Abstract
Study question Is methylphenidate beneficial or harmful for the treatment of attention-deficit/hyperactivity disorder (ADHD) in children and adolescents?
Methods Electronic databases were searched up to February 2015 for parallel and crossover randomised clinical trials comparing methylphenidate with placebo or no intervention in children and adolescents with ADHD. Meta-analyses and trial sequential analyses (TSA) were conducted. Quality was assessed using GRADE. Teachers, parents, and observers rated ADHD symptoms and general behaviour.
Study answer and limitations The analyses included 38 parallel group trials (n=5111, median treatment duration 49 days) and 147 crossover trials (n=7134, 14 days). The average age across all studies was 9.7 years. The analysis suggested a beneficial effect of methylphenidate on teacher rated symptoms in 19 parallel group trials (standardised mean difference (SMD) −0.77, n=1698), corresponding to a mean difference of −9.6 points on the ADHD rating scale. There was no evidence that methylphenidate was associated with an increase in serious adverse events (risk ratio 0.98, nine trials, n=1532; TSA adjusted intervention effect RR 0.91). Methylphenidate was associated with an increased risk of non-serious adverse events (1.29, 21 trials, n=3132; TSA adjusted RR 1.29). Teacher rated general behaviour seemed to improve with methylphenidate (SMD −0.87, five trials, n=668) A change of 7 points on the child health questionnaire (CHQ) has been deemed a minimal clinically relevant difference. The change reported in a meta-analysis of three trials corresponds to a mean difference of 8.0 points on the CHQ (range 0-100 points), which suggests that methylphenidate may improve parent reported quality of life (SMD 0.61, three trials, n=514). 96.8% of trials were considered high risk of bias trials according to the Cochrane guidelines. All outcomes were assessed very low quality according to GRADE.
What this study adds The results suggest that among children and adolescents with a diagnosis of ADHD, methylphenidate may improve teacher reported symptoms of ADHD and general behaviour and parent reported quality of life. However, given the risk of bias in the included studies, and the very low quality of outcomes, the magnitude of the effects is uncertain. Methylphenidate is associated with an increased risk of non-serious but not serious adverse events.
Funding, competing interests, data sharing Region Zealand Research Foundation and Copenhagen Trial Unit. Competing interests are given in the full paper on bmj.com. Full data are available in the version of this review published in The Cochrane Library.
Introduction
Attention-deficit/hyperactivity disorder (ADHD) is one of the most commonly diagnosed and treated childhood psychiatric disorders,1 with a prevalence of 3.4%.2 It is increasingly seen as a developmental disorder, which has high comorbidity with other psychiatric disorders.3 Diagnosis is made through recognition of excessive inattention, hyperactivity, and impulsivity in children before 12 years of age, which impairs their functioning or development.4 5
Methylphenidate has been used for the treatment of ADHD for over 50 years and is now globally the most common drug treatment for the disorder.6 7 Despite the widespread use of methylphenidate no comprehensive systematic review has been done of both benefits and harms. Fifteen reviews of the effect of methylphenidate on the symptoms of ADHD in children and adolescents have been published.8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 None of them were conducted using Cochrane methodology and none prepublished a peer reviewed protocol. Thirteen did not undertake subgroup analyses on comorbidity influencing treatment effects 8 9 10 11 12 13 14 15 16 18 19 21 22 nor did they control for the treatment effect on subtypes of ADHD.8 10 11 15 16 17 18 19 21 22 Ten did not consider dosage.9 10 12 13 15 16 18 19 20 22 Seven meta-analyses combined outcome data across raters and observers8 9 10 15 16 17 20 and eight did not separate outcomes for inattention and hyperactivity or impulsivity.8 10 11 12 13 15 16 22 Nine failed to present spontaneous adverse events10 11 12 13 14 15 16 18 22 and 14 did not report adverse events measured by rating scales.8 10 11 12 13 14 15 16 17 18 19 20 21 22 Eleven reviews 8 9 10 11 12 13 14 16 17 21 22 did not follow ‘gold standard’ guidelines—that is, the Cochrane Handbook23 or the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines.24 25 Risk of random errors, risk of bias, and trial quality were not systematically assessed in 11 reviews.8 9 10 11 12 13 14 15 16 17 22 Language bias (exclusion of non-English publications) was present in four reviews,10 14 19 22 and narrow or unreported search strategies in four reviews8 11 16 20 may have compromised data collection and, ultimately the meta-analyses.
To avoid these flaws we conducted a systematic review of the benefits and harms of methylphenidate in children and adolescents with ADHD using the Cochrane Handbook23 and PRISMA guidelines.24 25 This article presents the results of a systematic review focusing on the benefits and harms of methylphenidate in randomised clinical trials.26 A second systematic review will focus on harms in non-randomised studies.27
Methods
We used Cochrane methodology,23 following our published protocol.28
Study selection
We included both parallel and crossover randomised clinical trials comparing all types of methylphenidate with placebo or no intervention in children and adolescents from 3 to 18 years of age (two trials recruited a small number of participants aged 19 to 21) with ADHD. Trials were included irrespective of language, publication year, publication type, or publication status. After the exclusion of duplicates and studies not meeting the inclusion criteria, we obtained full text articles as per protocol.28
Inclusion criteria
In one trial the diagnosis used for ADHD had to be determined according to the Diagnostic and Statistical Manual of Mental Disorders (third edition, third edition revised, fourth edition, fourth edition revised, or fifth edition),4 or according to International Classification of Diseases ninth or 10th revisions (ICD-9 or ICD-10 codes).5 At least 75% of participants had to be aged less than 19 years and the mean age of the study population had to be less than 19 years. We included trials in which participants had comorbidities; however, at least 75% of the participants were required to have an intellectual quotient in the normal range (IQ >70).
Search strategy and selection criteria
We searched the Cochrane Central Register of Controlled Trials (The Cochrane Library 2015, Issue 2), Medline, Embase, CINAHL, PsycINFO, ISI Conference Proceedings Citation Index, Science and Conference Proceedings Citation Index-Social Science & Humanities (Web of Science), ClincalTrials.gov, and WHO’s International Clinical Trials Registry Platform up to February 2015 using two different search strategies, one for efficacy and one for adverse events. The complete search strategy is available in the Cochrane review.26 We screened reference lists of identified reviews, meta-analyses, and a selection of included trials for additional relevant articles. Furthermore, we contacted pharmaceutical companies, including Shire, Medice (represented in Denmark by HB Pharma), Janssen-Cilag, and Novartis for published and unpublished data. Emails were also sent to experts in the discipline requesting data on unpublished or ongoing studies.
Outcomes
The primary outcomes were symptoms of ADHD (inattention, hyperactivity, and impulsivity), both short term (six months or less) and long term (more than six months), and serious adverse events. We defined the latter as any event that led to death, was life threatening, required hospital admission or prolongation of existing hospital stay, resulted in persistent or major disability, and any important medical event that may have jeopardised the participant’s life or required intervention to prevent it. All other adverse events were considered non-serious.29
Secondary outcomes were non-serious adverse events, general behaviour, and quality of life. We assessed all non-serious adverse events, including growth, cardiological, neurological, gastrointestinal, and sleep events, and appetite. We rated general behaviour at school and home using psychometric validated instruments. Behaviour was classified according to length of assessment as short (six months or less) or long term (more than six months). Quality of life was measured by psychometric validated instruments.
Patient involvement
No patients were involved in setting the research question or the outcome measures, nor were they involved in the design and implementation of the study. There are no plans to involve patients in dissemination of the results.
