Abstract
Aims: The present study is to investigate changes in serum concentrations of matrix metalloproteinase-9 (MMP-9) and vascular endothelial growth factor (VEGF) before and after percutaneous ethanol injection (PEI) in primary hepatic carcinomas (PHC), and their effects on the prognosis. Methods: A total of 100 patients with PHC received PEI treatment in our hospital between July 2010 and July 2014. Another 100 PHC patients who had PHC resected were included as control group. For PEI treatment, anhydrous ethanol was slowly injected into the tumor every 2-3 days for consecutive 4-10 times. The evaluation of treatment efficacy was performed in accordance with the standards by Union for International Cancer Control. Serum concentrations of MMP-9 and VEGF were determined using enzyme-linked immunosorbent assay. The median values of MMP-9 and VEGF concentrations were used as the cutoff value to discriminate high and low MMP-9 and VEGF contents. Kaplan-Meier plots were used to examine how serum concentrations of MMP-9 and VEGF affected postoperative survival of PHC patients. Results: PEI treatment decreased the serum contents of MMP-9 and VEGF after the surgery. PEI had high effectiveness against PHC tumors during the surgery. PEI treatment led to higher survival rate in PHC patients compared with PHC resection. Serum levels of MMP-9 and VEGF were related to different Child grading, Kps scoring, BCLC staging and AFP contents. Lower preoperative serum concentrations of MMP-9 and VEGF might lead to longer survival time of PHC patients after PEI. Conclusions: PEI treatment alters serum concentrations of MMP-9 and VEGF in PHC patients, which may have great effect on the prognosis.
Keywords: Matrix metalloproteinase-9, vascular endothelial growth factor, percutaneous ethanol injection, primary hepatic carcinoma
Introduction
Primary hepatic carcinoma (PHC) is one of the most common malignant tumors in the world, with the survival rate being lower than 5% [1]. Due to the lack of the first symptoms and late diagnosis, only 10-40% patients with PHC are suitable for surgery. In addition, the postoperative recurrence rate was high, reaching 30-50% in 3 years and 85-95% in 5 years [1,2]. Treatment of PHC by percutaneous ethanol injection (PEI) guided by ultrasound has already been widely used clinically due to its easy operation, reliable effects, and low costs [3-5]. The growth of PHC is closely related to the overexpression of multiple growth factors, with complex molecular mechanisms [6]. Recent studies show that matrix metalloproteinase-9 (MMP-9) is related to tumor angiogenesis [7]. Vascular endothelial growth factor (VEGF) is a kind of pro-angiogenic growth factor that has the strongest effect known by now. Currently, there is neither report on changes in serum MMP-9 and VEGF concentrations after PHC treatment by PEI, nor the prediction of PHC prognosis according to these concentrations. In the present study, serum concentrations of MMP-9 and VEGF are monitored before and after PEI treatment, and relative factors that may have effects on the prognosis of PHC are evaluated.
Materials and methods
Patients
A total of 100 patients with PHC received PEI treatment in our hospital between July 2010 and July 2014. The inclusion criteria were: i) pathological diagnosis; ii) confirmed diagnosis by more than two types of imaging methods; iii) in accordance with Child staging (A/B) and Barcelona Clinic Liver Cancer (BCLC) staging (A/B); iv) normal coagulation. Exclusion criteria were: i) multiple metastases inside and outside the liver with portal vein invasion; ii) ascites; iii) abnormal coagulation; iv) levels of aminopherase being more than 3 times of normal values. Among the 100 patients who received PEI treatment, there were 46 males and 54 females, with an age range of 27-64 years (median age, 47 years). According to Child staging, 69 cases were A, and 31 cases were B. According to BCLC, 72 cases were A, and 28 cases were B. Another 100 PHC patients who had PHC resected were included as control group Table 1. All procedures were approved by the Ethics Committee of The Second Hospital of Ningbo City. Written informed consents were obtained from all patients or their families.
Table 1.
