Abstract
Background: The importance of postoperative gastrointestinal function recovery is being increasingly recognized. In this multi-center randomized controlled study, we evaluated the efficacy and safety of Evodia hot compress (ECS) plus electro-acupuncture (EA) for patients who developed postoperative gastrointestinal tract dysfunction after abdominal surgery. Methods: 1009 patients who developed postoperative gastrointestinal tract dysfunction after abdominal surgery were enrolled. All patients received conventional therapies for 7 days from the 1st postoperative day and were randomly assigned to receive coarse salt hot compress, Evodia hot compress or Evodia hot compress plus electro-acupuncture twice a day for 7 days. Results: The mean time to first flatus and to first bowel sounds was comparable among the four groups (P>0.05). The control group had a significantly shorter time to defecation compared with patients receiving coarse salt hot compress, Evodia hot compress or Evodia hot compress plus electro-acupuncture (P<0.05). In patients undergoing open hepatectomy, the time to first defecation was the shortest in those who received Evodia hot compress plus electro-acupuncture (89.3±25.5 h), which was significantly different from that of controls(134±31.1 h), those who received coarse salt hot compress (106.7±36.4 h) and those who received Evodia hot compress (109.9±42.1 h) (P<0.05) in patients undergoingopen cholecystectomy, the time to first defecation was the shortest in those who received Evodia hot compress (73.1± 24.7), which was significantly different from that of controls (77.8±29.7), those who received coarse salt hot compress 90.5±30.2) and those who received Evodia hot compress plus electro-acupunctur (83.9±34.0). Conclusion: Evodia hot compress plus electro-acupuncture confers benefit in postoperative recovery of gastrointestinal function of patients who have undergone abdominal surgery and it is overall safe to use. Trial registration: Chinese Clinical Trial RegistryChiCTR-TRC-09000527.
Keywords: Evodia hot compress, electro-acupuncture, abdominal surgery, gastrointestinal function
Introduction
Postoperative gastrointestinal tract dysfunction (PGID), which is multi-factorial in onset, is very common and is associated with increased patient suffering [1,2]. The importance of postoperative gastrointestinal function recovery is being increasingly recognized. Strategies such as good preoperative preparation, regional local anesthesia, limited surgical incision, early mobilization and oral diet have become the main measures to improve the recovery of gastrointestinal function [3-5]. Although a variety of strategies reduce PGID, including multimodal postoperative rehabilitation and minimally invasive surgery, none of these measures have been completely successful in shortening the duration of PGID.
Hot compress has been widely applied for PGID in clinical practice. Previous experience from clinical observations suggested that Chinese herbal hot compress [6] and electro-acupuncture are effective in promoting the recovery of gastrointestinal function after gastrointestinal surgery [7]. Our retrospective study of Evodia hot compress for 153 patients undergoing abdominal surgery [6] showed that Evodia hot compress significantly promoted the recovery of flatus and borborygmus. A randomized study demonstrated that early application of Evodia hot compress and acupuncture effectively promoted gastrointestinal function, and also shortened the recovery of intestinal peristalsis and the time to first flatus and defecation [8,9].
Acupuncture has been used in China for thousands of years and is widely accepted in China and is being increasingly used in other parts of the world. It is cost-effective and minimally invasive with a very low incidence of side effects and it is well known as an effective therapeutic regimen of postoperative pain, gastrointestinal motility disorders and vomiting [10,11]. Although prior studies have investigated the effects of acupuncture on gastrointestinal motility in humans, its role in treating PGID is less clear, data and literature are scarce [12-14]. Several animal studies have revealed that acupuncture exerts effect on gastrointestinal function through the sympathetic and parasympathetic efferent pathways [15-17]. In a randomized controlled study of 40 patients, electro-acupuncture significantly reduced the time to the first anal exhaust, the first defecation and the first solid food intake [18]. These clinical studies, however, have a relatively small sample size.
In this multi-center randomized controlled study, we evaluated the efficacy and safety of Evodia hot compress plus electro-acupuncture for patients who developed PGID following abdominal surgery.