Data extraction and synthesis
Seventeen reviewers extracted the data independently in the first of a two phase process.26 In the second phase, a different reviewer checked the extracted data and disparities were resolved through discussion between extractors, or consultation with the first author (OJS) where consensus was not reached.26 For additional questions and missing data we contacted the authors of trials. Furthermore, we contacted all authors of the crossover trials to obtain data for all periods of the trial. We used Mendeley and Google Drive online software programs for data exchange and storage. Six authors entered the data into Review Manager 5.3.26
Dichotomous data were summarised as risk ratios with 95% confidence intervals. We used continuous data to calculate the mean difference between groups (with 95% confidence intervals) if the same measure was used in all trials, or we calculated the standardised mean difference where different outcome measures were used for the same construct in different trials. To assess the minimal clinical relevant difference, we transformed the standardised mean difference into mean difference using scales with published minimal clinical relevant difference. To our knowledge the only published minimal clinical relevant difference on scales measuring our outcomes are 6.6 points for the ADHD rating scale (ADHD symptoms, the scale ranging from 0 to 72 points)30 and 7.0 points for the child health questionnaire (quality of life, the scale ranging from 0 to 100).31 Fixed effect and random effects models were applied and discrepancies between the results investigated.
Because crossover trials are more prone to bias owing to carry-over effects, period effects, and errors in unit of analysis,32 we conducted a subgroup analysis. We analysed data from the first period in crossover trials with data from parallel trials. Our original intent was to adjust for the effect of the unit of analysis error in crossover trials by conducting a covariate analysis; however, the data were insufficient. We tested for the possibility of a carry-over effect and period effect and found similar treatment effects in the parallel group trials plus the first period of the crossover trials compared to the second period of the crossover trials. We found no statistically significant subgroup differences between the two groups but high heterogeneity in the subgroup analyses. We therefore present the analyses separately.
The treatment effect was defined as an improvement in the symptoms of ADHD, general behaviour, or quality of life. Teachers, observers, or parents rated symptoms and general behaviour. We considered these data as different outcomes and teacher rated measures as the primary outcome because symptoms of ADHD are more readily detectable in the school setting.33
We used the teacher rated symptoms of ADHD from parallel group or first period of crossover trials as our primary analysis to test the robustness of this estimate with several subgroup analyses:
Type of scale.
Dose of methylphenidate (low dose: ≤20 mg/day or ≤0.6 mg/kg/day compared to moderate or high dose: >20 mg/day or >0.6 mg/kg/day).
Design (parallel group trials compared to first phase and end of trial of crossover trials).
Drug status before randomisation—“drug naïve” (if >80% of participants were naive) compared to “previous use of drug” (>80% of participants used the drug previously).
Risk of bias (low risk of bias trials compared to high risk of bias trials).
Age—comparing trials of participants aged 2 to 6 years to those of participants aged 7 to 11 years and to those aged 12 to 18 years.
Sex—boys compared to girls.
Comorbidity—participants with comorbid disorders compared to participants without comorbid disorders.
Type of ADHD—predominantly participants with inattentive type compared to participants with combined type.
Types of raters—parents compared to observers compared to teachers.
Trials with cohort selection bias of all participants compared to trials without cohort selection bias of all participants.
Trials using fixed doses compared to trials using initial titration.
Sensitivity analyses
We conducted sensitivity analyses to ascertain whether our findings were sensitive to decisions during the review (for example, our assessment of clinical heterogeneity), the combination of both change scores and end of trial scores in one meta-analysis, and inclusion of studies with participants of IQ less than 70 or aged more than 18 years.
Consequently we undertook sensitivity analyses excluding trials using change scores,34 35 36 37 38 trials with participants of IQ less than 70,39 40 41 42 and trials including some participants aged more than 18 years.43 44
No valid method exists for combining the results of trials rated as high risk and low risk of bias.23 We performed sensitivity analyses grouping together the trials with similar classifications of bias and investigated the impact on intervention effects.
Trial sequential analysis
A meta-analysis should include a calculation of a required information size at least as large as the sample size of an adequately powered single trial to reduce the risks of random errors, taking into consideration the heterogeneity of the meta-analysis.45 46 Trial sequential analysis is a program that calculates the required information size for a meta-analysis, providing adjusted statistical thresholds for benefits, harms, or futility before the required information size is reached.46 47 48 49 Trial sequential analysis can thereby control the risks of type I and type II errors due to sparse data and repetitive testing of accumulating data.46 47 48 49 Meta-analyses not reaching the required information size are analysed with trial sequential monitoring boundaries analogous to interim monitoring boundaries in a single trial, requiring more stringent Z values to declare benefits or harms.46 If a trial sequential analysis results in insignificant findings before the required information size has been reached (no Z curve crossing of the trial sequential monitoring boundaries), the conclusion should be that more trials are needed to either accept or reject the intervention effect used for calculating the required sample size. If the cumulated Z curve enters the futility area, the anticipated intervention effect can be rejected.
For the trial sequential analysis calculations of binary outcomes we included trials with zero events by substituting zero with 0.5.46 50
For the outcomes of total number of serious adverse events and total number of non-serious adverse events, we calculated the a priori diversity adjusted required information size (that is, the number of participants required to detect or reject a specific intervention effect in the meta-analysis) on the following assumptions46 47 48 49 51: the proportion of participants in the control group with adverse events, a relative risk reduction or increase of 20% (25% for serious adverse events), a type I error of 5%, a type II error of 20%, and the observed diversity of the meta-analysis.
Quality of evidence
For each included trial, data extractors independently evaluated all risk of bias domains (listed below), resolving any disagreements by discussion. We assigned each bias domain to one of three categories: low risk of bias, uncertain risk of bias, or high risk of bias, according to the Cochrane guidelines.23 Owing to the risk of overestimation of beneficial intervention effects and underestimation of harmful intervention effects in randomised clinical trials with unclear or high risk of bias,52 53 54 55 56 57 58 we assessed the influence of the risk of bias on our results (see subgroup analyses). We used the following domains to assess the risk of bias in the included trials23 59: generation of allocation sequence, allocation of concealment, blinding of participants and staff, blinding of outcome assessors, incomplete outcome data, selective outcome reporting, and vested interest (trial was funded by parties that might have had a conflict of interest (for example, a manufacturer of methylphenidate) or there were potential conflicts of interests among authors because they had been working for companies producing or selling methylphenidate, or both). We considered trials with low risk of bias in all domains to be at low risk of bias and trials with one or more unclear or inadequate component to be at high risk of bias. For 32% (59/185) of the included trials we noted a specific type of bias occurring before randomisation. Non-responders to methylphenidate, responders to placebo, or participants who had adverse events due to the drug were excluded as a consequence of exclusion criteria or after a titration phase. Such trials have limited external validity and, to identify whether this cohort selection bias had an effect on estimates of effects, we did subgroup analyses (see above).
We assessed and graded the evidence according to the grading of recommendations assessment, development, and evaluation (GRADE) for high risk of bias, imprecision, indirectness, heterogeneity, and publication bias.60 The analyses were conducted with Review Manager 5.3 (Review Manager 2014) and the trial sequential analysis program.46 50 61
Results
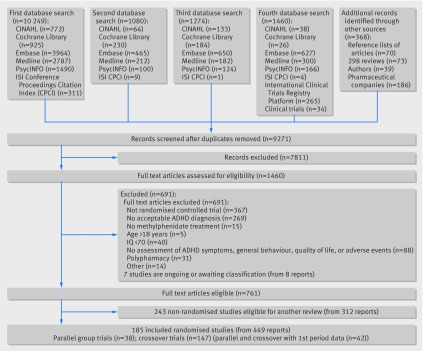
We identified 14 431 records. After removal of duplicates and irrelevant references we retrieved 1461 publications in full text for assessment of eligibility. Overall we excluded 691 publications for not meeting the inclusion criteria and eight because they were classified as either awaiting classification or as ongoing studies. In this review we included the remaining 761 publications (69 in non-English languages) describing 185 randomised clinical trials and 243 non-randomised studies (fig 1).62 When information to assess eligibility or bias was missing or data were missing or unclear we contacted the authors of the studies. Authors of 161 trials were contacted up to two times and answers were received for 92 trials.
