Summary
Objectives
Although postmastectomy radiation therapy (PMRT) has been shown to reduce breast cancer burden and improve survival, PMRT may negatively influence outcomes after reconstruction. The goal of this study was to compare current opinions of plastic and reconstructive surgeons (PRS) and surgical oncologists (SO) regarding the optimal timing of breast reconstruction for patients requiring PMRT.
Methods
Members of the American Society of Plastic Surgeons (ASPS), the American Society of Breast Surgeons (ASBS), and the Society of Surgical Oncology (SSO) were asked to participate in an anonymous web-based survey. Responses were solicited in accordance to the Dillman method, and they were analyzed using standard descriptive statistics.
Results
A total of 330 members of the ASPS and 348 members of the ASBS and SSO participated in our survey. PRS and SO differed in patient–payor mix (p < 0.01) and practice setting (p < 0.01), but they did not differ by urban versus rural setting (p = 0.65) or geographic location (p = 0.30). Although PRS favored immediate reconstruction versus SO, overall timing did not significantly differ between the two specialists (p = 0.14). The primary rationale behind delayed breast reconstruction differed significantly between PRS and SO (p < 0.01), with more PRS believing that the reconstructive outcome is significantly and adversely affected by radiation. Both PRS and SO cited “patient-driven desire to have immediate reconstruction” (p = 0.86) as the primary motivation for immediate reconstruction.
Conclusions
Although the optimal timing of reconstruction is controversial between PRS and SO, our study suggests that the timing of reconstruction in PMRT patients is ultimately driven by patient preferences and the desire of PRS to optimize aesthetic outcomes.
Keywords: Postmastectomy radiation therapy, Breast reconstruction, Immediate breast reconstruction, Delayed breast reconstruction, Delayed–immediate breast reconstruction, Current practices
Introduction
The integration of cross-disciplinary interventions from surgical oncology, reconstructive surgery, and radiation therapy has improved outcomes and quality of life for patients with locally invasive breast cancer. Although these interventions have improved survival, the optimal timing of breast reconstruction in relation to postmastectomy radiation therapy (PMRT) remains a controversial topic between plastic and reconstructive surgeons (PRS) and surgical oncologists (SO). For example, many patients require radiation following mastectomy, an intervention referred to as PMRT.1–4 Although breast reconstruction is an essential part of patient care, it also has the potential to complicate further cancer treatment. Conversely, radiation therapy may compromise the overall aesthetic outcome and patient satisfaction with the repair.
Three options exist for breast reconstruction. “Immediate” breast reconstruction may be performed following the mastectomy under the same course of anesthesia. “Delayed” breast reconstruction is performed at a later time as a separate operation. “Delayed–immediate breast reconstruction,” described subsequently, is a two-step procedure that stakes a claim to the middle ground between the immediate and delayed methods.2,4 In all methods, a subsequent, smaller touch-up procedure is typically employed some months after the first reconstructive operation.
Each method offers distinct advantages and disadvantages. Immediate breast reconstruction yields superior short-term aesthetic, psychosocial, and quality of life results compared with delayed reconstruction.2,5 Immediate reconstruction only involves a single initial operation, a shorter period of hospitalization, and a lower overall cost.2,6–9 Some studies suggest that all patients should pursue immediate reconstruction following mastectomy on account of the psychosocial benefits, regardless of age or associated comorbidities.10–12
Immediate reconstruction is widely preferred if PMRT is not anticipated. However, in some cases, the need for PMRT cannot be reliably determined until review of the permanent tissue sections. Some authors note a slight increase in complications such as increased susceptibility to infection, decreased wound-healing capacity, tissue fibrosis, shrinkage, and decreased elasticity in immediate reconstruction.13–17 It has also been associated with a higher rate of late complications compared with delayed reconstruction. In addition, immediate reconstruction may possibly increase the amount of radiation needed for effective radiotherapy, and theoretically it may increase the radiation dose to the heart and lungs.18
Delayed breast reconstruction avoids these disadvantages, and it may be preferable for patients who will require PMRT (i.e., patients with stage III+ breast cancer). However, delayed reconstruction results in neither superior oncological outcomes nor improved technical feasibility compared with immediate reconstruction.19–21 In addition, while several studies have reported complications secondary to radiotherapy in the setting of immediate breast reconstruction, there is a lack of firm consensus in the literature.22,23
Some authors advocate a middle ground in the form of delayed–immediate reconstruction, a two-stage method combining elements of both other methods. Delayed–immediate reconstruction optimizes reconstruction in patients who may require postoperative PMRT.24–26 A skin-sparing mastectomy is performed, and a tissue expander is placed to prevent the skin envelope from shrinking down and becoming irreversibly contracted and scarred. If needed, PMRT is administered with the tissue expander in place, thus sparing the anticipated autologous reconstruction from radiation damage. The expander is then replaced with autologous tissue at a second stage. This method allows patients who do not require PMRT to receive the benefits of skin-sparing mastectomy with aesthetic outcomes similar to those of immediate reconstruction. However, patients who do require PMRT receive a skin-preserving delayed reconstruction, which effectively imports a large mass of healthy unirradiated autologous tissue to augment the blood supply of native radiation-damaged breast skin. This helps mitigate the aesthetic complications that can occur after immediate breast reconstruction followed by PMRT.
