Abstract
Objective: Schizophrenia is a mental disorder and characterized by abnormal social behavior and failure to recognize what is real. The current study was to explore the long-term effects of cognitive rehabilitation training on schizophrenia. Methods: Eighty six cases of hospitalized patients with schizophrenia were randomly divided into study group and control group. The relapse and employment (attending school) rates were used as indicators to assess the treatment effect. All patients were followed up by 2 years. Kaplan-Meier survival analysis was conducted with relapse and employment (attending school) rates. Results: The rates of relapse in the study group and the control group were 18% and 41%, and relapse free survival time was 22.22 months and 18.55 months; the rates of employment (attending school) were 64% and 43%, and not employment (attending school) time were 10.68 months and 15.74 months, respectively. There was significant difference between the two groups (P<0.05). Conclusions: We found that the cognitive rehabilitation training could significantly reduce schizophrenic relapse rate, prolong the time of patients without relapse, improve the employment (attending school) rate, and shorten the discharged time, which is a powerful treatment method to improve social competence in schizophrenia patients.
Keywords: Cognitive rehabilitation training, Kaplan-Meier survival analysis, long-term follow-up, schizophrenia, pharmacotherapy treatment, psychosocial function
Introduction
Schizophrenia is a mental disorder, which affects approximately 0.4%-1% of the population worldwide [1,2]. For many patients, schizophrenia is a lifelong disease and those with schizophrenia take themselves as having minimal competence, social value or self-efficacy [3,4]. Generally, schizophrenia is characterized by abnormal social behavior and cognitive impairment [5], including those in psychomotor speed, attention, memory, and executive functions, which are thought to underlie the severe functional disability associated with this illness [6-8]. Environmental and genetic factors are known to influence the risk of suffering from schizophrenia, however, the mechanistic basis for these gene-environment interactions remains unrevealed.
Current drug treatments of schizophrenia mainly rely on antagonism of D2 dopamine receptor by incorporating a spectrum of actions at other G-protein coupled receptors. Despite the advanced development in the pharmacotherapy for the illness, a substantial proportion of patients continue to be plagued by impairments in social and occupational functioning [9]. And 30% of schizophrenia patients experience persistent psychotic symptoms despite two or more adequate trials of antipsychotic treatment, which is defined as “treatment-resistant schizophrenia (TRS)” [10]. Moreover, unemployment, lack of reliable friends, and leisure activities are associated with low subjective quality of life in the patients, and treatment of schizophrenia patients has remained a persistent public health challenge. For this purpose, rehabilitation programs aimed at enhancing community functioning and quality of life are currently being developed [11,12].
Although the topic of cognitive remediation in schizophrenia received little attention until 2000s, it has been firmly established. The field developed as a result of the need to address that severe psychosocial impairments must contend with despite the widespread use of psychopharmacologic treatments [13]. Rehabilitative training such as social and vocational skills involve targeted interventions that aim to inspire participants to acquire important life skills, thereby reducing existing impairments in social and role functioning [13,14]. However, most previous studies focused on a particular dimension of psychosocial functioning or a very restricted number of cognitive measures. Few studies have reported the long-term outcome and ending impact of schizophrenia patients in life after cognitive rehabilitation training. In the current study, we aimed to explore whether the subjects receiving cognitive rehabilitation training would live a normal life over a two years follow-up period based on the relapse and employment (attending school) rates. We expected that our study would help to assess the long-term effect of cognitive rehabilitation training on the life quality of patients with schizophrenia.
Patients and methods
Patients
86 schizophrenia patients were enrolled in the current study since April 2007 to October 2011 in the People’s Hospital of Guangxi Zhuang Autonomous Region. Patients included should meet the criteria for schizophrenia according to CCMD-3 (Psychiatric branch of Chinese medical association) [15], 18 to 44 years old, with education background superior than middle school, and with disease course shorter than ten years (Table 1). Cases who received second generation antipsychotics and nootropic, had dementia, severe body disease and no cognitive disorder, were excluded from the study. The project was approved by the People’s Hospital of Guangxi Zhuang Autonomous Region. The ethics committee approved the relating screening, inspection, and data collection of the patients, and all subjects signed a written informed consent form. All works were undertaken following the provisions of the Declaration of Helsinki.
Table 1.