Fig 1 Flow of studies through review
Of the 185 randomised clinical trials, 38 were parallel group (n=5111 participants) and 147 were crossover (n=7134 participants) trials, with a total of 12 245 participants. Participants of both sexes were included. Participants were aged between 3 and 18 years, but two trials included a small number of participants aged 19 to 21 years. The mean age was 9.7 years. The majority of these trials were conducted in high income countries. The median duration of treatment in the parallel group trials was 49 days (range 1-425 days, mean 75 days) and in the crossover trials was 14 days (1-56 days, mean 16 days). No parallel group trials and only six crossover trials (3.2%, 285 participants) seemed to have low risk of bias in all domains, and accordingly 179 (96.8%) trials were considered high risk of bias trials. By using GRADE, we rated the quality of evidence as being very low for all outcomes.
Symptoms of ADHD
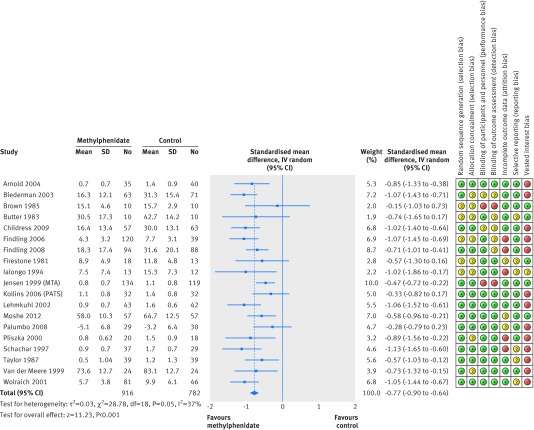
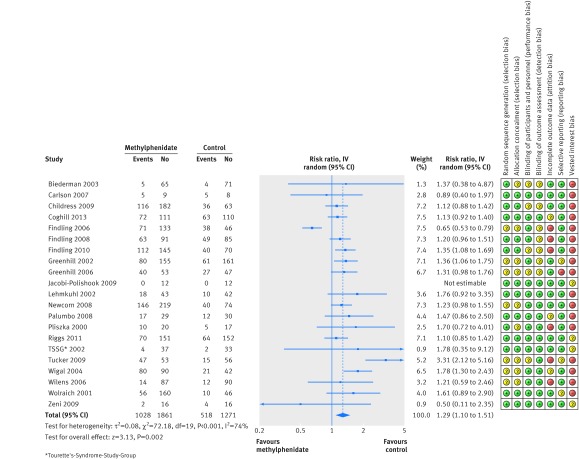
Data on symptoms of ADHD in our analyses were available from 25 parallel group trials and 74 crossover trials (53.0%) reporting on such symptoms. The results showed an effect of methylphenidate on teacher rated symptoms in the parallel group trials (standardised mean difference −0.77, 95% confidence interval −0.90 to −0.64, 19 trials, 1698 participants, fig 2). This corresponds to a mean difference of −9.6 points (95% confidence interval −13.75 to −6.38) on the ADHD rating scale, which was larger than the minimal clinical relevant difference of −6.6 points. No publication bias was detected (Egger’s test P=0.81). All the trials had high risk of bias, primarily as a result of vested interest, lack of blinding of participants, lack of outcome assessor blinding, selective outcome reporting, or selection bias. Some but not all bias risks were present in most studies. The result of the GRADE assessment was “very low quality” owing to high risks of bias and heterogeneity. The intervention effect was significantly influenced by choice of scale (test for subgroup differences, P=0.006). Long term trials had a smaller effect (standardised mean difference −0.47, 95% confidence interval −0.72 to −0.22, one trial, 253 participants) compared to short term trials (−0.81, −0.94 to −0.68, 18 trials, 1445 participants; test for subgroup difference, P=0.02). Trials including participants with previous use of drugs before randomisation resulted in a larger effect (−1.06, −1.33 to −0.79, two trials, 286 participants) compared to trials including participants naive to the drugs (−0.63, −0.94 to −0.31, four trials, 431 participants; test for subgroup difference, P=0.04). However, no significant influences on the observed treatment effects were found according to dose, trial design, cohort selection bias (trials with optimal titration, exclusion of non-responders, placebo responders, or participants with methylphenidate adverse events before randomisation) and trials with initial titration or fixed doses. One trial included in the meta-analysis reported change from baselines scores37 rather than endpoint data. Removing this trial did not change the estimate noticeably.
Fig 2 Teacher rated symptoms of attention-deficit/hyperactivity disorder in parallel group trials.
The end of last period crossover trials also showed a significant treatment effect, with a standardised mean difference of −0.93 (95% confidence interval −1.06 to −0.80, 59 trials, 5145 participants) that was not significantly influenced by risk of bias (test for subgroup difference, P=0.09). The benefit, however, was significantly greater with higher doses of methylphenidate (−0.98, −1.13 to −0.84, 36 trials, 3413 participants) compared to low doses (−0.73, −0.89 to −0.57, 42 trials, 3408 participants; test for subgroup difference, P=0.02). Three trials included participants with an IQ <70,40 41 42 but removing these did not change the estimate noticeably.
Additional subgroup analyses
Additional subgroup analyses on symptoms of ADHD in parallel group trials and first period crossover trials showed that neither age nor comorbidity significantly influenced the intervention effect. The intervention effect was significantly influenced by subtype of ADHD, with a higher intervention effect for the inattentive subtype (standardised mean difference −1.31, 95% confidence interval −1.61 to −1.01, one trial, 204 participants) compared to the combined type (0.65, −1.30 to 2.60, two trials, 559 participants; test for subgroup difference, P=0.05), but this difference was based on sparse data. We found no evidence of a carry-over effect in the crossover trials in a subgroup analysis between the first period and the second period data from four crossover trials. First period (−0.64, −0.85 to −0.44, four trials, 372 participants) and second period (−0.91, −1.18 to −0.65, four trials, 372 participants; test for subgroup difference, P=0.1).
Our analyses investigating the difference between raters showed no significant differences: teacher rated (−0.78, −0.93 to −0.63, 19 trials, 1689 participants), observer rated (−0.61, −0.87 to −0.35, nine trials, 1826 participants), and parent rated (−0.65, −0.81 to −0.50, 21 trials, 2179 participants), test for subgroup difference, P=0.37.
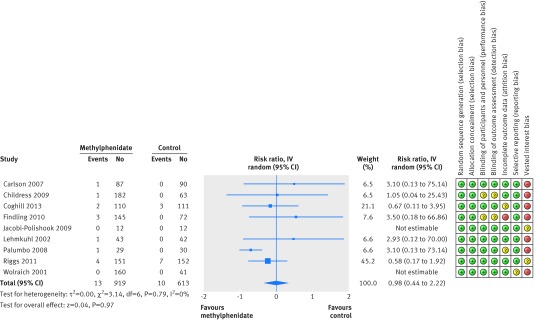
Serious adverse events
We could only include nine parallel group trials (4.9%) reporting serious adverse events. For these trials methylphenidate was not associated with an overall increase in total number of serious adverse events (risk ratio 0.98, 95% confidence interval 0.44 to 2.22, 1532 participants, fig 3). All the trials had high risk of bias owing to vested interest, incomplete outcome data, lack of blinding, and selective outcome reporting. The GRADE assessment was very low quality as a result of high risk of bias and imprecision. Eight crossover trials reported serious adverse events at the end of the last period. These trials did not seem to differ between intervention groups (risk ratio 1.62, 95% confidence interval 0.34 to 7.71, 1721 participants; I2=0%, P=0.65).