Patients and methods
Patient population and study design
All the authors had access to the study data and had reviewed and approved the final manuscript. This multi-center randomized controlled study enrolled eligible patients who had received abdominal surgery between October 2009 and December 2011 at the participating centers. Patients were included in the study 1) if they were aged between 18 and 75 years; 2) if they had undergone moderate abdominal surgery (in according with the Operation Grading Management Guideline of the Ministry of Health of the People’s Republic of China) whose duration was between 1 and 4 hours with anesthesia lasting 1.5 to 5 hours; 3) if they developed abdominal pain, constipation and other symptoms of gastrointestinal dysfunction post surgery; 4) if they required a fasting diet post surgery. Patients were excluded 1) if they were allergic to Evodia and acupuncture needles; 2) if they had severe malnutrition with serum albumin <21 g/L or prealbumin <0.10 g/L; 3) if their intraoperative estimated blood loss was more than 1000 mL; 4) if they had severe cardiovascular, liver, kidney, brain or lung disease or mental illness; 5) if they had severe postoperative bowel adhesions requiring a second abdominal surgery; 6) if they had cachexia due to a malignancy; 7) if they had breast cancer requiring extended radical mastectomy.
The study was approved by the local ethical committees or institutional review boards at each participating institution and all patients or their legally acceptable surrogates provided written informed consent. The study has been registered in the Chinese Clinical Trial Registry (http://www.chictr.org/) (No. ChiCTR-TRC09000527).
Randomization procedures
Randomization procedures were conducted at the National Center for Design Measurement and Evaluation in Clinical Research of Guangzhou University of Chinese Medicine using a computer-generated randomization list with PROC PLAN (SAS 9.2; the SAS Institute, Cary, NC, USA). The randomization was coded numerically with 1 for the control group, 2 for the coarse salt hot compress group, 3 for the Evodia hot compress group, and 4 for the Evodia hot compress plus electro-acupuncture group. The list was delivered via telephone, facsimile or text message to each participating site using the validated web-based randomization system, the Central Randomization Allocation System for Clinical Trials. Data management and data entry were completed at the web-based data management system with a double cross-checking approach. Participating centers were pre-added in the system. Common users of the system at each center were granted corresponding permission and user-names in advance. They accessed the system, input patient demographic data, and selected items according to the inclusion/exclusion criteria. The system then automatically decided whether a patient was eligible or not for participating in the study.
Study supervision
The steering committee developed the trial protocol and supervised the scientific conduct of the study. The steering committee had full access to the trial data, approved the statistical analysis plan, and assumed complete responsibility for the final interpretation of the results. All study committees are listed in the Appendix. The steering committee wrote the manuscript, and was responsible for decisions with regard to publication. All the authors vouch for the veracity and completeness of the data and analyses.
Study intervention
Eligible patients were randomly assigned to the control group, the coarse salt hot compress group (CS), the Evodia hot compress group or the Evodia hot compress plus electro-acupuncture group (ECS & EA). All patients received conventional therapies including antibiotics therapy for 7 days from the 1st postoperative day. The standard procedures of Evodia and coarse salt hot compress and electro-acupuncture are listed in the supplementary Materials and Methods. In the coarse salt hot compress group, patients received coarse salt (Guangzhou Salt Industry Corp., Guangzhou, China) hot compress twice a day for 7 days. In the Evodia hot compress group, patients received Evodia and coarse salt hot compress twice a day for 7 days. In the Evodia hot compress plus electro-acupuncture group, patients received Evodia and coarse salt hot compress and electro-acupuncture twice a day for 7 days. The hot compress therapy with coarse salt and/or Evodia was performed by trained nurses according to a predetermined standard operating procedure. Electro-acupuncture was performed by qualified operators.
Patient evaluation
The primary outcome of the study was time to first defecation, flatus and borborygmus after the surgery. Time to first defecation, flatus and bowel sounds was from the time when the surgery was completed until the first observed passage of stool, the first observed passing of flatus, and the first observed bowel sounds, respectively. Patients were monitored daily from the 1st postoperative day to the 7th postoperative day for defecation, flatus and borborygmus. Patient compliance was also evaluated.
Safety evaluation
Vital signs and adverse events were monitored throughout the study. Safety assessments were based mainly on the occurrence, frequency, and severity of adverse events, and were also based on comprehensive indexes, including physical examination, electrocardiography, and routine laboratory investigations. For all adverse events, where necessary, patients were withdrawn from the study.
