Abstract
Guidelines call for healthcare organizations to provide emotional support for clinicians involved in adverse events, but little is known about these organizations seek to meet this need. We surveyed U.S. members of ASHRM about the presence, features, and perceived efficacy of their organization’s provider support program. The majority reported that their organization had a support program, but features varied widely and there are substantial opportunities to improve services. Provider support programs should enhance referral mechanisms and peer support, critically appraise the role of Employee Assistance Programs, and demonstrate their value to institutional leaders.
Introduction
Healthcare workers involved in adverse outcomes often experience deeply negative feelings such as guilt, embarrassment, self-doubt, and fear.(1–4) These individuals, often referred to as “second victims,”(3) may have reactions that persist for months and can effect health, behavior, and work performance.(5,6) For example, involvement in a harmful error can lead to difficulty sleeping, reduced job satisfaction, and anxiety that influences medical judgment.(7) For some individuals, recurrent memories of the adverse event contribute to burnout, depression, and suicidal ideation.(8,9) The ordeal of litigation further exacerbates suffering.(10) The emotional impact of adverse events on caregivers can also be an issue of patient safety. One study found an association between involvement in an error and increased self-report of errors in the following months.(11)
To address these concerns, experts and national guidelines now call for institutions to create systems to support clinicians after adverse events.(12,13) Such support programs have been conceptualized as an integral component of initiatives to improve patient safety, transparency, and Just Culture.(14) Unfortunately, organizations often fail to meet the needs of their clinicians. A large survey in the U.S. and Canada showed that 90% of physicians feel that hospitals and healthcare organizations fail to adequately support them in coping with stress associated with medical errors.(7) While the majority of these physicians reported interest in seeking counseling after a serious error, most perceived significant barriers to pursuing such support. Many of the concerns identified, such as doubts about the confidentiality of services, and difficulty taking time off from work, can be overcome with institutional commitment to building a robust provider support program with different support options.
Although most healthcare workers perceive inadequacy in the existing support systems, a few organizations have developed effective models for the care of clinicians involved in medical error.(15) For example, Medically Induced Trauma Support Services (MITSS) in Boston and the forYOU program at the University of Missouri Health Care have developed systems that are targeted to the needs of clinicians.(16,17) These groups have produced exemplary practices and tools for healthcare organizations interested in establishing programs to care for the caregiver. However, despite growing awareness about these leading programs, little is known about the prevalence and characteristics of provider support systems at U.S. healthcare facilities.
Understanding the current state of provider support programs could help to explain the dissatisfaction physicians and other clinicians feel about healthcare organizations following adverse events. Additionally, data about existing resources could help organizations, such as the American Society for Healthcare Risk Management (ASHRM), to develop targeted advocacy efforts. Risk managers are well positioned to recognize and respond to the emotional fallout from adverse events, particularly due to their role as early responders to serious adverse events. Risk managers may personally provide emotional support, and may be involved in recommending, developing, and implementing systems that help clinicians to cope and recover. Through their longitudinal interactions with clinicians involved in disclosure and litigation, risk managers may also possess valuable insight into the availability and features of existing support systems. Therefore, we undertook a national survey of the membership of ASHRM to describe the perceptions of risk managers about the characteristics of provider support programs.
Methods
Setting and survey sample
Between May 14, 2013 and July 30, 2013, invitations to participate in a confidential web survey were sent electronically to 5272 members of ASHRM. ASHRM, established in 1980, is a personal membership group of the American Hospital Association (AHA), with approximately 5,800 members at the time of the survey. ASHRM does not track the number of healthcare institutions represented by their membership. Their membership is 85% female, the majority are clinical risk managers, and 92% have worked in healthcare for over 10 years (Mary LaRusso, email communication, September 2014). Surveys were not sent to members of ASHRM who self-identified as students or who were living outside of the United States. Participation was encouraged through 3 email reminders. Respondents were also entered into a drawing to win one of four $50 gift cards.
Because more than one ASHRM members may work at a single facility, the survey requested information that might help to identify duplicate entries. Participants were asked to provide the first four letters of their facility name and the city in which it is located. We removed 60 entries representing exact city and facility matches, preferentially keeping the data entered by the participant with the greatest number of years of employment at that facility.
Survey content
The questionnaire was drafted based on information from semi-structured interviews with five experts in the fields of patient safety, risk management, and the emotional impact of involvement in adverse events. These experts included three co-authors (PIM, RH, AWW). All questions were newly developed for this study. Questions were refined through pilot testing by 12 risk managers representing nine healthcare organizations in Washington State. The questionnaire was built and administered in REDCap, a secure web-based data-capture and management instrument hosted at the University of Washington.(18) Definitions of “Adverse Event”, “Healthcare worker”, “Wellness Program”, and “Employee Assistance Program” were provided at the beginning of the instrument. We used the Institute of Medicine definition of adverse event and developed definitions of the other terms.(19) We defined a healthcare worker as “an employee or volunteer of a medical institution who is involved in patient care (e.g. physicians, nurses, therapists, pharmacists, technicians, social workers, clerks, etc.),” a wellness program as “an internal program designed to promote healthcare workers’ health and provide support, education and resources to those with emotional, behavioral or physical health concerns,” and an employee assistance program as “an employee benefit that offers confidential counseling to assist employees to address personal and work issues that might adversely impact emotional well-being and work performance.”