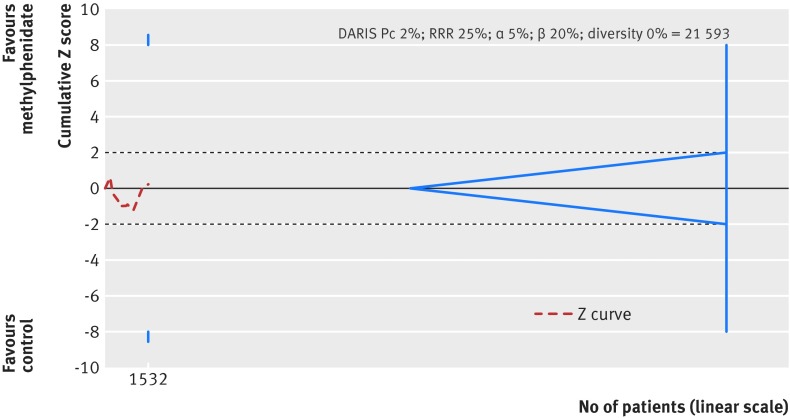
Fig 3 Serious adverse events in parallel group trials. Green=low risk of bias; yellow=uncertain risk of bias; red=high risk of bias. See Cochrane review for details of references26
We conducted trial sequential analysis on the “total serious adverse events” outcome, involving nine parallel group trials. We had planned to use a relative risk reduction of 20% but owing to too large a distance between the accrued information and the required information the program rejected to calculate and draw an interpretable figure. We therefore increased the relative risk reduction to 25%. We included trials with zero serious adverse events by substituting a constant of 0.5 for zero. We calculated the diversity adjusted required information size (DARIS) on the basis of serious adverse events in the control group of 2%; a relative risk reduction or increase in the experimental group of 25%; type I error of 5%; type II error of 20% (80% power); and diversity (D2) of 0%, the DARIS was 21 593 participants. The cumulative Z curve did not cross the conventional or trial sequential monitoring boundaries for benefit, harm, or futility (fig 4). As only less than 7% of the DARIS was accured, risks of random type II error cannot be excluded. The trial sequential analysis adjusted intervention effect is risk ratio 0.91% (95% confidence interval 0.02 to 33.2). Therefore, the total sample size in the meta-analysis of serious adverse events for 1532 participants was considerably under powered to identify a difference in serious adverse events.
Fig 4 Trial sequential analysis on total number of serious adverse events. DARIS=diversity adjusted required information size; RRR=relative risk reduction
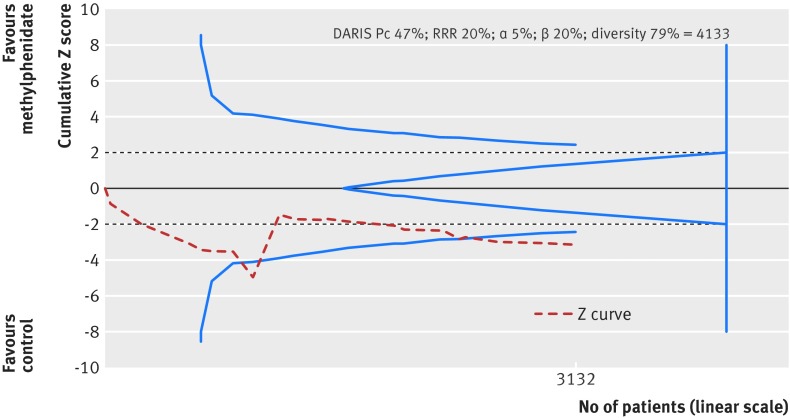
Non-serious adverse events
We could only include 26 parallel group trials (14.0%) reporting non-serious adverse events. Methylphenidate was associated with an overall risk of total number of non-serious adverse events by 29% (risk ratio 1.29, 95% confidence interval 1.10 to 1.51, 21 trials, 3132 participants, fig 5). All trials had high risk of bias owing to lack of blinding of participants, lack of outcome assessor blinding, vested interest, selective outcome reporting, and incomplete outcome data. The GRADE assessment was very low quality as a result of high risk of bias and heterogeneity. Heterogeneity was substantial between trials (τ²=0.08, χ²=61.94, df=12, P<0.001); I²=81%), which did not seem to be related to dose (test for subgroup difference between low dose and high dose methylphenidate, P=0.57). The adverse events reported over all trials included neurological, digestive, urinary, circulatory, respiratory, reproductive, skeletal, muscular, and immunological adverse events as well as physical measures such as difference in height, weight, body mass index, and vital signs. The most common non-serious adverse events were decreased appetite (risk ratio 3.66, 95% confidence interval 2.56 to 5.23, 16 trials, 2962 participants; I2=18%) and sleep problems (1.60, 1.15 to 2.23, 13 trials, 2416 participants; I2=0%).
Fig 5 Non-serious adverse events in parallel group trials. Green=low risk of bias; yellow=uncertain risk of bias; red=high risk of bias. See Cochrane review for details of references26
Sixty seven crossover trials reported non-serious adverse events at the end of the second period. For these trials methylphenidate was associated with an overall increase in total number of non-serious adverse events (risk ratio 1.33, 95% confidence interval 1.11 to 1.58, 21 trials, 2072 participants). The most common specific non-serious adverse events were decreased appetite (3.04, 2.35 to 3.94, 35 trials, 3862 participants, I2=40%) and sleep problems (1.57, 1.20 to 2.06, 31 trials, 3270 participants, I2=47%).
We conducted trial sequential analysis on the total number of non-serious adverse events outcome including 21 parallel groups or end of first period crossover trials (fig 6). The diversity adjusted required information size was calculated based on a proportion of adverse events in the control group of 47%, a relative risk reduction or increase of 20% in the experimental group, a type I error of 5%, a type II error of 20% (80% power), and a diversity (D2) of 79%. The diversity adjusted required information size was 4133 participants. The cumulative Z curve (red line) crossed the trial sequential monitoring boundary for harm (blue inward sloping line) after the seventh trial, then regressed, and crossed the boundary again after the 17th trial. Thereafter it never regressed. The trial sequential analysis adjusted risk ratio was 1.29 (95% confidence interval 1.06 to 1.56). Accordingly, we can exclude random error as a cause of the finding.
Fig 6 Trial sequential analysis on total number of non-serious adverse events. DARIS=diversity adjusted required information size; RRR=relative risk reduction
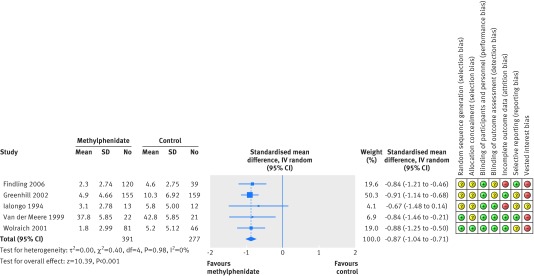
General behaviour
We could only include seven parallel group trials and 19 crossover trials (13.0%) reporting general behaviour. The standardised mean difference of teacher rated general behaviour in parallel group trials was −0.87 (95% confidence interval −1.04 to −0.71, five trials, 668 participants, fig 7). It was not possible to transform this estimate to a widely used validated scale. All the trials were high risk of bias owing to uncertainty about the method used for sequence generation and allocation of concealment, vested interest, incomplete outcome data, and selective outcome reporting. The GRADE assessment was very low quality owing to a high risk of bias and indirectness. Neither the type of scales nor the dose significantly influenced the intervention effect. The crossover trial analysis also showed a beneficial treatment effect (standardised mean difference −0.69, 95% confidence interval −0.78 to −0.60, 16 trials, 2014 participants). The intervention effect was not influenced by dose of methylphenidate. All crossover trials were considered high risk of bias.