Currently, the optimal timing of reconstruction and PMRT in the treatment of breast cancer remains a controversial topic, with different viewpoints from each type of specialist.26,27 As stated, the goal of this study is to assess and compare the opinions of PRS and SO on this topic.
Methods
Members of the American Society of Plastic Surgeons (ASPS), the American Society of Breast Surgeons (ASBS), and the Society of Surgical Oncology (SSO) were invited to participate in an anonymous, web-based survey of their preferred timing and method of breast reconstruction in patients who will receive PMRT. Responses were systematically solicited in a manner consistent with the total design method as outlined by D.A. Dillman.28 In this regard, participants were surveyed in the contexts of geographical location, patient–payor mix, and practice setting.
Statistical analysis was performed in Statistical Analysis System (SAS) Version 9.3 (SAS Institute, Cary, NC, USA). Standard descriptive statistics were used to determine the distribution of each question. Practice profiles including patient–payor mix, geographic location, and type of practice setting were summarized using descriptive statistics. Frequencies and percentages were calculated. Chisquared and Cochran–Armitage Trend tests were used to investigate differences between PRS and SO.
Results
A total of 330 ASPS and 348 combined members of the ASBS and SSO participated in the survey. The respondents represented all four major geographic distributions within the United States, with most PRS practicing in the West (27.9%) and most SO practicing in the Northeast (28.7%).
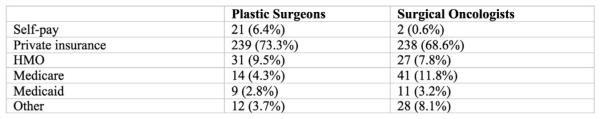
With regard to practice setting, respondents predominantly represented private practice (75.5% of PRS and 52.3% of SO) followed by university/teaching hospitals (22.4% of PRS and 32.0% of SO) (Figure 1). The type of practice setting significantly differed among PRS and SO (p < 0.01) as did patient–payor mix between the two specialists (p < 0.01). A significantly greater portion of SO practiced in specialized cancer centers versus PRS (15.7% vs. 2.1%), whereas more PRS than SO were in private practice (75.5% vs. 52.3%) (Figure 1). However, SO and PRS did not significantly differ by urban versus rural setting (p = 0.65) or geographic location (p = 0.30).
Figure 1.
Physician practice setting.
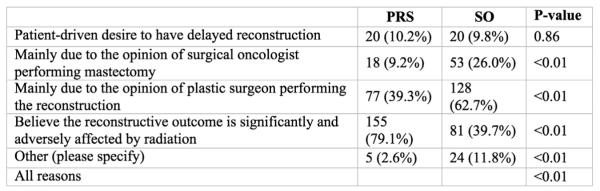
With respect to patient–payor mix, a larger proportion of the PRS patient population was self-pay (6.4% vs. 0.6%), whereas a larger proportion of the SO patient population had Medicare (11.8% vs. 4.3%) (Figure 2).
Figure 2.
Patient insurance payors.
PRS and SO did not significantly differ in the overall types or timing of reconstruction offered to their patients; both groups offered similar types of autologous- and prosthetic-based reconstructions, and both groups performed mostly immediate reconstructions (p = 0.14). It should be noted, however, that among the various repair types, the SO were significantly more likely to refer patients for DIEP/superficial inferior epigastric artery (SIEA) flaps as opposed to PRS (p < 0.0001) (Figure 3).
