Abstract
Background and Purpose
There are few evidence-based programs for stroke family caregivers post-discharge. The purpose of this study was to evaluate efficacy of the Telephone Assessment and Skill-Building Kit (TASKII), a nurse-led intervention enabling caregivers to build skills based on assessment of their own needs.
Methods
A total of 254 stroke caregivers (primarily female TASK II/ISR 78.0%/78.6%; white 70.7%/72.1%; about half spouses 48.4%/46.6%) were randomized to the TASKII intervention (n=123) or to an Information, Support, and Referral (ISR) group (n=131). Both groups received 8 weekly telephone sessions, with a booster at 12 weeks. General linear models with repeated measures tested efficacy, controlling for patient hospital days and call minutes. Pre-specified 8 week primary outcomes were depressive symptoms (with Patient Health Questionnaire Depressive Symptom Scale PHQ-9≥5), life changes, and unhealthy days.
Results
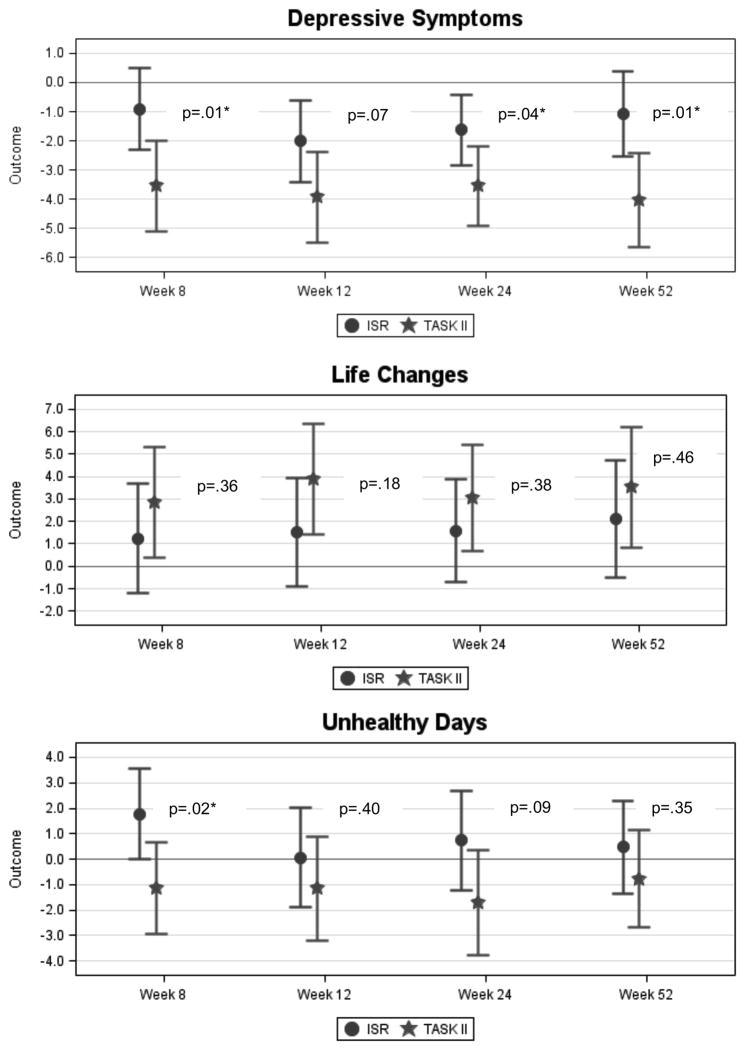
Among caregivers with baseline PHQ-9≥5, those randomized to the TASK II intervention had a greater reduction in depressive symptoms from baseline to 8, 24, and 52 weeks and greater improvement in life changes from baseline to 12 weeks compared to the ISR group (p<.05); but not found for the total sample. Although not sustained at 12, 24, or 52 weeks, caregivers randomized to the TASK II intervention had a relatively greater reduction in unhealthy days from baseline to 8 weeks (p<.05)
Conclusions
The TASK II intervention reduced depressive symptoms and improved life changes for caregivers with mild to severe depressive symptoms. The TASK II intervention reduced unhealthy days for the total sample, although not sustained over the long term.
Keywords: Stroke, Family Caregivers, Depression, Psychosocial Factors, Clinical Trial
Introduction
Despite decline in stroke mortality in past decades, stroke remains a leading cause of disability, with about 45% of stroke survivors being discharged home, 24% to inpatient rehabilitation facilities, and 31% to skilled nursing facilities.1 Most stroke survivors eventually return home, although many family members are unprepared for the caregiving role and have many unmet needs during the early discharge period.2–4 Despite this, caregivers commonly receive little attention from health-care providers.5,6
Caregiver depressive symptoms, negative life changes, and unhealthy days often result from unmet caregiver needs. Many caregivers (30% to 52%) suffer from depression,7–10 with studies reporting higher rates in the caregivers than in the stroke survivors.7 Studies show that family caregivers are at risk for negative life changes, psychosocial impairments, poor health, and even mortality as a result of providing care.8, 9, 11–13 Furthermore, the caregiver’s emotional well-being can influence the stroke survivor’s depressive symptoms.14–16 In addition, the caregiver’s depressive symptoms can affect the stroke survivor’s recovery,15 communication, social participation, and mood.16 Finally, caregiver stress is a leading cause of institutionalization for stroke survivors and other older adults.9, 17,18
Recommendations for stroke family caregiver education and support include: (a) assessment of caregiver needs and concerns; (b) counseling focused on problem solving and social support; (c) information on stroke-related care; and (d) attention to caregivers’ emotional and physical health.19 A recent scientific statement on stroke family caregiving recommended individualized caregiver interventions that combine skill-building (e.g., problem solving, stress management, goal setting) with psycho-educational strategies to improve caregiver outcomes.20–23 There are few evidence-based, easy-to-deliver programs for family caregivers of stroke survivors post-discharge that incorporate these recommendations. The revised Telephone Assessment and Skill-Building Kit (TASKII) clinical trial addressed these recommendations by offering a comprehensive, multi-component program that enables caregivers to assess their needs, build skills in providing care, deal with personal responses to caregiving, and incorporate skill-building strategies into their daily lives.