Fig 7 Teacher rated general behaviour in parallel group trials. Green=low risk of bias; yellow=uncertain risk of bias; red=high risk of bias. See Cochrane review for details of references26
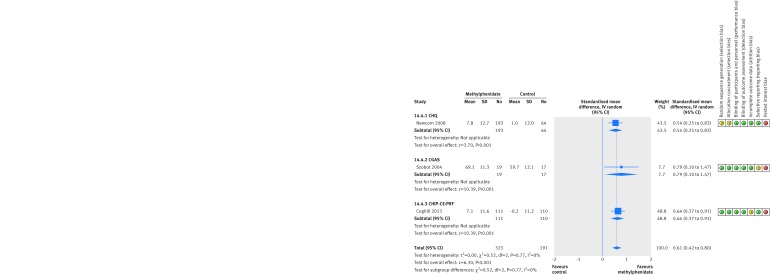
Quality of life
Only three parallel group trials (1.6%) reported quality of life. There was a small beneficial effect on quality of life (standardised mean difference 0.61, 95% confidence interval 0.42 to 0.80, three trials, 514 participants, fig 8), which corresponds on the child health questionnaire scale to a mean difference of 8.0 points (95% confidence interval 5.49 to 10.46), which is larger than the minimal clinical relevant difference of 7.0.31 However, the estimate relies on only three trials and all three had high risk of bias, primarily due to lack of blinding of participants, selective outcome reporting, and vested interests. The GRADE assessment was very low quality owing to high risk of bias and indirectness.
Fig 8 Quality of life in parallel group trials. Green=low risk of bias; yellow=uncertain risk of bias; red=high risk of bias. See Cochrane review for details of references26
Discussion
In this meta-analysis and trial sequential analysis we found that methylphenidate reduces the symptoms of ADHD in children and adolescents. We also observed a possible small beneficial effect on quality of life and general behaviour. The apparent effects of methylphenidate on both the ADHD rating scale and the child health questionnaire should be considered clinically relevant based on our predefined minimal relevant differences. However, our present results are based on trials that by GRADE are considered very low quality and may be prone to bias.
The use of methylphenidate is associated with a relatively high risk of non-serious adverse events in general. Just over a quarter of children and adolescents seemed to experience non-serious adverse events after methylphenidate treatment. Although methylphenidate has been reported to cause rare but serious cardiac events as well as sudden cardiac death,63 it did not appear to cause an increase in serious adverse events in the short term in our meta-analysis. However, the data on serious adverse events was underpowered as shown by the trial sequential analysis adjusted confidence interval and there were no data available from randomised trials on the long term incidence of such events. Our findings should be seen in the context of the low quality of the included trials owing to avoidable methodological limitations—for example, inadequate sequence generation and allocation concealment, lack of blinding, selection bias, incomplete outcome data, reporting bias, and possible bias caused by vested interest.57 64 Only six of 185 trials with a total of 183 participants seemed to be at low risk of bias in all domains. Even the trials originally considered at low risk of bias may in fact be trials with high risk of bias owing to lack of blinding despite the use of placebo, as methylphenidate gives rise to several easily recognisable adverse events that can lead to loss of blinding and influence the rating of symptoms and adverse events. We found no trials employing nocebo tablets (“active placebo”) in the controls, thus the extent of this bias cannot be assessed. Furthermore, heterogeneity might have influenced the results.
Strength and limitations of this study
This systematic review has several strengths. We developed a protocol for this review according to instructions provided in the Cochrane Handbook for Systematic Reviews of Interventions.23 Our protocol was published before we embarked on the review itself. We conducted extensive searches of relevant databases, and we requested published and unpublished data from pharmaceutical companies manufacturing methylphenidate, including Shire, Medice (represented in Denmark by HB Pharma), Janssen-Cilag, and Novartis. Two review authors, working independently, selected trials for inclusion and extracted data. Disagreements were resolved by discussion with team members. We assessed risk of bias in all trials according to recommendations provided in the Cochrane Handbook for Systematic Reviews of Interventions.23 In addition, this review meta-analysed adverse events for the same intervention and used trial sequential analysis methodology to control the risks of false positive results in meta-analysis owing to sparse data and repetitive analyses of data.46 47 50 61
It may be considered a drawback that we did not search the databases of the US Food and Drug Administration and European Medicines Agency for unpublished trials. 65The median duration of drug treatment was less than two months and few trials had a duration of more than six months. Therefore there is little that can be concluded about the benefits and harms of methylphenidate use for longer than six months. When comparing short term trials (six months or less) with long term trials (more than six months), we found that the treatment effect for teacher rated symptoms of ADHD decreased over time. This was not the case for independent assessor rated and parent rated symptoms of ADHD, where there were no significant differences between short term and long term duration of trials. We could identify no trials that examined the effect of more extended use of treatment on young people’s general behaviour. Overall, there is a lack of evidence about the long term effects of methylphenidate in children and adolescents with ADHD.
Some researchers have argued that parents’ evaluations of the symptoms of ADHD may not be as reliable as those of other raters such as teachers of preschool children66 or college students.67 One study suggested that there was inconsistency in ratings between parents.68 In the Multimodal ADHD Treatment (MTA) trial, information provided by parents was not always thought to be strong.69 However, we found no differences between different raters.
Agreements and disagreements with other studies or reviews
During the past 15 years, several reviews investigating the efficacy of methylphenidate for ADHD (with or without meta-analyses) have been published. Fifteen reviews on the efficacy of methylphenidate treatment for children and adolescents with ADHD have pooled the results of ADHD rating scales.8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 These reviews have several shortcomings, as described in our introduction. Most did not assess the risk of bias of the included studies or adverse events. Moreover, none of these reviews considered the risks of random errors. Therefore, the true estimate of the treatment is not known and information about adverse events from several randomised clinical trials is missing. All of these reviews and meta-analyses reported a large effect of methylphenidate. The meta-analysis in our review showed an effect of methylphenidate on some outcomes but because we identified that almost all of the trials have a high risk of bias, we do not know the true intervention effect. We also found a large risk of outcome reporting bias in the outcomes for both serious and non-serious adverse events
A recent Cochrane systematic review evaluated the effects of methylphenidate in adults with ADHD.70 The effect sizes across the different assessments of symptoms were similar to those found in our analyses (standardised mean difference 0.60). The authors noted that data on adverse events were limited by the short duration of the included trials.70 Despite the similar effects of methylphenidate on symptoms observed in our reviews, we have judged the quality of evidence in our own review, as well as that in Epstein 2014,71 to be lower than that of Epstein and colleagues’.
Implications for practice
The results of meta-analyses suggest that methylphenidate may improve teacher reported ADHD symptoms, teacher reported general behaviour, and parent reported quality of life among children and adolescents with a diagnosis of ADHD. However, the low quality of the underpinning evidence means that we cannot be certain of the magnitude of the effects.
Within the short follow-up periods typical of the included trials, there is some evidence that methylphenidate is associated with increased risk of non-serious adverse events, such as sleep problems and decreased appetite, but no evidence that it increases the risk of serious adverse events.
Implications for research
Better designed trials are needed to assess the benefits of methylphenidate. Because of the frequency of non-serious adverse events associated with methylphenidate, the particular difficulties for blinding of participants and outcome assessors point to the advantage of large, “nocebo tablet” controlled trials. These use a placebo-like substance that causes adverse events in the control arm that are comparable to those associated with methylphenidate. Such trials ought first to be conducted in adults with ADHD. We also acknowledge that investigators can directly carry out nocebo controlled trials in children and adolescents if they can argue that young people with ADHD are different from adults with the disorder.