The questionnaire asked respondents about their training, duration of experience, and basic demographic information. Participants were queried about whether their healthcare organization had a support program for healthcare workers involved in adverse events, or if one was planned. If a program was in place or planned, the survey asked about characteristics of the program including who can access it, what referral mechanisms and triggers are used, who provides support, and how responders are trained. They were also asked to describe the funding, leadership, organization, and legal protection for the program, as well as their perception of the program’s efficacy at identifying and supporting healthcare workers. All participants, including those representing institutions without support programs, were asked about the leadership environment and the perceived interest and backing for provider support programs among relevant stakeholders.
The institutional review board of the University of Washington approved this survey. The survey was reviewed and approved without change by the ASHRM research committee.
Statistical analysis
Descriptive statistics included means and standard deviations for continuous variables and percentages for categorical variables. Categorical variables were compared using Pearson chi square, and Fisher’s exact tests as appropriate. All tests were two-tailed and a p-value less than .05 was considered significant. We intended for the survey to be exploratory and therefore did not apply a Bonferroni adjustment to correct for inflated Type-I rate. Comparisons were limited to plausible associations. Forward conditional step-wise logistic regressions were performed to model associations between predictor variables and reported program effectiveness. Respondents reported the effectiveness of their program at 1) identifying and 2) supporting providers involved in adverse events on a four-option scale. Response options were dichotomized as “Ineffective” when respondents reported their programs as “Very ineffective” or “Somewhat ineffective,” or as “Effective” when reported as “Somewhat effective” or “Very effective.” Program features and perceptions of institutional barriers to implementation and access were used as predictor variables. Each of these variables were proportions and treated as categorical in the analyses. Analyses were performed using SPSS Version 19.0 (IBM, Armonk, NY).
Results
Characteristics of respondents
Surveys were completed by 635 of the 5272 eligible ASHRM members, for an overall response rate of 12.0%. We excluded 60 respondents who represented facilities with more than one response, leaving an analytic sample of 575 individuals from unique facilities (10.9%). These individuals were 87.1% female, with a mean age of 53.4 years (Table 1). The respondents possessed considerable institutional and personal experience; the average time spent in healthcare was 28.1 years, and the average employment at their current facility averaged 12.4 years. The participating population also reported extensive professional training and certification. Nursing degrees (RN, BSN, MSN) were the most common clinical degrees, earned by 61.7% of respondents. Risk management certifications (CPHRM, ARM, LHRM) were held by more than half (56.2%) of respondents. A majority of survey participants (60.2%) reported multiple degrees and/or certifications.
Table 1.
Characteristics of 575 survey respondents regarding provider support systems
| Age | Mean years (Std Dev) | 53.4 | (8.4) |
| Gender (%, n) | Female Male |
87.1% 11.7% |
(501) (67) |
| Degrees held (%, n) | RN/BSN MBA or MHA Other Masters degrees JD MSN MD PhD |
61.7% 12.5% 12.3% 12.3% 11.8% 1.6% 0.5% |
(355) (72) (71) (71) (68) (9) (3) |
| Certifications Held (%, n) | CRHRM CPHQ ARM CPCU Other certificates or licenses |
47.3% 11.3% 6.1% 0.7% 16.9% |
(272) (65) (35) (4) (97) |
| Years worked in healthcare field | Mean (Std Dev) | 28.1 | (10.1) |
| Years worked at current facility | Mean (Std Dev) | 12.4 | (10.5) |
| Role at current facility (select all that apply) | Risk Manager Executive Clinician Lawyer Other |
82.8% 14.1% 6.4% 5.2% 21.4% |
(476) (81) (37) (30) (123) |
Responses may not sum to 100% due to rounding and non-response
Most respondents reported a primary role at their employer as a risk manager (82.8%). Others reported holding a senior leadership position, such as executive, patient safety officer, director of quality, or compliance officer (Table 1). Although the majority worked at a single facility, 9% of respondents reported responsibilities spanning multiple entities, such as affiliated hospitals, skilled nursing facilities, clinics, or corporate headquarters. Survey participants represented a variety of work environments, with the largest group (36.9%) employed at a private hospital within a healthcare network (Table 2).
Table 2.
Characteristics of 575 healthcare facilities
| Survey question | Response | Percent (n) | |
|---|---|---|---|
| Which best describes your facility type? | Private hospital in a network Private unaffiliated hospital University-based hospital Rural/Critical access hospital County or State hospital Private multispecialty group Federal or Veterans Affairs hospital Ambulatory surgery center Other |
36.9% 14.4% 12.2% 6.8% 5.7% 4.5% 0.5% 0.5% 18.3% |
(212) (83) (70) (39) (33) (26) (3) (3) (105) |
| Does your organization have a program to provide emotional support to healthcare workers after adverse events? | Yes No, but one is planned in the next year No, and there are no plans to create one Don’t know |
73.6% 7.3% 13.0% 6.1% |
(423) (42) (75) (35) |
Responses may not sum to 100% due to rounding and non-response
Provider support program prevalence
The majority (73.6%) of respondents reported that their organization had a program to provide emotional support to healthcare workers after adverse events (Table 2). In addition, 7.3% indicated that although their institution currently lacked a provider support program, they planned to initiate one in the coming year. The average age of existing programs was 12.1 years (Inter-quartile range 5–15). Among the 110 respondents (19.1%) from institutions without any provider support program, four were aware of a prior program that had been discontinued.
