Abstract
Background
Contrast-balanced dichoptic experience with perceptual-learning tasks or simple games has been shown to improve visual acuity significantly in amblyopia. However, these tasks are intensive and repetitive, and up to 40% of unsupervised patients are noncompliant. We investigated the efficacy of a potentially more engaging movie method to provide contrast-balanced binocular experience via complementary dichoptic stimulation.
Methods
Eight amblyopic children 4–10 years of age were enrolled in a prospective cohort study to watch 3 dichoptic movies per week for 2 weeks on a passive 3D display. Dichoptic versions of 18 popular animated feature films were created. A patterned image mask of irregularly shaped blobs was multiplied with the movie images seen by the amblyopic eye and an inverse mask was multiplied with the images seen by the fellow eye. Fellow-eye contrast was initially set at a reduced level that allowed binocular vision and was then incremented by 10% at each visit. Best-corrected visual acuity, random dot stereoacuity, and interocular suppression were measured at baseline and 2 weeks.
Results
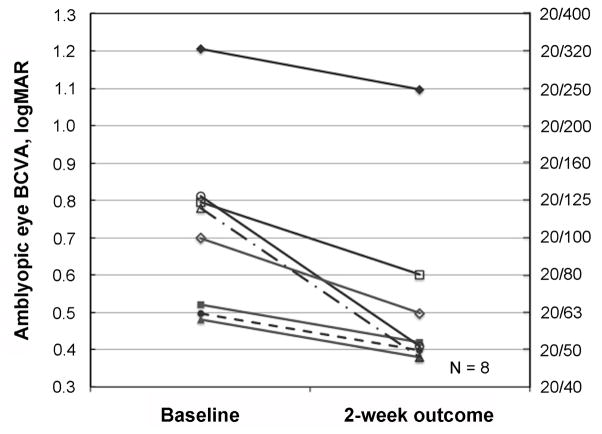
Mean amblyopic eye visual acuity (with standard error of the mean) improved from a logarithm of minimum angle of resolution of 0.72 ± 0.08 at baseline to 0.52 ± 0.09 (P = 0.003); that is, 2.0 lines of improvement at the 2-week outcome visit. No significant change in interocular suppression or stereoacuity was found.
Conclusions
Passive viewing of dichoptic feature films is feasible and could be a promising new treatment for childhood amblyopia. The maximum improvement that may be achieved by watching dichoptic movies remains to be determined. No known side effects are associated with this new treatment.
Amblyopia has been classically treated by patching of the fellow eye to force use of the amblyopic eye. However, recent years have seen a growing appreciation of the role of binocular dysfunction (suppression) in amblyopia that has motivated a reformulation of amblyopia treatment. Many amblyopic patients have a structurally intact binocular visual system that can be revealed by decreasing the fellow-eye contrast to reduce interocular suppression.1,2 Repeated experience with active dichoptic perceptual-learning tasks and dichoptic iPod/iPad game play has been shown to improve visual acuity significantly in amblyopic children and adults.3–15 Furthermore, visual acuity improvements gained through binocular iPad game play were maintained for at least 12 months.16
In general, the dichoptic tasks and games used in amblyopia treatment were designed to provide contrast-balanced binocular vision, with low contrast for the fellow eye and high contrast for the amblyopic eye. However, dichoptic perceptual learning tasks are intensive and repetitive, and the simple dichoptic games used to date have limited appeal; up to 40% of unsupervised patients are noncompliant with the assigned 16 hours of game play over 4 weeks.12,14,17 Thus, although the contrast-balanced binocular treatment approach has been shown to be efficacious in laboratory settings, noncompliance limits its effectiveness as a home-based treatment. We investigated the efficacy of a potentially more engaging contrast-balanced binocular experience for amblyopic children—viewing popular animated feature films with complementary dichoptic stimulation. If the feature film approach has efficacy similar to the contrast-balanced perceptual learning tasks and games in this proof-of-concept study, it may lead to home-based binocular amblyopia therapy with greater compliance.