Figure 3.
Type of breast reconstruction offered to patients. a: Preferred type of immediate reconstruction with PMRT. b: Portion of reconstructions that are immediate versus delayed. c: Preference toward timing of reconstruction involving PMRT. d: Primary reasons for immediate reconstruction in patients with planned PMRT.
By contrast, in the setting of PMRT and immediate reconstruction, PRS and SO had significant differences. SO tended to prefer tissue expanders/implants more than PRS did (52.6% vs. 39.5%; p < 0.01), whereas PRS favored pedicled TRAM flaps more than SO did (17.6% vs. 11.4%; p < 0.01) (Figure 3a).
The majority of both PRS and SO indicated that 75% or more of their overall breast reconstructions are immediate (Figure 3b).
Although both groups performed mostly immediate reconstructions, the vast majority of both PRS and SO preferred delayed or delayed–immediate reconstruction in patients undergoing reconstruction and requiring PMRT (Figure 3c).
In the small percentage of cases where immediate breast reconstruction was performed when PMRT was planned, >65% of both PRS and SO cited patient preference as the most common reason for performing immediate reconstruction. The opinion of the SO was the one significant difference between the respondent groups in this area (Figure 3d).
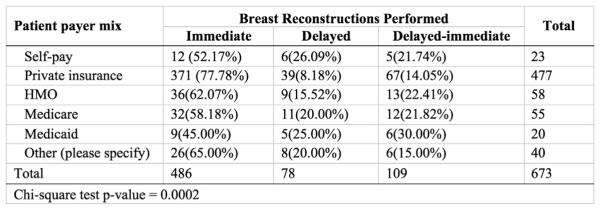
Interestingly, a minority of PRS (19%) and SO (23%) believed that the reconstructive outcome is not affected by radiation therapy. However, in the setting of delayed reconstruction, the most common rationale cited for delaying the repair by PRS was that the reconstructive outcome is significantly and adversely affected by radiation (79%) (Figure 4). The majority of SO respondents chose delayed reconstruction because of the opinion of the PRS performing the surgery (63%; p < 0.01). For patients receiving a delayed–immediate repair, PRS and SO did not disagree on patient preference as a driving reason behind the timing of the procedure (p = 0.93), but disagreed on the underlying rationale for this modality.
Figure 4.
Primary reason for delayed reconstruction in patients who will require PMRT.
Although minor variation existed between groups, our study found that most surgeons in both groups prefer to wait for 6–9 months before performing a second procedure after PMRT is given, presumably to give the irradiated soft-tissue envelope sufficient time to heal before another surgery. However, the groups differed on the sequence of expansion in the context of temporary expanders (p < 0.01). The vast majority of PRS preferred complete expansion first followed by radiation treatment (60.7%). By contrast, SO did not strongly prefer a particular option for handling the temporary tissue expansion.
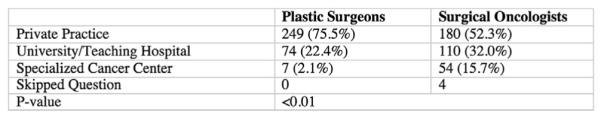
Because practice setting and payor mix may impact treatment decisions, we conducted further analysis based upon these two variables.29 We ultimately found that PRS and SO in private practice do not choose different repair modalities than PRS and SO in specialized cancer centers and university/teaching hospitals (p = 0.23). However, we found that the patient–payor mix correlates with the chosen repair modality (p < 0.01). Patients with private insurance tended to have immediate reconstruction (77.78%), whereas patients with self-pay or Medicaid were more likely to have delayed reconstruction (Figure 5).
Figure 5.
Payor mix and reconstructions performed.
Discussion
We found that the SO and PRS preferences did not significantly differ by urban versus rural location (P = 0.65) or by geography (P = 0.30). These data suggest that the survey respondents represent institutions from larger cities spread evenly throughout the United States.
We found statistically significant demographic differences between SO and PRS with regard to patient–payor mix (P < 0.01) and the type of practice setting (P < 0.01). This may be due to the fact that patients who visit PRS for aesthetic and elective procedures may also opt to visit their same surgeon for a postmastectomy reconstruction. Furthermore, it is likely that SO may be more represented in academic or in university settings and specialized cancer centers. This might skew responses where reported practices reflect the standard of care at a multidisciplinary cancer center where we would naturally expect an intrinsically higher level of consensus between SO and PRS rather than the specific individual preferences of a subspecialty. This nuance could be investigated by studying how preferences in patient management differ from center to center.