Basic clinical data of patients with PEI
| Parameters | No. of patients | |
|---|---|---|
| Age (years)* | > 45 | 76 |
| ≤ 45 | 34 | |
| Kps scores | 100 points | 52 |
| ≥ 90 points | 8 | |
| Liver function: Child grading | A | 35 |
| B | 65 | |
| Hepatitis | Hepatitis B virus | 57 |
| Hepatitis C virus | 35 | |
| Other | 8 | |
| BCLC staging | A | 56 |
| B | 44 | |
| AFP content (µg/L)** | > 400 µg/L | 45 |
| ≤ 400 µg/L | 15 | |
| Tumor diameter*** | > 3 cm | 68 |
| ≤ 3 cm | 32 | |
| Tumor number | Single tumor | 51 |
| Multiple tumors | 49 | |
Note: BCLC, Barcelona Clinic Liver Cancer. AFP, alpha-fetoprotein.
average age was 49.6 ± 14.9 years, and age range was 27-64 years.
average AFP content was 522.3 ± 197.8 µg/L, and range of AFP content was 124-900 µg/L.
average tumor diameter was 3.1 ± 1.4 cm, and range of tumor diameter was 1.6-5.4 cm.
PEI guided by ultrasound
The patients lay down in supine position, and were anaesthetized locally at puncture site using 2% lidocaine (5 ml). Under the guidance of ultrasound, anhydrous ethanol was slowly injected into the tumor every 2-3 days for consecutive 4-10 times. None of the patients received transcatheter arterial chemoembolization, chemotherapy or other special treatments during the surgery and follow-ups. The evaluation of treatment efficacy was performed in accordance with the standards by Union for International Cancer Control. A complete remission (CR) is defined as complete disappearance of all manifestations of tumors. A partial remission (PR) is defined for cancer as 50% or greater reduction in the measurable parameters of tumor growth. Stable disease (SD) is defined for cancer as < 50% reduction or ≤ 25% enlargement in the measurable parameters of tumor growth. Progressive disease (PD) is defined for cancer as > 25% enlargement in the measurable parameters of tumor growth.
Enzyme-linked immunosorbent assay (ELISA)
Peripheral venous blood (3 ml) was collected before and 1, 2 and 3 years after the surgery and stored at -80°C. Serum concentrations of MMP-9 and VEGF were determined using human Perforin ELISA kit (Dakewe Biotech Company, Shenzhen, China) according to the manufacturer’s manual. The absorbance of each sample was measured in replica using a microplate reader (PT-DR200Bs, Potenov Technology Co., Ltd., Beijing, China) under 450 nm. The median values of MMP-9 and VEGF concentrations were recorded and used as the cutoff value to discriminate high and low MMP-9 and VEGF contents.
Statistical analysis
The results were analyzed using SPSS 19.0 statistical software (IBM, Armonk, NY, USA). The data were expressed as means ± standard deviation. The differences before and after surgery were compared using t-test. Kaplan-Meier plots were used to examine how serum concentrations of MMP-9 and VEGF affected postoperative survival of PHC patients. P < 0.05 was considered statistically significant.
Results
PEI treatment decreases the serum contents of MMP-9 and VEGF after the surgery
To measure the serum contents of MMP-9 and VEGF before and after PEI treatment, ELISA was performed. Before PEI, the concentrations of MMP-9 and VEGF in patient group were significantly higher than those in control group (P < 0.001). In addition, the serum concentrations of MMP-9 and VEGF in patient group at year 1 and 2 after the surgery were significantly lower than those before the surgery, respectively (P < 0.001). However, the serum concentrations of MMP-9 and VEGF at year 3 after the surgery were increased to levels higher than those at year 2 after the surgery (P < 0.05) (Table 2). These results suggest that PEI treatment decreases the serum contents of MMP-9 and VEGF after the surgery.
Table 2.