Characteristics of 423 institutions with provider support programs
Program scope and personnel
The respondents who represented the 423 institutions with provider support programs described diverse program characteristics with some common features. The programs described were almost all designed to be available to any healthcare worker at that institution; 94.5% were available on any patient care unit or clinical service at the institution, and 93.9% were available to employees of all professions. The 6.1% of programs that restricted access for some employees typically excluded non-clinical staff.
Programs commonly used multiple situational triggers and referral mechanisms to initiate support, but largely relied on the initiative of healthcare workers, their supervisors, and risk managers to connect the healthcare worker with support providers (Table 3). Nearly all programs reported that they facilitated support services when requested by the healthcare worker (93.6%). Approximately three quarters of programs initiated support based on the concern of risk managers and other leaders, but less than half had systems to specifically engage healthcare workers involved in litigation or an active surveillance and referral program. Although 48.7% of respondents indicated that support would be offered to any healthcare worker involved in an adverse event, automatic contact from a support team member after any adverse event was uncommon (18.2%). Telephone or pager hotlines were available at 61.5% of provider support programs.
Table 3.
Reported characteristics of 423 provider support programs
| Survey question | Response | Percent of respondents selecting “Yes” |
|---|---|---|
| “Select the situations in which support is offered to a healthcare worker (Select all that apply)”
| ||
| If the healthcare worker requests it | 93.6% (396) | |
| If a risk manager or another leader feels it is warranted | 75.9% (321) | |
| If a healthcare worker is involved in an adverse event, regardless of whether or not they request support or appear to need it | 48.7% (206) | |
| If the healthcare worker is named as a defendant in a lawsuit | 47.3% (200) | |
| If a healthcare worker’s responses to a screening instrument used to detect distress indicate that it is warranted | 18.4% (78) | |
| Other | 5.4% (23) | |
|
| ||
| “What mechanisms are available for healthcare workers to access support? (Select all that apply)”
| ||
| Self referral | 95.5% (404) | |
| Department leader or unit manager referral | 79.1% (335) | |
| Risk manager referral | 69.7% (295) | |
| Telephone or pager hotline | 61.5% (260) | |
| Impromptu peer referral | 36.9% (156) | |
| Automatic referral (e.g. support team contacts healthcare workers after any adverse event | 18.2% (77) | |
| Active surveillance by peers trained to look for distressed healthcare workers | 13.7% (58) | |
| Other | 3.3% (14) | |
|
| ||
| “Who provides support for healthcare workers? (Select all that apply)”
| ||
| Employee Assistance Program (EAP) employees | 89.6% (379) | |
| Risk managers | 54.1% (229) | |
| Pastoral care staff | 46.6% (197) | |
| Human resources/Personnel office | 38.8% (164) | |
| Clinical support providers (MD or PhD) | 37.6% (159) | |
| Social workers | 34.8% (147) | |
| Peers trained in providing support | 21.3% (90) | |
| Support groups | 10.6% (45) | |
| Other | 9.0% (38) | |
|
| ||
| “Where is your healthcare worker support program located within the organizational structure of your healthcare institution (Select all that apply)”
| ||
| Employee Assistance Program (EAP) | 90.1% (381) | |
| Risk management | 27.9% (118) | |
| Wellness program | 25.8% (109) | |
| Quality improvement/Patient Safety | 13.5% (57) | |
| Nursing/Patient Care Services | 13.2% (56) | |
| Medical director or executive leadership office | 12.1% (51) | |
| Specific clinical department (e.g. Internal Medicine or Psychiatry) | 10.6% (45) | |
| Claims management | 8.7% (37) | |
| Profession liability insurer outside your institution | 8.7% (37) | |
Support providers at the 423 institutions with support programs varied in their professional background (Table 3), although the participation of Employee Assistance Program (EAP) staff was widespread (89.6%). Risk managers also played a prominent role, providing support at 54.1% of healthcare facilities. At 14.2% of facilities, EAP personnel were the only support providers available, and another 9.0% of facilities relied exclusively on a combination of risk managers and EAP. At 38.8% of facilities, training on how to provide support was available, whereas most respondents either reported they didn’t know if such training was available (40.4%) or confirmed it was not available (20.8%). Only a minority of respondents reported having a manual or guide for providing emotional support (14.4%).
A majority of respondents (66.0%) reported that their facility’s program was prepared to support groups of healthcare workers as well as individuals, although a substantial minority (21.7%) replied “don’t know.” A majority of respondents (65.0%) also reported that their program had a mechanism to arrange time away from clinical service for healthcare workers involved in an adverse event, although 21.7% answered “don’t know” about the availability of that function. A minority of survey participants could identify the model on which their program was developed. Those who reported the model most often indicated that the program was developed internally (29.8%), or with components of internal and external models (12.3%). Commonly cited external models included Critical Incident Stress Management, Medically Induced Trauma Support Services (MITSS), and the forYOU program at University of Missouri Health Care.
