Abstract
Large-scale population-based imaging studies of preclinical and clinical heart disease are becoming possible due to the advent of standardized robust non-invasive imaging methods and infrastructure for big data analysis. This gives an exciting opportunity to gain new information about the development and progression of heart disease across population groups. However, the large amount of image data and prohibitive time required for image analysis present challenges for obtaining useful derived data from the images. Automated analysis tools for cardiac image analysis are only now becoming available. This paper reviews the challenges and possible solutions to the analysis of big imaging data in population studies. We also highlight the potential of recent large epidemiological studies using cardiac imaging to discover new knowledge on heart health and well-being.
Keywords: Cardiac MRI, Cardiac atlas, Anatomical models
Introduction
The burden of cardiovascular disease (CVD) is rapidly increasing due to higher prevalence of obesity, diabetes, and metabolic syndrome [1]. Our current understanding of multivariate risk factors involved in the etiology of CVD is largely due to prospective population-based research studies such as the Framingham Heart Study [2], the MONICA project [3], and the INTERHEART study [4]. These have established the now well-known major cardiovascular risk factors of hypertension, smoking, lipid profile, obesity, diabetes, and inactivity [5]. These studies demonstrate the value of population-based longitudinal studies for predicting and preventing cardiovascular disease.
Recently, non-invasive imaging has been incorporated into several large-scale prospective longitudinal studies, in order to develop predictive biomarkers derived from cardiac structural and functional measurements [6, 7•]. Longitudinal follow-up and monitoring of events enable examination of the progression of disease from sub-clinical manifestations (e.g., remodeling) to clinical symptoms, and the study of the relationship between imaging-derived biomarkers and adverse events. In particular, cardiac magnetic resonance (CMR) imaging is increasingly used in cohort-based studies, since it requires no ionizing radiation or anatomical “windows” and has high resolution and reproducibility [8–10]. CMR has a wide range of contrast mechanisms and can provide detailed information on cardiac morphology (size, shape) and function (ventricular pump function, tissue strain and torsion, regional wall motion abnormalities), flow, and microstructure [11, 12]. The combination of non-invasive imaging with epidemiological and clinical data offers a rich source of “big heart data,” which opens up new avenues of exploration to improve our understanding of the progression of sub-clinical disease across different population groups [13]. These studies therefore form a substantial part of the global move to P4 medicine (predictive, preventive, personalized, and participatory) [14] through big data informatics.
A substantial hurdle that must be overcome for this vision to be realized is the prohibitively large resource currently required for quantification of clinically meaningful parameters from the vast amounts of image information available. Current clinical practice typically requires manual assessment of the images, which is time consuming and prone to subjective bias in the measurements. Robust and accurate automated image analysis is required for objective assessment of imaging bio-markers. This review examines the challenges involved and recent steps towards this goal.
Large-Scale Cardiovascular Imaging Studies
Examples of large-scale studies which explicitly performed cardiovascular imaging for mechanistic insights into disease progression are summarized below.
Multi-Ethnic Study of Atherosclerosis
The Multi-Ethnic Study of Atherosclerosis (MESA) was designed to investigate the manifestation of sub-clinical disease and the progression to clinical symptoms in several population sub-groups in the USA (African-American, Chinese, Hispanic, and white) [15]. Initiated in 2000, MESA has followed 6814 men and women aged 45–84 years old across six centers for over 10 years. The analysis of 10 years' follow-up has recently been completed for around 3000 participants [16]. CMR was utilized to assess sub-clinical disease processes [17]. A substantial ancillary study program facilitates data sharing and collaborations.
Jackson Heart Study
The Jackson Heart Study (JHS) was designed to investigate the mechanism of cardiovascular disease in African-Americans living in the southeastern USA (Jackson, MS) [18, 19]. Overall, 5302 people aged 21–84 years participated. This high-risk group has increased mortality from cardiovascular disease as well as higher incidence of hypertension, obesity, and diabetes. Economic, sociocultural, behavioral, dietary, and physical activity measures were related with cardio-metabolic risk factors [20]. Both CT and CMR examinations were acquired in approximately 3000 participants to measure heart function and calcium scores [21].
