Abstract
Although syncope and nephrotic syndrome are frequently encountered independently in pediatric practice, syncope as the initial symptom for nephrotic syndrome is rarely observed in the pediatric age group. In this report, we present the case of 3-year-old boy with nephrotic syndrome who presented with a history of three episodes of syncope before admission. The syncope occurred after excessive fluid loss or inadequate intake of fluids and was relieved spontaneously. History taking revealed that the early morning palpebral edema, and laboratory tests showed decreased plasma protein levels and elevated serum lipid levels. Nephrotic syndrome was diagnosed, but could not be confirmed histopathologically because the patient’s parent refused consent for biopsy. The patient was managed with fluid expansion, correction of acidosis, and improvement of microcirculation to prevent recurrence of syncope, and glucocorticoids were administered to prevent disease progression.
Keywords: Syncope, nephrotic syndrome, plasma protein, blood lipid
Introduction
Nephrotic syndrome is the most common glomerular disease affecting children [1]. However, syncope as the initial presenting symptom has been rarely reported in patients with nephrotic syndrome. In a previous publication, a 7-year-old white girl was reported to have sudden loss of consciousness without any preceding symptoms due to massive pulmonary embolism, but no evidence of original disease excepting for nephrotic-range proteinuria [2]. We present here a case of a young boy who presented with a history of repeated syncope.
Case presentation
The patient was a 3-year-old boy admitted to our hospital for three episodes of syncope. The first episode occurred on an empty stomach; lasted for five minutes; and was accompanied by pallor of the lips and face, hyperhidrosis, and loss of consciousness. Thereafter, the patient had two similar episodes of syncope. Medical history and family history were negative. On admission, the patient’s vital signs were as follows: blood pressure, 90/60 mmHg; body temperature, 36.5°C; pulse rate, 86 beats per minute; and respiration rate, 24 breaths per minute. Physical examination did not show any abnormalities.
Diagnosis
The results of the laboratory tests were as follows: blood sugar level, 5.2 mmol/L; serum cholesterol level, 7.15 mmol/L; serum low-density lipoprotein level, 4.79 mmol/L; serum apolipoprotein B level, 1.43 g/L; serum apolipoprotein A level, 1.01 g/L; serum albumin level, <25 g/L. Further, no abnormalities were detected in the ultrasound examinations of heart and urinary system; electrocardiogram; ambulatory electroencephalogram; nuclear magnetic resonance imaging of the head; and head-up tilt test. Detailed history taking revealed that the patient had been having palpebral edema, especially in the morning, which was relieved after commencement of daily activities. No history of significant oliguria was noted. The pediatric nephrology department was consulted, and the diagnosis of nephrotic syndrome (primary/simple type) was made; however, pathological examination could not be performed to confirm the diagnosis since the parents refused consent for biopsy. The patient was administered metacortadracin (2 mg/(kg·d) as three divided does daily for 6-9 as well as rheomacrodex (10 g/d), salvianolate (50 mg/d), and dipyridamole (25 mg/d) to improve renal circulation. Written informed consent was obtained from the patient for publication of this Case report and any accompanying images (Figure 1).
Figure 1.
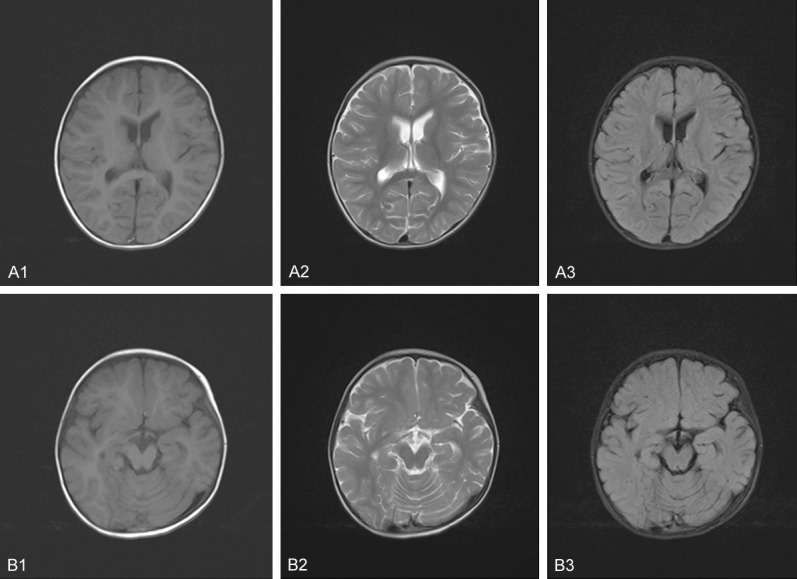
Magnetic Resonance Imaging of the brain. A1, B1: T1-weighted images; A2, B2: T2-weighted images; A3, B3: Flair images.
