Abstract
Background
The relationship between intake of fruits and vegetables (F/V) during young adulthood and coronary atherosclerosis later in life is unclear.
Methods and Results
We studied participants of the Coronary Artery Risk Development in Young Adults (CARDIA) study, a cohort of young, healthy black and white individuals at baseline (1985–1986). Intake of F/V at baseline was assessed using a semi-quantitative interview administered diet history and CAC was measured at year 20 (2005–2006) using computed tomography. We used logistic regression to adjust for relevant variables and estimate the adjusted odds ratios (OR) and 95% confidence intervals (CI) across energy-adjusted, sex-specific tertiles of total servings of F/V per day. Among our sample (n=2,506), the mean (SD) age at baseline was 25.3 (3.5) years and 62.7% were female. After adjustment for demographics and lifestyle variables, higher intake of F/V was associated with a lower prevalence of CAC: OR (95% CI) =1.00 (reference), 0.78 (0.59–1.02), and 0.74 (0.56–0.99), from the lowest to the highest tertile of F/V, p-value for trend <0.001. There was attenuation of the association between F/V and CAC after adjustment for other dietary variables but the trend remained significant: OR (95% CI): 1.00 (reference), 0.84 (0.63–1.11), and 0.92 (0.67–1.26), p-value for trend <0.002].
Conclusions
In this longitudinal cohort study, higher intake of F/V during young adulthood was associated with lower odds of prevalent CAC after 20 years of follow-up. Our results reinforce the importance of establishing a high intake of F/V as part of a healthy dietary pattern early in life.
Keywords: Epidemiology, Nutrition, Diet, Coronary Disease, Atherosclerosis, Imaging
Introduction
Healthy lifestyle choices are essential for the prevention of cardiovascular disease (CVD). A dietary pattern high in fruits and vegetables (F/V) in middle-aged adults has been associated with reduced rates of coronary heart disease (CHD), stroke, and CVD mortality.1–6 Atherosclerotic plaque formation, the hallmark of CVD, is known to begin early in life,7 but if and how F/V intake in young individuals impacts this process is unclear.
Population based lifestyle interventions hold significant potential to reduce rates of CVD and will be increasingly relied upon as the US model of healthcare changes.8,9 Middle-aged adults, often motivated by the near-term risk of a CVD event, frequently adopt healthier lifestyle patterns, including dietary changes, though they may already have developed a significant atherosclerotic plaque burden. Adopting a healthy diet earlier in life holds the potential to have a greater impact on CVD risk reduction but evidence supporting this concept is lacking. Knowledge of the relationship between dietary patterns in young adults and future CVD is essential as public health strategies are developed to target the most efficacious dietary interventions.
Coronary artery calcium (CAC), a direct marker of coronary atherosclerosis, is a strong predictor of future CHD events and a powerful CVD risk stratification tool.10,11 CAC has been shown to predict mortality independent of age and even minimal amounts of coronary calcification (CAC score 1–10) have been associated with a substantial increase in mortality compared to individuals with no CAC.12,13
The Coronary Artery Risk Development in Young Adults (CARDIA) Study provides a unique opportunity to analyze the association between dietary factors during young adulthood and atherosclerosis later in life. In this study, we sought to define the relationship between dietary intake of F/V during young adulthood and the prevalence of CAC after 20 years of follow-up.
Methods
Study Design and Population
The CARDIA study is a prospective cohort designed to evaluate the progression of cardiovascular risk factors and CVD. Thorough descriptions of the study design and procedures have been previously published.14–16 Briefly, in 1985–1986, 5,115 black and white men and women, aged 18–30 years, were recruited from 4 urban sites across the United States: Birmingham, Alabama; Chicago Illinois, Minneapolis, Minnesota; and Oakland, California. Participants have been followed for more than 25 years with detailed demographic and clinical data, including anthropometric and laboratory measures, as well as assessments of subclinical atherosclerosis. The retention rate for the surviving cohort was 72% at year 20. Examination protocols were reviewed and approved by institutional review boards at each site, and written informed consent was obtained from every participant at each examination.
Of the 3,549 individuals with follow-up data from the year 20 visit, 541 participants were excluded for the following reasons: 422 were missing CAC scores, 4 were missing F/V intake at year 0, 1 underwent a female-to-male transgender conversion, 113 were missing covariate data, and 1 was a significant outlier for reported F/V intake. Of the remaining 3,008 participants, we excluded 502 individuals due to extreme reported energy intake (<800 or >4,000 kcal/d), leaving 2,506 participants for the primary analysis.
Assessment of diet and F/V intake
Diet was assessed at year 0 and year 20 using the interviewer-administered CARDIA Diet History.17,18 Interviewers asked questions about dietary consumption of various food groups within the past month. A positive response would trigger additional information-gathering questions. For example, a positive response to the question “Do you eat fresh fruit?” would trigger the additional questions “Which fruits from the following list do you eat and how often” and “How much do you typically eat”. The fruits and vegetables included in the diet history are listed in Table 1. Data on consumption of frozen and canned fruits and vegetables was also collected. Potatoes, including fried potatoes, were not included as vegetables, nor were legumes which consistent of dried beans, dried peas, and lentils. All reported foods were grouped according to the nutritional data system for research, 2005 food groups (modified United States department of agriculture food grouping scheme) developed at the nutrition coordinating center at the University of Minnesota.17,18 Reported foods were assigned to one of 165 subgroups within 9 major food groups, including each of fruit and vegetables. Intake of each food group was calculated as the sum of the servings a food in each food group was eaten per day. In addition, standard serving sizes for all foods were calculated based on gram weight information obtained from the nutritional data system for research software program and the United States department of agriculture pyramid servings database.17,18 Therefore, for each participant, the number of servings for each reported food was calculated based on a standard serving (gram weight given the form of the food). Food-group intake was calculated as servings per day. All servings of fruits and vegetables were combined into a single category to determine the servings of F/V per day. This value was then energy adjusted to a dietary intake of 2,000 kcal/d.
Table 1.
Fruits and vegetables included in the interviewer-administered CARDIA Diet History.
| Vegetables | Fruits |
|---|---|
| Artichokes | Apples |
| Asparagus | Apricots |
| Avocado | Bananas |
| Beans (Green, Lima, Wax) | Berries |
| Beets | Cherries |
| Broccoli | Figs |
| Brussel Sprouts | Grapefruit |
| Cabbage | Grapes |
| Carrots | Kiwi |
| Celery | Kumquats |
| Cauliflower | Melons |
| Eggplant | Nectarines |
| Greens | Oranges |
| Mushrooms | Peaches |
| Okra | Pears |
| Olives | Pineapples |
| Onions | Plums |
| Parsnips | Strawberries |
| Peas | Tangerines |
| Peppers | |
| Rutabagas | |
| Seaweed | |
| Sprouts | |
| Spinach | |
| Squash | |
| Sweet Potatoes | |
| Tomatoes | |
| Turnips |
Assessment of CAC
CAC was assessed using computed tomography (CT) and analyzed as either present or absent (CAC=0 vs CAC>0) for all individuals who underwent CAC scanning at the year 20 follow-up. The CT protocol at the year 20 exam consisted of 2 sequential non-contrast CT scans performed on electron beam CT scanners (Chicago and Oakland centers: Imatron C-150, GE Healthcare, Waukesha, Wisconsin) or multidetector CT scanners (Birmingham center: GE Lightspeed, GE Healthcare, Waukesha, Wisconsin; Minneapolis center: Volume Zoom, Siemens Medical Solutions, Erlangen, Germany). The methodology and validity of the CAC assessment process has been previously described in detail.19,20 Scans were read by a trained reader who was blinded to the participant’s characteristics. The CAC score was totaled from the amount of measured plaque in the epicardial coronary arteries using the modified Agatston method to account for slice thickness.21 The presence of CAC was defined as having a positive, non-zero score, using the average of the two scans. Discordant scans were infrequent (3.6%) and independently adjudicated by two CARDIA investigators.