UK Biobank
UK Biobank (UKB) is an extensive study that recruited 500, 000 people aged between 40 and 69 years in 2006–2010 from across the UK. Questionnaires, physical examinations, and biological samples have been obtained. An imaging enhancement sub-study has recently begun with the aim of imaging 6000 participants in the pilot phase [7•], with the objective of scaling up to 100,000 participants over a 5–6-year period. Imaging modalities include CMR examinations, abdominal MRI, brain MRI, carotid ultrasound, and DEXA. Data are being made available on request.
Canadian Partnership for Tomorrow Project
The Canadian Partnership for Tomorrow Project (CPTP) aims to develop a comprehensive study to understand how environment, lifestyle, and genetics contribute to chronic diseases [22]. Recently, a $16m initiative to gather detailed information from about 10,000 participants was announced (The Canadian Alliance for Healthy Hearts and Minds), including data on environments, lifestyle, and behaviors that could affect their cardiovascular health. Participants will be assessed by MRI evaluation of the brain, blood vessels, heart, and liver.
ICELAND MI
ICELAND MI is an epidemiologic cohort study of the prevalence of myocardial infarction in older individuals. A total of 936 participants were randomly selected from men and women aged 67–93 years. CMR scans were collected, including gadolinium contrast images to identify scar tissue. This study has shown that a high degree of undiagnosed myocardial infarction exists in this cohort and that CMR was able to detect infarction more readily than standard methods [23].
Framingham Offspring Study
The Framingham Offspring study [24] was initiated in 1971 as a continuation of the highly successful Framingham study. Participants undergo periodic examinations every 3–4 years including comprehensive interim history, physical examination, blood pressure, blood tests, as well as other testing on a cycle-specific basis. Of these participants, 1707 underwent CMR scans during 2002–2006 [25].
The Dallas Heart Study
The Dallas Heart Study was initiated in 2000 and designed as a single-center population-based study of multiethnic cardiovascular disease in Dallas County, TX. Of 6101 participants interviewed, 2971 received imaging examinations including cardiac MRI, electron beam CT, and dual-energy X-ray absorptiometry. Cardiac MRI revealed two to three times higher prevalence of LV hypertrophy in blacks than in whites [26].
Registries
Registries such as the EuroCMR registry [27] seek to evaluate the utility and efficacy of imaging in the clinical context. The main goal is to evaluate the prognostic potential of CMR as well as cost-effectiveness. More than 27,000 consecutive patients have been enrolled from 57 centers in 15 countries in the EuroCMR registry. Similarly, the Global CMR registry has recently been established to collate MRI patient data from around the world with 44,000 cases contributed to date.
Data Sharing Initiatives
Sharing imaging and clinical data with the wider research community is essential to the development of the field [28]. Central to this data sharing framework is a secured protection of private patient data, as required under the Health Insurance Portability and Accountability Act (HIPAA) regulations in the USA and Directive 95/46/EC in the EU. In order to facilitate data sharing, all data must be obtained with institutional review board approval and informed participant consent compatible with data sharing. Data must be de-identified and participant confidentiality and privacy must be protected so that the identity of the participants remains unknown.
Infrastructure to support data sharing has been developed by the Cardiac Atlas Project (CAP), a worldwide consortium to host large-scale cardiac image data with derived analyses and associated diagnostic information [29]. Over 3000 CMR cases have been contributed to the database from several different studies. More than 20 research groups worldwide are using this resource for various research activities, including large-scale generalization of cardiac motion for percutaneous coronary intervention, characterization of shape variation for medical device design, learning-based registration to extract morphological information, quantification of local cardiac remodeling for electromechanical simulations, and automatic identification of wall motion abnormalities.
In order to pool data from several disparate studies, any bias in the results due to imaging or analysis protocol must be removed, so that data from all studies can be compared on a level playing field. Atlas-based bias correction methods have been proposed for solving this problem [30]. Patient-specific models of heart shape and motion are used to provide a standard coordinate system, which maps the heart according to anatomical location. The shape parameters of the models give information on the shape mean and variation across the cohort, as well as the progression of remodeling due to disease or the benefits of treatment. CAP has developed methods to pool data from different sources in a standardized manner and to correct bias arising from imaging or analysis protocol. CAP is endorsed by the Society for Cardiovascular Magnetic Resonance, which maintains an upload site where cases can be contributed to the atlas project [31].