Serum levels of matrix metalloproteinase-9 (MMP-9) and vascular endothelial growth factor (VEGF) before and after PEI treatment
| Groups | MMP-9 (ng/ml) | P values | VEGF (pg/ml) | P values | |
|---|---|---|---|---|---|
| Control group | 206.4 ± 105.7 | 219.9 ± 90.2 | |||
| Treatment groups | Before PEI | 313.7 ± 75.5 | 0.001 | 386.6 ± 107.4 | 0.001 |
| 1 year after PEI | 275.7 ± 89.2 | 0.000 | 246.6 ± 94.1 | 0.000 | |
| 2 years after PEI | 109.1 ± 56.6 | 0.000 | 83.1 ± 30.2 | 0.000 | |
| 3 years after PEI | 263.8 ± 90.6 | 0.006 | 204.8 ± 54.5 | 0.000 |
Note: MMP-9, matrix metalloproteinase-9; VEGF, vascular endothelial growth factor; PEI, percutaneous ethanol injection.
PEI has high effectiveness against PHC tumors during the surgery
To evaluate the sizes of tumors and to identify bleeding at the edges of the tumors, ultrasonography was used. Ultrasonographic images showed that PEI led to necrosis of the tumor, without bleeding signs (Figure 1). Using the evaluation criteria set by Union for International Cancer Control, 73 cases were CR, 15 cases were PR, 9 cases were SD, and 3 cases were PD, resulting in an effectiveness rate of 88.0%. The results indicate that PEI has high effectiveness against PHC tumors during the surgery.
Figure 1.
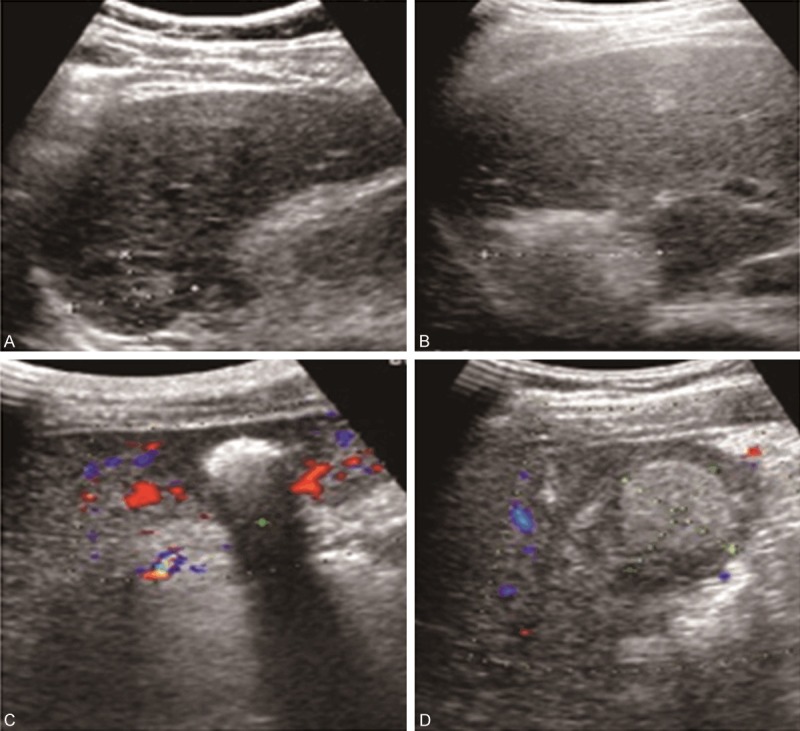
Ultrasonography before and after surgery. A. Ultrasound image obtained before PEI; B. Ultrasound image obtained immediately after PEI, showing enhanced postoperative echogenic nodules; C. Ultrasound image obtained one month after PEI, showing enhanced echogenic nodules and a little blood around the tumor; D. Ultrasound image obtained 6 months after PEI, showing enhanced echogenic nodules but not blood sign inside and around the tumor.
PEI treatment leads to higher survival rate in PHC patients compared with PHC resection
To investigate the survival rate of PHC patients after PEI, we followed up the patients for 3 years. In the treatment group, 12 cases were lost in follow-up, while 15 cases in control group were lost in follow-up. At year 1 and 2 after PEI, the survival rates of treatment group were not significantly different from those of control group (P > 0.05). However, the survival rate of treatment group at year 3 was significantly higher than that of control group (P < 0.05) (Table 3). The result suggests that PEI treatment leads to higher survival rate in PHC patients compared with PHC resection.