Statistical analysis
A sample size of 1008 was chosen to achieve at least a statistical power of 90 percent to detect a difference in time to first defecation, flatus or borborygmus, with an assumed two-sided type I error of 0.05 and a dropout rate of 15 percent. Data analysis was performed with PASW 18.0 software. The statistical analyses were pre-specified and performed on an intention-to-treat basis. The ITT analysis will include all patients who are randomized, and the per-protocol (PP) analysis included patients who completed the study and did not have major protocol violations. All analyses were based on the ITT population, and the result of the ITT analysis was compared with the PP analysis to assess the sensitivity. All missing data were analyzed using the last observation carried forward (LOCF) imputation method. Changes from baseline in outcome measurement among the four groups were analyzed using ANOVA or Kruskal-Wallis test when appropriate. The least significant difference (LSD) methods for multi-comparisons were performed if the tests were statistically significant. Safety analysis was analyzed mainly using descriptive statistics. All statistical tests were two-tailed with a significance level set at α=0.05.
Results
Patient demographic and baseline characteristics
The study flowchart is shown in Figure 1. Between October 2009 to December 2011, 1485 patients underwent abdominal surgery; of these, 456 patients were excluded because they failed to meet the eligibility criteria and 1029 patients were eligible for the study. Twenty patients were excluded due to age, randomized number mistaken and selection and exclusion criteria, and finally 1009 patients were randomized to treatment and had a baseline assessment and at least one post-baseline assessment and constituted the full analysis set. One hundred and fourteen patients were lost to follow-up, including 26 patients who withdrew from the study, 58 patients who did not comply with the treatment protocol, 31 patients who took gastro-kinetic agents, and 6 patients who were wrongly assigned, and yet 7 patients of the all 121 patients who were rejected due to at least two of the above reasons. As a result, 895 patients constituted the per-protocol analysis set. Patient demographic and baseline characteristics are shown in Table 1. The four groups of patients were comparable in demographic and baseline characteristics.
Figure 1.
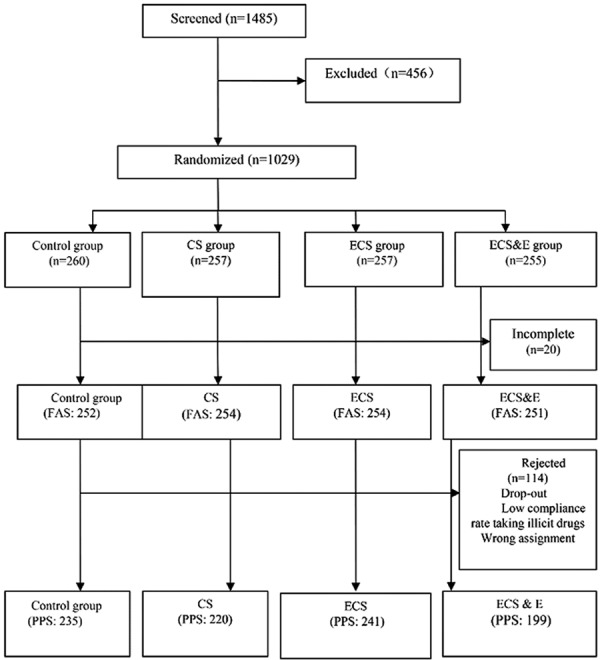
The study flowchart. ECS: Evodia hot compress; EA: Electro-acupuncture; ECS & EA: Evodia hot compress plus electro-acupuncture group.
Table 1.