Atlas-based methods have been applied in the MESA baseline cohort to investigate the shape variation among subcohorts [32•]. Figure 1 shows the analysis pipeline. Contours derived from the core laboratory were adjusted for breath-hold misregistration and registered to a common coordinate system. Principal component analysis was used to characterize global shape distributions. After correction for height, the dominant shape component was associated with heart size. After size, the second dominant shape component was sphericity at end-diastole (13 %) and concentricity at end-systole (10 %). The resulting shape components distinguished differences due to ethnicity and risk factors with greater statistical power than traditional mass and volume indices.
Fig 1.
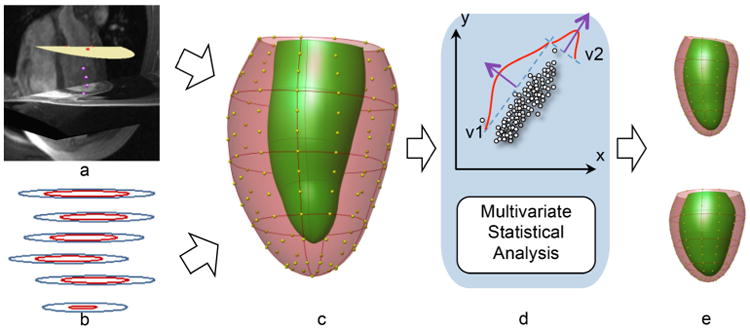
Flow chart of the atlas construction: a fiducial landmarks defined on the images (3D view from anterior), b contours drawn by the core lab, c 3D finite element model showing shape control points (yellow), d calculation of remodeling indices, e variation in “sphericity” remodeling index (upper and lower panels show ±2σ shape variation from the mean). (Modified with permission from Medrano-Gracia et al. [32•]
Challenges
With large population-based studies involving medical imaging, there is an enormous amount of data processing required. Without automated processing methods, this data mountain would be insurmountable. Crucial to the development of such methods is the availability of benchmark datasets with validated ground truth. These are essential for the validation of algorithms and objective comparison of the strengths and weaknesses of different methods. Several problem areas are considered below, with emphasis on open “challenges”: community-driven collaborative projects, often held in association with a conference, designed to enable researchers to compare and contrast different methods applied to standardized datasets with common ground truth. An index of challenges in general biomedical image analysis can be found at http://www.grand-challenge.org/, while more specialized cardiac image and modeling analysis challenges are available at http://www.cardiacatlas.org/web/guest/challenges.
Ventricular Function
Balanced steady-state free precession CMR imaging can provide the most accurate estimates of mass and volume of any imaging modality. Several automated methods have been proposed for locating the inner and outer contours of the left and right ventricles; for a review, see [33]. Common methods include graph cut [34] or level set [35]segmentation methods, and multi-atlas registration and label propagation methods [35]. Benchmarking studies are particularly useful in this area but are limited by the need for validated ground truth. Traditionally, experts manually draw contours on each image, but this is counterproductive for high-volume data due to time-consuming and painstaking processes. This has resulted in limited numbers of cases with expert ground truth.
In 2009, a left ventricular segmentation challenge was held using 45 cases from a mixed patient dataset (normal, heart failure, myocardial infarction, and hypertrophy) by using expert-drawn contours as the ground truth at end-diastolic and end-systolic frames [36]. The data are in the public domain and can be accessed directly via the Cardiac Atlas Project website. To leverage the robustness and usability of large-scale data for ventricular function benchmarking, an updated challenge was held in 2011 with more cases (200 patients with myocardial infarction) and ground truth available for all frames in the cine sequence [37]. An interesting feature of this work is the ability to update the consensus contours using statistical fusion methods. If a new dataset meets certain quality requirements, with acceptable bias and precision, the ground truth contours can be updated to incorporate this new information. This resulted in a mechanism by which researchers can continue to upload results and refine the ground truth [37]. As more groups participate, the consensus becomes more robust and less influenced by any particular contributor.
Flow
Blood flow is directly related to the morphology and function of the cardiovascular system. Accurate blood flow measurement remains a challenge because of the process involving flow velocity field mapping inside heart chambers and through the great vessels as well [38]. Flow through an image slice or within a 3D block of tissue must be analyzed by firstly segmenting the vasculature and secondly integrating the phase contrast velocity within the vessel over time [39]. Goel et al. [40] developed a method for automatically identifying the ascending and descending aorta and computing flow in phase contrast MRI acquisitions, and applied this to 1884 participants of the Dallas Heart Study. Two challenges relating to computational analysis of blood flow with MRI velocity data have made single-case benchmark data available to the community [41, 42].