Program Administration
The most common administrative home within the healthcare institution’s organizational structure was “EAP” (90.1%), although respondents often identified additional departments that partnered with EAP (Table 3). When asked “who leads the program?”, the most common response was “Don’t know” (32.6%), followed by “program leader or director” (31.7%), and “executive champion” (12.3%). “Other” leadership was identified by 94 respondents (22.2%), representing a variety of individuals in human resources, pastoral care, social work, risk management, EAP, and outside contractors. The survey asked respondents to indicate all of the ways the support program was funded. Most identified a component funded by EAP (78%), followed by liability insurance coverage, volunteer effort from existing personnel, and facility funds (each 13.7%). Facility funds predominantly came from human resources (8.8%) and risk management (2.6%), although a few respondents reported support from grant funding (1.2%) or funding at personal cost to the employee (2.8%). Most respondents were not knowledgeable about the specific annual budget for the program at their facility. Seven respondents provided specific amounts, ranging from $0 to $50,000.
When asked to describe how the healthcare worker support program at their institution is designed to be confidential, the most common response was that it was protected when provided by an EAP (83.9%). Other mechanisms included protection by invoking provider-patient relationship when a licensed healthcare provider is involved (35.5%), attorney-client privilege with involvement of defense counsel (28.8%), work-product privilege through a professional liability insurer program (18.7%), adoption as part of a hospital or group-based quality-improvement program (16.8%) or guarantees that use of the program will not be shared with the employer when provided by peers (11.3%).
Provider support program efficacy and maintenance
Over half of respondents from the 423 organizations with provider support programs perceived that their program was somewhat (49.9%) or very (18.2%) effective at identifying healthcare workers in emotional distress after involvement in an adverse event. Respondents from programs with EAP only were less likely than those from programs with other support providers to report effective identification of healthcare workers in distress (63.6% vs. 83.5%, p=0.001). Most respondents perceived that their program was somewhat (47.3%) or very (26.5%) effective at providing support and somewhat (42.8%) or very (29.6%) effective at helping staff return to work after an adverse event.
Nearly two thirds of respondents (63.8%) acknowledged at least one barrier to maintaining a program for healthcare worker support at their institution. The most common challenges were: funding (27.2%), lack of clinical leaders to serve as peer support personnel (22.2%), lack of buy-in by executive leadership (17.0%), and uncertainty about best practices (14.9%). Approximately three fourths of respondents (78.7%) identified at least one barrier that they believed would prevent healthcare workers from accessing support at their institution. Barriers included “concern that it won’t be kept confidential” (54.4%), “concern that they might be judged negatively by colleagues” (50.1%), “taking time away from work (44.2%), “the belief that support will not be effective” (40.9%), and “concern that their support history would be placed in their permanent record” (30.5%).
Characteristics of 42 institutions with provider support programs in development
Data regarding the 42 facilities planning to create a provider support program within the next year were limited by respondents’ lack of certainty about institutional plans in approximately a third of cases. Nonetheless, notable differences emerged in comparison with existing programs. Compared with established programs, planned programs were more likely to report that they will make training available for support providers (76.2% vs. 38.8%, p<0.001), incorporate active peer surveillance (42.9% vs. 13.7%, p<0.001) and automatic contact by support teams (45.2% vs. 18.2%, p<0.001), and use a screening tool for distress (38.1% vs. 18.4%, p=0.005). Compared with existing programs, programs in planning were less likely to be administered by EAP (19% vs. 90.1%, p<0.001), and more likely to base their design on an externally developed model (40.5% vs. 29.8%, p<0.001) such as MITSS or forYOU. Planned programs were more likely than existing programs to provide support through peers (54.8% vs. 21.3%, p<0.001) and support groups (23.8% vs. 10.6%, p<0.001).
Among the 42 respondents representing provider support programs in development, 40 (95.2%) identified at least one barrier to initiating the planned program. The most common barriers included funding (54.8%), uncertainty about best practices (50%) and a lack of clinical leaders to serve as support providers (33.3%).
Characteristics of 110 institutions without provider support programs or plans to create one
Respondents from 110 institutions indicated their organization lacked a provider support programs and had no plans to create one, or reported they were unsure if one existed. Respondents from these institutions perceived variable interest among local stakeholders for establishing a program to support healthcare workers. Respondents perceived high levels of support among nurses, risk managers, and patient safety officers, believing that about three-quarters were “somewhat” or “very” interested in such a program, (nurses 74.5%, risk managers 73.6%, and patient safety officers 65.5%). Respondents perceived the lowest levels of interest among executives and physicians, believing that less than half of these groups were somewhat or very interested in a program (executives 40.0%, physicians 41.8%).