Table 3.
Survivals of patients with PHC at 1, 2 and 3 years after surgery
| Groups | Cases | Year 1 | Year 2 | Year 3 | |||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Cases | Survival rate | Cases | Survival rate | Cases | Survival rate | ||
| Treatment group | 88 | 84 | 95.4% | 72 | 81.8% | 61 | 69.3% |
| Control group | 85 | 81 | 95.2% | 68 | 80.0% | 52 | 61.1% |
| P values | > 0.005 | > 0.05 | < 0.05 | ||||
Preoperative serum levels of MMP-9 and VEGF are related to different Child grading, Kps scoring, BCLC staging and AFP contents
To study how different clinical characteristics correspond to the levels of MMP-9 and VEGF, we carried out ELISA. The data showed that different Child grading, Karnofsky performance scoring (Kps), BCLC staging, and alpha-fetoprotein (AFP) content led to significantly different serum concentrations of MMP-9 and VEGF (P < 0.05). However, differences in age, hepatitis type and tumor size failed to cause significantly different serum concentrations of MMP-9 and VEGF (P > 0.05) (Table 4). The results indicate that preoperative serum levels of MMP-9 and VEGF are related to different Child grading, Kps scoring, BCLC staging and AFP contents.
Table 4.
Serum concentrations of MMP-9 and VEGF under different clinical conditions before surgery
| Clinical characteristics | MMP-9 (ng/ml) | P values | VEGF (pg/ml) | P values | |
|---|---|---|---|---|---|
| Child grading | A | 301.3 ± 117.1 | 0.04 | 320.5 ± 170.4 | 0.05 |
| B | 396.8 ± 135.0 | 416.5 ± 154.1 | |||
| Kps scoring (points) | 100 | 234.6 ± 91.8 | 0.05 | 326.9 ± 74.4 | 0.02 |
| ≥ 90 | 425.5 ± 146.7 | 435.7 ± 186.2 | |||
| Vascular invasion | Yes | 436.7 ± 158.2 | 0.01 | 491.2 ± 209.8 | 0.01 |
| No | 366.0 ± 129.1 | 314.0 ± 167.2 | |||
| Types of hepatitis | Hepatitis B virus | 394.2 ± 152.7 | 0.75 | 488.6 ± 127.5 | 0.63 |
| Hepatitis C virus | 358.7 ± 173.0 | 351.0 ± 193.4 | |||
| Others | 400.7 ± 120.2 | 335.3 ± 185.1 | |||
| AFP content (µg/L) | > 400 | 413.7 ± 268.3 | 0.02 | 431.6 ± 194.9 | 0.08 |
| ≤ 400 | 371.2 ± 161.9 | 295.5 ± 98.3 | |||
| Tumor size | > 3 cm | 393.8 ± 174.2 | 0.67 | 391.4 ± 126.5 | 0.46 |
| ≤ 3 cm | 302.1 ± 102.9 | 291.4 ± 92.3 | |||
| Age (years) | > 60 | 321.7 ± 113.9 | 0.36 | 318.7 ± 138.4 | 0.72 |
| ≤ 60 | 296.5 ± 92.9 | 312.1 ± 100.3 | |||
| BCLC staging | A | 250.7 ± 82.8 | 0.03 | 359.1 ± 123.3 | 0.01 |
| B | 395.1 ± 106.6 | 438.9 ± 264.5 | |||
Note: MMP-9, matrix metalloproteinase-9; VEGF, vascular endothelial growth factor; BCLC, Barcelona Clinic Liver Cancer. AFP, alpha-fetoprotein.