Perfusion
The automated analysis of myocardial blood flow (perfusion) remains challenging, since there is no standard perfusion imaging protocol. Quantification of absolute blood flow in milliliters per gram per minute required detailed knowledge of the pulse sequence parameters, in order to correct for the non-linear relationship between contrast concentration and signal intensity [43]. There are also several methods available for quantitative analysis [44]. However, some methods have shown promising results for quantification on a pixel basis [45]. A benchmark dataset has been provided for testing motion correction algorithms in the 2014 STACOM perfusion challenge [46].
Landmark Detection
The location and motion of specific landmarks is useful for quantifying cardiac structural and functional characteristics and as a precursor for other analyses such as ventricular mass and volume quantification. For example, the location of the mitral valve provides longitudinal shortening as well as enables the base of the left ventricle to be located. A landmark detection challenge in 2012 made 200 cases with manual ground truth available for validation and benchmarking [42]. Machine learning methods show promise for landmark detection but require large datasets with manual ground truth in order to train the algorithms [47, 48].
Scar Quantification
Late gadolinium enhancement provides a robust method for quantifying the scar burden in patients with myocardial infarction [49]. A left ventricular scar identification challenge was held in 2012 [42]. The challenge made available 30 late gadolinium enhancement MRI data sets to participants for segmentation of enhanced regions from post-myocardial infarction from 15 patients and 15 pigs that had been subjected to myocardial ischemia. Ground truth was established by using manual segmentations from experienced clinical observers.
Left atrial scar burden is also important for evaluation of atrial fibrillation, both for identification of patients at risk and for the evaluation of ablation therapy. A benchmark challenge for left atrial scar burden was performed recently in association with the International Symposium of Biomedical Imaging [50].
Motion Analysis
CMR tissue tagging provides direct measures of tissue function [51]. Myocardial tissue tagging was used in a sub-set of the MESA cohort to evaluate tissue function independently of geometric pump function [52]. The Harmonic Phase method was used for analysis since this is automatic after contours enclosing the heart have been defined [53]. However, phase unwrapping errors and lack of resolution can cause problems. Feature tracking methods can provide robust estimates of global strain from untagged cine images, although regional strain estimates are more variable [54]. These methods were derived from speckle tracking algorithms designed for echo-cardiographic data [55]. All three of these methods were compared in an open challenge for motion estimation in which data from 15 volunteers and a phantom were made available for benchmarking and validation [56].
T1 Mapping
Information on myocardial cellular structure can be inferred from the local tissue T1, and non-contrast T1 mapping methods are now available [57] which give information on the extra-cellular matrix [58]. Non-contrast T1 mapping is being employed in the UK Biobank CMR extension [7•]. Pre- and post-contrast T1 maps can be used to calculate extra-cellular volume [59]. These methods are not currently standardized, but several methods have been proposed for automated analysis [60, 61].
Conclusions
Large-scale population-based studies of cardiovascular disease are increasingly utilizing non-invasive imaging methods to investigate the mechanisms behind disease development and predict future outcomes. This presents challenges for data processing due to the enormous amount of data generated. These are being met by community-driven benchmarking and validation studies, which are sharing data for the objective evaluation of analysis methods.
Acknowledgments
The Cardiac Atlas project was supported by Award Number R01HL087773 from the National Heart, Lung, and Blood Institute, NIH.
Footnotes
Compliance with Ethics Guidelines: Conflict of Interest Pau Medrano-Gracia and Avan Suinesiaputra declare that they have no conflict of interest.
Alistair A. Young and Brett R. Cowan report personal fees from Siemens Healthcare but report no overlap with the current work.
Human and Animal Rights and Informed Consent This article does not contain any studies with human or animal subjects performed by any of the authors.
Contributor Information
Pau Medrano-Gracia, Email: p.medrano@auckland.ac.nz.
Brett R. Cowan, Email: b.cowan@auckland.ac.nz.
Avan Suinesiaputra, Email: a.suinesiaputra@auckland.ac.nz.
Alistair A. Young, Email: a.young@auckland.ac.nz.