At the 110 facilities without an identified provider support program, approximately half of respondents believed that executive leaders were somewhat or very aware of the emotional impact of adverse events on healthcare workers (52.7%). However, they perceived that a minority of leaders (30.0%) were at least somewhat committed to establishing a program for provider support. The majority (57.3%) of survey participants themselves reported low familiarity with the National Quality Forum’s “Care for the Caregiver” best practice that recommends implementation of a provider support program. When asked about the barriers to initiating a provider support program, the most common responses were: funding (66.4%), buy-in by executive leadership (50.0%), lack of clinical leaders to serve as peer support personnel (47.3%), and uncertainty about how to initiate or organize a program (45.5%).
Features associated with the perception of support program success
Using forward conditional step-wise logistic regression, we identified features associated with the perception that the program was reported as somewhat or very effective at identifying healthcare workers in emotional distress. The significant variables related to specific access mechanisms and barriers, types of support providers, confidentiality, and buy-in by leaders (Table 4). Fewer variables were associated with the perception that the program was reported as at best somewhat ineffective or at least somewhat effective at providing support, but also centered on access mechanisms, support providers, and leadership buy-in (Table 4).
Table 4.
Step-Wise Regression Models Predicting Perception of Program Efficacy in two domains
| Response 1: Program is somewhat or very effective at identification of healthcare workers in distress because of involvement in an adverse event
| ||
|---|---|---|
| Variable | Odds Ratio (95% CI) | P Value |
| Mechanisms to access support include: “Department leader or unit manager referral” | 4.04 (2.04 – 8.00) | <0.001 |
| How support is designed to be confidential: “Protected by work product privilege through a professional liability insurer provider support program” | 3.64 (1.19 – 11.14) | 0.024 |
| Support providers include: “Risk Managers” | 2.07 (1.09 – 3.94) | 0.027 |
| Support is offered if: “A HCW is involved in AE, regardless of whether they request support or appear to need it” | 2.23 (1.20 – 4.15) | 0.011 |
| Barriers to HCWs accessing support include: “Belief that support will not be effective” | 0.53 (0.29 – 0.99) | 0.046 |
| Barriers to HCWs accessing support include: “Concern that they might be judged negatively by colleagues” | 0.50 (0.26 – 0.95) | 0.036 |
| Barriers to maintaining the program include: “Buy-in by executive leadership” | 0.32 (0.17 – 0.62) | 0.001 |
| Response 2: Program is somewhat or very effective with regard to provision of support for healthcare workers in emotional distress
| ||
|---|---|---|
| Variable | Odds Ratio (95% CI) | P Value |
| HCW support program location within the organizational structure: “QI/Patient Safety” | 5.64 (1.27 – 25.06) | 0.023 |
| Mechanisms to access support include: “Department leader or unit manager referral” | 4.28 (2.17 – 8.42) | <0.001 |
| Barriers to initiating the program include: “Buy-in by executive leadership” | 0.41 (0.19 – 0.89) | 0.025 |
| Barriers to initiating the program include: “A lack of clinical leaders to serve as peer support personnel” | 0.36 (0.17 – 0.77) | 0.008 |
Abbreviation: Healthcare Worker (HCW), Adverse Event (AE), Quality Improvement (QI)
Discussion
Healthcare workers commonly experience significant distress after adverse events,(7) with potentially serious consequences for their wellbeing, patient safety, and institutions. National guidelines call for healthcare institutions to emotionally support affected clinicians, but little is known about how institutions attempt to meet this need. Our study sheds light on the prevalence and characteristics of U.S. provider support programs. We found that although approximately three quarters of responding healthcare organizations have some form of program, they vary widely in structure and staffing and many lacked important elements recommended by national standards. If this finding is generalizable, it indicates that many support programs require redesign to meet the needs of suffering clinicians. In addition, the absence of any formalized support program at a quarter of U.S. hospitals suggests a substantial deficit in assistance for coping with stressful adverse events. Improving existing support programs and establishing programs where they are absent represent urgent opportunities for U.S. healthcare leaders,(20) who have identified physician wellness as a “missing quality indicator”.(21)
In addition, existing support programs described in our study rarely employ processes to contact and engage all clinicians who may be attempting to cope with stressful adverse events. This matters because of the general reluctance of clinicians to seek assistance. Relying on clinicians to initiate communication with support services is likely to limit the benefit of existing programs to a minority of those in need. Prior studies show that physicians perceive multiple practical barriers to accessing support services after involvement in medical errors.(7,20) It is disheartening that respondents to our survey were more likely to perceive the same barriers to accessing support (concerns about confidentiality, efficacy, and judgment by colleagues) than physicians surveyed nine years earlier. Although comparisons may be limited by differences between physicians and risk managers, the finding suggests that little progress has been made during that time and points to an urgent need for solutions based on culture reform and enhanced referral systems. Our findings highlight the need for institutions to widely adopt improvements such as referrals by watchful department leaders and reaching out to support to all clinicians after adverse events, regardless of whether support appears necessary. Engaging institutional leaders is another essential step; lack of “buy-in” from executive leaders was frequently cited as a barrier to obtaining adequate support for suffering clinicians.