Methods
Design
A prospective randomized controlled clinical trial design, with outcome data collectors blinded to treatment assignment, was used to evaluate the efficacy of the revised TASKII relative to an Information, Support, and Referral (ISR) comparison group. Both groups received written materials, 8 weekly calls from a nurse, and a booster session one month later. The study was approved by the Indiana University Office of Research Compliance Human Subjects Office (Institutional Review Board) for protection of human subjects and by each facility where recruitment occurred. Recruitment occurred 1/5/11 through 7/10/13. Enrolled subjects gave informed consent.
The primary aim was to examine the short-term (immediately post-intervention at 8 weeks) and longer-term, sustained (12, 24, and 52 weeks) efficacy of the TASK II intervention relative to the ISR comparison group for improving caregivers’ depressive symptoms, caregiving-related life changes, and unhealthy days. For depressive symptoms, primary analyses were performed for the subgroup with mild to severe depressive symptoms at baseline; secondary analyses for depressive symptoms used the entire cohort. Selected covariates were included in the analyses to adjust for group differences in potential confounders.
Participants
A total of 254 stroke family caregivers were randomized to either the TASK II group (n=123) or to the ISR comparison group (n=131). Family caregivers were recruited from 2 rehabilitation hospitals and 6 acute care hospitals in the Midwest. Participants were screened within 8 weeks after the survivor was discharged home. Caregivers were included if the following criteria were met: was the primary caregiver (unpaid family member or significant other), 21 or more years of age, fluent in the English language, had access to a telephone, had no difficulties hearing or talking on the telephone, planned to be providing care for one year or longer, and were willing to participate in 9 calls from a nurse and 5 data collection interviews. Caregivers were excluded if: the patient had not had a stroke, did not need help from the caregiver, or was going to reside in a nursing home or long-term care facility; the caregiver scored <16 on the Oberst Caregiving Burden Scale Task Difficulty Subscale24 or < 4 on a 6-item cognitive impairment screener.25 In addition, caregivers and stroke survivors were excluded if either was pregnant; a prisoner or on house arrest; had a terminal illness (e.g., cancer, end-of-life condition, renal failure requiring dialysis); had a history of Alzheimer’s, dementia, or severe mental illness (e.g., suicidal tendencies, severe untreated depression or manic depressive disorder, schizophrenia); or had been hospitalized for alcohol or drug abuse.
Study Protocol
Study Instruments
The Patient Health Questionnaire Depressive Symptom Scale (PHQ-9), measuring 9 depressive indicators from the DSM-IV, has been widely used in clinical and research settings.26 Depressive symptom severity are categorized as: no depressive symptoms (0–4), mild (5–9), moderate (10–14), moderately severe (15–19), or severe (20–27).26 Evidence of internal consistency reliability has been documented in primary care and with stroke caregivers.11,12 The Cronbach alpha for the PHQ-9 for this study was 0.82.
The 15-item Bakas Caregiving Outcomes Scale (BCOS) was used to measure life changes (i.e., changes in social functioning, subjective well-being, and physical health) specifically as a result of providing care.11 Content, construct, and criterion-related validity have been documented, as well as internal consistency reliability in stroke caregivers.11 Cronbach alpha for the BCOS for this study was 0.87.
Unhealthy Days (UD) were measured by summing two items asking caregivers to estimate the number of days in the past 30 days that their own physical and/or mental health had not been good, with a cap of 30 days.27 The UD measure has been used to track population health status as part of the Behavioral Risk Factor Surveillance System (BRFSS) used across states and communities in support of Healthy People 2010.27 Strong evidence of construct, concurrent, and predictive validity has been documented, as well as reliability and responsiveness.27
Caregiver and survivor characteristics were measured using a demographic form, along with the Chronic Conditions Index,28 Cognitive Status Scale,29 and the Stroke Specific Quality of Life Proxy (SS SSQOL proxy);30 all instruments have acceptable psychometric properties and have been used in the context of stroke.
TASK II Intervention Arm
Stroke caregivers randomized to the TASK II intervention group received the TASK II Resource Guide and a pamphlet from the American Heart Association (AHA) entitled “Caring for Stroke Survivors.”31 The TASK II Resource guide included the Caregiver Needs and Concerns Checklist (CNCC)2 addressing five areas of needs: a) finding information about stroke; b) managing the survivor’s emotions and behaviors; c) providing physical care; d) providing instrumental care; and e) dealing with personal responses to providing care; along with corresponding Tip Sheets addressing each of the items on the CNCC.32 Five skill-building tip sheets were included that respectively addressed strengthening existing skills, screening for depressive symptoms, maintaining realistic expectations, communicating with healthcare providers, and problem solving, as well as a stress management workbook for the caregiver and stroke survivor.32 The TASK II intervention added the use of the BCOS at the fifth call for caregivers to further assess their life changes and to select corresponding tip sheets.33 Calls to caregivers in the TASK II group focused on training caregivers how to identify and prioritize their needs and concerns, find corresponding tip sheets, and address their priority needs and concerns using innovative skill-building strategies.
Information Support and Referral (ISR) Comparison Arm
Stroke caregivers randomized to the ISR group received only the AHA pamphlet.31 Calls to caregivers in the ISR group focused on providing support through the use of active listening strategies.32,33 Both groups received 8 weekly calls from a nurse with a booster call at 12 weeks. Caregivers in both groups were encouraged to seek additional information from the American Stroke Association (ASA) or from their healthcare providers.