References
Papers of particular interest, published recently, have been highlighted as:
• Of importance
- 1.Murray CJ, Vos T, Lozano R, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2197–223. doi: 10.1016/S0140-6736(12)61689-4. [DOI] [PubMed] [Google Scholar]
- 2.Dawber TR, Meadors GF, Moore FE., Jr Epidemiological approaches to heart disease: the Framingham Study. Am J Public Health Nation's Health. 1951;41:279–81. doi: 10.2105/ajph.41.3.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rosamond WD, Chambless LE, Folsom AR. Survival trends, coronary event rates, and the MONICA project. Monitoring trends and determinants in cardiovascular disease. Lancet. 1999;354:864–5. doi: 10.1016/s0140-6736(05)75933-x. [DOI] [PubMed] [Google Scholar]
- 4.Rosengren A, Hawken S, Ounpuu S, et al. Association of psychosocial risk factors with risk of acute myocardial infarction in 11119 cases and 13648 controls from 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364:953–62. doi: 10.1016/S0140-6736(04)17019-0. [DOI] [PubMed] [Google Scholar]
- 5.Kannel WB, Dawber TR, Kagan A, Revotskie N, Stokes J., 3rd Factors of risk in the development of coronary heart disease—six year follow-up experience. The Framingham Study. Ann Intern Med. 1961;55:33–50. doi: 10.7326/0003-4819-55-1-33. [DOI] [PubMed] [Google Scholar]
- 6.Wong ND. Epidemiological studies of CHD and the evolution of preventive cardiology. Nat Rev Cardiol. 2014;11:276–89. doi: 10.1038/nrcardio.2014.26. [DOI] [PubMed] [Google Scholar]
- 7•.Petersen SE, Matthews PM, Bamberg F, et al. Imaging in population science: cardiovascular magnetic resonance in 100,000 participants of UK Biobank—rationale, challenges and approaches. J Cardiovasc Magn Reson. 2013;15:46. doi: 10.1186/1532-429X-15-46. Summarizes the rationale for CMR in large scale population studies. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Buechel EV, Kaiser T, Jackson C, Schmitz A, Kellenberger CJ. Normal right- and left ventricular volumes and myocardial mass in children measured by steady state free precession cardiovascular magnetic resonance. J Cardiovasc Magn Reson. 2009;11:19. doi: 10.1186/1532-429X-11-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grothues F, Moon JC, Bellenger NG, Smith GS, Klein HU, Pennell DJ. Interstudy reproducibility of right ventricular volumes, function, and mass with cardiovascular magnetic resonance. Am Heart J. 2004;147:218–23. doi: 10.1016/j.ahj.2003.10.005. [DOI] [PubMed] [Google Scholar]
- 10.Mooij CF, de Wit CJ, Graham DA, Powell AJ, Geva T. Reproducibility of MRI measurements of right ventricular size and function in patients with normal and dilated ventricles. J Magn Reson Imaging. 2008;28:67–73. doi: 10.1002/jmri.21407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Young AA, Prince JL. Cardiovascular magnetic resonance: deeper insights through bioengineering. Annu Rev Biomed Eng. 2013;15:433–61. doi: 10.1146/annurev-bioeng-071812-152346. [DOI] [PubMed] [Google Scholar]
- 12.Pitcher A, Ashby D, Elliott P, Petersen SE. Cardiovascular MRI in clinical trials: expanded applications through novel surrogate endpoints. Heart. 2011;97:1286–92. doi: 10.1136/hrt.2011.225904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hinojar R, Botnar R, Kaski JC, Prasad S, Nagel E, Puntmann VO. Individualized cardiovascular risk assessment by cardiovascular magnetic resonance. Futur Cardiol. 2014;10:273–89. doi: 10.2217/fca.13.102. [DOI] [PubMed] [Google Scholar]
- 14.Hood L, Friend SH. Predictive, personalized, preventive, participatory (P4) cancer medicine. Nat Rev Clin Oncol. 2011;8:184–7. doi: 10.1038/nrclinonc.2010.227. [DOI] [PubMed] [Google Scholar]
- 15.Bild DE, Bluemke DA, Burke GL, et al. Multi-ethnic study of atherosclerosis: objectives and design. Am J Epidemiol. 2002;156:871–81. doi: 10.1093/aje/kwf113. [DOI] [PubMed] [Google Scholar]