Future trials should publish depersonalised individual participant data and report all outcomes, including adverse events. This will enable researchers conducting systematic reviews to assess differences between intervention effects according to sex, age, type of ADHD, presence of co-morbidities and dose. Finally, the findings highlight the urgent need for large randomised trials of non-pharmacological treatments.
Conclusions
Methylphenidate use in children and adolescents may improve the symptoms of ADHD, general behaviour, and quality of life. It does not seem to cause an increased risk of serious adverse events in the short term but was associated with a relatively high risks of non-serious adverse events. These findings should be interpreted in the light of several limitations, including the lack of blinding, outcome reporting bias, heterogeneity, and the consequent very low quality of evidence for all outcomes. More long term randomised nocebo tablet (active placebo) controlled clinical trials without risks of bias are necessary to allow firm decisions on methylphenidate treatment in children and adolescents with ADHD. We believe that nocebo controlled trials should be conducted first in adults with ADHD.
What is already known on this topic
Methylphenidate has been used for the treatment of attention-deficit/hyperactivity disorder for over 50 years and is globally the most common treatment for the disorder
Despite the widespread use of methylphenidate, no comprehensive systematic reviews of benefits and harms have been done
What this study adds
The results of meta-analyses suggest that methylphenidate may improve teacher reported ADHD symptoms, teacher reported general behaviour, and parent reported quality of life among children and adolescents with a diagnosis of ADHD
The low quality of the underpinning evidence means that the magnitude of the effects is uncertain
Within the short follow-up periods typical of the included trials, there is some evidence that methylphenidate is associated with increased risk of non-serious adverse events, such as sleep problems and decreased appetite, but no evidence that it increases the risk of serious adverse events
We thank Janus Christian Jacobsen (Copenhagen Trial Unit) for elaborating the idea of conducting this review; Trine Lacoppidan Kæstel (research librarian, Psychiatric Research Unit, Region Zealand, Denmark) for her help with the search of studies and description of the measurement scales; Lise Aagaard (University of Southern Denmark) for the advice given during the work of this review; Jesper Pedersen (Department of Childrens and Youths Psychiatry, Region Zealand, Denmark) for backing up this project; Torben Bille (Pediatric Department, Holbaek Hospital, Copenhagen, Denmark) for helping to write the protocol and for performing the selection of studies; Maria Gaardahl, Kim Boesen, Farhad Shokraneh, and Rene Spijker for helping with the translation of articles in Japanese, Italian, Turkish, Farsi and Dutch; Nadia Pedersen (Psychiatric Research Unit) for helping with finalising the review; Martina Riegl (senior medical assessor, Medicine and Healthcare products Regulatory Agency, Special Populations Unit (Paediatrics), London) for helping with data extraction and assessment of risk of bias; Jacob Riis (user experience lead, the Nordic Cochrane Centre, Copenhagen, Denmark) and Rasmus Moustgaard (senior systems architect, the Nordic Cochrane Centre, Copenhagen, Denmark) for help on issues regarding Review Manager. We thank Geraldine McDonald (coordinating editor), Joanne Wilson (managing editor), Gemma O’Loughlin (assistant managing editor), and Margaret Anderson (trials search coordinator) of the Cochrane Developmental, Psychosocial and Learning Problems Group for providing help and support. We are grateful for the advice and support of Toby Lasserson (senior editor) and David Tovey (editor in chief) of the Cochrane Central Editorial Unit.
We also thank the many authors who responded to our requests for further information on their trials, and the editors and peer reviewers of the Cochrane Group and the BMJ for helpful comments on our Cochrane review, which also influenced the wording of the present version.
ER and HBK are co-second authors on this review. This review is an abridged version of a Cochrane systematic review: Storebø OJ, Ramstad E, Krogh HB, et al. Methylphenidate for attention deficit hyperactivity disorder (ADHD) in children and adolescents. Cochrane Database Syst Rev 2015 (In press).
Contributors: OJS, CGl, MS,SR, CGr, KBR, and ES wrote the protocol. KBR developed the search strategy. OJS, ER, HK,TDN, MS, MH, FLM, SR, and KBR carried out the study selection. OJS, ER, HK, TDN, MS, SR, MH, CGJ, FLM, CMM, DG, KBR, DG, MZ, RK, and ES carried out the data extraction and evaluation of bias. OJS and CGl developed the analytical strategy. OJS, ER, HBK, MH, FLM, and CRMM entered data into RevMan. OJS, ER, HBK, MH, FLM, and CRMM conducted the statistical analysis. All authors participated in the discussion and writing of the final review. OJS is the guarantor.
Funding: This study received funding from Region Zealand Research Foundation, Psychiatric Research Unit, Region Zealand Psychiatry, Roskilde, Denmark and the Copenhagen Trial Unit, Centre for Clinical Intervention Research, Copenhagen University Hospital, Copenhagen, Denmark.
Competing interests: All authors have completed the ICMJE uniform disclosure for at www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare: CRMM receives financial research support from the government agencies: Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES) and Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq); has served as speaker to Novartis, developed educational material for Novartis; received travel awards from the Health Technology Assessment Institute (IATS), Universidade Federal do Rio Grande do Sul (UFRGS), and travel and registration support to the 4th World Congress on ADHD from the World Federation of ADHD; MZ sits on the Paediatric Medicines Expert Advisory Group at the Medicines and Healthcare Regulatory Agency, which considers applications regarding the licensing of paediatric medicines. Payment for MZ’s attendance at this meeting goes to his NHS organization. RK is currently employed by South Asian Cochrane Centre, funded by Indian Council for Medical Research, India and Effective Healthcare Research Consortium (DFID), UK. CG received funds from the Lundbeck Foundation to finance part of her Ph.D in the paediatric field on Tourette Syndrome. CG confirms that none of these funds were used to work on this review.
Ethical approval: Not required.
Data sharing: Full data are available in the version of this Cochrane review published by The Cochrane Library (www.cochrane library.com).
Transparency: The lead author (OJS) affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Cite this as: BMJ 2015;351:h5203
References
- 1.Scahill L, Schwab-Stone M. Epidemiology of ADHD in school-age children. Child Adolesc Psychiatr Clin N Am 2000;9:541-55. [PubMed] [Google Scholar]
- 2.Polanczyk GV, Salum GA, Sugaya LS, Caye A, Rohde LA. Annual research review: a meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. J Child Psychol Psychiatry 2015;56:345-65. [DOI] [PubMed] [Google Scholar]
- 3.Schmidt S, Petermann F. Developmental psychopathology: Attention Deficit Hyperactivity Disorder (ADHD). BMC Psychiatry 2009;9:58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.American Psychiatric Association. Diagnostic and statistical manual of mental disorders : DSM-5. APA; 2013.
- 5.World Health Organization. The ICD-10 classification of mental and behavioural disorders: clinical descriptions and diagnostic guidelines. WHO; 1992.
- 6.Kadesjö B. ADHD hos barn och vuxna [ADHD in children and adults]. Socialstyrelsen; 2002.
- 7.National Institute for Health and Care Excellence. Attention deficit hyperactivity disorder: diagnosis and management of ADHD in children, young people and adults. (Clinical guideline CG72.) 2008. www.nice.org.uk/guidance/cg72.