Materials and Methods
This study was approved by the Institutional Review Board of University of Texas Southwestern Medical Center and conformed to all local laws and complied with regulations of the US Health Insurance Portability and Accountability Act of 1996. Written informed consent was obtained from all parents/guardians.
Eight amblyopic children (4–10 years) were referred by 2 pediatric ophthalmologists. To be eligible, children had to have a best-corrected visual acuity, expressed as the logarithm of the minimum angle of resolution (logMAR), of ≥0.5 logMAR in the amblyopic eye, ≤0.2 logMAR in the fellow eye, and an interocular differences of ≥0.2 logMAR. Strabismic children were eligible to participate only if misalignment of the visual axes had been successfully treated with glasses and/or surgery (defined as ≤5Δresidual strabismus). In addition, to be eligible, children had to have been wearing spectacle correction for at least 3 months prior to the baseline visit; furthermore, their referring ophthalmologist had to be willing to forgo other amblyopia treatments (if any) during the 2-week study period. Exclusion criteria were prematurity ≥8 weeks, developmental delay, and coexisting ocular or systemic diseases. Medical records were obtained from the referring ophthalmologists to extract diagnosis, cycloplegic refraction, and treatment plan.
Dichoptic Movies
During the 2-week study period, children wore glasses with polarized lenses to watch 6 dichoptic movies shown on a passive 3D display (LG Electronics USA; Englewood, NJ) in our laboratory. Dichoptic versions of 18 popular animated feature films were created. A screenshot from one of the movies is shown in Figure 1. The high-contrast image (left) was presented to the amblyopic eye and the low-contrast image (right) to the fellow eye. A patterned image mask composed of irregularly shaped blobs was multiplied with the images seen by the amblyopic eye, and the inverse patterned mask was multiplied with the images seen by the fellow eye. As a result, some parts of the image were only seen by one eye, some parts were only seen by the other eye, and some parts were seen by both eyes. It was necessary to piece the two eyes’ views together in order to appreciate the movies. The shape and location of the blobs were varied dynamically every 10 seconds.
FIG 1.
A screenshot from one of the dichoptic movies. The two eyes’ views are shown side by side for the sake of clarity but were displayed superimposed on a 3D monitor in the study. The high-contrast image (left) was presented to the amblyopic eye and low-contrast image (right) to the fellow eye. A patterned image mask composed of irregularly shaped blobs was multiplied with the images seen by the amblyopic eye, and the inverse patterned mask was multiplied with the images seen by the fellow eye. The shape and location of the blobs were varied dynamically every 10 seconds.
Study Protocol
The fellow-eye contrast was initially set individually for each amblyopic child at a reduced level that allowed binocular vision, based on the child’s dichoptic motion coherence threshold.2 Specifically, the initial contrast for the fellow eye was set to the dichoptic motion coherence threshold of −0.10, with a minimum setting of 0.20 and a maximum setting of 0.60. Children traveled to our laboratory 3 days per week and watched one movie per day. The fellow eye contrast was incremented by 10% for each subsequent movie (eg, with an initial contrast setting for the fellow eye of 0.30, subsequent movies would have fellow-eye contrasts of 0.33, 0.36, 0.40, 0.44, and 0.48). Each child was accompanied by at least one parent/guardian during the movie sessions to ensure compliance (polarized glasses wear and attention to the movie). Compliance was also confirmed by study personnel at 15- to 30-minute intervals.
Best-corrected visual acuity, random dot stereoacuity, and interocular suppression were measured at the baseline and 2-week outcome visits. Best-corrected visual acuity was obtained for each eye with the ATS-HOTV18 for children <7 years of age or E-ETDRS for children ≥7 years of age.19,20 Random dot stereoacuity was evaluated using the Randot Preschool Stereoacuity Test (Stereo Optical Co Inc, Chicago, IL), the Stereo Butterfly Test (Stereo Optical Co Inc), and the Lang-Stereotest I (Lang-Stereotest AG; Küsnacht, Switzerland).