Patient demographic and baseline characteristics
| Variables | All patients | Group A | Group B | Group C | Group D | P |
|---|---|---|---|---|---|---|
|
| ||||||
| n=1009 | n=252 | n=254 | n=252 | n=251 | ||
| Age Mean (SD) year | 53.7 (13.3) | 53.5 (12.8) | 54.3 (13.1) | 53.7 (14.1) | 53.2 (13.1) | 0.811 |
| Male gender, n (%) | 508 (50.3) | 129 (51.2) | 127 (50.0) | 133 (52.8) | 119 (47.4) | 0.672 |
| History of abdominal surgery, n (%) | 1009 | 252 | 254 | 252 | 251 | |
| Yes | 182 (18.0) | 51 (20.2) | 45 (17.7) | 46 (18.3) | 40 (15.9) | 0.659 |
| Stool habits in previous 3 months, n (%) | 846 | 207 | 211 | 212 | 216 | |
| <1 time/d | 32 (3.8) | 10 (4.8) | 6 (2.8) | 6 (2.8) | 10 (4.6) | 0.854 |
| 1 time/d | 776 (91.7) | 188 (90.8) | 194 (91.9) | 198 (93.4) | 196 (90.8) | |
| >1 time/d | 38 (4.5) | 9 (4.2) | 11 (5.3) | 8 (3.8) | 10 (4.6) | |
| Stool characteristics in previous 3 months, n (%) | 996 | 247 | 254 | 249 | 246 | |
| Hard | 40 (4.0) | 6 (2.4) | 16 (6.3) | 9 (3.6) | 9 (3.7) | 0.553 |
| Rotten | 145 (14.6) | 40 (16.2) | 39 (15.4) | 35 (14.1) | 31 (12.6) | |
| Soft | 135 (13.6) | 40 (16.2) | 29 (11.4) | 35 (14.1) | 31 (12.6) | |
| Watery | 9 (0.9) | 3 (1.2) | 3 (1.2) | 2 (0.8) | 1 (0.4) | |
| Normal | 667 (67.0) | 158 (64.0) | 167 (65.7) | 168 (67.5) | 174 (70.7) | |
| Underlying disease, n (%) | 271 | 60 | 60 | 81 | 70 | 0.093 |
| Diabetes | 36 (13.3) | 8 (13.3) | 5 (8.3) | 11 (13.6) | 12 (17.1) | |
| Coronary heart disease | 11 (4.1) | 4 (6.7) | 2 (3.3) | 4 (4.9) | 1 (1.4) | |
| Chronic obstructive pulmonary disease | 2 (0.7) | 1 (1.7) | 0 (0.0) | 0 (0.0) | 1 (1.4) | |
| Hypertension | 97 (35.8) | 14 (23.3) | 22 (36.7) | 32 (39.5) | 29 (41.4) | |
| Others | 125 (46.1) | 33 (55.0) | 31 (51.7) | 34 (42.0) | 27 (38.6) | |
Group A, the control group; group B, the coarse salt hot compress group; group C, the Evodia hot compress group; group D, the Evodia hot compress + electro-acupuncture group. SD: standard deviation.
The primary outcomes
The primary outcome measures of the study are summarized in Table 2. The mean time to first flatus and to first bowel sounds was comparable among the four groups (P>0.05). The control group had a significantly shorter time to defecation (84.8±44.3 h) compared with patients in the coarse salt hot compress group (95.3±44.8 h), the Evodia hot compress group (87.0±42.4) or the Evodia hot compress plus electro-acupuncture group (87.2±41.3 h) (P<0.05).
Table 2.
The primary outcome measures in the intention to treat population
| Group A | Group B | Group C | Group D | P * | |
|---|---|---|---|---|---|
|
| |||||
| n=244 | n=248 | n=248 | n=247 | ||
| Time to first flatus, h | 0.179 | ||||
| Mean (SD) | 51.6 (29.6) | 56.0 (30.0) | 54.2 (27.1) | 52.5 (26.5) | |
| Range | 6.9-162.3 | 7.3-163.5 | 7.0-135.6 | 6.5-136.8 | |
| Time to first defecation, h | 0.033 | ||||
| Mean (SD) | 84.8 (44.3) | 95.3 (44.8) | 87.0 (42.4) | 87.2 (41.3) | |
| Range | 8.5-284.3 | 15.2-261.5 | 7.0-223.0 | 14.8-338.1 | |
| Time to first bowel sound, h | 0.344 | ||||
| Mean (SD) | 65.2 (42.9) | 65.4 (38.8) | 59.5 (31.8) | 58.5 (29.6) | |
| Range | 8.0-350.0 | 9.0-298.0 | 10.0-184.0 | 5.0-171.0 | |
Kruskal-Wallis H test.
Group A, the control group; group B, the coarse salt hot compress group; group C, the Evodia hot compress group; group D, the Evodia hot compress + electro-acupuncture group; SD: standard deviation.