Other covariates
Information on age, gender, race, education, cigarette smoking, alcohol intake, and physical activity was obtained by using a structured interview and self-administered questionnaires. Participants reported highest grade of school completed and education was classified into 5 categories (less than high school, high school graduate, some college, college degree, and post-graduation education). Income was not collected at baseline but was collected at the year 5 follow-up and was categorized into 3 categories (<$25,000, $25,000–$50,000, and >$50,000). Smoking was classified as never, former, or current smoker. Alcohol consumption was analyzed in 5 categories based on self-reported consumption of alcoholic drinks per week (<1, 1–2, 3–6, 7–14, 14+). Physical activity was self-reported and classified into 5 categories based on the question, “Compared to other people your age and sex, what number would you choose for rating your physical activity during the past year: 1=physically inactive, 2, 3=moderately active, 4, 5=very active”. Height and weight were measured at baseline and the year 20 exam and recorded to the nearest 0.5cm and 0.2 kg, respectively. Body mass index (BMI), in kg/m2, was derived from these measures. Seated blood pressure was obtained after 5 minutes of rest with a random-zero sphygmomanometer at year 0 and an automated device (Omron) at year 20. Three blood pressure measurements were taken and the average of the 2nd and 3rd measurements was used as the measured blood pressure. Patients were asked to fast for 12 hours before blood was collected for measurement of serum lipids and glucose.
Statistical Analysis
Baseline characteristics were determined according to sex-specific tertiles of energy adjusted intake of F/V as calculated from the baseline exam. Baseline characteristics are described as mean (SD) or median (range) for continuous variables based on normality and number (percentage) for categorical variables. We dichotomized CAC into zero and non-zero scores given the strong predictive value of a CAC score of zero and the increased CVD risk for individuals with even minimal CAC.13
Logistic regression was used to calculate prevalence odds ratios (OR) for CAC across energy adjusted, sex-specific tertiles of F/V intake. We built sequential models based on a priori knowledge. Model 1 was adjusted for age and race. Model 2 was adjusted for age, race, BMI, smoking, alcohol, physical activity, income, center and education. We obtained a p-value for linear trend by creating a new variable that was assigned the median F/V intake in each tertile and fitting the new variable into the regression model. We analyzed this association in the total sample as well as in a sex-stratified approach. We chose to include the sex-stratified analysis because the prevalence of CAC is known to vary by sex,10 and two previous studies suggested the relationship between F/V intake and CHD varies according to sex.2,3 Given that the prevalence of CAC (16.6%) was somewhat higher than what is typically considered a “rare outcome”, we also performed a relative risk regression model to estimate adjusted prevalence ratios of CAC with corresponding 95% confidence interval.
We performed several additional analyses to try and isolate the effect of F/V intake during young adulthood from other dietary factors by including F/V intake at the year 20 exam as well as other dietary factors from the baseline exam. We chose additional dietary variables based on a prior knowledge and clinical relevance including dairy, nuts, legumes, eggs, fish, beef, refined grain bread, refined grain pasta, cakes/cookies/doughnuts, fried potatoes, salt intake, sugar sweetened soft drinks, and frequency of fast food intake for further exploration of confounding. Finally, we included potential mediators in a model including systolic blood pressure, low-density lipoprotein (LDL) and high-density lipoprotein (HDL) cholesterol, and fasting blood sugar as measured at the year 20 follow-up.
Results
The mean age of the 2,506 participants at baseline was 25.3 (SD 3.5) years, and 1,571 (62.7%) were women. The baseline characteristics of the women and men in the study according to energy-adjusted tertiles of F/V intake are shown in Table 2. Women and men with higher intake of F/V were more likely to be older, white, more educated, and less likely to smoke. The median intake of F/V adjusted to a 2,000-kcal/d diet was 8.9 servings per day in women in the top tertile compared to 3.3 servings per day in the bottom tertile. F/V intake was slightly lower in men (7.2 servings per day in the top tertile versus 2.6 servings per day in the bottom tertile). Baseline dietary intake of the women and men in the study according to energy-adjusted tertiles of F/V intake are shown in Table 3. Individuals in our study with a high intake of F/V had a higher intake of fish, and lower intake of refined carbohydrates, salt, and fast food compared to those with low intake of F/V.
Table 2.
Baseline characteristics of women and men in CARDIA according to energy-adjusted tertiles of fruit and vegetable intake.