Demographic information of the cases enrolled in the present study
| Item | Group A | Group B | |
|---|---|---|---|
| Gender | Male | 22 | 25 |
| Female | 20 | 19 | |
| Age | 29.71±6.36 | 28.95±7.38 | |
| Education background | Junior high school | 24 | 27 |
| Above senior high school | 18 | 17 | |
| Domicile | Countryside | 34 | 33 |
| Town | 8 | 11 | |
| Psychopharmacologic treatments | Sulpiride | 23 | 27 |
| Perphenazine | 8 | 9 | |
| Chlorpromazine | 6 | 5 | |
| Thioridazine | 5 | 3 |
Grouping and treatment
Patients were randomly divided into two groups: control group (Group A, including 42) patients and cognitive rehabilitation training group (Group B, including 44 patients). There was no significant difference between the two groups in sex composition (P = 0.679), ages (P = 0.611), education background (P = 0.690), domicile (P = 0.506), and psychopharmacologic treatments (P = 0.820) (Table 1). The severity of schizophrenia of all patients were evaluated based on Positive and Negative Syndrome Scale (PANSS), Digit Span Test (DS), Verbal Fluency Test (VF), and Wisconsin Card Sorting Test (WCST). For WCST, numbers of response administered (Ra), categories completed (Cc), response corrected (Rc), response preservative errors (Rpe) were recorded.
For patients in Group A, only psychopharmacologic treatment was conducted: patients were treated with one type of the following first generation antipsychotics (FGA) based on their conditions and drug tolerance, including perphenazine, chlorpromazine, sulpiride, and thioridazine. For patients in Group B, an integrated therapy combined with psychopharmacologic treatment and cognitive rehabilitation training was set up. Detail items of the cognitive rehabilitation training were shown in Table 2. Data of patients who came up with severe side effects or turned to another type of antipsychotics was excluded from further analysis. Both groups were subjected to the treatment for three months and those who met the “healing” criteria (Table 3) [16] were followed up.
Table 2.
Detail items of the cognitive rehabilitation training
| Item | |
|---|---|
| Training of memory and attention | 1. Training of visual memory; 2. Training of digital memory; 3. Training of verbal memory; 4. Training of memory, including walking a maze, jigsaw, etc |
| Training of language expression and logic | 1. Information and language stimulation; 2. Graphic sequence reasoning, digital sequence reasoning, symbol reasoning, etc. |
| Training of execution | Setting a task for patients to describe how to complete |
| Training of coordination | Patients were asked to finish daily life all by themselves, and participate in the manual operation, collective activity, and competitive games |
| Training of cognitive rehabilitation | 30 min each time, two times each week, 12 weeks each treatment. The training began with visual then to abstract |
Table 3.
Assessing criteria of clinical outcomes
| Clinical outcome | Criteria |
|---|---|
| Healing | PANSS value reduced by more than 70% after the treatment |
| Relapse | PANSS value increased by more than 25% during the follow-up; significant suicide or hurting people tendency lasted for more than one week |
| Employment or attending school | Being employed or attending school for more than one month |
Evaluation of the treatment effect
The treatment effects of the two therapies were evaluated based on the difference of the tests mentioned above between the baseline and after the treatments. PANSS values were recorded every three months after the treatments. Moreover, relapse or employment (attending school) was taken as end events. Criteria of clinical outcomes of patients were shown in Table 3 [16,17].
Statistical analysis
All the data were expressed in the form of mean ± SD. T-test and Chi-square test were conducted. The Kaplan-Meier method was used to estimate survival curve, and survival differences were analyzed by the log-rank test. All the statistical analysis were conducted using SPSS version 16.0 (IBM, Armonk, NY, USA).
Results
Cognitive rehabilitation training significantly improved the performance in different tests
There was no significant difference in PANSS, DS, VF, and WCST performance between Group A and Group B before the treatment (Table 4). After three months being subjected to the two therapies, conditions of all the patients were improved, especial for patients receiving integrated therapy. However, patients in Group B showed significant improvement in all the tests (P<0.05) while those in Group A showed little improvement in DS, VF, and WCST test (Table 4).
Table 4.
Comparison of cognitive function between the two groups after the treatments
| Group A | Group B | ||
|---|---|---|---|
| PANSS | Baseline | 94.40±13.55 | 92.14±12.81 |
| 12 weeks treatment | 61.45±8.95* | 60.75±11.79* | |
| DS | Baseline | 4.36±1.34 | 4.55±1.07 |
| 12 weeks treatment | 4.55±1.63 | 6.64±1.46*,# | |
| VF | Baseline | 3.69±1.85 | 3.70±1.39 |
| 12 weeks treatment | 3.74±1.64 | 4.68±1.54*,# | |
| Ra | Baseline | 114.86±15.39 | 113.82±13.75 |
| 12 weeks treatment | 112.81±14.14 | 105.59±13.77*,# | |
| Cc | Baseline | 2.64±1.43 | 2.82±1.57 |
| 12 weeks treatment | 2.76±1.57 | 3.68±0.64*,# | |
| Rc | Baseline | 47.00±18.17 | 48.59±16.18 |
| 12 weeks treatment | 44.64±16.33 | 59.66±10.55*,# | |
| Rpe | Baseline | 21.50±9.30 | 20.18±8.16 |
| 12 weeks treatment | 19.67±6.71 | 16.05±5.95*,# |
Significantly different compared with baseline, P<0.05;
significantly different compared with Group A, P<0.05.