Treatment Fidelity and Training
The Treatment Fidelity Checklist34 addressing design, training, delivery, receipt, and enactment was used to maintain and track treatment fidelity for both the TASK II intervention and ISR procedures.35 Training included the use of detailed training manuals and podcasts, training booster sessions, self-evaluation of audio recordings, evaluation by supervisors, quality checklists, and frequent team meetings.35 Protocol adherence was excellent at 80% for the TASK II and 92% for the ISR. 35 Focus groups with nurses yielded further evidence for treatment fidelity. 35
Study Timetable and Assessments
Baseline data collection occurred within 8 weeks after the stroke survivor was discharged home because the early discharge period is a time when caregivers need the most information and skills related to providing care.2, 3, 6, 36, 37 Follow-up data were collected at 8 weeks (immediately post-intervention), with longer-term follow-up data collected at 12 weeks (after the booster session) and at 24 and 52 weeks to explore sustainability of the intervention. Enrollment occurred 1/21/13 through 7/10/13, with follow-up data collection at 52 weeks completed 7/9/14.
Randomization and Masking
After baseline, caregivers were assigned to groups using a block randomized approach with stratification by recruitment site, type of relationship (spouse vs. adult child/other), and baseline depressive symptoms (PHQ-9<5 no depressive symptoms; PHQ-9≥5 mild to severe depressive symptoms). Random allocation sequence was generated using SAS PROC PLAN38 to create the randomized blocks within strata to obtain, as closely as possible, similar numbers and composition (balance) between the groups, and facilitate maintenance of blinding of data collectors. After baseline data collection, the project manager informed the biostatistician of the caregiver’s recruitment site, type of relationship, and depressive symptoms (PHQ-9 score). The biostatistician then notified the project manager of the group assignment, who mailed the appropriate materials to the caregiver and assigned a nurse. Separate nurses were used for TASK II and ISR groups to prevent treatment diffusion. Data collectors were blinded to the caregiver’s randomization status at subsequent data collection points. Separate team meetings were held with outcome data collectors to maintain blinding.
Sample Size and Statistical Analysis
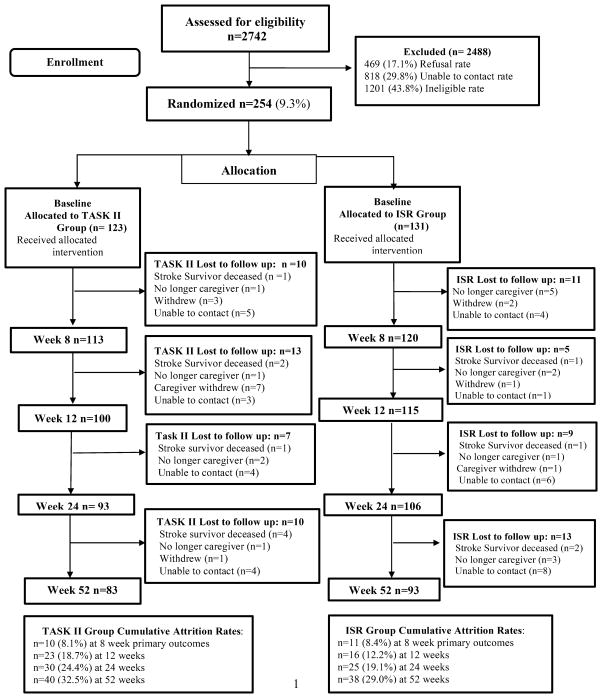
The participant flow diagram is provided in Figure 1. Of the 2742 stroke caregivers assessed for eligibility, 254 were randomized to the TASK II intervention (n =123) or to the ISR comparison group (n = 131). The refusal rate was minimal at 17.1%; 29.8% caregivers were unable to be contacted; and 43.8% were ineligible, primarily because the survivor did not need help from a family caregiver, or the survivor was residing in a nursing home or long-term care facility. Attrition rates ranged from 8.1% at 8 weeks to 32.5% at 52 weeks for the TASK II group and 8.4% at 8 weeks to 29.0% at 52 weeks for the ISR group. The sample size was determined based on pilot data anticipating a 10% attrition rate for the 8 week time point for the primary outcomes using power estimates. Given the full sample of 100 subjects per group, a .20 effect size provided a power of .81 to detect the treatment by time interactions. Given the 10% attrition rate, a sample of 220 caregivers would be needed. To complete those being assessed for eligibility, enrollment exceeded the projected 220 caregivers by an additional 34 caregivers (Total 254 caregivers). Based on pilot data of 38% screening positive for depressive symptoms (PHQ-9 ≥5), it was estimated that there would be a total of 76 caregivers (38 per group), which would provide a power of .81 to detect an effect size of .33 for the treatment by time interaction using a 5% Type I error rate. The sample consisted of a total of 111 caregivers (49 TASK II; 62 ISR) who screened positive for depressive symptoms.
Figure 1.
Participant Flow Diagram.
Study data were collected and managed using REDCap electronic data capture tools hosted at Indiana University.39 All analyses were conducted using SAS version 9.438 Baseline equivalence in demographic characteristics and outcome measures between TASK II and ISR groups was tested using independent samples t (continuous variables) or chi-square (categorical variables). Variables with significant differences between the two groups were selected as covariates. Using an intent-to-treat approach, dependent variables consisting of change relative to baseline value for depressive symptoms, life changes, and unhealthy days were entered into general linear models.40 These models incorporated covariates and took into account the correlation among repeated measures on the same individual.41
Results
Caregivers in TASK II and ISR groups were similar across all demographic characteristics (Table 1). Caregivers were primarily female (78.0%, TASK II; 78.6% ISR), about half spouses (48.4%, TASK II; 46.6%, ISR), predominantly White (70.7%, TASK II; 72.1%, ISR), and ranged in age from 22 to 87 years. Stroke survivors were similar across demographic characteristics, except that survivors whose caregivers were in the ISR group had spent relatively more days in the hospital (TASK II mean [SD] = 17.8 [15.7]; ISR mean [SD] = 23.1 [23.4]; p= 0.037) (Table 2). While stroke severity was not directly measured, caregiver perceptions of the survivor’s functioning as measured by the SSQOL Proxy30 were similar for both groups (Table 2). As expected, the number of minutes across all calls with the nurse (i.e., intervention dosage) differed between groups and was used as a covariate in the models (TASKII mean [SD] = 215.2 [100.8]; ISR mean [SD] = 128.1 [85.8], t = −7.38, p<.001).35 Primary outcome means were similar between caregivers in the two groups at baseline (Table 3).