| Women | Fruit/Vegetable consumption in servings/day per 2000 kcal | |||
|---|---|---|---|---|
| Characteristics | Q1 (median, range) | Q2 | Q3 | P for trend |
| 3.3 (0.3–4.3) | 5.4 (4.3–6.7) | 8.9 (6.7–25.8) | ||
| N | 523 | 524 | 524 | |
| Age (y) | 24.6 ±3.8 | 25.3 ± 3.5 | 25.8 ± 3.4 | <0.01 |
| Race (% white) | 41.3 | 57.6 | 64.3 | <0.01 |
| Current smoker (%) | 31.4 | 22.9 | 18.5 | <0.01 |
| Alcohol consumption (%) | 0.21 | |||
| None | 53.0 | 44.5 | 42.4 | |
| 1–2/week | 15.1 | 17.8 | 25.6 | |
| 3–6/week | 19.1 | 23.3 | 18.9 | |
| 1-<2/day | 8.4 | 9.9 | 10.7 | |
| 2+/day | 4.4 | 4.6 | 2.5 | |
| Education | <0.01 | |||
| Less than high school | 10.5 | 5.2 | 2.1 | |
| High school | 38.4 | 22.9 | 18.5 | |
| Some college | 33.5 | 34.7 | 33.8 | |
| 4 years of college | 12.4 | 26.7 | 30.2 | |
| Post-grad | 5.2 | 10.5 | 15.5 | |
| Income (%) | <0.01 | |||
| <25,000 | 47.8 | 30.4 | 30.7 | |
| 25,000–<50,000 | 35.9 | 41.5 | 37.6 | |
| 50,000+ | 16.4 | 28.0 | 31.7 | |
| Physical Activity Rating | <0.01 | |||
| 1: % physically inactive | 12.2 | 8.8 | 6.3 | |
| 2 | 15.9 | 15.7 | 15.3 | |
| 3: % moderately active | 42.6 | 42.2 | 38.9 | |
| 4 | 16.1 | 18.9 | 24.6 | |
| 5: % very active | 13.2 | 14.5 | 14.9 | |
| BMI (kg/m2) | 24.7 ± 5.9 | 23.9 ± 4.8 | 24.1 ± 4.8 | 0.06 |
| LDL Cholesterol (mg/dL) | 111.7 ± 30.9 | 109.5 ± 30.6 | 106.1 ± 28.8 | <0.01 |
| HDL Cholesterol (mg/dL) | 54.5 ± 12.7 | 56.6 ± 12.6 | 57.6 ± 12.7 | <0.01 |
| Glucose (mg/dL) | 80.3 ± 12.1 | 81.2 ± 18.4 | 80.6 ± 7.1 | 0.68 |
| Systolic blood pressure (mm Hg) | 106.7 ± 9.5 | 106.2 ± 9.7 | 105.4 ± 9.1 | 0.02 |
| Energy (kcal/d) | 2215 ± 710 | 2117 ± 693 | 1955 ± 640 | <0.01 |
| Men | Fruit/Vegetable consumption in servings/day per 2000 kcal | |||
| Characteristics | Q1 (median, range) | Q2 | Q3 | P for trend |
| 2.6 (0.6–3.4) | 4.4 (3.5–5.4) | 7.2 (5.4–22.8) | ||
| N | 311 | 312 | 312 | |
| Age (y) | 25.1 ± 3.5 | 25.5 ± 3.5 | 25.7 ± 3.2 | 0.03 |
| Race (% white) | 59.8 | 62.5 | 70.5 | <0.01 |
| Current smoker (%) | 29.3 | 21.5 | 18.3 | <0.01 |
| Alcohol consumption (%) | 0.45 | |||
| None | 28.0 | 26.6 | 34.6 | |
| 1–2/week | 13.5 | 13.5 | 16.7 | |
| 3–6/week | 22.8 | 24.7 | 22.8 | |
| 1-<2/day | 21.5 | 21.8 | 14.1 | |
| 2+/day | 14.2 | 13.5 | 11.9 | |
| Education | <0.01 | |||
| Less than high school | 8.7 | 7.7 | 3.2 | |
| High school | 23.8 | 20.2 | 18.9 | |
| Some college | 36.7 | 30.1 | 26.9 | |
| 4 years of college | 16.7 | 25.0 | 35.3 | |
| Post-grad | 14.2 | 17.0 | 15.7 | |
| Income (%) | 0.01 | |||
| <25,000 | 31.3 | 31.8 | 28.0 | |
| 25,000–<50,000 | 45.2 | 38.8 | 35.2 | |
| 50,000+ | 23.5 | 29.4 | 36.9 | |
| Physical Activity Rating | <0.01 | |||
| 1: % physically inactive | 5.8 | 4.2 | 3.5 | |
| 2 | 15.1 | 11.9 | 11.5 | |
| 3: % moderately active | 40.8 | 38.1 | 36.9 | |
| 4 | 18.7 | 27.6 | 25.6 | |
| 5: % very active | 19.6 | 18.3 | 22.4 | |
| BMI (kg/m2) | 24.2 ±3.7 | 24.6 ± 3.3 | 24.1 ± 3.2 | 0.66 |
| LDL Cholesterol (mg/dL) | 111.2 ± 31.2 | 113.4 ± 30.9 | 112.6 ± 31.7 | 0.58 |
| HDL Cholesterol (mg/dL) | 49.2 ± 12.4 | 49.6 ± 12.6 | 49.5 ± 10.6 | 0.76 |
| Glucose (mg/dL) | 83.8 ± 9.2 | 83.5 ± 10.7 | 84.2 ± 9.4 | 0.60 |
| Systolic blood pressure (mm Hg) | 114.8 ± 10.4 | 113.7 ± 9.7 | 114.9 ± 10.4 | 0.90 |
| Energy (kcal/d) | 2755 ± 722 | 2685 ± 701 | 2630 ± 741 | 0.03 |
Table 3.
Baseline dietary characteristics of women and men in CARDIA according to energy-adjusted tertiles of fruit and vegetable intake.
| Women | Fruit/Vegetable consumption in servings/day per 2000 kcal | |||
|---|---|---|---|---|
| Characteristics* | Q1 (median, range) | Q2 | Q3 | P for trend |
| 3.3 (0.3–4.3) | 5.4 (4.3–6.7) | 8.9 (6.7–25.8) | ||
| N | 523 | 524 | 524 | |
| Dairy | 2.8 ± 2.0 | 2.7 ± 2.0 | 2.3 ± 1.5 | <0.01 |
| Nuts | 0.5 ± 1.1 | 0.5 ± 1.0 | 0.6 ± 0.9 | 0.12 |
| Legumes | 0.2 ± 0.3 | 0.2 ± 0.3 | 0.4 ± 1.0 | <0.01 |
| Eggs | 0.5 ± 0.5 | 0.4 ± 0.4 | 0.4 ± 0.4 | <0.01 |
| Fish | 0.8 ± 1.1 | 0.9 ± 1.1 | 1.1 ± 1.3 | <0.01 |
| Beef | 1.5 ± 2.4 | 1.2 ± 1.8 | 1.0 ± 1.6 | 0.01 |
| Bread/rolls-refined grain | 2.4 ± 1.9 | 1.7 ± 1.3 | 1.1 ± 1.1 | <0.01 |
| Pasta-refined grain | 0.5 ± 0.5 | 0.4 ± 0.5 | 0.4 ± 0.4 | <0.01 |
| Cakes, cookies, doughnuts | 0.5 ± 0.7 | 0.4 ± 0.4 | 0.3 ± 0.4 | <0.01 |
| Fried potatoes | 0.3 ± 0.3 | 0.2 ± 0.3 | 0.2 ± 0.3 | <0.01 |
| Frequency salt use at home (%) | <0.01 | |||
| Never | 7.7 | 8.6 | 15.3 | |
| Sometimes | 26.0 | 37.9 | 39.7 | |
| Often | 20.8 | 20.3 | 20.9 | |
| Almost Always | 45.6 | 33.1 | 24.1 | |
| Sweetened soft drinks | 1.2 ± 1.7 | 0.6 ± 1.0 | 0.4 ± 0.7 | <0.01 |
| Fast food (times/month) | <0.01 | |||
| ≤2/month | 27.3 | 34.9 | 53.9 | |
| 3–5/month | 26.7 | 27.0 | 21.0 | |
| 6–11/month | 14.0 | 16.2 | 9.5 | |
| 12+/month | 32.1 | 22.0 | 15.5 | |
| Men | Fruit/Vegetable consumption in servings/day per 2000 kcal | |||
| Characteristics* | Q1 (median, range) | Q2 | Q3 | P for trend |
| 2.6 (0.6–3.4) | 4.4 (3.5–5.4) | 7.2 (5.4–22.8) | ||
| N | 311 | 312 | 312 | |
| Dairy | 3.3 ± 2.1 | 3.2 ± 3.7 | 2.8 ± 1.9 | 0.02 |
| Nuts | 0.6 ± 0.9 | 0.7 ± 1.0 | 0.9 ± 1.4 | 0.01 |
| Legumes | 0.2 ± 0.3 | 0.2 ± 0.3 | 0.3 ± 0.7 | <0.01 |