- 16.Bild DE, McClelland R, Kaufman JD, et al. Ten-year trends in coronary calcification in individuals without clinical cardiovascular disease in the multi-ethnic study of atherosclerosis. PLoS One. 2014;9:e94916. doi: 10.1371/journal.pone.0094916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bluemke DA, Kronmal RA, Lima JA, et al. The relationship of left ventricular mass and geometry to incident cardiovascular events: the MESA (Multi-Ethnic Study of Atherosclerosis) study. J Am Coll Cardiol. 2008;52:2148–55. doi: 10.1016/j.jacc.2008.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Harman J, Walker ER, Charbonneau V, Akylbekova EL, Nelson C, Wyatt SB. Treatment of hypertension among African Americans: the Jackson Heart Study. J Clin Hypertens (Greenwich) 2013;15:367–74. doi: 10.1111/jch.12088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Taylor HA., Jr The Jackson Heart Study: an overview. Ethn Dis. 2005;15(S6):1–3. [PubMed] [Google Scholar]
- 20.Clark CR, Ommerborn MJ, Hickson DA, et al. Neighborhood disadvantage, neighborhood safety and cardiometabolic risk factors in African Americans: biosocial associations in the Jackson Heart study. PLoS One. 2013;8:e63254. doi: 10.1371/journal.pone.0063254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Carr JJ. The revolution in risk assessment and disease detection made possible with non-invasive imaging: implications for population science. Ethn Dis. 2013;22:S1–24.7. [PubMed] [Google Scholar]
- 22.Borugian MJ, Robson P, Fortier I, et al. The Canadian Partnership for Tomorrow Project: building a pan-Canadian research platform for disease prevention. CMAJ: Can Med Assoc J=J l'Assoc Med Can. 2010;182:1197–201. doi: 10.1503/cmaj.091540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schelbert EB, Cao JJ, Sigurdsson S, et al. Prevalence and prognosis of unrecognized myocardial infarction determined by cardiac magnetic resonance in older adults. JAMA: J Am Med Assoc. 2012;308:890–6. doi: 10.1001/2012.jama.11089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wolf PA, D'Agostino RB, Belanger AJ, Kannel WB. Probability of stroke: a risk profile from the Framingham Study. Stroke; J Cerebral Circ. 1991;22:312–8. doi: 10.1161/01.str.22.3.312. [DOI] [PubMed] [Google Scholar]
- 25.Chuang ML, Gona P, Hautvast GL, et al. CMR reference values for left ventricular volumes, mass, and ejection fraction using computer-aided analysis: the Framingham Heart Study. J Magn Reson Imaging. 2014;39:895–900. doi: 10.1002/jmri.24239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Drazner MH, Dries DL, Peshock RM, et al. Left ventricular hypertrophy is more prevalent in blacks than whites in the general population: the Dallas Heart Study. Hypertension. 2005;46:124–9. doi: 10.1161/01.HYP.0000169972.96201.8e. [DOI] [PubMed] [Google Scholar]
- 27.Bruder O, Wagner A, Lombardi M, et al. European Cardiovascular Magnetic Resonance (EuroCMR) registry—multi national results from 57 centers in 15 countries. J Cardiovasc Magn Reson. 2013;15:9. doi: 10.1186/1532-429X-15-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Flanders AE. Medical image and data sharing: are we there yet? Radiographics. 2009;29:1247–51. doi: 10.1148/rg.295095151. [DOI] [PubMed] [Google Scholar]
- 29.Fonseca CG, Backhaus M, Bluemke DA, et al. The Cardiac Atlas Project—an imaging database for computational modeling and statistical atlases of the heart. Bioinformatics. 2011;27:2288–95. doi: 10.1093/bioinformatics/btr360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Medrano-Gracia P, Cowan BR, Bluemke DA, et al. Atlas-based analysis of cardiac shape and function: correction of regional shape bias due to imaging protocol for population studies. J Cardiovasc Magn Reson. 2013;15:80. doi: 10.1186/1532-429X-15-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Society of Cardiovascular Magnetic Resonance. 2012 http://www.scmr.org/Research/cap-dicom-transfer.html.