Table 1.
Caregiver Characteristics with group equivalence.
| Caregiver Characteristics | TASK II | ISR | P value |
|---|---|---|---|
| CG age in years, Mean (SD, range) | 54.0 (12.5, 26 – 83) | 54.7 ( 11.4, 22 – 87) | 0.627 |
| CG gender, N (%) | |||
| Male | 27 ( 22.0) | 28 ( 21.4) | 0.911 |
| Female | 96 ( 78.0) | 103 ( 78.6) | |
| CG race, N (%) | |||
| White | 87 ( 70.7) | 93 ( 72.1) | 0.877 |
| African-American | 30 ( 24.4) | 33 ( 25.6) | |
| American Indian /Alaskan Native | 1 ( 0.8) | 0 | |
| Asian | 2 ( 1.6) | 1 ( 0.8) | |
| More than 1 Race | 3 ( 2.4) | 2 ( 1.6) | |
| Ethnicity, N (%) | |||
| Hispanic/Latino | 3 (2.5) | 0 | 0.110 |
| Non-Hispanic/Non-Latino | 116 (97.5) | 128 (100.0) | |
| CG education years, Mean (SD, range) | 13.8 ( 2.8, 8 – 21) | 13.5 ( 2.5, 7 – 22) | 0.357 |
| CG perceived income, N (%) | |||
| Just have enough to make ends meet | 51 ( 41.8) | 55 ( 42.3) | 0.807 |
| Comfortable | 35 ( 28.7) | 41 ( 31.5) | |
| Not enough to make ends meet | 36 ( 29.5) | 34 ( 26.2) | |
| CG employment, N (%) | |||
| Employed full-time | 39 ( 32.2) | 46 ( 35.1) | 0.594 |
| Employed part-time | 14 ( 11.6) | 12 ( 9.2) | |
| Unemployed | 15 ( 12.4) | 25 ( 19.1) | |
| Retired | 27 ( 22.3) | 28 ( 21.4) | |
| Homemaker | 10 ( 8.3) | 7 ( 5.3) | |
| Other | 16 ( 13.2) | 13 ( 9.9) | |
| CG type of relationship, N (%) | 0.810 | ||
| Spouse | 59 (48.4) | 61 (46.6) | |
| Son or daughter (in law) | 39 (32.0) | 37 (28.2) | |
| Other relative | 15 ( 12.3) | 18 ( 13.7) | |
| Friend | 2 ( 1.6) | 4 ( 3.1) | |
| Other | 7 ( 5.7) | 11 ( 8.4) | |
| CG length of care months, Mean (SD) | 13.0 ( 63.5, 0 – 684) | 18.5 ( 64.8, 0 – 492) | 0.498 |
| CG care days per week, N (%) | |||
| Daily (7 days per week) | 100 ( 81.3) | 107 ( 81.7) | 0.369 |
| 5–6 days per week | 7 ( 5.7) | 9 ( 6.9) | |
| 3–4 days per week | 10 ( 8.1) | 4 ( 3.1) | |
| 1–2 days per week | 5 ( 4.1) | 9 ( 6.9) | |
| Less than one day per week | 1 ( 0.8) | 2 ( 1.5) | |
| CG depression diagnosed, N (%) | |||
| No | 86 ( 70.5) | 93 ( 71.0) | 0.930 |
| Yes | 36 ( 29.5) | 38 ( 29.0) | |
| CG antidepressants, N (%) | |||
| No | 80 ( 65.6) | 85 ( 64.9) | 0.909 |
| Yes | 42 ( 34.4) | 46 ( 35.1) | |
| CG counseling depression, N (%) | |||
| No | 98 ( 81.7) | 108 ( 83.7) | 0.668 |
| Yes | 22 ( 18.3) | 21 ( 16.3) | |
| CG # chronic conditions, Mean (SD) | 2.2 ( 1.9, 0 – 9) | 2.2 ( 1.7, 0 – 7) | 0.963 |
Note: a. *p<.05; **p<.01; ***p<.001; b. independent samples t-test (continuous variables) and chi-square (categorical variables) were used to test equivalence.
Table 2.
Survivor Characteristics with group equivalence.
| Stroke Survivor Characteristics | TASK II | ISR | P value |
|---|---|---|---|
| SS age in years, Mean (SD, range) | 62.7 ( 14.5, 23 – 91) | 63.4 ( 14.5, 25 −94) | 0.685 |
| SS gender, N (%) | |||
| Male | 60 ( 49.6) | 66 ( 50.8) | 0.852 |
| Female | 61 ( 50.4) | 64 ( 49.2) | |
| SS race, N (%) | |||
| White | 87 ( 71.3) | 92 ( 71.3) | 0.877 |
| African-American | 32 ( 26.2) | 36 ( 27.9) | |
| Asian | 1 ( 0.8) | 1 ( 0.8) | |
| Hawaiian/Pacific Islander | 1 ( 0.8) | 0 | |
| Other or Unknown | 1 ( 0.8) | 0 | |
| Ethnicity, N (%) | |||
| Hispanic / Latino | 1 (0.9) | 0 | 0.478 |
| Non-Hispanic / Non-Latino | 116 (99.1) | 128 (100.0) | |
| SS education years, Mean (SD, range) | 13.0 ( 2.7, 0 – 20) | 12.7 ( 2.6, 7 – 23) | 0.320 |
| SS hospital days, Mean (SD, range) | 17.8 ( 15.7, 0 – 83) | 23.1 ( 23.4, 0 – 103) | 0.037* |
| SS # days discharge to study enrollment, Mean (SD, range) | 40.0 (39.2, 7 – 56) | 37.5 (19.0, 4 – 56) | 0.525 |