Lower preoperative serum concentrations of MMP-9 and VEGF may lead to longer survival time of PHC patients after PEI
To test the effect of preoperative serum contents of MMP-9 and VEGF on the survival time of PHC patients, we performed Kaplan-Meier analysis. The median values of MMP-9 and VEGF concentrations were 321.9 ng/ml and 380.5 pg/ml, respectively. For MMP-9, 54 PHC patients had values greater than the median value; for VEGF, 51 patients had values greater than the median value. Kaplan-Meier analysis showed that PHC patients with serum MMP-9 and VEGF contents higher than median values had relatively shorter survival time (P < 0.05) (Figure 2). The result suggests that lower preoperative serum concentrations of MMP-9 and VEGF may lead to longer survival time of PHC patients after PEI.
Figure 2.
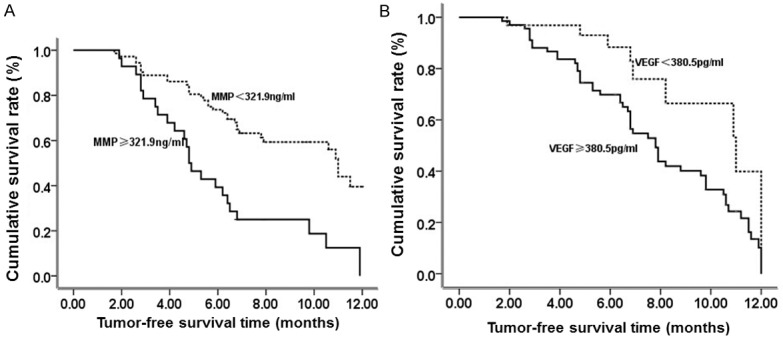
Progression-free survival curves after percutaneous ethanol injection. Effect of serum concentrations of MMP-9 (A) and VEGF (B) on the survival of patients with primary hepatic carcinoma after percutaneous ethanol injection was evaluated. Serum concentrations of MMP-9 and VEGF were determined using enzyme-linked immunosorbent assay. The median values of MMP-9 and VEGF concentrations were recorded and used as the cutoff value to discriminate high and low MMP-9 and VEGF contents. Kaplan-Meier analysis was performed to examine the survival rate and time of primary hepatic carcinoma patients after percutaneous ethanol injection.
Discussion
PHC has dual blood supplies and grows fast, usually leading to vascular invasion and metastasis. Therefore, the success rate of resection of PHC is low, with 90% recurrence rate within 5 years after surgery. As a minimally invasive treatment method, PEI is already widely used as a clinical treatment for PHC [8,9], effectively enhancing the survival rate of patients. It was reported that, after PEI treatment, the survival rates of PHC patients reached 93.7%, 73.8%, 53.1% and 47.6% at year 1, 3, 5 and 8, respectively [10]. The present study shows that the survival rates of PHC patients are 95.4%, 81.8% and 69.3% at year 1, 2 and 3 after PEI treatment. These results demonstrate that PEI treatment has good long-term effect for PHC and significantly prolongs the survival rate of PHC patients.
MMP-9 belongs to a protease family that is dependent on Zinc ions. Researches show that MMP-9 participates in various pathological processes such as angiogenesis, tumor invasion and metastasis, and inflammation responses. MMP-9 is overexpressed in many malignant tumors, playing important roles in the invasion and metastasis of malignant tumors. VEGF, as a kind of pro-angiogenic growth factor, usually induces endothelial proliferation, promotes the secretion of MMPs from stromal cells, and provides necessary nutrients for new blood vessels. Therefore, MMP-9 and VEGF play important roles in the occurrence and development of PHC. The present study showed that the concentrations of MMP-9 and VEGF in serum were significantly reduced at year 1 and 2 after PEI treatment compared with those before PEI. However, the levels of MMP-9 and VEGF were increased at year 3 after PEI, reaching a level higher than those at year 2. The reduced levels of MMP-9 and VEGF may be due to the dehydration and necrosis of tumor cells after PEI, while the increased levels of MMP-9 and VEGF indicate that angiogenesis around the tumor may lead to recurrence. Therefore, changes in serum concentrations of MMP-9 and VEGF can be used as a good indicator for the evaluation of PEI effectiveness. In the present study, ultrasonography during follow-ups showed significant necrosis of tumors without obvious blood flow.