Gastrointestinal function recovery according to types of surgery
We further analyzed the recovery of gastrointestinal function according to surgery types. In patients undergoing open hepatectomy, the time to first defecation was the shortest in those who received Evodia hot compress plus electro-acupuncture (89.3±25.5 h), which was significantly different that of controls (134.±31.1 h), those who received coarse salt hot compress (106.7±36.4 h) and those who received Evodia hot compress (109.9±42.1 h) (P<0.05) (Table 3). In patients undergoing open cholecystectomy, the time to first defecation was the shortest in those who received Evodia hot compress (73.1±24.7 h) followed by controls (77.8±29.7 h) while those who received coarse salt hot compress had the longest time to first defecation (90.5±30.2 h) (P<0.05). No significant difference was observed in other parameters with regards to surgery types.
Table 3.
Subgroup analysis of outcome measures in the intention to treat population according to surgery types
| Group A | Group B | Group C | Group D | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||
| N | Mean (SD) | N | Mean (SD) | N | Mean (SD) | N | Mean (SD) | P * | |
| Open hepatectomy | |||||||||
| Time to first flatus, h | 11 | 70.2 (32.1) | 20 | 66.0 (25.5) | 16 | 66.6 (29.6) | 19 | 60.3 (24.6) | 0.648 |
| Time to first defecation, h | 11 | 134 (31.1) | 20 | 106.7 (36.4) | 16 | 109.9 (42.1) | 19 | 89.3 (25.5) | 0.013 |
| Time to first bowel sound, h | 11 | 77.5 (27.2) | 20 | 73.4 (32.2) | 16 | 67.2 (39.5) | 19 | 61.2 (27.2) | 0.474 |
| Laparoscopic hepatectomy | |||||||||
| Time to first flatus, h | 3 | 42.4 (21.9) | 7 | 59.9 (39.9) | 3 | 35.2 (13.4) | 3 | 37.4 (14.3) | 0.931 |
| Time to first defecation, h | 3 | 74.8 (30.1) | 7 | 104.7 (55.4) | 3 | 50.9 (9.0) | 3 | 93.6 (19.6) | 0.402 |
| Time to first bowel sound, h | 3 | 66.3 (42.9) | 7 | 55.9 (23.8) | 3 | 44.3 (14.5) | 3 | 40.0 (18.0) | 0.609 |
| Open cholecystectomy | |||||||||
| Time to first flatus, h | 57 | 56.2 (21.1) | 51 | 60.4 (19.7) | 61 | 51.9 (19.8) | 60 | 55.1 (20.3) | 0.265 |
| Time to first defecation, h | 57 | 77.8 (29.7) | 51 | 90.5 (30.2) | 60 | 73.1 (24.7) | 60 | 83.9 (34.0) | 0.028 |
| Time to first bowel sound, h | 56 | 61.2 (38.9) | 50 | 63.5 (39.4) | 62 | 56.8 (26.8) | 60 | 60.7 (26.1) | 0.896 |
| Laparoscopic cholecystectomy | |||||||||
| Time to first flatus, h | 27 | 34.3 (28.5) | 26 | 28.2 (15.6) | 23 | 33.6 (20.1) | 32 | 22.8 (24.9) | 0.801 |
| Time to first defecation, h | 27 | 63.6 (39.6) | 26 | 62.5 (30.9) | 23 | 69.7 (39.9) | 32 | 57.1 (23.9) | 0.634 |
| Time to first bowel sound, h | 27 | 37.2 (20.7) | 26 | 37.8 (18.1) | 23 | 32.0 (16.4) | 32 | 35.9 (21.0) | 0.776 |
| Open gastrectomy | |||||||||
| Time to first flatus, h | 17 | 84.3 (35.6) | 18 | 84.9 (34.7) | 23 | 73.5 (25.8) | 19 | 84.5 (21.9) | 0.537 |
| Time to first defecation, h | 17 | 113.5 (27.8) | 18 | 122.3 (45.9) | 23 | 114.7 (45.4) | 19 | 121.6 (38.0) | 0.797 |
| Time to first bowel sound, h | 17 | 116.65 (70.8) | 18 | 94.7 (39.0) | 22 | 76.4 (28.4) | 19 | 80.6 (26.1) | 0.059 |
| Laparoscopic gastrectomy | |||||||||
| Time to first flatus, h | 3 | 46.7 (30.1) | 6 | 47.7 (22.5) | 1 | 21.5 (0.0) | 2 | 46.6 (2.5) | 0.589 |
| Time to first defecation, h | 3 | 67.1 (39.3) | 6 | 78.1 (36.9) | 1 | 43.5 (0.0) | 2 | 58.4 (14.3) | 0.597 |
| Time to first bowel sound, h | 3 | 41.0 (19.1) | 7 | 55.7 (35.9) | 1 | 43.0 (0.0) | 2 | 62.5 (9.2) | 0.581 |
| Open enterectomy | |||||||||
| Time to first flatus, h | 63 | 55.7 (27.4) | 70 | 62.0 (28.1) | 60 | 65.3 (26.4) | 58 | 59.9 (25.1) | 0.332 |