Cognitive rehabilitation training significantly improved the relapse rate, and employment (attending school) rate of schizophrenia patients
Relapse data of two patients in Group A and six patients in Group B was lost to follow up. 17 cases in Group A relapsed during the two years follow-up while only eight cases in Group B showed symptom of schizophrenia again. The relapse rates were 41% and 18% for Group A and Group B, respectively (P = 0.022) (Figure 1). The survival without relapse times for Group A and Group B were 18.6 months and 22.2 months, respectively and the median was 24 months for both groups.
Figure 1.
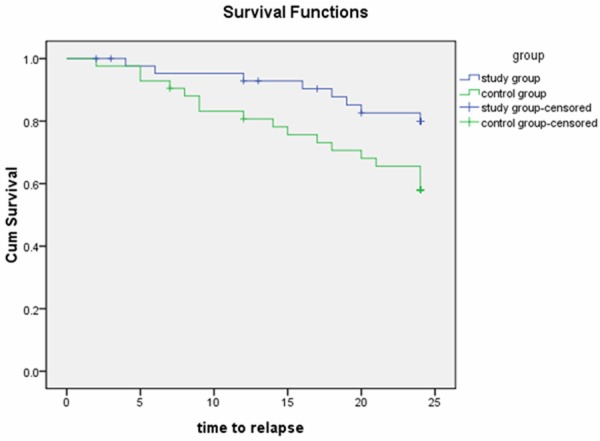
Survival curve of accumulative relapse rate.
Data of employment (attending school) rate of two cases were lost in Group A and three cases in Group B. 18 cases in Group A returned to work or school compared with 28 cases in Group B. The average times of non-employment (attending school) were 15.7 months for Group A and 10.7 for Group B and medians were 24 months and 4 months, respectively. The employment (attending school) rate of Group A was 43% compared with 64% for Group B (P = 0.03) (Figure 2).
Figure 2.
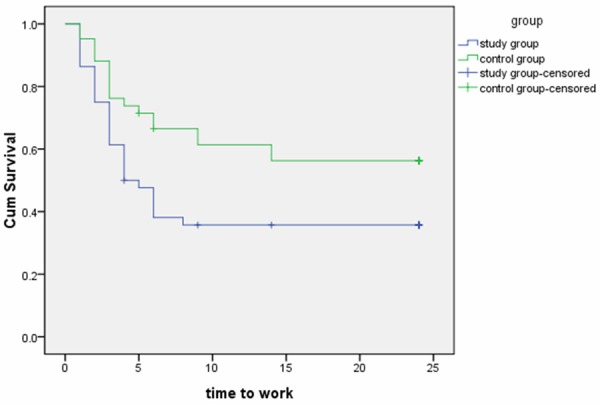
Survival curve of accumulative employment (attending school) rate.
Discussions
Schizophrenia is a multidimensional disorder involving a complex set of biological, psychological, and sociocultural factors that interact to undermine functioning throughout the course of the illness [18]. Despite the advanced development of drug treatments of schizophrenia, a substantial proportion of patients continue to be plagued by impairments in social and occupational functioning due to the relapse of the illness. And cognitive intervention, which are used to improve the life quality of schizophrenia patients, are gaining attention for their role in the social and occupational dysfunction that accompanies schizophrenia. The present study focused on the ending impact of schizophrenia patients participating in a rehabilitation program. Previous studies seldom focused on this part of cognitive rehabilitation training.
Our results revealed that after the cognitive rehabilitation training, patients in Group B showed significant improvement in PNASS, DS, VF, and WCST tests while patients in Group A just got improved in PNASS test (Table 3). The data was indicative of the treatment effect of cognitive rehabilitation training on attention, memory, and language fluency in schizophrenia patients. Moreover, in WCST test, the number of Rc increased dramatically, which showed the improvement of error correcting capability in schizophrenia patients; and the numbers of Ra and Cc were significantly different between the two groups after the treatment and between before and after training in Group B, these indicators represented the improvement of psychomotor in schizophrenia patients (Table 3).