Underutilization also has the pernicious effect of allowing leaders to mistakenly conclude that low rates of use indicate that existing support is effective or even unnecessary. To counter this misperception, healthcare organizations should establish systems to quantify, track, and promote provider support service use. It is encouraging that nearly all of the programs described were designed to support the full array of healthcare workers and departments at their institution. This inclusivity suggests a useful platform for expanding the use of systems to actively contact clinicians who may require services but do not voluntarily seek them.
We found widespread utilization of EAP as a means of supporting clinicians, sometimes as the sole means to meet provider support needs. Although EAP may offer diverse benefits to employees, there are disadvantages to relying on EAP services in the aftermath of adverse events. We found that an EAP functioning alone was associated with lower perceived success at identifying distressed healthcare workers. One reason for this lack of perceived efficacy might be low rates of utilization; prior studies show that only 29% of physicians would seek support from an EAP.(20) The low appeal of EAP may relate to a lack of tailoring to the needs of healthcare workers involved in adverse events, a lack of relevant training for EAP staff, or the use of non-clinician support providers who may lack credibility with healthcare workers.
Because EAP services are typically outsourced and may be located off-site, they are unlikely to include the peer support that has become a cornerstone of leading programs.(15,20) EAP services also may not coordinate effectively with on-site quality improvement, risk management, and other referral sources. Conversely, we found that support programs organized by the quality improvement or patient safety department, rather than an EAP, were associated with greater perceived efficacy. It is reassuring that only 19% of programs-in-development plan to rely on an EAP, whereas more than half will use peer support, reflecting an emerging consensus that in-house peer supporters offer a greater ability to identify and respond to staff needs relative to EAP.(15) For those healthcare organizations that currently rely on EAP, leaders should critically assess EAP utilization, capabilities, and integration.
The commitment and backing of institutional leaders are key to ensuring the development and sustainability of a robust provider support program. However, across the board, respondents cited financing as a barrier to implementing provider support programs. As organizations face significant fiscal challenges in today’s healthcare environment, risk managers should emphasize the return on investment from provider support programs to win the support of executive leaders. Healthcare organizations experience significant costs when a physician or nurse leaves work due to the emotional impact of an adverse event or burnout. In 2004, the average cost of losing a physician was estimated to be $123,000 in recruiting fees ($153,859 in 2014 currency) and $2M in lost revenues ($2.5M in 2014).(22) The cost of replacing a medical/surgical or specialty nurse was estimated to be $47,403 ($59,296 in 2014) and $85,197 ($106,572 in 2014), respectively.(23) As physician shortages increase in some specialties, and chronic nursing shortages persist, strategies to minimize turnover become even more valuable. Even when workers do not leave, distress resulting from adverse events has the potential to worsen productivity, quality, and safety. Leaders should be engaged to create an understanding that funding provider support services represents a strategy to both protect human capital and to enhance the culture of safety.
The majority of respondents felt that provider support programs at their institution were at least somewhat successful at supporting clinicians after adverse events. Although we lack corresponding data from the same institutions regarding healthcare worker’s perceptions, this result does not align with prior studies of physicians, who overwhelmingly reported inadequate support.(7) This potential disconnect highlights the need for program evaluation metrics based on surveys of healthcare workers and more intensive services for those who are still struggling despite initial support.
Respondents confirmed prior reports that healthcare workers’ concerns about lack of confidentiality are a barrier to seeking provider support.(7) Leaders can help to address this barrier, but should seek legal counsel about options for preserving confidentiality given the variability among state laws.(24) Some organizations may structure programs as part of quality improvement activities protected under state and federal laws. Other organizations, including professional liability insurers, may protect programs by treating a clinician’s event report as notification in anticipation of litigation. Finally, some organizations may opt out of a formal structure for confidentiality protection and minimize the risk of discoverability by assuming the clinician will discuss only their feelings as opposed to the facts surrounding the adverse event while excluding any documentation of the encounter. Describing the program as being based on a coaching model may avoid the stigma of receiving mental healthcare,(20) particularly in light of credentialing and reappointment applications requesting information about whether a provider has sought mental healthcare. Utilizing risk managers as peer supporters may complicate efforts to address healthcare workers’ concerns about confidentiality, as clinicians may perceive a conflict of interest with risk managers’ duties to investigate adverse events. The provider support protocol can include a description such as the following:
“The Peer Support Program relies on volunteer clinician members, retained as consultants to the Claims Department, who are trained to contact members by telephone to offer short-term, confidential, emotional support, coaching, and resources following report of an adverse event to the Claims Department. Reported events are notification in anticipation of litigation. Peer Support Consultants do not review medical records or provide clinical feedback or opinions. No documentation is maintained regarding the content of discussion. These activities are part of [FACILITY’s] Quality Improvement Plan and must be kept confidential. The trained provider support staff and providers and staff participants are bound by the terms of [cite relevant state law], and shall not be permitted or required to testify in any civil action as to information learned in any Provider Support activity.”(25)
The above description can be tailored for provider support programs adopted as part of a facility’s quality improvement program.#
Our study has important limitations. First, the low response rate indicates that the work could be vulnerable to non-response bias. However, it is reassuring that the basic demographics of our respondents (age, years in healthcare, and job description) are similar to those of the overall ASHRM membership. Second, the respondent population is heterogeneous; the fact that 18.4% of respondents described their place of employment as “other” may mean the results include ASHRM members who do not represent healthcare facilities, such as insurance companies. Because many insurers have begun to invest in provider support programs for their insured, they remain an important population to include in analysis. Additionally, the presence of multiple “other” facility names beginning with “St” or “Sain” suggests that many faith-based hospital systems did not identify with the available facility descriptions. Third, the survey population may not have been familiar with all details of the provider support program at their institution. Fourth, results may have been affected by social desirability bias, in particular with respect to perceptions of support program efficacy at facilities that rely heavily on risk managers to provide support. Fifth, our ability to draw firm conclusions about programs in development is limited by the possibility that the programs may change by the time they are fully implemented. Sixth, our analysis of factors associated with perceived effectiveness was exploratory and should be confirmed with further studies. Finally, we did not survey the recipients of support about their experiences, which would have allowed for direct correlation between program features and outcomes; we used respondent opinions of efficacy as a surrogate that may be inaccurate.