Severity of interocular suppression was quantified using a dichoptic motion coherence test based on a concept first described by Mansouri and colleauges.2 Children wore glasses with polarized lenses to view dichoptic random dot kinematograms presented in a 22° diameter aperture on a passive 3D display (LG Electronics USA, Englewood, NJ). The amblyopic eye saw dots moving in a coherent direction (signal) and the fellow eye saw dots moving in random directions (noise). The task was to indicate the direction of coherent motion. Contrast was fixed at 1.0 for the amblyopic eye; contrast was initially set to 0.0 for the fellow eye and incremented in a 2-down-1-up staircase to determine the maximum tolerated fellow-eye contrast before the amblyopic eye was suppressed and the child could no longer report the direction of coherent motion. The maximum tolerated fellow eye contrast provided a quantitative measurement of the severity of suppression; the higher the level, the lower the severity of suppression.
Questionnaire
In order to informally assess the effect of standard movie and television watching on best-corrected visual acuity, we administered a questionnaire to the parents of the participants via Google Forms. The questionnaire collected retrospective data on how many hours children watched movies or television shows per day at home prior to the baseline visit, with or without patching. We identified the two consecutive visits to each participant’s pediatric ophthalmologist that occurred prior to baseline and extracted the best-corrected visual acuity from the medical records from these visits to assess the effects of television/movie viewing on visual acuity.
Data Analysis
Efficacy of watching the dichoptic movies was evaluated using paired t tests for the primary amblyopic eye best-corrected visual acuity outcome, and the secondary suppression outcome.
Results
All 8 referred amblyopic children (6 females [75%]) were enrolled. Baseline characteristics are summarized in Table 1. The cohort included 3 children (38%) with anisometropic amblyopia, 1 (13%) with strabismic amblyopia, and 4 (50%) with combined mechanism amblyopia. Amblyopic eye visual acuity ranged from 0.50 to 1.20 logMAR at baseline, and all had nil stereoacuity. None of the children in the study had manifest tropia following treatment with glasses and/or surgery. Prior to baseline, all children had worn glasses for ≥9 months with excellent compliance. Two participants had no amblyopia treatment prescribed other than spectacle correction prior to the baseline visit. Six children had patching treatment for ≥8 months prior to baseline; 2 had discontinued patching for more than 1 year prior to the baseline visit due to lack of continued visual acuity improvement despite reported good compliance and 4 stopped patching in order to participate in the study (these children also reported good compliance with patching).
Table 1.
Baseline characteristics of amblyopic children enrolled in the dichoptic movie study
| Patient | Sex | Type of amblyopiaa | Age, years | Amblyopic eye VA, logMar | Random dot stereoacuity | Cycloplegic refraction | Tropiab | Glasses | Strabismus surgery | Duration of spectacle wear prior to baseline, years | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Right eye | Left eye | ||||||||||
| 1 | M | A | 4.9 | 0.70 | nil | +6.25 +1.00 × 110 | +5.00 +1.00 × 085 | Ortho | Y | N | 0.8 |
| 2 | F | Ac | 7.2 | 1.20 | nil | +2.75 +2.25 × 100 | +2.50 +0.25 × 105 | Ortho | Y | N | 1.4 |
| 3 | F | A | 9.3 | 0.80 | nil | +4.50 +0.50 × 030 | +2.50 +0.25 × 120 | Ortho | Y | N | 1.8 |
| 4 | F | S | 7.3 | 0.80 | nil | +2.00 +0.75 × 180 | +1.50 +1.00 × 180 | Ortho | Y | N | 4.3 |
| 5 | F | C | 4.7 | 0.50 | nil | +1.75 | +3.50 | Ortho | Y | Y | 0.8 |
| 6 | F | C | 7.3 | 0.80 | nil | +3.25 +0.50 × 085 | +1.00 | Ortho | Y | Y | 3.9 |
| 7 | M | C | 8.2 | 0.50 | nil | +3.75 | +5.25 | Ortho | Y | Y | 4.8 |
| 8 | F | C | 10.7 | 0.50 | nil | +3.00 | +4.25 | Ortho | Y | N | 4.4 |
| Mean | 7.4 | 0.72 | 2.8 | ||||||||
| SD | 2.0 | 0.24 | 1.7 | ||||||||
LogMAR, logarithm of the minimum angle of stereoacuity; SD, standard deviation; VA, visual acuity.