| Eggs | 0.7 ± 0.7 | 0.7 ± 0.8 | 0.6 ± 0.6 | 0.07 |
| Fish | 0.8 ± 1.3 | 1.0 ± 1.3 | 1.2 ± 1.5 | <0.01 |
| Beef | 1.9 ± 1.7 | 1.7 ± 1.2 | 1.3 ± 1.2 | <0.01 |
| Bread/rolls-refined grain | 3.1 ± 2.0 | 2.5 ± 1.8 | 1.7 ± 1.6 | <0.01 |
| Pasta-refined grain | 0.5 ± 0.5 | 0.6 ± 0.5 | 0.6 ± 0.8 | 0.03 |
| Cakes, cookies, doughnuts | 0.6 ± 0.7 | 0.6 ± 0.6 | 0.4 ± 0.5 | 0.03 |
| Fried potatoes | 0.3 ± 0.3 | 0.3 ± 0.4 | 0.3 ± 0.4 | 0.12 |
| Frequency salt use at home (%) | <0.01 | |||
| Never | 8.3 | 13.0 | 18.0 | |
| Sometimes | 40.7 | 37.8 | 42.3 | |
| Often | 25.2 | 30.6 | 21.3 | |
| Almost Always | 25.8 | 18.6 | 18.4 | |
| Sweetened soft drinks | 1.2 ± 1.4 | 0.8 ± 1.1 | 0.5 ± 0.8 | <0.01 |
| Fast food (times/month) | <0.01 | |||
| ≤2/month | 23.2 | 25.4 | 39.1 | |
| 3–5/month | 20.7 | 21.8 | 28.7 | |
| 6–11/month | 14.8 | 21.8 | 28.7 | |
| 12+/month | 41.3 | 35.5 | 16.6 | |
Dietary variables are reported in servings per day unless specified otherwise
In an age and race-adjusted model analyzed according to sex-specific tertiles, F/V intake was inversely associated with prevalent CAC and this association persisted and remained statistically significant after adjustment for BMI, smoking, alcohol, physical activity, income, center and education (Table 4). The correlation between F/V intake at baseline and year 20 was modest (Spearman r-value 0.33, p<0.0001). Updating F/V intake at year 20 did not appreciably alter the results [OR (95% CI): 1.00 (reference), 0.76 (0.57–1.02), and 0.73 (0.53–1.00), p-value for trend across tertiles <0.001].
Table 4.
Adjusted prevalence odds ratios (95% CI) for CAC at the year 20 exam according to energy-adjusted, sex-specific tertiles of servings of F/V per day at the baseline exam in CARDIA.
| Total (n=2,506) |
|||||
|---|---|---|---|---|---|
| Tertiles of F/V |
CAC Cases |
Model 1 | Model 2 | Model 3 | Model 4 |
| T1 | 158/834 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| T2 | 131/836 | 0.71 (0.55–0.93) | 0.78 (0.59–1.02) | 0.76 (0.57–1.02 | 0.84 (0.63–1.11) |
| T3 | 128/836 | 0.65 (0.50–0.85) | 0.74 (0.56–0.99) | 0.73 (0.53–1.00) | 0.92 (0.67–1.26) |
| P for linear trend | <0.001 | <0.001 | <0.001 | 0.002 |
Model 1 is adjusted for age and race.
Model 2 is adjusted for age, race, body mass index, smoking, alcohol, physical activity, income, center, and education.
Model 3 is adjusted for the variables in model 2 as well as intake of fruits and vegetables at year 20.
Model 4 is adjusted for the variables in model 2 as well as multiple dietary variables assessed at baseline including intake of dairy, nuts, legumes, eggs, fish, beef, refined grain bread, refined grain pasta, cakes/cookies/doughnuts, fried potatoes, salt intake, sugar sweetened soft drinks, and frequency of fast food intake.
Abbreviations: CI – Confidence Interval, CAC – Coronary Artery Calcium, F/V – Fruits and Vegetables, CARDIA – Cardiac Artery Risk Development in Young Adults
There was attenuation of the association between F/V and CAC after adjustment for other dietary factors that might be associated with CAC development (dairy, nuts, legumes, eggs, fish, beef, refined grain bread, refined grain pasta, cakes/cookies/doughnuts, fried potatoes, salt intake, sugar sweetened soft drinks, and frequency of fast food intake) but the trend remained significant: OR (95% CI): 1.00 (reference), 0.84 (0.63–1.11), and 0.92 (0.67–1.26), p-value for trend across the tertiles 0.002. The inclusion of legumes as a vegetable did not meaningfully change the results of the analysis (results not shown).
Adjusting for potential mediators including systolic blood pressure, LDL and HDL cholesterol, and fasting blood sugar did not meaningfully alter the relationship: OR (95% CI): 1.00 (reference), 0.79 (0.60–1.04), and 0.78 (0.58–1.03), p-value for trend <0.001. Repeating the multivariable analysis (model 2) using relative risk regression yielded similar results [OR (95% CI): 1.00 (reference), 0.83 (0.67–1.02), 0.80 (0.64–1.00), p-value for trend across the tertiles <0.001].
A multivariable-adjusted analysis of intake of F/V separately showed a similar benefit for fruits and vegetables respectively: OR (95% CI) were 1.00 [reference], 0.92 [0.70–1.20], and 0.85 [0.64–1.12] from lowest to highest tertiles of fruit intake (p-value for trend 0.002), and 1.00 [reference], 0.84 [0.64–1.12], 0.81 [0.61–1.08] for corresponding tertiles of vegetable intake (p-value for trend <0.001).
When stratified by sex, the inverse association between F/V intake and CAC appeared limited to women compared to men (p-value for interaction 0.05 in the multivariable model). In the multivariable model, women in top tertile of F/V intake were 45% less likely to have prevalent CAC compared to women in the bottom tertile: OR (95% CI) 1.0 (ref), 0.73 (0.48–1.10), and 0.55 (0.35–0.87), p-value for trend 0.01, Figure 1. Conversely, reported intake of F/V did not appear to be associated with prevalent CAC among men: OR (95% CI) 1.0 (ref), 0.77 (0.52–1.12), 0.89 (0.60–1.31), p-value for trend 0.67, p-value for interaction 0.05, Figure 1.
Figure 1.