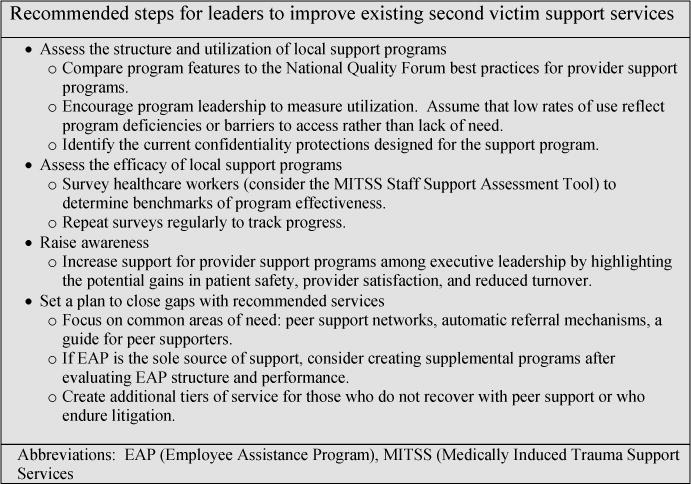
Despite these limitations, this is the first and largest study of its kind. The novel information presented is valuable for risk managers and ASHRM because it highlights the ongoing need for action at both the local and national level to advance care for caregivers involved in adverse events. Our results demonstrate a need for healthcare leaders to carefully scrutinize the structure and performance of their provider support systems. Significant opportunities remain to create metrics centered on the needs of healthcare workers and to accelerate adoption of known best practices, such as peer support programs.
Figure 1.
Acknowledgments
We wish to acknowledge Geri Amori and Mary LaRusso for their coordination of the generous logistical support provided by ASHRM.
Funding: Agency for Healthcare Research and Quality (Grant R18HS019531), and funding for REDCap through National Institutes of Health (UL RR025014). The funding sources had no role in the design, conduct, or reporting of the study or in the decisions to submit the manuscript for publication.
Footnotes
Author Contributions: Study conception and design: All
Acquisition of data: White
Analysis and interpretation of data: White, Brock
Drafting of manuscript: White, Brock, McCotter, Hofeldt
Critical Revision: All
Financial Disclosure: None
Contributor Information
Andrew A. White, Assistant Professor of Medicine, Department of Medicine, University of Washington School of Medicine, Seattle, Washington.
Doug Brock, Associate Professor, Department of Family Medicine and MEDEX Northwest, University of Washington School of Medicine, Seattle, Washington.
Patricia I. McCotter, Director, Patient Safety Innovations and Provider Support, Physicians Insurance A Mutual Company/Experix, Seattle, WA.
Ron Hofeldt, Director, Physician Affairs, Physicians Insurance A Mutual Company/Experix, Seattle, WA.
Hanan H. Edrees, Doctoral candidate, Department of Health Policy & Management, Johns Hopkins Bloomberg School of Public Health, Baltimore, Maryland.
Albert W. Wu, Professor of Health Policy and Management and Medicine, Johns Hopkins Bloomberg School of Public Health, Baltimore, Maryland.
Sarah Shannon, Associate Professor of Nursing, Department of Biobehavioral Nursing and Health Systems, University of Washington, Seattle, Washington.
Thomas H. Gallagher, Professor, Department of Medicine and Department of Bioethics & Humanities, University of Washington School of Medicine, Seattle, Washington.