A, anisometropic; C, combined mechanism; S, strabismic.
Angle of deviation at near measured by simultaeous prism and cover test with habitual glasses.
Astigmatic anisometropia.
During the 2-week study period, each amblyopic child watched 6 dichoptic movies, for a mean total time (with standard deviation [SD]) of 9.4 ± 0.9 hours. All children completed the study. The mean amblyopic eye best-corrected visual acuity (with standard error of the mean [SE]) improved from 0.72 ± 0.08 logMAR at baseline to 0.52 ± 0.09 logMAR at the 2-week visit (t7 = 4.38, P = 0.003, N = 8); that is, 2.0 lines of improvement. As shown in Figure 2, all 8 children had improved amblyopic eye best-corrected visual acuity at the 2-week outcome visit; 3 children with 0.5 logMAR baseline best-corrected visual acuity improved 0.1 logMAR (1 line), 4 children with 0.7–0.8 logMAR baseline BCVA improved 0.2–0.4 logMAR (2–4 lines), and 1 child with 1.2 logMAR baseline BCVA improved 0.1 logMAR (1 line). Fellow-eye BCVA did not change significantly during the 2-week study (mean change ± SE = 0.04 ± 0.03 logMAR; ie, 2 letters worse; t7 = 1.45; P = 0.19; N = 8).
FIG 2.
Amblyopic eye BCVA at baseline and 2-week outcome visits. Data points that would otherwise be superimposed have been jittered slightly for clarity. All eight children had improved amblyopic eye BCVA.
Interocular suppression was measured in the 7 of the 8 children at baseline and the 2-week outcome visit. In this brief 2-week study, no significant reduction in suppression was found (t6 = 0.77, P = 0.47, N = 7).
Parents of 6 of 8 children responded to the questionnaire about movie and television viewing time prior to the baseline. All reported that the child watched regular television or movies 1–2 hours daily during the months prior to the baseline visit. During the TV or movie watching, 3 of the children were patching and 3 were not. With a mean (± SD) interval of 7.8 ± 3.8 months between the first and second ophthalmology office visits, the mean best-corrected visual acuity (± SE) was 0.54 ± 0.11 logMAR on the initial visit and 0.50 ± 0.07 logMAR on the second visit, just before baseline (t5 = 2.57, P = 0.74). Our retrospective data are consistent with the concept that regular TV or movie viewing alone, either monocular or binocular, does not improve vision in the amblyopic eyes. However, because of the small sample size and the anecdotal nature of the data, we cannot draw any firm conclusions in this regard.
Discussion
The preliminary results of this proof-of-concept study demonstrate that passive viewing of dichoptic feature films is feasible and indicate the potential for a new treatment for childhood amblyopia. Although a separate control group was not incorporated in this pilot study, our retrospective data showed that regular TV/movie viewing (either monocular or binocular) for months prior to our study did not result in improved best-corrected visual acuity in the amblyopic eye. However, controlled clinical trials are needed to evaluate this potential amblyopia treatment more fully.
As in our previous study using binocular iPad games,12 no significant change in the severity of suppression after dichoptic movie watching was found in the current study. Similar results were also observed by Knox and colleagues, 9 who treated amblyopic children using binocular video games. On the other hand, using the same method to assess severity of suppression, several studies reported a significant reduction in suppression in adults after repeated binocular game play and that the change in severity was correlated with change in visual acuity.3–8,10 Because many of the adult studies required repeated practice and/or testing on the dichoptic motion coherence task,3–8,10 the adults may have experienced perceptual learning improvements in task performance that simply coincided with their visual acuity gains.