In addition, there was a significantly higher proportion of SO who offered DIEP/SIEA flaps as part of their overall care regimen when compared with PRS. Once again, this may be in part explained by the fact that more SO in this study represented academic or university settings and specialized cancer centers. It is well established that DIEP/SIEA flaps are more technically demanding, and therefore they require significantly more advanced training. This observation may be in part explained by the fact that specialized academic or cancer centers are more likely to have available sophisticated facilities and plastic surgeons with advanced fellowships and microsurgical training.
The overall timing preferences for breast reconstruction did not differ between PRS and SO (p = 0.14). In general, patients of surveyed SO were significantly more likely to have immediate, rather than delayed breast reconstruction. Again, this may be due to the increased availability of plastic surgeons at the larger institutions of the surveyed SO respondents.
For patients undergoing autologous reconstruction and requiring PMRT, both PRS and SO overwhelmingly favored delayed reconstruction or delayed–immediate reconstruction over immediate reconstruction. Patient-driven desire was the primary reason for pursuing immediate repair when PMRT was planned. In addition, SO weighted “the opinion of the SO performing mastectomy” more than PRS colleagues as a primary reason for choosing immediate reconstruction. This suggests that SO may be less likely to be influenced by the opinion of PRS than the converse regarding the timing of immediate reconstruction with planned PMRT.
Unlike immediate reconstruction, almost every rationale for delayed breast reconstruction differed between PRS versus SO (p < 0.01). Only “patient-driven desire to have delayed reconstruction” was similar (p = 0.86).
For delayed–immediate reconstruction, SO more often favored opinions of SO or PRS as a motivating factor (p < 0.01 for both). However, PRS predominantly cited aesthetic outcome as the most important reason for pursuing delayed–immediate reconstruction (p < 0.05). Compared with SO, it is possible that PRS may be more familiar with managing the complications and poorer outcomes often associated with radiation and breast reconstruction. In addition, it is clear that SO have a stronger preference for tissue expansion/implants than PRS in the setting of immediate breast reconstruction and PMRT. In the context of immediate breast reconstruction and PMRT, SO prefer tissue expansion and implant reconstruction, whereas PRS prefer autologous tissue reconstruction. This difference in preference may also be due to PRS familiarity with the much greater risk of complications and unplanned surgery when PMRT is introduced into an implant-based reconstruction.29
Regarding delayed–immediate reconstruction, most PRS endorsed complete expansion before radiotherapy, whereas most SO favored partial expansion followed by radiation and then followed by complete expansion (p < 0.05 for both). The preference by SO may reflect a belief that the deflation of the expander may allow for more optimal administration of radiation therapy. Conversely, PRS may be more concerned by possible soft-tissue contraction that often occurs following PMRT and which can limit later expansion.
Our study was limited by a <100% questionnaire completion rate; a small percentage of respondents skipped some questions or selected “other.” Furthermore, our questionnaire did not ask the respondents to further clarify what percentage of the breast reconstructions performed in their respective practice settings required PMRT. We did not ask for patient data to validate surgeon preferences, so responses reflected clinician’s self-perception rather than actual history of surgical procedures. Finally, our simple survey assessed preferences, and it did not elaborate on more nuanced decision making made by clinicians, patients, and their families.
Conclusion
The results of this survey provide insight into the preferences of PRS and SO regarding the timing of the reconstruction following PMRT. Although there is some concordance between the two groups, our data suggest that the timing of the reconstruction is driven primarily by patient preference and PRS concern for optimal aesthetic outcome. Nevertheless, these discrepancies, the growing complexity of treatment, and the ever-evolving dynamic of interdisciplinary care emphasize the need for further dialog between surgical and oncologic colleagues to maximize outcomes for breast cancer patients.
Acknowledgments
Funding
None.
Footnotes
Conflicts of interest
We do not have any relevant conflicts of interest to disclose.