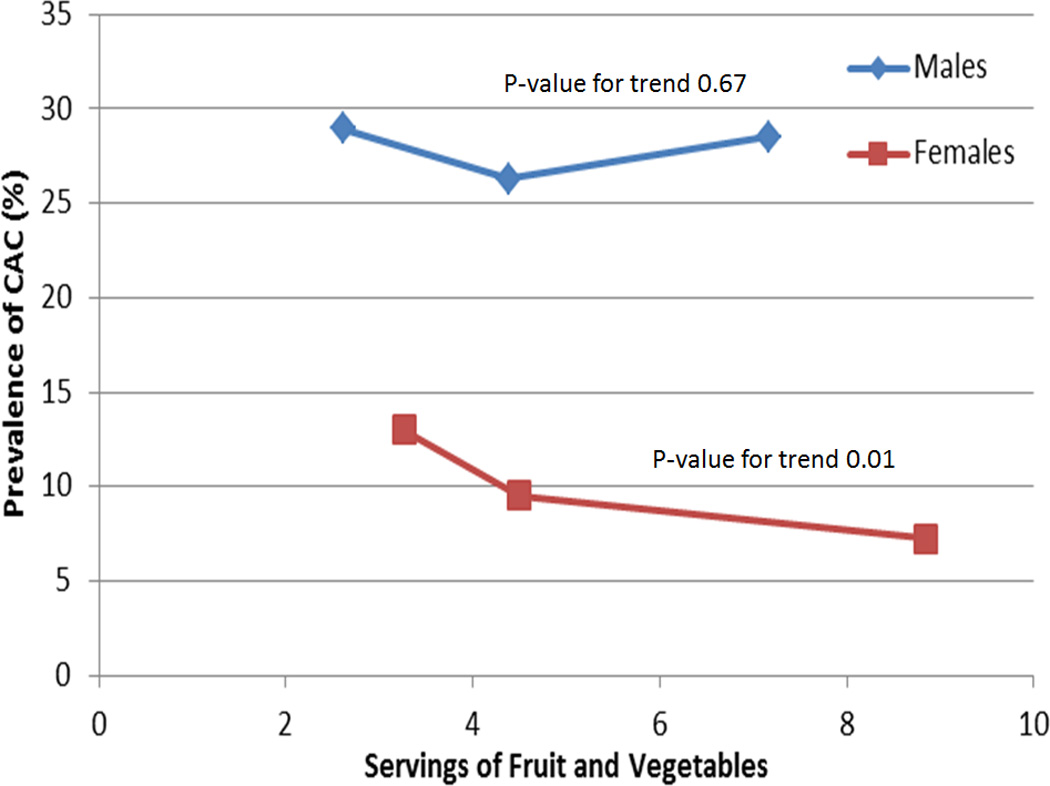
Prevalence of CAC at the year 20 exam according to energy-adjusted tertiles of servings of F/V per day at the baseline exam in men and women in CARDIA.
In women, a model with the additional examination of other dietary factors (dairy, nuts, legumes, eggs, fish, beef, refined grain bread, refined grain pasta, cakes/cookies/doughnuts, fried potatoes, salt intake, sugar sweetened soft drinks, and frequency of fast food intake) did not alter the trend seen between F/V intake and CAC: OR (95% CI) were 1.00 [reference], 0.74 (0.48–1.14), and 0.56 (0.34–0.94), from lowest to highest tertiles of F/V intake in women, p-value for trend 0.03. There was minimal attenuation of the relationship between F/V intake during young adulthood and CAC at year 20 in women with the updated use of year 20 F/V data: OR (95% CI), 1.00 [reference], 0.74 [0.47–1.16], and 0.58 [0.35–0.97], for corresponding tertiles of F/V intake. Also, the relationship between F/V and CAC in women did not appear to be significantly mediated by SBP, LDL cholesterol, HDL cholesterol, or fasting blood sugar, as addition of these variables (measured at the year 20 follow-up) did not alter the relationship: OR (95% CI) 1.00 (reference), 0.75 (0.49–1.14), and 0.58 (0.37–0.93), from lowest to highest tertiles in women). The addition of other dietary variables, F/V intake at year 20, as well as potential mediators did not substantially alter the non-significant relationship between F/V and CAC in men (results not shown).
Discussion
We found a significant inverse association between F/V intake during young adulthood and the prevalence of CAC later in life. After adjustment for relevant variables, young adults in the top tertile who averaged 7–9 servings per day of F/V at baseline were approximately 25% less likely to have any CAC after 20 years of follow-up compared to the bottom tertile who averaged 2–4 servings of F/V per day. An analysis of F/V individually showed a similar benefit for each food group. There was attenuation of the association between F/V and CAC after additional adjustment for other dietary factors but the trend in the association remained significant. Our results support endorsing intake of F/V in young adults as part of an overall healthy dietary pattern aimed at reducing future CVD.
Previous studies demonstrating an inverse association between F/V intake and CHD and CVD have largely been limited to middle-aged adults. A meta-analysis of observational cohorts (mean age ~ 50 years) found that each additional serving of F/V was associated with a risk reduction of 4% (95% CI: 1% to 4%) for a CHD event.4 An analysis from the National Health and Nutritional Examination Survey evaluated the relationship between F/V and CVD, finding that individuals who reported consuming F/V three or more times per day was associated with a 37% (95% CI: 21% to 49%) lower rate of CVD mortality compared to individuals who reported consuming F/V <1 time per day.6 In both of these studies, the benefit of F/V intake was similar for men and women.
The lack of association between F/V intake and CAC in men in our study may be due to a lack of power, as our study included only 935 male participants. However, a less significant association between CVD and F/V intake in men has been seen in other studies. Data from the European Prospective Investigation into Cancer and Nutrition (EPIC)-Heart study demonstrated a 15% (95% CI: 6% to 23%) lower risk for CHD mortality per 80gram/day increase in fruit and vegetable intake in women, but a non-significant 2% (95% CI: −2% to +2%) CHD mortality reduction in men (p-value for heterogeneity 0.007).2 Similar findings were reported in a cohort of Japanese women and men.3 In the CHD risk factor study INTERHEART, the 3 lifestyle behaviors associated with a lower risk of CHD were F/V intake, exercise, and moderate alcohol consumption, and the protective effects of exercise and moderate alcohol consumption were larger in women compared to men with a trend towards F/V intake being more protective in women as well.22 Although the protective benefit of lifestyle behaviors against CHD may be more pronounced in women, the results of our study should not be used to minimize the potential health benefits of F/V intake for men, as several other studies have found positive associations from F/V intake for men, including lower rates in CVD, cancer, and all-cause mortality.1,4–6,23,24 Individuals in our study with a high intake of F/V generally had a healthier dietary pattern overall, including a higher intake of fish, and less intake of refined carbohydrates, salt, and fast food compared to those with low intake of F/V. The association between F/V and CAC may be influenced by a corresponding decrease in intake of unhealthy substances as opposed to a direct benefit of F/V, and adjustment for multiple dietary variables did result in some attenuation of the association between F/V and CAC although the trend remained significant. This finding is consistent with a recent global analysis that suggested that insufficient intake of healthy foods is responsible for a larger burden of chronic disease than what is due to excessive intake of unhealthy foods.25
There are multiple potential mechanisms by which F/V intake could lead to a reduction in atherosclerotic plaque formation, including improved lipids, lower blood pressure, and increased intake of various antioxidant micronutrients.26 Observational studies have suggested more optimal lipid values in individuals with higher F/V intake,27 but randomized trials have failed to confirm this relationship.28,29 Two randomized trials demonstrated a reduction in systolic blood pressure with increased intake of F/V.28,30 In our study, adjusting for systolic blood pressure, HDL cholesterol, and LDL cholesterol did not substantially attenuate the relationship between F/V intake and CAC, suggesting alternative mechanisms. Vitamins and other antioxidant micronutrients have long been hypothesized to have significant cardiovascular benefits,31 but multiple randomized trials evaluating various supplemented micronutrients have failed to show CVD benefit.32,33 The results of our study lend further support to the importance of emphasizing consumption of whole foods, including F/V, as opposed to use of nutritional supplements. F/V contain multiple components beyond antioxidants that may confer a cardiovascular benefit, including multiple different vitamins, phytochemicals, and electrolytes.34