- 32•.Medrano-Gracia P, Cowan BR, Ambale-Venkatesh B, et al. Left ventricular shape variation in asymptomatic populations: the Multi-Ethnic Study of Atherosclerosis. J Cardiovasc Magn Reson. 2014;16:56. doi: 10.1186/s12968-014-0056-2. This study provides the first large scale description of heart shape variation in the asyptomatic population. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Petitjean C, Dacher JN. A review of segmentation methods in short axis cardiac MR images. Med Image Anal. 2011;15:169–84. doi: 10.1016/j.media.2010.12.004. [DOI] [PubMed] [Google Scholar]
- 34.Jolly MP, Guetter C, Lu X, Xue H, Guehring J. Automatic segmentation of the myocardium in cine MR images using deformable registration. In: Camara O, Mansi T, Pop M, Rhode K, Sermesant M, Young AA, editors. Statistical atlases and computational models of the heart imaging and modelling challenges. Springer; 2013. pp. 98–108. [Google Scholar]
- 35.Feng C, Li C, Zhao D, Davatzikos C, Litt H. Segmentation of the left ventricle using distance regularized two-layer level set approach. Med Image Comput Comput Assist Interv. 2013;16:477–84. doi: 10.1007/978-3-642-40811-3_60. [DOI] [PubMed] [Google Scholar]
- 36.Radau P, Lu Y, Connelly K, Paul G, Dick AJ, Wright GA. Evaluation framework for algorithms segmenting short axis cardiac MRI. MIDAS J. 2009;49 [Google Scholar]
- 37.Suinesiaputra A, Cowan BR, Al-Agamy AO, et al. A collaborative resource to build consensus for automated left ventricular segmentation of cardiac MR images. Med Image Anal. 2014;18:50–62. doi: 10.1016/j.media.2013.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sengupta PP, Pedrizzetti G, Kilner PJ, et al. Emerging trends in CV flow visualization. JACC Cardiovasc Imaging. 2012;5:305–16. doi: 10.1016/j.jcmg.2012.01.003. [DOI] [PubMed] [Google Scholar]
- 39.Markl M, Wallis W, Brendecke S, Simon J, Frydrychowicz A, Harloff A. Estimation of global aortic pulse wave velocity by flow-sensitive 4D MRI. Magn Reson Med. 2010;63:1575–82. doi: 10.1002/mrm.22353. [DOI] [PubMed] [Google Scholar]
- 40.Goel A, McColl R, King KS, Whittemore A, Peshock RM. Fully automated tool to identify the aorta and compute flow using phase-contrast MRI: validation and application in a large population based study. J Magn Reson Imaging. 2014;40:221–8. doi: 10.1002/jmri.24338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Camara O, Mansi T, Pop M, Rhode K, Sermesant M, Young AA. Statistical atlases and computational models of the heart. imaging and modelling challenges. 2013:2014. [Google Scholar]
- 42.Camara O, Mansi T, Pop M, Rhode K, Sermesant M, Young AA. Imaging and modelling challenges 2012. Berlin: Springer; 2013. Statistical atlases and computational models of the heart. [Google Scholar]
- 43.Jerosch-Herold M. Quantification of myocardial perfusion by cardiovascular magnetic resonance. J Cardiovasc Magn Reson. 2010;12:57. doi: 10.1186/1532-429X-12-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pack NA, DiBella EV. Comparison of myocardial perfusion estimates from dynamic contrast-enhanced magnetic resonance imaging with four quantitative analysis methods. Magn Reson Med. 2010;64:125–37. doi: 10.1002/mrm.22282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hsu LY, Groves DW, Aletras AH, Kellman P, Arai AE. A quantitative pixel-wise measurement of myocardial blood flow by contrast-enhanced first-pass CMR perfusion imaging: microsphere validation in dogs and feasibility study in humans. JACC Cardiovasc Imaging. 2012;5:154–66. doi: 10.1016/j.jcmg.2011.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.The STACOM 2014 perfusion motion correction challenge. 2014 https://www.cardiacatlas.org/web/stacom2014/moco-introduction.