| SS # strokes, N (%) | |||
| 1 | 82 ( 68.3) | 77 ( 60.2) | 0.519 |
| 2 | 21 ( 17.5) | 28 ( 21.9) | |
| 3 | 10 ( 8.3) | 11 ( 8.6) | |
| ≥4 | 7 (5.8) | 12 (9.4) | |
| SS inpatient rehab, N (%) | |||
| No | 23 ( 18.9) | 29 ( 22.5) | 0.478 |
| Yes | 99 ( 81.1) | 100 ( 77.5) | |
| SS # outpatient rehab therapy visits past 3 months, Mean (SD, range) | 9.7 (12.5, 0 – 75) | 10.0 (12.7, 0 – 90) | .853 |
| SS depression diagnosed, N (%) | |||
| No | 77 ( 63.6) | 74 ( 56.5) | 0.247 |
| Yes | 44 ( 36.4) | 57 ( 43.5) | |
| SS antidepressants, N (%) | |||
| No | 68 ( 56.2) | 71 ( 54.2) | 0.750 |
| Yes | 53 ( 43.8) | 60 ( 45.8) | |
| SS counseling depression | |||
| No | 102 ( 85.0) | 116 ( 88.5) | 0.406 |
| Yes | 18 ( 15.0) | 15 ( 11.5) | |
| SS # chronic conditions (proxy), Mean (SD, range) | 4.0 ( 1.6, 1 – 9) | 4.1 ( 1.8, 0 – 9) | 0.466 |
| SS Cogn Status Score (proxy), Mean (SD, range) | 34.0 ( 5.3, 16 – 40) | 33.7 ( 5.4, 13 – 40) | 0.596 |
| SS SSQOL 7 domain scores (proxy), Mean (SD, range) | |||
| Thinking | 2.7 ( 1.1) | 2.7 ( 1.1) | 0.764 |
| Language | 3.9 ( 1.0) | 3.8 ( 1.1) | 0.394 |
| Vision | 4.1 ( 1.0) | 4.3 ( 0.9) | 0.257 |
| Energy | 2.2 ( 1.2) | 2.1 ( 1.1) | 0.731 |
| Physical function | 3.3 ( 1.0) | 3.2 ( 1.0) | 0.554 |
| Mental function | 2.9 ( 1.0) | 3.0 ( 1.1) | 0.655 |
| Role function | 2.2 (1.0) | 2.3 (1.0) | 0.748 |
| SS SSQOL 7 domain total (proxy) | 3.3 ( 0.7) | 3.2 ( 0.7) | 0.576 |
Note: a. *p<.05; **p<.01; ***p<.001; b. independent samples t-test (continuous variables) and chi-square (categorical variables) were used to test equivalence.
Table 3.
Primary outcomes at baseline with group equivalence.
| Outcome Measures | TASK II (N=123) | ISR (N=131) | P value |
|---|---|---|---|
| Depressive symptoms (PHQ-9), mean (SD, range) | 5.4 (5.1, 0–25) | 5.4 (4.6, 0–21) | 0.991 |
| Depressive symptoms (PHQ-9) ≥ 5, mean (SD, range) | 9.4 (4.5, 5–25) | 8.9 (3.8, 5–21) | 0.465 |
| CG depressive symptoms (PHQ-9 <5 vs ≥5), N (%) | |||
| PHQ-9 score <5 | 65 ( 52.8) | 65 ( 49.6) | 0.607 |
| PHQ-9 score ≥5 | 58 ( 47.2) | 66 ( 50.4) | |
| Life changes (BCOS), mean (SD, range) | 56.2 (11.2, 19–93) | 55.9 (9.5, 27–89) | 0.788 |
| Unhealthy days (UD), mean (SD, range) | 9.7 (9.82, 0–30) | 8.5 (9.83, 0–30) | 0.340 |
Note: a. *p<.05; **p<.01; ***p<.001; b. independent samples t-test (continuous variables) was used to test equivalence.
Primary End Point (8 Weeks)
At baseline, 47.2% of caregivers in the TASK II group and 50.4% in the ISR group reported mild to severe depressive symptoms (PHQ-9 ≥ 5) (Table 3). Among these caregivers, those in the TASK II group reported a greater reduction in depressive symptoms from baseline to 8 weeks than those in the ISR group (mean difference [SE] = −2.6 [1.1], p = 0.013) (Table 4). This represented a statistically significant interaction between time and treatment. Secondary analyses for depressive symptoms were not significant using the total sample. Groups were similar from baseline to 8 weeks for life changes. Caregivers in the TASK II group reported a greater reduction in unhealthy days from baseline to 8 weeks than those in the ISR group (mean difference [SE] = −2.9 [1.3], p = 0.025) (Table 4). Caregivers within the TASK II group reported improvements in depressive symptoms in both the subgroup (p<.001) and the entire cohort (p<.05) and life changes (p<.05) from baseline to 8 weeks (Table 4).
Table 4.
Least square means of change scores from baseline to post-baseline for primary outcomes by group.