Cognitive functions play different roles in psychosocial functioning improvement [19], and training of cognitive function would make important impact on human organs through environmental factors [20-22]. Bell et al [23] found that the cognitive rehabilitation training could improve the social competence of schizophrenia patients by increasing the employment (attending school) rate. Similar pattern was also observed in the present study: patients with cognitive rehabilitation training had a dramatically higher employment (attending school) rate and lower relapse rate than those in control group (Figures 1 and 2). Moreover, the relapse free survival time of patients in Group B was also longer during the training program. The visual memory and sustained attention enhancement during the program could reinforce improvement in the community functioning dimensions, which was more effective even than career training. McGurk and Mueser [24] indicated that dramatic superiority of cognitive rehabilitation training over career training would be noticed after three to four years.
In conclusion, it was found that the cognitive rehabilitation training could significantly reduce schizophrenic relapse rate, prolong the time of patients without relapse, and improve the employment (attending school) rate. The results showed the powerful potential of cognitive rehabilitation training on the improvement of social competence in schizophrenia patients. While the results of the current study are promising, our findings may not generalize to other ethnic groups. And the study needs to be replicated with larger samples over a longer period.
Acknowledgements
This study was supported by the Medical and Health Research Program of Health and Family Planning Commission of Guangxi Zhuang Autonomous Region (No. Z2007162 and Z2014631) and Scientific Research and Technology Development Program of Qingxiu District, Naning, Guangxi (No. 2012S03).
Disclosure of conflict of interest
None.
References
- 1.Zhang XY, Al Jurdi RK, Zoghbi AW, Chen da C, Xiu MH, Tan YL, Yang FD, Kosten TR. Prevalence, demographic and clinical correlates of suicide attempts in Chinese medicated chronic inpatients with schizophrenia. J Psychiatr Res. 2013;47:1370–1375. doi: 10.1016/j.jpsychires.2013.05.024. [DOI] [PubMed] [Google Scholar]
- 2.Skokou M, Gourzis P. Demographic features and premorbid personality disorder traits in relation to age of onset and sex in paranoid schizophrenia. Psychiatry Res. 2014;215:554–559. doi: 10.1016/j.psychres.2014.01.018. [DOI] [PubMed] [Google Scholar]
- 3.Beck EM, Cavelti M, Wirtz M, Kossowsky J, Vauth R. How do socio-demographic and clinical factors interact with adherence attitude profiles in schizophrenia? A cluster-analytical approach. Psychiatry Res. 2011;187:55–61. doi: 10.1016/j.psychres.2010.10.012. [DOI] [PubMed] [Google Scholar]
- 4.Gaudiano BA, Miller IW, Herbert JD. The treatment of psychotic major depression: is there a role for adjunctive psychotherapy? Psychother Psychosom. 2007;76:271–277. doi: 10.1159/000104703. [DOI] [PubMed] [Google Scholar]
- 5.Rosti-Otajarvi E, Mantynen A, Koivisto K, Huhtala H, Hamalainen P. Neuropsychological rehabilitation has beneficial effects on perceived cognitive deficits in multiple sclerosis during nine-month follow-up. J Neurol Sci. 2013;334:154–160. doi: 10.1016/j.jns.2013.08.017. [DOI] [PubMed] [Google Scholar]
- 6.Green MF, Kern RS, Braff DL, Mintz J. Neurocognitive deficits and functional outcome in schizophrenia: are we measuring the “right stuff”? Schizophr Bull. 2000;26:119–136. doi: 10.1093/oxfordjournals.schbul.a033430. [DOI] [PubMed] [Google Scholar]
- 7.Fervaha G, Foussias G, Agid O, Remington G. Motivational and neurocognitive deficits are central to the prediction of longitudinal functional outcome in schizophrenia. Acta Psychiatr Scand. 2014;130:290–299. doi: 10.1111/acps.12289. [DOI] [PubMed] [Google Scholar]
- 8.Cervellione KL, Burdick KE, Cottone JG, Rhinewine JP, Kumra S. Neurocognitive deficits in adolescents with schizophrenia: longitudinal stability and predictive utility for short-term functional outcome. J Am Acad Child Adolesc Psychiatry. 2007;46:867–878. doi: 10.1097/chi.0b013e318054678d. [DOI] [PubMed] [Google Scholar]
