
Figure 3.
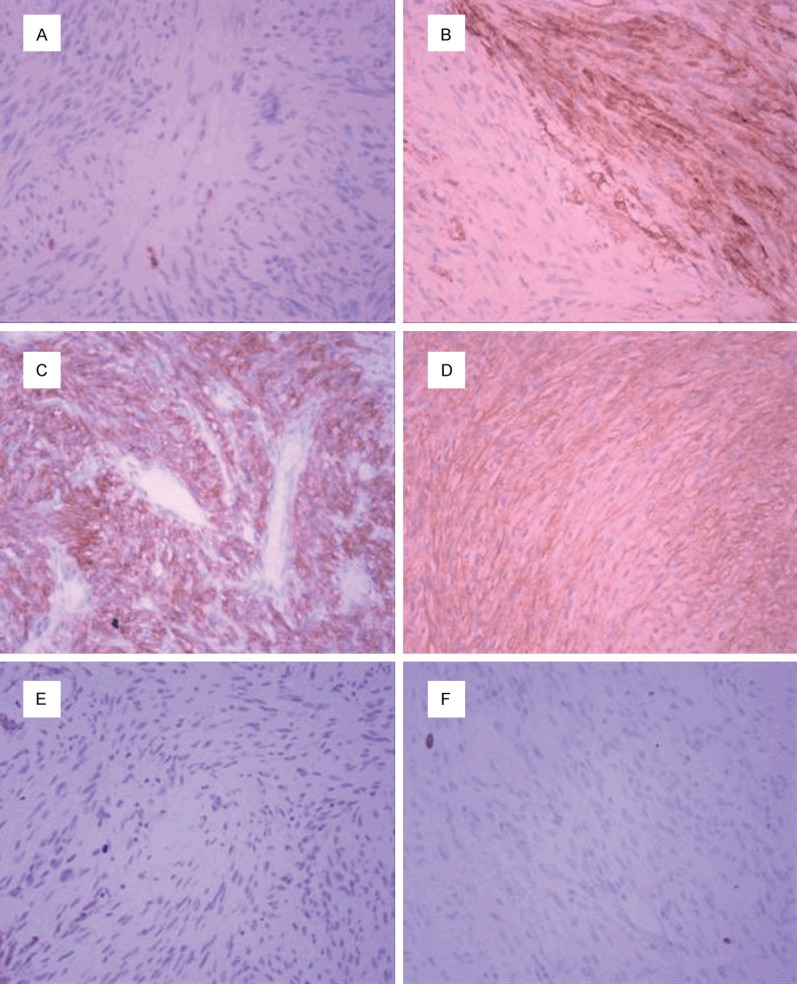
A: Immunohistochemical stains were negative for S-100 marker. B: Immunohistochemical stains were negative for CD-34 marker. C: Immunohistochemical stains were negative for c-Kit (CD117) marker. D: Immunohistochemical stains were negative for DOG-1 marker. E: Immunohistochemical stains were positive for smooth muscle actin (SMA) marker. F: Immunohistochemical stains were positive for marker.
Discussion
With the development of endoscopic techniques, equipment and instruments, more and more advanced endoscopic techniques were applied in clinic. There are many methods, including endoscopic submucosal excavation (ESE), endoscopic full-thickness resection (EFR) and submucosal tunelling endoscopic resection (STER), which are more and more widely used in clinical practices. Tunnel endoscopy is a new therapeutic technique developed from natural orifice endoscopic transluminal surgery (NOTES) [4] and endoscopic submucosal dissection [5]. The submucosal tunneling endoscopic resection for submucosal tumors of the esophagogastric junction originating from the muscularis propria layer is safe and effective, provided accurate histopathologic evaluation, and is curative for SMTs of the deep MP layers at the EGJ. But the average maximum diameter of the lesions was 21.5 mm (range 6-35 mm) [6].
Compared with traditional open surgery and laparoscopic surgery, the submucosal tunneling endoscopic resection is of little trauma and less complications, leading to faster recovery and fewer days of hospitalization. The volume of esophageal leiomyoma arising in the muscularis propria of this patient is the largest of all the patients treated by STER technology. The volume is significantly larger than 35 mm reported at home and abroad and with fewer complications, clear pathological diagnosis and good follow-up effect [6]. Therefore, I believe that almost of the esophageal tumors arising in the muscularis propria diagnosed by EUS can be treated by STER technology. The advantage is to resect the lesion, including its underlying muscularis propria layer and serosa, completely and to maintain the integrity of the digestive tract. It can avoid gastrointestinal fistulas and abdominal cavity secondary infection caused by Endoscopic Submucosal Dissection (ESD). The resection of gastrointestinal tumor arising in the muscularis propria become less invasive and more safety. The patients are less suffering and the hospital cost is lower.
Acknowledgements
This work supported by the Natural Science Foundation of Shandong Province of China (ZR2014HM106).
Disclosure of conflict of interest
None.
References
- 1.Xu MD, Yao LQ. Clinical value of tunnel endoscopy for the treatment of esophagogastric diseases. Chin J Gastrointesi Surg. 2012;15:659–661. [PubMed] [Google Scholar]
- 2.Inoue H, Minami H, Kobayashi Y, Sato Y, Kaga M, Suzuki M, Satodate H, Odaka N, Itoh H, Kudo S. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy. 2010;4:265–271. doi: 10.1055/s-0029-1244080. [DOI] [PubMed] [Google Scholar]
- 3.Xu MD, Cai MY, Zhou PH, Qin XY, Zhong YS, Chen WF, Hu JW, Zhang YQ, Ma LL, Qin WZ, Yao LQ. Submucosal tunneling endoscopic resection: a new technique for treating upper GI Submucosal tumors originating from the muscularis propria layer. Gastrointest Endosc. 2012;75:195–199. doi: 10.1016/j.gie.2011.08.018. [DOI] [PubMed] [Google Scholar]
- 4.Sumiyama K, Gostout CJ, Rajan E, Bakken TA, Knipschield MA. Submucosal endoscopy with mucosal flap safety valve. Gastrointest Endosc. 2007;65:688–694. doi: 10.1016/j.gie.2006.07.030. [DOI] [PubMed] [Google Scholar]
- 5.Lee CK, Lee SH, Chung IK, Lee TH, Lee SH, Kim HS, Park SH, Kim SJ, Kang GH, Cho HD. Human diagnostic transgastric peritoneoscopy with the submucosal tunnel technique performed with the patient under conscious sedation (with video) Gastrointest Endosc. 2010;72:889–891. doi: 10.1016/j.gie.2010.01.035. [DOI] [PubMed] [Google Scholar]
- 6.Wang XY, Xu MD, Yao LQ, Zhou PH, Pleskow D, Li QL, Zhang YQ, Chen WF, Zhong YS. Submucosal tunneling endoscopic resection for submucosal tumors of the esophagogastric junction originating from the muscularis propria layer: a feasibility study (with videos) Surg Endosc. 2014;28:1971–1977. doi: 10.1007/s00464-014-3420-2. [DOI] [PubMed] [Google Scholar]