None of the children in the present study had improved random dot stereoacuity at the 2-week outcome visit, whereas other studies evaluating binocular treatment have reported that 50% to 60% achieved improved stereoacuity.3–10 This difference may in part be due to the different stereoacuity tests employed, including some with monocular cues.21–23 That monocular cues may underlie artifactual stereoacuity results is underscored by reports in which patients with tropias of 4°–20° (8Δ–40Δ) achieved stereoacuity of 20–500 arcsec.3–5
In conclusion, children achieved 1–4 lines of improvement in visual acuity with just 6 sessions (9 hours) of dichoptic movie viewing over 2 weeks. Patching, by comparison, requires 120 hours of treatment to achieve 1 line of improvement in amblyopic children who have already been treated with spectacles for 12–16 weeks.24 The maximum improvement that may be achieved by watching dichoptic movies remains to be determined. Whether improvements in visual acuity persist also remains to be determined. If these preliminary results are confirmed in a controlled clinical trial, passive viewing of dichoptic feature films could be useful as a primary, supplemental, or maintenance treatment for amblyopia.
Acknowledgments
This research was supported by NEI Grant EY022313, CIHR 53346 and a Fight for Sight 2013 Postdoctoral Award. It was performed at the Retina Foundation of the Southwest in Dallas, TX.
Footnotes
Conflict of interest: McGill University holds two patents for this dichoptic movie treatment. Drs. Reynaud and Hess are the named inventors. Other authors have no commercial relationships to disclose.
Data presented at 41st Annual Meeting of the American Association for Pediatric Ophthalmology and Strabismus, New Orleans, Louisiana, March 25–29, and at the Annual Meeting of the Association for Research in Vision and Ophthalmology, Denver, Colorado, May 3–7, 2015.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Baker DH, Meese TS, Mansouri B, Hess RF. Binocular summation of contrast remains intact in strabismic amblyopia. Invest Ophthalmol Vis Sci. 2007;48:5332–8. doi: 10.1167/iovs.07-0194. [DOI] [PubMed] [Google Scholar]
- 2.Mansouri B, Thompson B, Hess RF. Measurement of suprathreshold binocular interactions in amblyopia. Vision Res. 2008;48:2775–84. doi: 10.1016/j.visres.2008.09.002. [DOI] [PubMed] [Google Scholar]
- 3.Hess RF, Mansouri B, Thompson B. A new binocular approach to the treatment of amblyopia in adults well beyond the critical period of visual development. Restor Neurol Neurosci. 2010;28:793–802. doi: 10.3233/RNN-2010-0550. [DOI] [PubMed] [Google Scholar]
- 4.Hess RF, Mansouri B, Thompson B. A binocular approach to treating amblyopia: antisuppression therapy. Optom Vis Sci. 2010;87:697–704. doi: 10.1097/OPX.0b013e3181ea18e9. [DOI] [PubMed] [Google Scholar]
- 5.Hess RF, Mansouri B, Thompson B. Restoration of binocular vision in amblyopia. Strabismus. 2011;19:110–18. doi: 10.3109/09273972.2011.600418. [DOI] [PubMed] [Google Scholar]
- 6.Goodman LK, Black JM, Phillips G, Hess RF, Thompson B. Excitatory binocular interactions in two cases of alternating strabismus. J AAPOS. 2011;15:345–9. doi: 10.1016/j.jaapos.2011.03.017. [DOI] [PubMed] [Google Scholar]
- 7.To L, Thompson B, Blum JR, et al. A game platform for treatment of amblyopia. IEEE Trans Neural Syst Rehabil Eng. 2011;19:280–89. doi: 10.1109/TNSRE.2011.2115255. [DOI] [PubMed] [Google Scholar]
- 8.Hess RF, Thompson B, Black JM, et al. An iPod treatment of amblyopia: an updated binocular approach. Optometry. 2012;83:87–94. [PubMed] [Google Scholar]