| Outcome Measures | N, N TASKII, ISR | TASK II Mean (SE)a | ISR Mean (SE)a | Difference Mean (SE)a | 95% CI | T | P |
|---|---|---|---|---|---|---|---|
| Depressive symptoms (PHQ9) | |||||||
| 8 weeks | 109, 117 | −1.0 (0.5)* | 0.1 (0.5) | −1.0 (0.7) | (−2.3, 0.3) | −1.6 | 0.116 |
| 12 weeks | 99, 112 | −1.4 (0.5)** | −0.8 (0.5) | −0.6 (0.6) | (−1.8, 0.7) | −0.9 | 0.359 |
| 24 weeks | 90, 103 | −1.1 (0.4)* | −0.6 (0.4) | −0.5 (0.6) | (−1.7, 0.7) | −0.9 | 0.398 |
| 52 weeks | 82, 92 | −1.5 (0.5)** | −0.4 (0.5) | −1.1 (0.7) | (−2.4, 0.3) | −1.6 | 0.122 |
| Depressive symptoms (PHQ9)b | |||||||
| 8 weeks | 49, 62 | −3.6 (0.8)*** | −0.9 (0.7) | −2.6 (1.1)* | (−4.7, −0.6) | −2.5 | 0.013 |
| 12 weeks | 45, 60 | −3.9 (0.8)*** | −2.0 (0.7)** | −1.9 (1.1) | (−4.0, −0.2) | −1.8 | 0.072 |
| 24 weeks | 43, 55 | −3.6 (0.7)*** | −1.6 (0.6)** | −1.9 (0.9)* | (−3.8, −0.1) | −2.1 | 0.041 |
| 52 weeks | 39, 48 | −4.0 (0.8)*** | −1.1 (0.7) | −3.0 (1.1)** | (−5.2, −0.8) | −2.7 | 0.008 |
| Life changes (BCOS) | |||||||
| 8 weeks | 109, 117 | 2.9 (1.3)* | 1.2 (1.2) | 1.6 (1.8) | (−1.9, 5.1) | 0.9 | 0.363 |
| 12 weeksc | 99, 112 | 3.9 (1.3)** | 1.5 (1.2) | 2.4 (1.8) | (−1.1, 5.9) | 1.4 | 0.178c |
| 24 weeks | 90, 103 | 3.1 (1.2)* | 1.6 (1.2) | 1.5 (1.7) | (−1.8, 4.8) | 0.9 | 0.384 |
| 52 weeks | 82, 92 | 3.5 (1.4)* | 2.1 (1.3) | 1.4 (1.9) | (−2.4, 5.2) | 0.7 | 0.465 |
| Unhealthy days | |||||||
| 8 weeks | 108, 116 | −1.1 (0.9) | 1.8 (0.9) | −2.9 (1.3)* | (−5.5, −0.4) | −2.3 | 0.025 |
| 12 weeks | 99, 111 | −1.2 (1.0) | 0.1 (1.0) | −1.2 (1.4) | (−4.1, 1.6) | −0.9 | 0.395 |
| 24 weeks | 90, 103 | −1.7 (1.0) | 0.7 (1.0) | −2.4 (1.4) | (−5.3, 0.4) | 1.7 | 0.094 |
| 52 weeks | 82, 92 | −0.8 (1.0) | 0.5 (0.9) | −1.2 (1.3) | (−3.9, 1.4) | −0.9 | 0.354 |
Note:
*p<.05; **p<.01; ***p<.001;
Subgroup who had PHQ-9 ≥5 at baseline;
Further analyses of the BCOS using the PHQ-9 ≥5 subgroup showed a significant group difference from baseline to 12 weeks (Difference Mean [SE] = 5.8 [2.9], 95% CI = [0.1, 11.6], t=2.0, p=0.046).
Primary end point in bold. Change scores were calculated by subtracting baseline from post-baseline scores.
Secondary End Points (12, 24, and 52 Weeks)
Similar to results at the primary end point, caregivers with PHQ ≥5 in the TASK II group reported a greater reduction in depressive symptoms than those in the ISR group from baseline to 24 weeks (mean difference [SE] = −1.9 [.09], p = 0.041) and baseline to 52 weeks (mean difference [SE] = −3.0 [1.1], p = 0.008); although, these results were not significant using the entire cohort (Table 4). Although life changes were similar for the full sample from baseline to 12 weeks (p = .178) (Table 4), for caregivers with PHQ-9 ≥ 5 at baseline, TASK II participants had greater improvement in life changes than ISR participants from baseline to 12 weeks (mean difference [SE] = 5.8 [2.9], p = 0.046). Moreover, caregivers within the TASK II group reported improvements in depressive symptoms for the PHQ≥5 subgroup (p<.001) and the entire cohort (p<.05) and life changes (p<.05) from baseline to 12, 24, and 52 weeks (Table 4). Caregivers within the ISR group reported improvement in depressive symptoms in the PHQ≥5 subgroup from baseline to 12 and 24 weeks (p<.01) (Table 4).
Discussion
At 8 weeks, the TASKII intervention, compared with the ISR group, reduced unhealthy days, did not significantly affect life changes, and reduced depressive symptoms in the subgroup that had mild to severe baseline depressive symptoms. As expected, secondary analyses of depressive symptoms using the entire cohort from baseline to 8, 12, 24, and 52 weeks were not significant. Some caregivers who were not depressed at baseline may have developed depressive symptoms over time; however, TASK II within group differences showed improvement in depressive symptoms at each follow up time point.
Fewer depressive symptoms
Nevertheless, the TASK II program for family caregivers of stroke survivors post-discharge successfully reduced depressive symptoms within a subgroup experiencing mild to severe depressive symptoms compared to those in the ISR group. These results were evident at our primary endpoint of 8 weeks and were sustained at both 24 and 52 weeks. Although other stroke caregiver intervention studies have reported improvements in caregiver depressive symptoms,20 only one study reported sustainability at 52 weeks.42 This study by Kalra and colleagues42 was a well-designed, randomized controlled clinical trial that tested the efficacy of a hands-on caregiver training program in a sample of 300 stroke caregivers. The intervention group received 3 to 5 inpatient sessions and 1 home visit focused on a variety of skills that included goal setting and tailored psycho-education, although tailoring of the intervention was based on the needs of the stroke survivor rather than the caregiver. The TASK II intervention is unique in that it is delivered completely by telephone, trains caregivers how to assess and address their own needs, and is applicable to a wide variety of stroke caregivers (e.g., spouses, adult children, others). Screening for and addressing caregiver depressive symptoms, as in the TASK II program, not only have the potential to improve caregiver outcomes,10, 12, 19, 20 but may improve the survivors’ recovery15 and reduce the potential for their long-term institutionalization.9, 17, 18
Improvement in life changes
At 8, 12, 24, and 52 weeks, the TASKII intervention did not significantly affect life changes for the total sample. However, the TASK II program improved caregiver life changes in caregivers with mild to severe depressive symptoms compared to those randomized to the ISR group at 12 weeks. Though life changes were similar for both TASK II and ISR groups across the total sample, it is possible that caregivers with some depressive symptoms experienced more life changes as a result of providing care. Life changes and depressive symptoms have been found to be correlated.10–12 Improvement in life changes in caregivers with some depressive symptoms builds upon our prior work with the original TASK intervention, which had little effect on life changes.33 For the TASK II intervention, we incorporated the BCOS into the intervention during the fifth call with the nurse as an additional assessment, encouraging caregivers to select priority needs that were targeted toward improving their own personal life changes. Further refinement of the TASK II intervention may be to use the BCOS earlier, (e.g., second or third call) to allow caregivers more time to address their own life changes. Only one other intervention study has reported life changes as an outcome in stroke caregivers.43 King and colleagues43 found that life changes improved for a group of caregivers who received a problem-solving intervention immediately post-intervention; however, results were not sustained at 6 months or 1 year, and there were high attrition rates. Generalizability was limited to spousal caregivers. Other intervention studies have measured similar quality of life concepts with mixed results.20 Caregivers commonly experience adverse life changes because they neglect their own needs while providing care, and they often need encouragement to care for themselves.2, 3, 10–12, 36 The TASK II intervention encourages caregivers to attend to the needs of the survivor and their own changes in social functioning, subjective well-being, and physical health.