| Time to first defecation, h | 63 | 100.6 (49.3) | 69 | 111.0 (50.6) | 60 | 104.2 (40.4) | 57 | 101.7 (39.5) | 0.807 |
| Time to first bowel sound, h | 63 | 81.5 (40.7) | 69 | 74.5 (42.6) | 59 | 72.7 (32.3) | 58 | 71.7 (31.0) | 0.617 |
| Laparoscopic enterectomy | |||||||||
| Time to first flatus, h | 45 | 35.3 (17.6) | 27 | 40.9 (24.6) | 46 | 39.9 (24.7) | 34 | 40.7 (26.6) | 0.927 |
| Time to first defecation, h | 45 | 61.7 (25.5) | 27 | 77.4 (35.1) | 46 | 70.6 (45.8) | 33 | 80.6 (61.2) | 0.266 |
| Time to first bowel sound, h | 44 | 51.4 (28.7) | 27 | 56.4 (32.0) | 43 | 49.8 (31.6) | 34 | 49.2 (37.8) | 0.838 |
| Others | |||||||||
| Time to first flatus, h | 18 | 49.7 (41.2) | 23 | 52.9 (40.1) | 15 | 58.7 (29.2) | 20 | 38.4 (22.0) | 0.325 |
| Time to first defecation, h | 18 | 88.3 (69.3) | 23 | 87.4 (50.6) | 15 | 92.6 (44.4) | 20 | 82.0 (29.7) | 0.822 |
| Time to first bowel sound, h | 18 | 42.7 (29.4) | 22 | 59.9 (38.8) | 15 | 59.8 (30.4) | 19 | 43.6 (23.6) | 0.240 |
Kruskal-Wallis H test.
Group A, the control group; group B, the coarse salt hot compress group; group C, the Evodia hot compress group; group D, the Evodia hot compress + electro-acupuncture group. h: hour.
Safety
A total of 14 (1.38%) adverse events were reported in this study (Table 4). The number of adverse events was 5 (2.0%) in the control group, 4 (1.6%) in the coarse salt hot compress group, 1 (0.4%) in the Evodia hot compress group and 4 (1.6%) in the Evodia hot compress plus electro-acupuncture group. None of these adverse events were treatment-emergent.
Table 4.
Adverse events among the four groups
| Group | Adverse events (n, %) | P | |
|---|---|---|---|
|
| |||
| No | Yes | ||
| Control group | 246 (98.0) | 5 (2.0) | 0.369 |
| Coarse salt group | 247 (98.4) | 4 (1.6) | |
| Evodia hot compress | 256 (99.6) | 1 (0.4) | |
| Evodia hot compress plus electro-acupuncture | 246 (98.4) | 4 (1.6) | |
| ALL | 995 (98.6) | 14 (1.4) | |
Fisher’s exact test.
Conclusion and discussion
In One Hundred Medicine of ShenNong’s Canon of Herbs, Evodia was first recorded in the category of the maturescent fruits of Rutaceae Evodia [19]. Evodia is a widely used herbal medicine for its anti-inflammatory and analgesic activities in China and has recently been studied for gastrointestinal disorders. PGID remains a clinically significant disease hampering postoperative recovery of patients undergoing abdominal surgery. Our retrospective study [7] showed that Evodia hot compress significantly promoted the recovery of flatus and borborygmus, a finding that is further supported by other investigators who demonstrated that early application of Evodia hot compress and acupuncture effectively promoted gastrointestinal function, and shortened the recovery of intestinal peristalsis and the time to first flatus and defecation [8,9]. The current study assessed the efficacy and safety of Evodia hot compress plus electro-acupuncture for patients who developed PGID after abdominal surgery. The results showed no significant difference in time to first flatus or first bowel sound among the four groups. Furthermore, time to first defecation in patients who received conventional therapy only was significantly shorter than that of patients receiving coarse salt hot compress, Evodia hot compress or Evodia hot compress plus electro-acupuncture. The findings indicated that coarse salt or Evodia hot compress offers no significant benefit beyond that by conventional therapy. Our findings differ from other investigators who showed that Evodia hot compress was beneficial to the recovery of postoperative gastrointestinal function [20,21] and our earlier retrospective study [7].