- 9.Knox PJ, Simmers AJ, Gray LS, Cleary M. An exploratory study: prolonged periods of binocular stimulation can provide an effective treatment for childhood amblyopia. Invest Ophthalmol Vis Sci. 2012;53:817–24. doi: 10.1167/iovs.11-8219. [DOI] [PubMed] [Google Scholar]
- 10.Li J, Thompson B, Deng D, Chan LY, Yu M, Hess RF. Dichoptic training enables the adult amblyopic brain to learn. Curr Biol. 2013;23:R308–9. doi: 10.1016/j.cub.2013.01.059. [DOI] [PubMed] [Google Scholar]
- 11.Hess RF, Babu RJ, Clavagnier S, Black J, Bobier W, Thompson B. The iPod binocular home-based treatment for amblyopia in adults: efficacy and compliance. Clin Exp Optom. 2014;97:389–98. doi: 10.1111/cxo.12192. [DOI] [PubMed] [Google Scholar]
- 12.Li SL, Jost RM, Morale SE, et al. A binocular iPad treatment for amblyopic children. Eye (Lond) 2014;28:1246–53. doi: 10.1038/eye.2014.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mansouri B, Singh P, Globa A, Pearson P. Binocular training reduces amblyopic visual acuity impairment. Strabismus. 2014;22:1–6. doi: 10.3109/09273972.2013.877945. [DOI] [PubMed] [Google Scholar]
- 14.Birch EE, Li SL, Jost RM, et al. Binocular iPad treatment for amblyopia in preschool children. J AAPOS. 2015;19:6–11. doi: 10.1016/j.jaapos.2014.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hess RF, Thompson B. Amblyopia and the binocular approach to its therapy. Vision Res. 2015;114:4–16. doi: 10.1016/j.visres.2015.02.009. [DOI] [PubMed] [Google Scholar]
- 16.Li SL, Jost RM, Morale SE, et al. Binocular iPad treatment of amblyopia for lasting improvement of visual acuity. JAMA Ophthalmol. 2015;133:479–80. doi: 10.1001/jamaophthalmol.2014.5515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vedamurthy I, Nahum M, Huang SJ, et al. A dichoptic custom-made action video game as a treatment for adult amblyopia. Vision Res. 2015;114:173–87. doi: 10.1016/j.visres.2015.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Moke PS, Turpin AH, Beck RW, et al. Computerized method of visual acuity testing: adaptation of the amblyopia treatment study visual acuity testing protocol. Am J Ophthalmol. 2001;132:903–9. doi: 10.1016/s0002-9394(01)01256-9. [DOI] [PubMed] [Google Scholar]
- 19.Beck RW, Moke PS, Turpin AH, et al. A computerized method of visual acuity testing: adaptation of the early treatment of diabetic retinopathy study testing protocol. Am J Ophthalmol. 2003;135:194–205. doi: 10.1016/s0002-9394(02)01825-1. [DOI] [PubMed] [Google Scholar]
- 20.Cotter SA, Chu RH, Chandler DL, et al. Reliability of the electronic early treatment diabetic retinopathy study testing protocol in children 7 to <13 years old. Am J Ophthalmol. 2003;136:655–61. doi: 10.1016/s0002-9394(03)00388-x. [DOI] [PubMed] [Google Scholar]
- 21.Fawcett SL, Birch EE. Validity of the Titmus and Randot circles tasks in children with known binocular vision disorders. J AAPOS. 2003;7:333–8. doi: 10.1016/s1091-8531(03)00170-8. [DOI] [PubMed] [Google Scholar]
- 22.Leske DA, Birch EE, Holmes JM. Real depth vs randot stereotests. Am J Ophthalmol. 2006;142:699–701. doi: 10.1016/j.ajo.2006.04.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Odell NV, Hatt SR, Leske DA, Adams WE, Holmes JM. The effect of induced monocular blur on measures of stereoacuity. J AAPOS. 2009;13:136–41. doi: 10.1016/j.jaapos.2008.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stewart CE, Stephens DA, Fielder AR, Moseley MJ, Cooperative M. Modeling dose-response in amblyopia: toward a child-specific treatment plan. Invest Ophthalmol Vis Sci. 2007;48:2589–94. doi: 10.1167/iovs.05-1243. [DOI] [PubMed] [Google Scholar]