Reduction of unhealthy days
Most notably, unhealthy days were reduced for the caregivers in the TASK II group compared to those randomized to the ISR group at our primary endpoint of 8 weeks. A trend toward fewer unhealthy days was noted for the TASK II group at 12, 24, and 52 weeks (Figure 2). Future enhancements of the TASK II program may be warranted to include a stronger focus on referring caregivers to health care providers to address their own physical and mental health needs. Addressing health conditions as well as preventive health care measures is important for both stroke survivors and family caregivers. The stroke family caregiver intervention literature is limited with regard to caregiver health;20 only two studies found improvement in general health of the caregiver.43,44 Other studies had non-significant findings using the SF-36 general health subscale.33, 45 TASK II intervention having a significant impact on a global measure of unhealthy days27 underscores the strength of the TASK II intervention and its potential to improve population health in general for family caregivers.
Figure 2.
Change plots by treatment and by time for Depressive Symptoms, Life Changes, and Unhealthy Days.
Limitations
The study employed a convenience sample of stroke caregivers recruited from acute care and inpatient rehabilitation settings in the Midwest where most of the participants were Caucasian and Non-Hispanic. Caregivers were recruited within 8 weeks of the survivor’s discharge to home, making findings less generalizable to long-term caregivers. Caregivers were older (mean age 54–55 years), making findings less applicable to younger caregivers who were also parents of young children. Survivor characteristics were collected by caregiver proxy. Future studies should incorporate more objective data from medical records or directly from the stroke survivors themselves. Finally, there were group differences in protocol adherence, time spent reading materials, and longer call time; although, longer call time with the nurses was used as a covariate in the analyses. While overall adherence for the TASK II group was 80% and the ISR group was 92%, the checklist for the TASK II group included additional items specific to the TASK II intervention that were repetitive and not needed during every call. Comparison of adherence percentages for shared items on the checklist was 90% for the TASK II group and 92% for the ISR group.35
Implications and Future Directions
Despite these limitations, the TASK II intervention is useful. It includes a close connection with current scientific and practice guidelines that recommend assessment of caregiver needs and concerns, as well as the use of a combination of psychoeducational and skill-building strategies.19–22 Training caregivers to assess their own needs and concerns and to address those using individualized skill-building strategies provides a caregiver-driven approach to self-care. The TASK II intervention is unique among intervention studies,20 because it is delivered completely by telephone, making it accessible to caregivers in both rural and urban home settings.32, 33, 35 Key attributes of the nurses delivering the intervention included the hiring of qualified, engaged nurses who had a registered nurses lisence.35 Education level did not matter as much as the quality of communication skills and the ability to follow the caregiver’s lead.35 Nurses commented on how telephone delivery sharpened their listening skills,35 similar to findings from another study in which telephone delivery allowed interveners to develop enhanced listening skills to compensate for the absence of visual cues.46 Future development of the intervention may involve enhanced use of other telehealth modes of delivery such as video, web-based, and remote monitoring technologies.47 The TASK II intervention has a documented track record of treatment fidelity, including structured protocols for nurse training.35 The challenge is how to implement the program into stroke systems of care. Future research is needed to enhance the TASK II program using innovative telehealth technologies and to implement the TASK II program into ongoing systems of stroke care.
Supplementary Material
Acknowledgments
The authors would like to acknowledge the assistance of Phyllis Dexter, PhD, RN, Indiana University School of Nursing, for her helpful review of this manuscript.
Sources of Funding
This study was funded by the National Institutes of Health, National Institute of Nursing Research, R01NR010388, and registered with the clinical trials identifier NCT01275495 https://www.clinicaltrials.gov/ct2/show/NCT01275495?term=Bakas&rank=3.
Footnotes
Clinical Trial Registration-URL: https://www.clinicaltrials.gov/ct2/show/NCT01275495?term=Bakas&rank=3. Unique identifier: NCT01275495 https://www.clinicaltrials.gov/ct2/show/NCT01275495?term=Bakas&rank=3
Disclosures
None.