References
- 1.Dean C, Chetty U, Forrest APM. Effects of immediate breast reconstruction on psychosocial morbidity after mastectomy. Lancet. 1983;321:459–62. doi: 10.1016/s0140-6736(83)91452-6. [DOI] [PubMed] [Google Scholar]
- 2.Chevray PM. Timing of breast reconstruction: immediate versus delayed. Cancer J. 2008;14:223–9. doi: 10.1097/PPO.0b013e3181824e37. [DOI] [PubMed] [Google Scholar]
- 3.Wilkins EG, et al. Prospective analysis of psychosocial outcomes in breast reconstruction: one-year postoperative results from the Michigan Breast Reconstruction Outcome Study. Plast Reconstr Surg. 2000;106:1014–25. doi: 10.1097/00006534-200010000-00010. discussion 1026–7. [DOI] [PubMed] [Google Scholar]
- 4.Kronowitz SJ, Robb GL. Breast reconstruction with postmastectomy radiation therapy: current issues. Plast Reconstr Surg. 2004;114:950–60. doi: 10.1097/01.prs.0000133200.99826.7f. [DOI] [PubMed] [Google Scholar]
- 5.Elder EE, et al. Quality of life and patient satisfaction in breast cancer patients after immediate breast reconstruction: a prospective study. Breast. 2005;14:201–8. doi: 10.1016/j.breast.2004.10.008. [DOI] [PubMed] [Google Scholar]
- 6.Carnevale A, et al. Radiation therapy after breast reconstruction: outcomes, complications, and patient satisfaction. Radiol Med. 2013;118:1240–50. doi: 10.1007/s11547-013-0947-6. [DOI] [PubMed] [Google Scholar]
- 7.Khoo A, Kroll SS, Reece GP, et al. A comparison of resource costs of immediate and delayed breast reconstruction. Plast Reconstr Surg. 1998;101:969–70. doi: 10.1097/00006534-199804040-00011. [DOI] [PubMed] [Google Scholar]
- 8.Cowen D, et al. Immediate post-mastectomy breast reconstruction followed by radiotherapy: risk factors for complications. Breast Cancer Res Treat. 2010;121:627–34. doi: 10.1007/s10549-010-0791-5. [DOI] [PubMed] [Google Scholar]
- 9.Hussien M, Salah B, Malyon A, Wieler-Mithoff EM. The effect of radiotherapy on the use of immediate breast reconstruction. Eur J Surg Oncol. 2004;30:490–4. doi: 10.1016/j.ejso.2004.03.005. [DOI] [PubMed] [Google Scholar]
- 10.Shah C, Kundu N, Arthur D, Vicini F. Radiation therapy following postmastectomy reconstruction: a systematic review. Ann Surg Oncol. 2013;20:1313–22. doi: 10.1245/s10434-012-2689-4. [DOI] [PubMed] [Google Scholar]
- 11.Atisha D, et al. Prospective analysis of long-term psychosocial outcomes in breast reconstruction: two-year postoperative results from the Michigan Breast Reconstruction Outcomes Study. Ann Surg. 2008;247:1019–28. doi: 10.1097/SLA.0b013e3181728a5c. [DOI] [PubMed] [Google Scholar]
- 12.Veronesi P, et al. Immediate breast reconstruction after mastectomy. Breast. 2011;20(Suppl. 3):S104–7. doi: 10.1016/S0960-9776(11)70305-8. [DOI] [PubMed] [Google Scholar]
- 13.Anavekar NS, Rozen WM, Le Roux CM, Ashton MW. Achieving autologous breast reconstruction for breast cancer patients in the setting of post-mastectomy radiotherapy. J Cancer Surviv. 2011;5:1–7. doi: 10.1007/s11764-010-0155-5. [DOI] [PubMed] [Google Scholar]
- 14.Behranwala KA, et al. The influence of radiotherapy on capsule formation and aesthetic outcome after immediate breast reconstruction using biodimensional anatomical expander implants. J Plast Reconstr Aesthet Surg. 2006;59:1043–51. doi: 10.1016/j.bjps.2006.01.051. [DOI] [PubMed] [Google Scholar]
- 15.Alderman AK, Jagsi R. Discussion: Immediate post-mastectomy breast reconstruction followed by radiotherapy: risk factors for complications. Breast Cancer Res Treat. 2010;121:635–7. doi: 10.1007/s10549-010-0878-z. [DOI] [PubMed] [Google Scholar]