However, it is still controversial that MMP-9 and VEGF play important roles in the growth, invasion and recurrence of PHC. Studies show that MMP-9 and VEGF expression in tumor tissues is related to PHC recurrence, with higher MMP-9 and VEGF expression corresponding to easier recurrence and metastasis of PHC [11,12]. By contrast, other studies indicate that the expression of MMP-9 and VEGF is not related to PHC prognosis [13,14]. A research paper suggests that MMP-9 is closely related to recurrence, and can be used as an indicator for the prediction of prognosis [15]. Immunohistochemical data show that the positive rate of VEGF in PHC accompanied by distal metastasis is 91%, which can be used as an important indicator to monitor tumor metastasis [16]. In the present study, different BCLC staging, Child grading, Kps scoring and vascular invasion influenced the effect of different MMP-9 and VEGF concentrations on prognosis. However, age, AFP contents, tumor diameter and hepatitis type failed to influence the effect of different MMP-9 and VEGF concentrations on prognosis. These observations indicate that changes in serum concentrations of MMP-9 and VEGF under different factors have important effect on prognosis. Elevated serum concentrations of MMP-9 and VEGF usually predict bad prognosis, so the determination of serum concentrations of MMP-9 and VEGF before surgery can promote the clinical benefits of these molecular markers. During follow-ups, angiogenesis observed around the tumor after PEI usually indicates progression of the disease. In the present study, progression-free survival curves were plotted according to Kaplan-Meier analysis. The data show that higher concentrations of MMP-9 and VEGF correspond to poorer treatment effect of PEI, indicating that serum concentrations of MMP-9 and VEGF after PEI have significant effect on the prognosis. In conclusion, PEI treatment has good long-term effect on PHC, significantly prolonging the survival rates of PHC patients. The levels of MMP-9 and VEGF are closely related to PHC growth. Therefore, MMP-9 and VEGF might potentially be used as important markers for the evaluation of prognosis after PEI treatment. Of note, inhibition of MMP-9 or VEGF expression in tumors might be of important clinical significance in promoting long-term prognosis.
Acknowledgements
This work was supported by Dr. Jianjun Zheng of The Second Hospital of Ningbo City.
Disclosure of conflict of interest
None.
References
- 1.Wang K, Liu G, Li J, Yan Z, Xia Y, Wan X, Ji Y, Lau WY, Wu M, Shen F. Early intrahepatic recurrence of hepatocellular carcinoma after hepatectomy treated with re-hepatectomy, ablation or chemoembolization: a prospective cohort study. Eur J Surg Oncol. 2015;41:236–242. doi: 10.1016/j.ejso.2014.11.002. [DOI] [PubMed] [Google Scholar]
- 2.Arii S, Yamaoka Y, Futagawa S, Inoue K, Kobayashi K, Kojiro M, Makuuchi M, Nakamura Y, Okita K, Yamada R. Results of surgical and nonsurgical treatment for small-sized hepatocellular carcinomas: a retrospective and nationwide survey in Japan. The Liver Cancer Study Group of Japan. Hepatology. 2000;32:1224–1229. doi: 10.1053/jhep.2000.20456. [DOI] [PubMed] [Google Scholar]
- 3.Guo J, Yang J, Wu M, Chen H, Li B. The significance of percutaneous ethanol injection guided by ultrasound in the treatment of liver cancer (with 2000 case report) Chinese Journal of Practical Surgery. 2001;21:494–495. [Google Scholar]