- 47.Lu X, Georgescu B, Jolly MP, et al. Cardiac anchoring in MRI through context modeling. Med Image Comput Comput Assist Interv. 2010;13:383–90. doi: 10.1007/978-3-642-15705-9_47. [DOI] [PubMed] [Google Scholar]
- 48.Mahapatra D. Automatic cardiac segmentation using semantic information from random forests. Journal of digital imaging. 2014 doi: 10.1007/s10278-014-9705-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kim RJ, Fieno DS, Parrish TB, et al. Relationship of MRI delayed contrast enhancement to irreversible injury, infarct age, and contractile function. Circulation. 1999;100:1992–2002. doi: 10.1161/01.cir.100.19.1992. [DOI] [PubMed] [Google Scholar]
- 50.Karim R, Housden RJ, Balasubramaniam M, et al. Evaluation of current algorithms for segmentation of scar tissue from late gadolinium enhancement cardiovascular magnetic resonance of the left atrium: an open-access grand challenge. J Cardiovasc Magn Reson. 2013;15:105. doi: 10.1186/1532-429X-15-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Axel L, Dougherty L. MR imaging of motion with spatial modulation of magnetization. Radiology. 1989;171:841–5. doi: 10.1148/radiology.171.3.2717762. [DOI] [PubMed] [Google Scholar]
- 52.Ambale-Venkatesh B, Armstrong AC, Liu CY, et al. Diastolic function assessed from tagged MRI predicts heart failure and atrial fibrillation over an 8-year follow-up period: the multi-ethnic study of atherosclerosis. Eur Heart J Cardiovasc Imaging. 2014;15:442–9. doi: 10.1093/ehjci/jet189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Osman NF, Kerwin WS, McVeigh ER, Prince JL. Cardiac motion tracking using CINE harmonic phase (HARP) magnetic resonance imaging. Magn Reson Med. 1999;42:1048–60. doi: 10.1002/(sici)1522-2594(199912)42:6<1048::aid-mrm9>3.0.co;2-m. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Augustine D, Lewandowski AJ, Lazdam M, et al. Global and regional left ventricular myocardial deformation measures by magnetic resonance feature tracking in healthy volunteers: comparison with tagging and relevance of gender. J Cardiovasc Magn Reson. 2013;15:8. doi: 10.1186/1532-429X-15-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Helle-Valle T, Crosby J, Edvardsen T, et al. New noninvasive method for assessment of left ventricular rotation: speckle tracking echo-cardiography. Circulation. 2005;112:3149–56. doi: 10.1161/CIRCULATIONAHA.104.531558. [DOI] [PubMed] [Google Scholar]
- 56.Tobon-Gomez C, De Craene M, McLeod K, et al. Benchmarking framework for myocardial tracking and deformation algorithms: an open access database. Med Image Anal. 2013;17:632–48. doi: 10.1016/j.media.2013.03.008. [DOI] [PubMed] [Google Scholar]
- 57.Messroghli DR, Radjenovic A, Kozerke S, Higgins DM, Sivananthan MU, Ridgway JP. Modified Look-Locker inversion recovery (MOLLI) for high-resolution T1 mapping of the heart. Magn Reson Med. 2004;52:141–6. doi: 10.1002/mrm.20110. [DOI] [PubMed] [Google Scholar]
- 58.Puntmann VO, Ucar EA, Baydes RH, et al. Aortic stiffness and interstitial myocardial fibrosis by native T1 are independently associated with left ventricular remodeling in patients with dilated cardiomyopathy. Hypertension. 2014 doi: 10.1161/HYPERTENSIONAHA.114.03928. [DOI] [PubMed] [Google Scholar]
- 59.Ugander M, Oki AJ, Hsu LY, et al. Extracellular volume imaging by magnetic resonance imaging provides insights into overt and sub-clinical myocardial pathology. Eur Heart J. 2012;33:1268–78. doi: 10.1093/eurheartj/ehr481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kellman P, Wilson JR, Xue H, Ugander M, Arai AE. Extracellular volume fraction mapping in the myocardium, part 1: evaluation of an automated method. J Cardiovasc Magn Reson. 2012;14:63. doi: 10.1186/1532-429X-14-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Moon JC, Messroghli DR, Kellman P, et al. Myocardial T1 mapping and extracellular volume quantification: a Society for Cardiovascular Magnetic Resonance (SCMR) and CMR Working Group of the European Society of Cardiology consensus statement. J Cardiovasc Magn Reson. 2013;15:92. doi: 10.1186/1532-429X-15-92. [DOI] [PMC free article] [PubMed] [Google Scholar]