Our analysis has several strengths including a large sample, extensive data on traditional cardiovascular risk factors, and a standardized approach to CAC assessment. It also has limitations. Given the observational nature of our study and the variance in the baseline characteristics across the F/V tertiles, residual confounding may still be present in the multivariable model. Equal numbers of men and women were enrolled in CARDIA at baseline but, due to a greater retention of women over time, our analysis contained significantly more women than men. Also, CAC is a surrogate marker of CHD, representative of subclinical atherosclerosis as opposed to actual CHD events, and we only analyzed a single measurement of CAC, thereby preventing analysis of the relationship between F/V intake and CAC progression. Additionally, not all exposures with established associations with CHD have been found to have a similar association with subclinical atherosclerosis. For instance, moderate alcohol consumption has a well-established association with a lower risk of CHD events but is associated with an increase in the prevalence of CAC35,36, suggesting a non-atherosclerotic mechanism. However, CAC is a strong predictor of future CHD events and was recently shown to be the only novel predictor with the capacity to substantially improve discrimination above and beyond traditional risk assessment.11 CAC has been shown to highly correlate with total atherosclerotic plaque burden, even more so than luminal stenosis.37,38
A sub-optimal diet is one of the leading contributors to the global burden of CVD, and methods to improve dietary patterns hold the potential to significantly impact CVD rates, even if those methods only lead to a modest shift in population CVD risk.12 The recently released American College of Cardiology/American Heart Association lifestyle guidelines encourage a diet that includes a high intake of F/V as a Class 1-Grade A recommendation to lower cardiovascular risk.9 Our results support this recommendation, reinforce the value of establishing healthy behaviors early in adulthood, and provide further credence for public health initiatives aimed at increasing F/V intake in adolescents and young adults.
Supplementary Material
Acknowledgments
Funding Source: The CARDIA study is conducted and supported by the National Heart, Lung, and Blood Institute (NHLBI) in collaboration with the University of Alabama at Birmingham (grants HHSN268201300025C and HHSN268201300026C), Northwestern University (grant HHSN268201300027C), University of Minnesota (grant HHSN268201300028C), Kaiser Foundation Research Institute (grant HHSN268201300029C), and Johns Hopkins University School of Medicine (grant HHSN268200900041C). CARDIA is also partially supported by the Intramural Research Program of the National Institute on Aging (NIA) and an intra-agency agreement between NIA and NHLBI (grant AG0005).
Footnotes
Disclosures: None.
References
- 1.Joshipura KJ, Hu FB, Manson JE, Stampfer MJ, Rimm EB, Speizer FE, Colditz G, Ascherio A, Rosner B, Spiegelman D, Willett WC. The effect of fruit and vegetable intake on risk for coronary heart disease. Ann Intern Med. 2001;134:1106–1114. doi: 10.7326/0003-4819-134-12-200106190-00010. [DOI] [PubMed] [Google Scholar]
- 2.Crowe FL, Roddam AW, Key TJ, Appleby PN, Overvad K, Jakobsen MU, Tjønneland A, Hansen L, Boeing H, Weikert C, Linseisen J, Kaaks R, Trichopoulou A, Misirli G, Lagiou P, Sacerdote C, Pala V, Palli D, Tumino R, Panico S, Bueno-de-Mesquita HB, Boer J, van Gils CH, Beulens JW, Barricarte A, Rodríguez L, Larrañaga N, Sánchez MJ, Tormo MJ, Buckland G, Lund E, Hedblad B, Melander O, Jansson JH, Wennberg P, Wareham NJ, Slimani N, Romieu I, Jenab M, Danesh J, Gallo V, Norat T, Riboli E European Prospective Investigation into Cancer and Nutrition (EPIC)-Heart Study Collaborators. Fruit and vegetable intake and mortality from ischaemic heart disease: results from the European Prospective Investigation into Cancer and Nutrition (EPIC)-Heart study. Eur Heart J. 2011;32:1235–1243. doi: 10.1093/eurheartj/ehq465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nakamura K, Nagata C, Oba S, Takatsuka N, Shimizu H. Fruit and vegetable intake and mortality from cardiovascular disease are inversely associated in Japanese women but not in men. J Nutr. 2008;138:1129–1134. doi: 10.1093/jn/138.6.1129. [DOI] [PubMed] [Google Scholar]
- 4.Dauchet L, Amouyel P, Hercberg S, Dallongeville J. Fruit and vegetable consumption and risk of coronary heart disease: a meta-analysis of cohort studies. J Nutr. 2006;136:2588–2593. doi: 10.1093/jn/136.10.2588. [DOI] [PubMed] [Google Scholar]
- 5.Joshipura KJ, Ascherio A, Manson JE, Stampfer MJ, Rimm EB, Speizer FE, Hennekens CH, Spiegelman D, Willett WC. Fruit and vegetable intake in relation to risk of ischemic stroke. JAMA. 1999;282:1233–1239. doi: 10.1001/jama.282.13.1233. [DOI] [PubMed] [Google Scholar]
- 6.Bazzano LA, He J, Ogden LG, Loria CM, Vupputuri S, Myers L, Whelton PK. Fruit and vegetable intake and risk of cardiovascular disease in US adults: the first National Health and Nutrition Examination Survey Epidemiologic Follow-up Study. Am J Clin Nutr. 2002;76:93–99. doi: 10.1093/ajcn/76.1.93. [DOI] [PubMed] [Google Scholar]
- 7.Tuzcu EM, Kapadia SR, Tutar E, Ziada KM, Hobbs RE, McCarthy PM, Young JB, Nissen SE. High Prevalence of Coronary Atherosclerosis in Asymptomatic Teenagers and Young Adults : Evidence From Intravascular Ultrasound. Circulation. 2001;103:2705–2710. doi: 10.1161/01.cir.103.22.2705. [DOI] [PubMed] [Google Scholar]