Our subgroup analysis revealed that in patients undergoing open cholecystectomy, coarse salt or Evodia hot compress even markedly slowed the time to first defecation compared to conventional therapy alone. Only in patients undergoing open hepatectomy did we observe a significantly reduced time to first defecation in patients who received Evodia hot compress plus electro-acupuncture. However, we found no significant difference in time to first defecation between patients receiving Evodia hot compress and those receiving conventional therapy only, suggesting that this reduction in time to first defecation was likely due to the effect of electro-acupuncture. The Zusanli acupoint (stomach meridian ST-36), which was used in the current study, can conduct Qi movement and promote Fu-organ circulation and relieve pain [22]. Electro-acupuncture at Zusanli has been shown to accelerate gastrointestinal tract food transit and motility and is widely used in treating gastrointestinal diseases. Electro-acupuncture at Zusanli has the potential to influence gastric mucous substances and enteroendocrine cells that may modulate digestive functions [23]. These may partially explain the beneficial effect which we observed in patients undergoing open hepatectomy who received Evodia hot compress plus electro-acupuncture.
In conclusion, this multi-center randomized controlled study demonstrates that Evodia hot compress plus electro-acupuncture significant benefit in postoperative recovery of gastrointestinal function of patients who have undergone abdominal surgery and it is overall safe to use.
Acknowledgements
The authors would like to thank graduate students from Guangzhou University of Chinese Medicine for technical assistance. This work was supported by the Eleventh Five-year Project of State Ministry of Science and Technology (No. 2008BAI53B031). This study was supported by the funding of 11th Five-Year Plan Support Project by Ministry of Science and Technology, 2008BAI53B031.
Disclosure of conflict of interest
None.
References
- 1.Mythen MG. Postoperative gastrointestinal tract dysfunction: an overview of causes and management strategies. Cleve Clin J Med. 2009;76(Suppl 4):S66–71. doi: 10.3949/ccjm.76.s4.11. [DOI] [PubMed] [Google Scholar]
- 2.Mythen MG. Postoperative gastrointestinal tract dysfunction. Anesth Analg. 2005;100:196–204. doi: 10.1213/01.ANE.0000139376.45591.17. [DOI] [PubMed] [Google Scholar]
- 3.Bruns H, Rahbari NN, Loffler T, Diener MK, Seiler CM, Glanemann M, Butturini G, Schuhmacher C, Rossion I, Buchler MW, Junghans T, group DT. Perioperative management in distal pancreatectomy: results of a survey in 23 European participating centres of the DISPACT trial and a review of literature. Trials. 2009;10:58. doi: 10.1186/1745-6215-10-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.van Bree SH, Nemethova A, Cailotto C, Gomez-Pinilla PJ, Matteoli G, Boeckxstaens GE. New therapeutic strategies for postoperative ileus. Nat Rev Gastroenterol Hepatol. 2012;9:675–83. doi: 10.1038/nrgastro.2012.134. [DOI] [PubMed] [Google Scholar]
- 5.Gutierrez MC, Moore PG, Liu H. Goal-directed therapy in intraoperative fluid and hemodynamic management. J Biomed Res. 2013;27:357–365. doi: 10.7555/JBR.27.20120128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tian S. Prevention and Treatment of Gynecological Post-Operational Gastro-intestinal Function Disorder by Umbilical Compressing with Evodia Fruit in 21 Patients. China’s Naturopathy. 2004;12:31–2. [Google Scholar]
- 7.Ji W, Chen Z. Effect of Medicated Ironing with Fructus Evodiae on Promoting Gastrointestinal Function Recovery after Abdominal Operation. Journal of Guangzhou University of Traditional Chinese Medicine. 2010;27:225–7. [Google Scholar]