References
- 1.Newman MC. The emotional impact of mistakes on family physicians. Arch Fam Med. 1996;5(2):71–75. doi: 10.1001/archfami.5.2.71. [DOI] [PubMed] [Google Scholar]
- 2.Christensen JF, Levinson W, Dunn PM. The heart of darkness: the impact of perceived mistakes on physicians. J Gen Intern Med. 1992;7(4):424–431. doi: 10.1007/BF02599161. [DOI] [PubMed] [Google Scholar]
- 3.Wu A. Medical error: the second victim. The doctor who makes the mistake needs help too. BMJ. 2000;320(7237):726–727. doi: 10.1136/bmj.320.7237.726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wu AW, Folkman S, McPhee S, Lo B. Do house officers learn from their mistakes? JAMA. 1991;265(16):2089–2094. [PubMed] [Google Scholar]
- 5.Scott SD, Hirschinger LE, Cox KR, McCoig M, Brandt J, Hall LW. The natural history of recovery for the healthcare provider “second victim” after adverse patient events. Qual Saf Health Care. 2009;18(5):325–330. doi: 10.1136/qshc.2009.032870. [DOI] [PubMed] [Google Scholar]
- 6.Schelbred AB, Nord R. Nurses’ experiences of drug administration errors. J Adv Nurs. 2007;60(3):317–324. doi: 10.1111/j.1365-2648.2007.04437.x. [DOI] [PubMed] [Google Scholar]
- 7.Waterman AD, Garbutt J, Hazel E, et al. The emotional impact of medical errors on practicing physicians in the United States and Canada. Jt Comm J Qual Patient Saf. 2007;33(8):467–476. doi: 10.1016/s1553-7250(07)33050-x. [DOI] [PubMed] [Google Scholar]
- 8.West CP, Tan AD, Habermann TM, Sloan JA, Shanafelt TD. Association of Resident Fatigue and Distress With Perceived Medical Errors. JAMA. 2009;302(12):1294–1300. doi: 10.1001/jama.2009.1389. [DOI] [PubMed] [Google Scholar]
- 9.Shanafelt TD, Balch CM, Dyrbre L, et al. Suicidal Ideation Among American Surgeons. Arch Surg. 2011;146(1):54–62. doi: 10.1001/archsurg.2010.292. [DOI] [PubMed] [Google Scholar]
- 10.Balch CM, Oreskovich MR, Dyrbre LN, et al. Personal Consequences of Malpractice Lawsuits on American Surgeons. J Am Coll Surg. 2011;213(5):657–667. doi: 10.1016/j.jamcollsurg.2011.08.005. [DOI] [PubMed] [Google Scholar]
- 11.West CP, Huschka MM, Novotny PJ, et al. Association of Perceived Medical Errors with Resident Distress and Empathy. JAMA. 2006;296(9):1071–1078. doi: 10.1001/jama.296.9.1071. [DOI] [PubMed] [Google Scholar]
- 12.National Quality Forum. Safe Practices for Better Healthcare – 2010 Update: A Consensus Report. Washington, DC: National Quality Forum; 2010. [Google Scholar]
- 13.Conway J, Federico F, Stewart K, Campbell MJ. Respectful management of serious clinical adverse events. Cambridge, Massachesetts: Institute for Healthcare Improvement; 2010. [Google Scholar]
- 14.Denham CR. TRUST : The 5 Rights of the Second Victim. J Patient Saf. 2007;3(2):107–119. [Google Scholar]
- 15.Pratt S, Kenney L, Scott SD, Wu AW. How to Develop a Second Victim Support Program : A Toolkit for Health Care Organizations. Jt Comm J Qual Patient Saf. 2012;38(5):235–240. doi: 10.1016/s1553-7250(12)38030-6. [DOI] [PubMed] [Google Scholar]
- 16.Scott SD, Hirschinger LE, Cox KR, et al. Caring for our own: deploying a systemwide second victim rapid response team. Jt Comm J Qual Patient Saf. 2010;36(5):233–240. doi: 10.1016/s1553-7250(10)36038-7. [DOI] [PubMed] [Google Scholar]
- 17.MITSS (Medically Induced Trauma Support Services) MITSS Tools: Tools for Building a Clinician and Staff Support Program. 2014 [website] http://www.mitsstools.org/tool-kit-for-staff-support-for-healthcare-organizations.html. Accessed July 27, 2014.
- 18.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap) – A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Institute of Medicine. To Err is Human: Building a Safer Health System. Washington, D.C: National Academy Press; 1999. [Google Scholar]
- 20.Hu YY, Fix ML, Hevelone ND, et al. Physicians’ Needs in Coping With Emotional Stressors The Case for Peer Support. Arch Surg. 2012;147(3):212–217. doi: 10.1001/archsurg.2011.312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wallace J, Lemaire J, Ghali W. Physician wellness: a missing quality indicator. Lancet. 2009;374(9702):1714–1721. doi: 10.1016/S0140-6736(09)61424-0. [DOI] [PubMed] [Google Scholar]
- 22.Misra-Hebert A, Kay R, Stoller J. A Review of Physician Turnover: Rates, Causes, and Consequences. Am J Med Qual. 2004;19(2):56–66. doi: 10.1177/106286060401900203. [DOI] [PubMed] [Google Scholar]
- 23.Hunt ST. Nursing Turnover: Costs, Causes, and Solutions. 2009 [website] http://www.uexcel.com/resources/articles/NursingTurnover.pdf. Accessed July 27, 2014.
- 24.de Wit ME, Marks CM, Natterman JP, Wu AW. Supporting second victims of patient safety events: shouldn’t these communications be covered by legal privilege? J Law Med Ethics. 2013;41(4):852–858. doi: 10.1111/jlme.12095. [DOI] [PubMed] [Google Scholar]
- 25.Physicians Insurance A Mutual Company. Internal Policy – Peer Support Program. 2014 [Google Scholar]