- 9.Miyamoto S, Miyake N, Jarskog LF, Fleischhacker WW, Lieberman JA. Pharmacological treatment of schizophrenia: a critical review of the pharmacology and clinical effects of current and future therapeutic agents. Mol Psychiatry. 2012;17:1206–1227. doi: 10.1038/mp.2012.47. [DOI] [PubMed] [Google Scholar]
- 10.Lieberman JA. Pathophysiologic mechanisms in the pathogenesis and clinical course of schizophrenia. J Clin Psychiatry. 1999;60(Suppl 12):9–12. [PubMed] [Google Scholar]
- 11.Cordier R, Newton Scanlan J. Cognitive remediation has global cognitive and functional benefits for people with schizophrenia when combined with psychiatric rehabilitation. Aust Occup Ther J. 2012;59:334–335. doi: 10.1111/j.1440-1630.2012.01022.x. [DOI] [PubMed] [Google Scholar]
- 12.Wexler BE, Bell MD. Cognitive remediation and vocational rehabilitation for schizophrenia. Schizophr Bull. 2005;31:931–941. doi: 10.1093/schbul/sbi038. [DOI] [PubMed] [Google Scholar]
- 13.Bartels SJ, Pratt SI. Psychosocial rehabilitation and quality of life for older adults with serious mental illness: recent findings and future research directions. Curr Opin Psychiatry. 2009;22:381–385. doi: 10.1097/YCO.0b013e32832c9234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kern RS, Glynn SM, Horan WP, Marder SR. Psychosocial treatments to promote functional recovery in schizophrenia. Schizophr Bull. 2009;35:347–361. doi: 10.1093/schbul/sbn177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gan JL, Duan HF, Yang JM, Shi ZJ, Zhang DW, Jiang ZK, Gao CY, Wang ZJ. [Proton magnetic resonance spectroscopy of prefrontal lobe and thalamus in schizophrenics: correlation with clinical characteristics] . Zhonghua Yi Xue Za Zhi. 2011;91:3034–3039. [PubMed] [Google Scholar]
- 16.Zhou HZ WZ. Clinical efficacy of paliperidone in treatment of first episode schizophrenia. J Pract Med. 2012;28:3986–3988. [Google Scholar]
- 17.Csernansky JG, Mahmoud R, Brenner R Risperidone-USA-79 Study Group. A comparison of risperidone and haloperidol for the prevention of relapse in patients with schizophrenia. N Engl J Med. 2002;346:16–22. doi: 10.1056/NEJMoa002028. [DOI] [PubMed] [Google Scholar]
- 18.Bellack AS, Green MF, Cook JA, Fenton W, Harvey PD, Heaton RK, Laughren T, Leon AC, Mayo DJ, Patrick DL, Patterson TL, Rose A, Stover E, Wykes T. Assessment of community functioning in people with schizophrenia and other severe mental illnesses: a white paper based on an NIMH-sponsored workshop. Schizophr Bull. 2007;33:805–822. doi: 10.1093/schbul/sbl035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Poletti S, Anselmetti S, Bechi M, Ermoli E, Bosia M, Smeraldi E, Cavallaro R. Computer-aided neurocognitive remediation in schizophrenia: durability of rehabilitation outcomes in a follow-up study. Neuropsychol Rehabil. 2010;20:659–674. doi: 10.1080/09602011003683158. [DOI] [PubMed] [Google Scholar]
- 20.Zhao WL, Yin XB. Comparable study on cognition impairment in schizophrenia patients. Frontier in Medicine. 2013;3:11–12. [Google Scholar]
- 21.Lee WK. Effectiveness of computerized cognitive rehabilitation training on symptomatological, neuropsychological and work function in patients with schizophrenia. Asia Pac Psychiatry. 2013;5:90–100. doi: 10.1111/appy.12070. [DOI] [PubMed] [Google Scholar]
- 22.Hogarty GE, Greenwald DP, Eack SM. Durability and mechanism of effects of cognitive enhancement therapy. Psychiatr Serv. 2006;57:1751–1757. doi: 10.1176/ps.2006.57.12.1751. [DOI] [PubMed] [Google Scholar]
- 23.Bell MD, Choi KH, Dyer C, Wexler BE. Benefits of cognitive remediation and supported employment for schizophrenia patients with poor community functioning. Psychiatr Serv. 2014;65:469–475. doi: 10.1176/appi.ps.201200505. [DOI] [PubMed] [Google Scholar]
- 24.McGurk SR, Mueser KT. Cognitive and clinical predictors of work outcomes in clients with schizophrenia receiving supported employment services: 4-year follow-up. Adm Policy Ment Health. 2006;33:598–606. doi: 10.1007/s10488-006-0070-2. [DOI] [PubMed] [Google Scholar]