- 8.Bloch MH, Panza KE, Landeros-Weisenberger A, Leckman JF. Meta-analysis: treatment of attention-deficit/hyperactivity disorder in children with comorbid tic disorders. J Am Acad Child Adolesc Psychiatry 2009;48:884-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Charach A, Yeung E, Climans T, Lillie E. Childhood attention-deficit/hyperactivity disorder and future substance use disorders: comparative meta-analyses. J Am Acad Child Adolesc Psychiatry 2011;50:9-21. [DOI] [PubMed] [Google Scholar]
- 10.Charach A, Carson P, Fox S, Ali MU, Beckett J, Lim CG. Interventions for preschool children at high risk for ADHD: a comparative effectiveness review. Pediatrics 2013;131:e1584-e1604. [DOI] [PubMed] [Google Scholar]
- 11.Faraone SV, Biederman J, Roe C. Comparative efficacy of Adderall and methylphenidate in attention-deficit/hyperactivity disorder: a meta-analysis. J Clin Psychopharmacol 2002;22:468-73. [DOI] [PubMed] [Google Scholar]
- 12.Faraone SV, Biederman J, Spencer TJ, Aleardi M. Comparing the efficacy of medications for ADHD using meta-analysis. Med Gen Med 2006;8:4. [PMC free article] [PubMed] [Google Scholar]
- 13.Faraone SV. Using Meta-analysis to compare the efficacy of medications for attention-deficit/hyperactivity disorder in youths. P T 2009;34:678-94. [PMC free article] [PubMed] [Google Scholar]
- 14.Faraone SV, Glatt SJ. A comparison of the efficacy of medications for adult attention-deficit/hyperactivity disorder using meta-analysis of effect sizes. J Clin Psychiatry 2010;71:754-63. [DOI] [PubMed] [Google Scholar]
- 15.Hanwella R, Senanayake M, de Silva V. Comparative efficacy and acceptability of methylphenidate and atomoxetine in treatment of attention deficit hyperactivity disorder in children and adolescents: a meta-analysis. BMC Psychiatry 2011;11:176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kambeitz J, Romanos M, Ettinger U. Meta-analysis of the association between dopamine transporter genotype and response to methylphenidate treatment in ADHD. Pharmacogenomics J 2014;14:77-84. [DOI] [PubMed] [Google Scholar]
- 17.King S, Griffin S, Hodges Z, et al. A systematic review and economic model of the effectiveness and cost-effectiveness of methylphenidate, dexamfetamine and atomoxetine for the treatment of attention deficit hyperactivity disorder in children and adolescents. Health Technol Assess 2006;10:iii-146. [DOI] [PubMed] [Google Scholar]
- 18.Maia CR, Cortese S, Caye A, et al. Long-term efficacy of methylphenidate immediate-release for the treatment of childhood ADHD: a systematic review and meta-analysis. J Atten Disord 2014; published online 10 Dec. [DOI] [PubMed]
- 19.Punja S, Zorzela L, Hartling L, Urichuk L, Vohra S. Long-acting versus short-acting methylphenidate for paediatric ADHD: a systematic review and meta-analysis of comparative efficacy. BMJ Open 2013;3:e002312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Reichow B, Volkmar FR, Bloch MH. Systematic review and meta-analysis of pharmacological treatment of the symptoms of attention-deficit/hyperactivity disorder in children with pervasive developmental disorders. J Autism Dev Disord 2013;43:2435-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schachter HM, Pham B, King J, Langford S, Moher D. How efficacious and safe is short-acting methylphenidate for the treatment of attention-deficit disorder in children and adolescents? A meta-analysis. CMAJ 2001;165:1475-88. [PMC free article] [PubMed] [Google Scholar]
- 22.Van der Oord S, Prins PJ, Oosterlaan J, Emmelkamp PM. Efficacy of methylphenidate, psychosocial treatments and their combination in school-aged children with ADHD: a meta-analysis. Clin Psychol Rev 2008;28:783-800. [DOI] [PubMed] [Google Scholar]
- 23.Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions. Version 5.1.0 [updated March 2011]. www.cochrane-handbook.org.
- 24.Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 2015;4:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 2009;339:b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Storebø O, Ramstad E, Krogh H, et al. Methylphenidate for attention deficit hyperactivity disorder (ADHD) in children and adolescents. Cochrane Database Syst Rev 2015 (In press). [DOI] [PMC free article] [PubMed]
- 27.Storebø O, Pedersen N, Krogh H, et al. Methylphenidate for attention deficit hyperactivity disorder (ADHD) in children and adolescents—assessment of harms in observational studies. Cochrane Database Syst Rev 2015; (In press). [DOI] [PMC free article] [PubMed]
- 28.Storebø OJ, Rosendal S, Skoog M, et al. Methylphenidate for attention deficit hyperactivity disorder (ADHD) in children and adolescents [Protocol]. Cochrane Database Syst Rev 2012;5:CD009885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.ICH Expert Working Group. ICH harmonized tripartite guideline: guideline for good clinical practice E6(R1) 1996. http://bit.ly/1B0jeJg. [PubMed]
- 30.Zhang S, Faries DE, Vowles M, Michelson D. ADHD Rating Scale IV: psychometric properties from a multinational study as a clinician-administered instrument. Int J Methods Psychiatr Res 2005;14:186-201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rentz AM, Matza LS, Secnik K, Swensen A, Revicki DA. Psychometric validation of the child health questionnaire (CHQ) in a sample of children and adolescents with attention-deficit/hyperactivity disorder. Qual Life Res 2005;14:719-34. [DOI] [PubMed] [Google Scholar]
- 32.Curtin F, Elbourne D, Altman DG. Meta-analysis combining parallel and cross-over clinical trials. III: The issue of carry-over. Stat Med 2002;21:2161-73. [DOI] [PubMed] [Google Scholar]
- 33.Hartman CA, Rhee SH, Willcutt EG, Pennington B. Modeling Rater Disagreement for ADHD: Are Parents or Teachers Biased? J Abnorm Child Psychol 2007;35:536-42. [DOI] [PubMed] [Google Scholar]
- 34.Carlson GA, Dunn D, Kelsey D, et al. A pilot study for augmenting atomoxetine with methylphenidate: safety of concomitant therapy in children with attention-deficit/hyperactivity disorder. Child Adolesc Psychiatry Ment Health 2007;1:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Findling RL, Short EJ, McNamara NK, et al. Methylphenidate in the treatment of children and adolescents with bipolar disorder and attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry 2007;46:1445-53. [DOI] [PubMed] [Google Scholar]
- 36.Newcorn JH, Kratochvil CJ, Allen AJ, et al. Atomoxetine and osmotically released methylphenidate for the treatment of attention deficit hyperactivity disorder: acute comparison and differential response. Am J Psychiatry 2008;165:721-30. [DOI] [PubMed] [Google Scholar]
- 37.Palumbo DR, Sallee FR, Pelham WE, Bukstein OG, Daviss WB, McDermott MP. Clonidine for attention-deficit/hyperactivity disorder: I. Efficacy and tolerability outcomes. J Am Acad Child Adolesc Psychiatry 2008;47:180-8. [DOI] [PubMed] [Google Scholar]
- 38.Tucker JD, Suter W, Petibone DM, et al. Cytogenetic assessment of methylphenidate treatment in pediatric patients treated for attention deficit hyperactivity disorder. Mutat Res 2009;677:53-8. [DOI] [PubMed] [Google Scholar]
- 39.Oesterheld JR, Kofoed L, Tervo R, Fogas B, Wilson A, Fiechtner H. Effectiveness of methylphenidate in Native American children with fetal alcohol syndrome and attention deficit/hyperactivity disorder: a controlled pilot study. J Child Adolesc Psychopharmacol 1998;8:39-48. [DOI] [PubMed] [Google Scholar]