- 8.Liu X, Fu M, Luo X, Cui D. The effect of medicated ironing combined with electro-acupuncture on gastrointestinal function recovery undergoing abdomen operation. Journal of Practical Traditional Chinese Medicine. 2012;28:91–2. [Google Scholar]
- 9.Zheng C, Li J, Zeng Y. Nursing interventions of Chinese Medicine on intestinal function after colorectal section. Modern Nursing. 2007;13:196. [Google Scholar]
- 10.Yin J, Chen J. Gastrointestinal motility disorders and acupuncture. Auton Neurosci. 2010;157:31–7. doi: 10.1016/j.autneu.2010.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Takahashi T. Acupuncture for functional gastrointestinal disorders. J Gastroenterol. 2006;41:408–17. doi: 10.1007/s00535-006-1773-6. [DOI] [PubMed] [Google Scholar]
- 12.Lin X, Liang J, Ren J, Mu F, Zhang M, Chen JD. Electrical stimulation of acupuncture points enhances gastric myoelectrical activity in humans. Am J Gastroenterol. 1997;92:1527–30. [PubMed] [Google Scholar]
- 13.Meng ZQ, Garcia MK, Chiang JS, Peng HT, Shi YQ, Fu J, Liu LM, Liao ZX, Zhang Y, Bei WY, Thornton B, Palmer JL, McQuade J, Cohen L. Electro-acupuncture to prevent prolonged postoperative ileus: a randomized clinical trial. World J Gastroenterol. 2010;16:104–11. doi: 10.3748/wjg.v16.i1.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ng SS, Leung WW, Mak TW, Hon SS, Li JC, Wong CY, Tsoi KK, Lee JF. Electroacupuncture reduces duration of postoperative ileus after laparoscopic surgery for colorectal cancer. Gastroenterology. 2013;144:307–313. e1. doi: 10.1053/j.gastro.2012.10.050. [DOI] [PubMed] [Google Scholar]
- 15.Li Y, Tougas G, Chiverton SG, Hunt RH. The effect of acupuncture on gastrointestinal function and disorders. Am J Gastroenterol. 1992;87:1372–81. [PubMed] [Google Scholar]
- 16.Luo D, Liu S, Xie X, Hou X. Electroacupuncture at acupoint ST-36 promotes contractility of distal colon via a cholinergic pathway in conscious rats. Dig Dis Sci. 2008;53:689–93. doi: 10.1007/s10620-007-9929-7. [DOI] [PubMed] [Google Scholar]
- 17.Iwa M, Matsushima M, Nakade Y, Pappas TN, Fujimiya M, Takahashi T. Electroacupuncture at ST-36 accelerates colonic motility and transit in freely moving conscious rats. Am J Physiol Gastrointest Liver Physiol. 2006;290:G285–92. doi: 10.1152/ajpgi.00068.2005. [DOI] [PubMed] [Google Scholar]
- 18.Wen Q, Chen W, Li J, Zhao Y, Li N, Wang C. [Adhesive ileus treated by electroacupuncture at Zhigou (TE 6) and Zusanli (ST 36): a randomized controlled study] . Chinese Acupuncture & Moxibustion. 2012;32:961–5. [PubMed] [Google Scholar]
- 19.Xu L. One Hundred Medicine of Shen Nong’s Canon of Herbs. Qing Dynasty. 1644AD. [Google Scholar]
- 20.Li Y, Deng F, WANG S, Chen Z, Cao L, Xie M. Related literature analysis of the efficacy of evidia promoting the recovery of gastrointestinal function. Journal of Emergency in Traditional Chinese Medicine. 2012;21:195–6. [Google Scholar]
- 21.Tian S, Wu Z. The study on the prevention of gastrointestinal dysfunction of gynecology surgery of 21 cases with umbilicus compressing. China’s Naturopathy. 2004;12:31–2. [Google Scholar]
- 22.Nie B, Dang R, Chen E. The application of basic research on Zusanli. Shanghai Journal of Acupuncture and Moxibustion. 2007;26:38–40. [Google Scholar]
- 23.Lee CH, Kim DK, Yook TH, Sasaki M, Kitamura N. Effectiveness of electroacupuncture at Zusanli (ST36) on the immunohistochemical density of enteroendocrine cells related to gastrointestinal function. J Acupunct Meridian Stud. 2012;5:63–71. doi: 10.1016/j.jams.2012.01.002. [DOI] [PubMed] [Google Scholar]