- 4.Weis S, Franke A, Berg T, Mossner J, Fleig WE, Schoppmeyer K. Percutaneous ethanol injection or percutaneous acetic acid injection for early hepatocellular carcinoma. Cochrane Database Syst Rev. 2015;1:CD006745. doi: 10.1002/14651858.CD006745.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Romero Gutierrez M, Ruano Diaz L, Munoz Lopez D, Artaza Varasa T, Gonzalez de Frutos C, Sanchez Ruano JJ, de la Cruz Perez G, Gomez Rodriguez R. Percutaneous ablation of hepatocellular carcinoma in older patients in clinical practice. Gastroenterol Hepatol. 2015;38:54–61. doi: 10.1016/j.gastrohep.2014.11.002. [DOI] [PubMed] [Google Scholar]
- 6.Pang RW, Joh JW, Johnson PJ, Monden M, Pawlik TM, Poon RT. Biology of hepatocellular carcinoma. Ann Surg Oncol. 2008;15:962–971. doi: 10.1245/s10434-007-9730-z. [DOI] [PubMed] [Google Scholar]
- 7.Kim A, Im M, Yim NH, Ma JY. Reduction of metastatic and angiogenic potency of malignant cancer by Eupatorium fortunei via suppression of MMP-9 activity and VEGF production. Sci Rep. 2014;4:6994. doi: 10.1038/srep06994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wu Y. The quantitative analysis of the treatment of liver cancer with percutaneous ethanol injection guided by ultrasound. Chinese And Foreign Medical Research. 2013;11:55–56. [Google Scholar]
- 9.Nakai M, Sato M, Yamada K, Ishii S, Minamiguchi H, Kimura M, Kishi K, Terada M, Kawai N. Percutaneous hot ethanol injection therapy (PHEIT) for hepatocellular carcinoma. Gan To Kagaku Ryoho. 2001;28:1633–1637. [PubMed] [Google Scholar]
- 10.Lin X, Lin L, Wu L, Xue E, He Y, Gao S. Transrectal ultrasound with head scanning probe in diagnosing rectal tumors. Chinese Journal of Medical Ultrasound. 2008;5:53–60. [Google Scholar]
- 11.Chao Y, Li CP, Chau GY, Chen CP, King KL, Lui WY, Yen SH, Chang FY, Chan WK, Lee SD. Prognostic significance of vascular endothelial growth factor, basic fibroblast growth factor, and angiogenin in patients with resectable hepatocellular carcinoma after surgery. Ann Surg Oncol. 2003;10:355–362. doi: 10.1245/aso.2003.10.002. [DOI] [PubMed] [Google Scholar]
- 12.Sakamoto Y, Mafune K, Mori M, Shiraishi T, Imamura H, Mori M, Takayama T, Makuuchi M. Overexpression of MMP-9 correlates with growth of small hepatocellular carcinoma. Int J Oncol. 2000;17:237–243. doi: 10.3892/ijo.17.2.237. [DOI] [PubMed] [Google Scholar]
- 13.Maatta M, Soini Y, Liakka A, Autio-Harmainen H. Differential expression of matrix metalloproteinase (MMP)-2, MMP-9, and membrane type 1-MMP in hepatocellular and pancreatic adenocarcinoma: implications for tumor progression and clinical prognosis. Clin Cancer Res. 2000;6:2726–2734. [PubMed] [Google Scholar]
- 14.An FQ, Matsuda M, Fujii H, Matsumoto Y. Expression of vascular endothelial growth factor in surgical specimens of hepatocellular carcinoma. J Cancer Res Clin Oncol. 2000;126:153–160. doi: 10.1007/s004320050025. [DOI] [PubMed] [Google Scholar]
- 15.Peng L, Wang S, Zhang F, Tang R. Research into the relationship of primary hepatic carcinoma invasion and metastasis with matrix metalloproteinase-9 and vascular endothelial growth factor. Chinese Journal of Hepatobiliary Surgery. 2003;9:42–44. [Google Scholar]
- 16.Tsunedomi R, Iizuka N, Tamesa T, Sakamoto K, Hamaguchi T, Somura H, Yamada M, Oka M. Decreased ID2 promotes metastatic potentials of hepatocellular carcinoma by altering secretion of vascular endothelial growth factor. Clin Cancer Res. 2008;14:1025–1031. doi: 10.1158/1078-0432.CCR-07-1116. [DOI] [PubMed] [Google Scholar]