- 8.Mozaffarian D, Afshin A, Benowitz NL, Bittner V, Daniels SR, Franch HA, Jacobs DR, Jr, Kraus WE, Kris-Etherton PM, Krummel DA, Popkin BM, Whitsel LP, Zakai NA American Heart Association Council on Epidemiology and Prevention, Council on Nutrition, Physical Activity and Metabolism, Council on Clinical Cardiology, Council on Cardiovascular Disease in the Young. Population approaches to improve diet, physical activity, and smoking habits: a scientific statement from the American Heart Association. Circulation. 2012;126:1514–1563. doi: 10.1161/CIR.0b013e318260a20b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Eckel RH, Jakicic JM, Ard JD, Miller NH, Hubbard VS, Nonas CA, de Jesus JM, Sacks FM, Lee I-M, Smith SC, Jr, Lichtenstein AH, Svetkey LP, Loria CM, Wadden TW, Millen BE, Yanovski SZ. 2013 AHA/ACC Guideline on Lifestyle Management to Reduce Cardiovascular Risk. J Am Coll Cardiol. 2014;63:2960–2984. doi: 10.1016/j.jacc.2013.11.003. [DOI] [PubMed] [Google Scholar]
- 10.Detrano R, Guerci AD, Carr JJ, Bild DE, Burke G, Folsom AR, Liu K, Shea S, Szklo M, Bluemke DA, O’Leary DH, Tracy R, Watson K, Wong ND, Kronmal RA. Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med. 2008;358:1336–1345. doi: 10.1056/NEJMoa072100. [DOI] [PubMed] [Google Scholar]
- 11.Yeboah J, McClelland RL, Polonsky TS, Burke GL, Sibley CT, O’Leary DH, Carr JJ, Goff DC, Greenland P, Herrington DM. Comparison of novel risk markers for improvement in cardiovascular risk assessment in intermediate-risk individuals. JAMA. 2012;308:788–795. doi: 10.1001/jama.2012.9624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tota-Maharaj R, Blaha MJ, McEvoy JW, Blumenthal RS, Muse ED, Budoff MJ, Shaw LJ, Berman DS, Rana JS, Rumberger J, Callister T, Rivera J, Agatston A, Nasir K. Coronary artery calcium for the prediction of mortality in young adults and elderly adults. Eur Heart J. 2012;33:2955–2962. doi: 10.1093/eurheartj/ehs230. [DOI] [PubMed] [Google Scholar]
- 13.Blaha MJ, Budoff MJ, Shaw LJ, Khosa F, Rumberger JA, Berman D, Callister T, Raggi P, Blumenthal RS, Nasir K. Absence of coronary artery calcification and all-cause mortality. JACC Cardiovasc Imaging. 2009;2:692–700. doi: 10.1016/j.jcmg.2009.03.009. [DOI] [PubMed] [Google Scholar]
- 14.Friedman GD, Cutter GR, Donahue RP, Hughes GH, Hulley SB, Jacobs DR, Jr, Liu K, Savage PJ. CARDIA: study design, recruitment, and some characteristics of the examined subjects. J Clin Epidemiol. 1988;41:1105–1116. doi: 10.1016/0895-4356(88)90080-7. [DOI] [PubMed] [Google Scholar]
- 15.Cutter GR, Burke GL, Dyer AR, Friedman GD, Hilner JE, Hughes GH, Hulley SB, Jacobs DR, Jr, Liu K, Manolio TA. Cardiovascular risk factors in young adults: the CARDIA baseline monograph. Control Clin Trials. 1991;12(suppl):1S–77S. doi: 10.1016/0197-2456(91)90002-4. [DOI] [PubMed] [Google Scholar]
- 16.Hughes GH, Cutter G, Donahue R, Friedman GD, Hulley S, Hunkeler E, Jacobs DR, Jr, Liu K, Orden S, Pirie P. Recruitment in the Coronary Artery Disease Risk Development in Young Adults (CARDIA) study. Control Clin Trials. 1987;8(suppl):68S–73S. doi: 10.1016/0197-2456(87)90008-0. [DOI] [PubMed] [Google Scholar]
- 17.McDonald A, Van Horn L, Slattery M, Hilner J, Bragg C, Caan B, Jacobs D, Jr, Liu K, Hubert H, Gernhofer N, Betz E, Havlik D. The CARDIA dietary history: development, implementation, and evaluation. J Am Diet Assoc. 1991;91:1104–1112. [PubMed] [Google Scholar]
- 18.Liu K, Slattery M, Jacobs D, Jr, Cutter G, McDonald A, Van Horn L, Hilner JE, Caan B, Bragg C, Dyer A. A study of the reliability and comparative validity of the CARDIA dietary history. Ethn Dis. 1994;4:15–27. [PubMed] [Google Scholar]
- 19.Carr JJ, Nelson JC, Wong ND, McNitt-Gray M, Arad Y, Jacobs DR, Jr, Sidney S, Bild DE, Williams OD, Detrano RC. Calcified coronary artery plaque measurement with cardiac CT in population-based studies: standardized protocol of Multi-Ethnic Study of Atherosclerosis (MESA) and Coronary Artery Risk Development in Young Adults (CARDIA) study. Radiology. 2005;234:35–43. doi: 10.1148/radiol.2341040439. [DOI] [PubMed] [Google Scholar]
- 20.Carr JJ, Crouse JR, III, Goff DC, Jr, D’Agostino RB, Jr, Peterson NP, Burke GL. Evaluation of sub-second gated helical CT for quantification of coronary artery calcium and comparison with electron beam CT. AJR Am J Roentgenol. 2000;174:915–921. doi: 10.2214/ajr.174.4.1740915. [DOI] [PubMed] [Google Scholar]
- 21.Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M, Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15:827–832. doi: 10.1016/0735-1097(90)90282-t. [DOI] [PubMed] [Google Scholar]
- 22.Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, McQueen M, Budaj A, Pais P, Varigos J, Lisheng L INTERHEART Study Investigators. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364:937–952. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 23.Jansen MC1, Bueno-de-Mesquita HB, Feskens EJ, Streppel MT, Kok FJ, Kromhout D. Quantity and variety of fruit and vegetable consumption and cancer risk. Nutr Cancer. 2004;48:142–148. doi: 10.1207/s15327914nc4802_3. [DOI] [PubMed] [Google Scholar]
- 24.Leenders M1, Sluijs I, Ros MM, Boshuizen HC, Siersema PD, Ferrari P, Weikert C, Tjønneland A, Olsen A, Boutron-Ruault MC, Clavel-Chapelon F, Nailler L, Teucher B, Li K, Boeing H, Bergmann MM, Trichopoulou A, Lagiou P, Trichopoulos D, Palli D, Pala V, Panico S, Tumino R, Sacerdote C, Peeters PH, van Gils CH, Lund E, Engeset D, Redondo ML, Agudo A, Sánchez MJ, Navarro C, Ardanaz E, Sonestedt E, Ericson U, Nilsson LM, Khaw KT, Wareham NJ, Key TJ, Crowe FL, Romieu I, Gunter MJ, Gallo V, Overvad K, Riboli E, Bueno-de-Mesquita HB. Fruit and vegetable consumption and mortality: European prospective investigation into cancer and nutrition. Am J Epidemiol. 2013;178:590–602. doi: 10.1093/aje/kwt006. [DOI] [PubMed] [Google Scholar]