- 16.Berry T, et al. Complication rates of radiation on tissue expander and autologous tissue breast reconstruction. Ann Surg Oncol. 2010;17(Suppl. 3):202–10. doi: 10.1245/s10434-010-1261-3. [DOI] [PubMed] [Google Scholar]
- 17.Tran NV, Chang DW, Gupta A, Kroll SS, Robb GL. Comparison of immediate and delayed free TRAM flap breast reconstruction in patients receiving postmastectomy radiation therapy. Plast Reconstr Surg. 2001 Jul;108(1):78–82. doi: 10.1097/00006534-200107000-00013. [DOI] [PubMed] [Google Scholar]
- 18.Buchholz TA, Kronowitz SJ, Kuerer HM. Immediate breast reconstruction after skin-sparing mastectomy for the treatment of advanced breast cancer: radiation oncology considerations. Ann Surg Oncol. 2002;9:820–1. doi: 10.1007/BF02574506. [DOI] [PubMed] [Google Scholar]
- 19.Meretoja TJ, et al. Local recurrence of stage 1 and 2 breast cancer after skin-sparing mastectomy and immediate breast reconstruction in a 15-year series. Eur J Surg Oncol. 2007;33:1142–5. doi: 10.1016/j.ejso.2007.03.022. [DOI] [PubMed] [Google Scholar]
- 20.Giacalone PL, et al. New concept for immediate breast reconstruction for invasive cancers: feasibility, oncological safety and esthetic outcome of post-neoadjuvant therapy immediate breast reconstruction versus delayed breast reconstruction: a prospective pilot study. Breast Cancer Res Treat. 2010;122:439–51. doi: 10.1007/s10549-010-0951-7. [DOI] [PubMed] [Google Scholar]
- 21.Schaverien MV, Macmillan RD, McCulley SJ. Is immediate autologous breast reconstruction with postoperative radiotherapy good practice?: a systematic review of the literature. J Plast Reconstr Aesthetic Surg. 2013;66:1637–51. doi: 10.1016/j.bjps.2013.06.059. [DOI] [PubMed] [Google Scholar]
- 22.Soong IS, Yau TK, Ho CM, et al. Post-mastectomy radiotherapy after immediate autologous breast reconstruction in primary treatment of breast cancers. Clin Oncol (R Coll Radiol) 2004 Jun;16:283–9. doi: 10.1016/j.clon.2004.01.007. [DOI] [PubMed] [Google Scholar]
- 23.Hunt KK, Baldwin BJ, Strom EA, et al. Feasibility of postmastectomy radiation therapy after TRAM flap breast reconstruction. Ann Surg Oncol. 1997 Jul-Aug;4(5):377–84. doi: 10.1007/BF02305549. [DOI] [PubMed] [Google Scholar]
- 24.Kronowitz SJ. Delayed-immediate breast reconstruction: technical and timing considerations. Plast Reconstr Surg. 2010 Feb;125(2):463–74. doi: 10.1097/PRS.0b013e3181c82d58. [DOI] [PubMed] [Google Scholar]
- 25.Kronowitz SJ, Hunt KK, Kuerer HM, et al. Delayed-immediate breast reconstruction. Plast Reconstr Surg. 2004 May;113(6):1617–28. doi: 10.1097/01.prs.0000117192.54945.88. [DOI] [PubMed] [Google Scholar]
- 26.Tadiparthi S, Alrawi M, Collis N. Two-stage delayed breast reconstruction with an expander and free abdominal tissue transfer: outcomes of 65 consecutive cases by a single surgeon. J Plast Reconstr Aesthetic Surg. 2011;64:1608–12. doi: 10.1016/j.bjps.2011.06.046. [DOI] [PubMed] [Google Scholar]
- 27.Kronowitz SJ, Kuerer HM. Advances and surgical decision-making for breast reconstruction. Cancer. 2006;107:893–907. doi: 10.1002/cncr.22079. [DOI] [PubMed] [Google Scholar]
- 28.Hoddinott SN, Bass MJ. The dillman total design survey method: a sure-fire way to get high survey return rates. Can Fam Physician. 1986;32 [PMC free article] [PubMed] [Google Scholar]
- 29.Kronowitz SJ, Robb GL. Radiation therapy and breast reconstruction: a critical review of the literature. Plast Reconstr Surg. 2009;124:395–408. doi: 10.1097/PRS.0b013e3181aee987. [DOI] [PubMed] [Google Scholar]