- 40.Pearson DA, Santos CW, Aman MG, et al. Effects of extended release methylphenidate treatment on ratings of attention-deficit/hyperactivity disorder (ADHD) and associated behavior in children with autism spectrum disorders and ADHD symptoms. J Child Adolesc Psychopharmacol 2013;23:337-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Smith BH, Pelham WE, Evans S, et al. Dosage effects of methylphenidate on the social behavior of adolescents diagnosed with attention-deficit hyperactivity disorder. Exp Clin Psychopharmacol 1998;6:187-204. [DOI] [PubMed] [Google Scholar]
- 42.Taylor E, Schachar R, Thorley G, Wieselberg HM, Everitt B, Rutter M. Which boys respond to stimulant medication? A controlled trial of methylphenidate in boys with disruptive behaviour. Psychol Med 1987;17:121-43. [DOI] [PubMed] [Google Scholar]
- 43.Green T, Weinberger R, Diamond A, et al. The effect of methylphenidate on prefrontal cognitive functioning, inattention, and hyperactivity in velocardiofacial syndrome. J Child Adolesc Psychopharmacol 2011;21:589-95. [DOI] [PubMed] [Google Scholar]
- 44.Szobot CM, Rohde LA, Katz B, et al. A randomized crossover clinical study showing that methylphenidate-SODAS improves attention-deficit/hyperactivity disorder symptoms in adolescents with substance use disorder. Braz J Med Biol Res 2008;41:250-7. [DOI] [PubMed] [Google Scholar]
- 45.Roberts I, Ker K, Edwards P, Beecher D, Manno D, Sydenham E. The knowledge system underpinning healthcare is not fit for purpose and must change. BMJ 2015;350:h2463. [DOI] [PubMed] [Google Scholar]
- 46.Wetterslev J, Thorlund K, Brok J, Gluud C. Trial sequential analysis may establish when firm evidence is reached in cumulative meta-analysis. J Clin Epidemiol 2008;61:64-75. [DOI] [PubMed] [Google Scholar]
- 47.Brok J, Thorlund K, Gluud C, Wetterslev J. Trial sequential analysis reveals insufficient information size and potentially false positive results in many meta-analyses. J Clin Epidemiol 2008;61:763-9. [DOI] [PubMed] [Google Scholar]
- 48.Brok J, Thorlund K, Wetterslev J, Gluud C. Apparently conclusive meta-analysis may be inconclusive—trial sequential analysis adjustment of random error risk due to repetitive testing of accumulating data in apparently conclusive neonatal meta-analysis. Int J Epidemiol 2009;38:287-98. [DOI] [PubMed] [Google Scholar]
- 49.Thorlund K, Devereaux PJ, Wetterslev J, et al. Can trial sequential monitoring boundaries reduce spurious inferences from meta-analysis? Int J Epidemiol 2009;38:276-86. [DOI] [PubMed] [Google Scholar]
- 50.Copenhagen Trial Unit. TSA trial sequential analysis. 0.9 Beta. [Computer program].Copenhagen Trial Unit 2011. http://ctu.dk/tsa/downloads.aspx.
- 51.Wetterslev J, Thorlund K, Brok J, Gluud C. Estimating required information size by quantifying diversity in random-effects model meta-analyses. BMC Med Res Methodol 2009;9:86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kjaergard LL, Villumsen J, Gluud C. Reported methodologic quality and discrepancies between large and small randomized trials in meta-analyses. Ann Intern Med 2001;135:982-9. [DOI] [PubMed] [Google Scholar]
- 53.Lundh A, Sismondo S, Lexchin J, Busuioc OA, Bero L. Industry sponsorship and research outcome. Cochrane Database Syst Rev 2012;12:MR000033. [DOI] [PubMed] [Google Scholar]
- 54.Moher D, Pham B, Jones A, et al. Does quality of reports of randomised trials affect estimates of intervention efficacy reported in meta-analysis? Lancet 1998;352:609-13. [DOI] [PubMed] [Google Scholar]
- 55.Savovic J, Jones HE, Altman DG, et al. Influence of reported study design characteristics on intervention effect estimates from randomized, controlled trials. Ann Intern Med 2012;157:429-38. [DOI] [PubMed] [Google Scholar]
- 56.Savovic J, Jones H, Altman D, et al. Influence of reported study design characteristics on intervention effect estimates from randomised controlled trials: combined analysis of meta-epidemiological studies. Health Technol Assess 2012;16:1-82. [DOI] [PubMed] [Google Scholar]
- 57.Schulz KF, Chalmers I, Hayes RJ, Altman DG. Empirical evidence of bias. Dimensions of methodological quality associated with estimates of treatment effects in controlled trials. JAMA 1995;273:408-12. [DOI] [PubMed] [Google Scholar]
- 58.Wood L, Egger M, Gluud LL, et al. Empirical evidence of bias in treatment effect estimates in controlled trials with different interventions and outcomes: meta-epidemiological study. BMJ 2008;336:601-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Gluud C, Nikolova D, Klingenberg SL. Cochrane Hepato-Biliary About the Cochrane Collaboration (Cochrane Review Groups (CRGs). Cochrane Rev Groups 2015;1(Art.No:LIVER). www.cochranelibrary.com/about/cochrane-review-groups.html.
- 60.Andrews J, Guyatt G, Oxman AD, et al. GRADE guidelines: 14. Going from evidence to recommendations: the significance and presentation of recommendations. J Clin Epidemiol 2013;66:719-25. [DOI] [PubMed] [Google Scholar]
- 61.Thorlund K, Engstrøm J, Wetterslev J, Brok J, Imberger G, Gluud C. User manual for Trial Sequential Analysis (TSA). Copenhagen Trial Unit, Centre for Clinical Intervention Research. Copenhagen, Denmark 2011;1. www.ctu.dk/tsa.
- 62.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA Statement. Open Med 2009;3:e123-e130. [PMC free article] [PubMed] [Google Scholar]
- 63.Martinez-Raga J, Knecht C, Szerman N, Martinez MI. Risk of serious cardiovascular problems with medications for attention-deficit hyperactivity disorder. CNS Drugs 2013;27:15-30. [DOI] [PubMed] [Google Scholar]
- 64.Lundh A, Sismondo S, Lexchin J, Busuioc OA, Bero L. Industry sponsorship and research outcome. Cochrane Database Syst Rev 2012;12:MR000033. [DOI] [PubMed] [Google Scholar]
- 65.Schroll JB, Bero L, Gotzsche PC. Searching for unpublished data for Cochrane reviews: cross sectional study. BMJ 2013;346:f2231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Murray DW, Kollins SH, Hardy KK, et al. Parent versus teacher ratings of attention-deficit/hyperactivity disorder symptoms in the preschoolers with Attention-Deficit/Hyperactivity Disorder Treatment Study (PATS). J Child Adolesc Psychopharmacol 2007;17:605-19. [DOI] [PubMed] [Google Scholar]
- 67.Lavigne JV, Dulcan MK, LeBailly SA, Binns HJ. Can parent reports serve as a proxy for teacher ratings in medication management of attention-deficit hyperactivity disorder? J Dev Behav Pediatri 2012;33:336-42. [DOI] [PubMed] [Google Scholar]
- 68.Caye A, Machado JD, Rohde LA. Evaluating parental disagreement in ADHD diagnosis: can we rely on a single report from home? J Atten Disord 2013; published online 4 Oct. [DOI] [PubMed]
- 69.Efstratopoulou M, Simons J, Janssen R. Concordance among physical educators’, teachers’, and parents’ perceptions of attention problems in children. J Atten Disord 2013;17:437-43. [DOI] [PubMed] [Google Scholar]
- 70.Epstein T, Patsopoulos NA, Weiser M. Immediate-release methylphenidate for attention deficit hyperactivity disorder (ADHD) in adults. Cochrane Database Syst Rev 2014;9:CD005041. [DOI] [PubMed] [Google Scholar]
- 71.Storebø O, Gluud C. Criticism to “Immediate-release methylphenidate for attention deficit hyperactivity disorder (ADHD) in adults”. Email to: T Epstein via Wiley Online Feedback form, 12 May 2015.