- 25.Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, Amann M, Anderson HR, Andrews KG, Aryee M, Atkinson C, Bacchus LJ, Bahalim AN, Balakrishnan K, Balmes J, Barker-Collo S, Baxter A, Bell ML, Blore JD, Blyth F, Bonner C, Borges G, Bourne R, Boussinesq M, Brauer M, Brooks P, Bruce NG, Brunekreef B, Bryan-Hancock C, Bucello C, Buchbinder R, Bull F, Burnett RT, Byers TE, Calabria B, Carapetis J, Carnahan E, Chafe Z, Charlson F, Chen H, Chen JS, Cheng AT, Child JC, Cohen A, Colson KE, Cowie BC, Darby S, Darling S, Davis A, Degenhardt L, Dentener F, Des Jarlais DC, Devries K, Dherani M, Ding EL, Dorsey ER, Driscoll T, Edmond K, Ali SE, Engell RE, Erwin PJ, Fahimi S, Falder G, Farzadfar F, Ferrari A, Finucane MM, Flaxman S, Fowkes FG, Freedman G, Freeman MK, Gakidou E, Ghosh S, Giovannucci E, Gmel G, Graham K, Grainger R, Grant B, Gunnell D, Gutierrez HR, Hall W, Hoek HW, Hogan A, Hosgood HD, 3rd, Hoy D, Hu H, Hubbell BJ, Hutchings SJ, Ibeanusi SE, Jacklyn GL, Jasrasaria R, Jonas JB, Kan H, Kanis JA, Kassebaum N, Kawakami N, Khang YH, Khatibzadeh S, Khoo JP, Kok C, Laden F, Lalloo R, Lan Q, Lathlean T, Leasher JL, Leigh J, Li Y, Lin JK, Lipshultz SE, London S, Lozano R, Lu Y, Mak J, Malekzadeh R, Mallinger L, Marcenes W, March L, Marks R, Martin R, McGale P, McGrath J, Mehta S, Mensah GA, Merriman TR, Micha R, Michaud C, Mishra V, Mohd Hanafiah K, Mokdad AA, Morawska L, Mozaffarian D, Murphy T, Naghavi M, Neal B, Nelson PK, Nolla JM, Norman R, Olives C, Omer SB, Orchard J, Osborne R, Ostro B, Page A, Pandey KD, Parry CD, Passmore E, Patra J, Pearce N, Pelizzari PM, Petzold M, Phillips MR, Pope D, Pope CA, 3rd, Powles J, Rao M, Razavi H, Rehfuess EA, Rehm JT, Ritz B, Rivara FP, Roberts T, Robinson C, Rodriguez-Portales JA, Romieu I, Room R, Rosenfeld LC, Roy A, Rushton L, Salomon JA, Sampson U, Sanchez-Riera L, Sanman E, Sapkota A, Seedat S, Shi P, Shield K, Shivakoti R, Singh GM, Sleet DA, Smith E, Smith KR, Stapelberg NJ, Steenland K, Stöckl H, Stovner LJ, Straif K, Straney L, Thurston GD, Tran JH, Van Dingenen R, van Donkelaar A, Veerman JL, Vijayakumar L, Weintraub R, Weissman MM, White RA, Whiteford H, Wiersma ST, Wilkinson JD, Williams HC, Williams W, Wilson N, Woolf AD, Yip P, Zielinski JM, Lopez AD, Murray CJ, Ezzati M, AlMazroa MA, Memish ZA. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2224–2260. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bazzano LA, Serdula MK, Liu S. Dietary intake of fruits and vegetables and risk of cardiovascular disease. Curr Atheroscler Rep. 2003;5:492–499. doi: 10.1007/s11883-003-0040-z. [DOI] [PubMed] [Google Scholar]
- 27.Djousse´ L, Arnett DK, Coon H, Province MA, Moore LL, Ellison RC. Fruit and vegetable consumption and LDL cholesterol: the National Heart, Lung, and Blood Institute Family Heart Study. Am J Clin Nutr. 2004;79:213–217. doi: 10.1093/ajcn/79.2.213. [DOI] [PubMed] [Google Scholar]
- 28.John JH, Ziebland S, Yudkin P, Roe LS, Neil HAW. Effects of fruit and vegetable consumption on plasma antioxidant concentrations and blood pressure: a randomized controlled trial. Lancet. 2002;359:1969–1974. doi: 10.1016/s0140-6736(02)98858-6. [DOI] [PubMed] [Google Scholar]
- 29.Zino S, Skeaff M, Williams S, Mann J. Randomised controlled trial of effect of fruit and vegetable consumption on plasma concentrations of lipids and antioxidants. BMJ. 1997;314:1787–1791. doi: 10.1136/bmj.314.7097.1787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, Bray GA, Vogt TM, Cutler JA. DASH collaborative research group. A clinical trial of the effects of dietary patterns on blood pressure. N Engl J Med. 1997;336:1117–1124. doi: 10.1056/NEJM199704173361601. [DOI] [PubMed] [Google Scholar]
- 31.Diaz MN, Frei B, Vita JA, Keaney JF., Jr Antioxidants and atherosclerotic heart disease. N Engl J Med. 1997;337:408–416. doi: 10.1056/NEJM199708073370607. [DOI] [PubMed] [Google Scholar]
- 32.Sesso HD, Christen WG, Bubes V, Smith JP, MacFadyen J, Schvartz M, Manson JE, Glynn RJ, Buring JE, Gaziano JM. Multivitamins in the prevention of cardiovascular disease in men: the Physicians' Health Study II randomized controlled trial. JAMA. 2012;308:1751–1760. doi: 10.1001/jama.2012.14805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Clarke R, Armitage J. Antioxidant vitamins and risk of cardiovascular disease. Review of large-scale randomised trials. Cardiovasc Drugs Ther. 2002;16:411–615. doi: 10.1023/a:1022134418372. [DOI] [PubMed] [Google Scholar]
- 34.Lichtenstein AH, Russell RM. Essential nutrients: food or supplements? Where should the emphasis be? JAMA. 2005;294:351–358. doi: 10.1001/jama.294.3.351. [DOI] [PubMed] [Google Scholar]
- 35.Burke GL, Mukamal KJ, Lima JA, Kronmal RA. Alcohol and coronary artery calcium prevalence, incidence, and progression: results from the Multi-Ethnic Study of Atherosclerosis (MESA) Am J Clin Nutr. 2008;88:1593–1601. doi: 10.3945/ajcn.2008.26420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pletcher MJ, Varosy P, Kiefe CI, Lewis CE, Sidney S, Hulley SB. Alcohol consumption, binge drinking, and early coronary calcification: findings from the Coronary Artery Risk Development in Young Adults Study. Am J Epidemiol. 2005;161:423–433. doi: 10.1093/aje/kwi062. [DOI] [PubMed] [Google Scholar]
- 37.Rumberger JA, Simons DB, Fitzpatrick LA, Sheedy PF, Schwartz RS. Coronary artery calcium area by electron-beam computed tomography and coronary atherosclerotic plaque area. A histopathologic correlative study. Circulation. 1995;92:2157e62. doi: 10.1161/01.cir.92.8.2157. [DOI] [PubMed] [Google Scholar]
- 38.Sangiorgi G, Rumberger JA, Severson A, Edwards WD, Gregoire J, Fitzpatrick LA, Schwartz RS. Arterial calcification and not lumen stenosis is highly correlated with atherosclerotic plaque burden in humans: a histologic study of 723 coronary artery segments using nondecalcifying methodology. J Am Coll Cardiol. 1998;31:126e33. doi: 10.1016/s0735-1097(97)00443-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