Discussion
Syncope is frequently the reason for admitting children to the emergency room [3,4]. In children, syncope can be classified as follows: syncope mediated by the autonomic nervous system; cardiac syncope; and cerebral syncope [5]. In this case, the evidence obtained did not point towards any of the abovementioned types of syncope or any systemic autoimmune disease.
The laboratory tests indicated elevated levels of urinary protein, serum cholesterol, serum low-density lipoprotein, serum apolipoprotein B, and serum apolipoprotein A and decreased levels of serum albumin. In addition, the patient had early morning palpebral edema and normal urine volume. Put together, these findings were consistent with the diagnosis of nephrotic syndrome. The behavioral disturbances have been found to be significantly associated with the frequency of relapse and low socioeconomic status [6]. To our knowledge, this is the first report of syncope manifesting as the first presenting symptom of nephrotic syndrome. Notably, the episodes of syncope in this case had occurred after inadequate intake or excessive loss of fluids; this could be potentially explained as follows. The urinary loss of blood protein leads to hypoproteinemia and severe edema, which significantly compromise the colloid osmotic pressure and effective blood volume [7,8]. Children have lower ability for compensatory changes in the cardiovascular system than adults; additionally, nausea, vomiting, diarrhea, infection, and reduced fluid intake can further worsen the reduction in effective blood volume in children, thereby leading to syncope.
The definite process of pathogenesis is yet to be determined. Nevertheless, management of the patient would involve steps for fluid expansion, correction of acidosis, and improvement of microcirculation, to restore the effective blood volume. In addition, glucocorticoids are recommended to prevent the progression of the disease [9].
Conclusion
We presented an unusual case of syncope presenting as the initial symptom of nephrotic syndrome. We believe that this case report highlights that repeated syncope can be a rare clinical presentation of nephrotic syndrome and that nephrotic syndrome should be considered in the differential diagnosis of syncope after inadequate intake or excessive loss of fluids. While the mechanism of the syncope in nephrotic syndrome still needs more researches.
Disclosure of conflict of interest
None.
Author contributions
Xue-mei Wu drafted the manuscript. Guang-liang Wang collected the infromations and helped to draft the manuscript. Jia-chun Feng revised the manuscript. All authors read and approved the final manuscript.
References
- 1.Yokoyama H, Maruyama S. [Overview of nephrotic syndrome in Japan] . Nihon Jinzo Gakkai Shi. 2014;56:460–463. [PubMed] [Google Scholar]
- 2.Ronco R, Catalan J, Salgado C, Vogel A. Syncope: a rare presentation of massive pulmonary embolism in a previously healthy girl. Pediatr Emerg Care. 2010;26:287–289. doi: 10.1097/PEC.0b013e3181d6da6b. [DOI] [PubMed] [Google Scholar]
- 3.Ganzeboom KS, Colman N, Reitsma JB, Shen WK, Wieling W. Prevalence and triggers of syncope in medical students. Am J Cardiol. 2003;91:1006–1008. A1008. doi: 10.1016/s0002-9149(03)00127-9. [DOI] [PubMed] [Google Scholar]
- 4.Serletis A, Rose S, Sheldon AG, Sheldon RS. Vasovagal syncope in medical students and their first-degree relatives. Eur Heart J. 2006;27:1965–1970. doi: 10.1093/eurheartj/ehl147. [DOI] [PubMed] [Google Scholar]
- 5.Mathias CJ, Deguchi K, Schatz I. Observations on recurrent syncope and presyncope in 641 patients. Lancet. 2001;357:348–353. doi: 10.1016/S0140-6736(00)03642-4. [DOI] [PubMed] [Google Scholar]
- 6.Guha P, De A, Ghosal M. Behavior profile of children with nephrotic syndrome. Indian J Psychiatry. 2009;51:122–126. doi: 10.4103/0019-5545.49452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang SJ, Tsau YK, Lu FL, Chen CH. Hypovolemia and hypovolemic shock in children with nephrotic syndrome. Acta Paediatr Taiwan. 2000;41:179–183. [PubMed] [Google Scholar]
- 8.Tabel Y, Mungan I, Karakurt C, Kocak G, Gungor S. Is edema in minimal change disease of childhood really hypovolemic? Int Urol Nephrol. 2008;40:757–761. doi: 10.1007/s11255-008-9344-9. [DOI] [PubMed] [Google Scholar]
- 9.Nishi S. [Guidelines for the treatment of nephrotic syndrome] . Nihon Jinzo Gakkai Shi. 2014;56:518–523. [PubMed] [Google Scholar]