References
- 1.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. on behalf of the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2015 update: a report from the American Heart Association. Circulation. 2015;131:e29–e322. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 2.Bakas T, Austin JK, Okonkwo KF, Lewis RR, Chadwick LC. Needs, concerns, strategies, and advice of stroke caregivers the first 6 months after discharge. J Neurosci Nurs. 2002;34:242–251. doi: 10.1097/01376517-200210000-00004. [DOI] [PubMed] [Google Scholar]
- 3.King RB, Semik PE. Stroke caregiving: difficult times, resource use, and needs during the first 2 years. J Gerontolog Nurs. 2006;32:37–44. doi: 10.3928/00989134-20060401-07. [DOI] [PubMed] [Google Scholar]
- 4.Quinn K, Murray C, Malone C. Spousal experiences of coping with and adapting to caregiving for a partner who has a stroke: a meta-synthesis of qualitative research. Disabil Rehabil. 2014;36:185–198. doi: 10.3109/09638288.2013.783630. [DOI] [PubMed] [Google Scholar]
- 5.King RB, Hartke RJ, Lee J, Raad J. The Stroke Caregiver Unmet Resource Needs Scale: Development and Psychometric Testing. J Neurosci Nurs. 2013;45:320–328. doi: 10.1097/JNN.0b013e3182a3ce40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ski C, O’Connell B. Stroke: the increasing complexity of carer needs. J Neurosci Nurs. 2007;39:172–179. [PubMed] [Google Scholar]
- 7.Berg AL, Palomaki H, Lonnqvist J, Lehtihalmes ML, Kaste M. Depression Among Caregivers of Stroke Survivors. Stroke. 2005;36:639–643. doi: 10.1161/01.STR.0000155690.04697.c0. [DOI] [PubMed] [Google Scholar]
- 8.Cameron JI, Cheung AM, Streiner DL, Coyte PC, Stewart DE. Stroke survivor depressive symptoms are associated with family caregiver depression during the first 2 years poststroke. Stroke. 2011;42:302–306. doi: 10.1161/STROKEAHA.110.597963. [DOI] [PubMed] [Google Scholar]
- 9.Han B, Haley WE. Family caregiving for patients with stroke: Review and analysis. Stroke. 1999;30:1478–1485. doi: 10.1161/01.str.30.7.1478. [DOI] [PubMed] [Google Scholar]
- 10.Pevroni H, Mohammad-Saeid D, Farahani-Nia M, Hoseini F. The relationship between perceived life changes and depression in caregivers of stroke patients. J Neurosci Nurs. 2012;44:329–336. doi: 10.1097/JNN.0b013e3182682f4c. [DOI] [PubMed] [Google Scholar]
- 11.Bakas T, Champion V, Perkins SM, Farran CJ, Williams CJ. Psychometric testing of the revised 15-item Bakas Caregiving Outcomes Scale. Nurs Res. 2006;55:346–355. doi: 10.1097/00006199-200609000-00007. [DOI] [PubMed] [Google Scholar]
- 12.McLennon SM, Bakas T, Jessup NM, Habermann BH, Weaver MT. Caregiver task difficulty and life changes among stroke family caregivers: relationship to level of depressive symptoms. Arch Phys Med Rehab. 2014;95:2484–2490. doi: 10.1016/j.apmr.2014.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schulz R, Beach SR. Caregiving as a risk factor for mortality: the caregiver health effects study. JAMA. 1999;282:2215–2219. doi: 10.1001/jama.282.23.2215. [DOI] [PubMed] [Google Scholar]
- 14.Chung ML, Bakas T, Plue LD, Williams LS. Effects of self-esteem, optimism, and perceived control on depressive symptoms in stroke survivor-spouse dyads. [Accessed October 15, 2015];J Cardiovasc Nurs. 2015 doi: 10.1097/JCN.0000000000000232. published online ahead of print February 5, 2015. http://journals.lww.com/jcnjournal/pages/articleviewer.aspx?year=9000&issue=00000&article=99639&type=abstract. [DOI] [PMC free article] [PubMed]
- 15.Grant JS, Clay OJ, Keltner NL, Haley WE, Wadley VG, Perkins MM, et al. Does caregiver well-being predict stroke survivor depressive symptoms? A mediation analysis. Top Stroke Rehab. 2013;20:44–51. doi: 10.1310/tsr2001-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Klinedinst NJ, Gebhardt MC, Aycock DM, Nichols-Larsen DS, Uswatte G, Wolf SL, et al. Caregiver characteristics predict stroke survivor quality of life at 4 months and 1 year. Res Nurs Health. 2009;32:592–605. doi: 10.1002/nur.20348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gaugler JE, Duval S, Anderson KA, Kane RL. Predicting nursing home admission in the US: a meta-analysis. BMC Geriatr. 2007;7:13. doi: 10.1186/1471-2318-7-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kao HS, McHugh ML. The role of caregiver gender and caregiver burden in nursing home placements for elderly Taiwanese survivors of stroke. Res Nurs Health. 2004;27:121–134. doi: 10.1002/nur.20007. [DOI] [PubMed] [Google Scholar]
- 19.Miller EL, Murray L, Richards L, Zorowitz RD, Bakas T, Clark P, et al. Comprehensive Overview of Nursing and Interdisciplinary Rehabilitation Care of the Stroke Patient: A Scientific Statement From the American Heart Association. Stroke. 2010;41:2402–2448. doi: 10.1161/STR.0b013e3181e7512b. [DOI] [PubMed] [Google Scholar]
- 20.Bakas T, Clark PC, Kelly-Hayes M, King RB, Lutz BJ, Miller EL on behalf of the American Heart Association Council on Cardiovascular and Stroke Nursing and the Stroke Council. Evidence for stroke family caregiver and dyad interventions: A statement for healthcare professionals from the American Heart Association and American Stroke Association. Stroke. 2014;45:2836–2852. doi: 10.1161/STR.0000000000000033. [DOI] [PubMed] [Google Scholar]
- 21.Duncan PW, Zorowitz R, Bates B, Choi JY, Glasberg JJ, Graham GD, et al. Management of adult stroke rehabilitation care: a clinical practice guideline. Stroke. 2005;36:e100–e143. doi: 10.1161/01.STR.0000180861.54180.FF. [DOI] [PubMed] [Google Scholar]
- 22.Lindsay P, Bayley M, Hellings C, Hill M, Woodbury E, Phillips S on behalf of the Canadian Stroke Strategy, a joint initiative of the Canadian Stroke Network and the Heart and Stroke Foundation of Canada. Canadian Best Practice Recommendations for Stroke Care: Summary. Can Med Assoc J. 2008;179:S1–S25. doi: 10.1503/cmaj.081536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Van Heugten C, Visser-Meily A, Post M, Lindeman E. Care for carers of stroke patients: evidence-based clinical practice guidelines. J Rehabil Med. 2006;38:153–158. doi: 10.1080/16501970500441898. [DOI] [PubMed] [Google Scholar]
- 24.Bakas T, Austin JK, Jessup SL, Williams LS, Oberst MT. Time and difficulty of tasks provided by family caregivers of stroke survivors. J Neurosci Nurs. 2004;36:95–106. doi: 10.1097/01376517-200404000-00007. [DOI] [PubMed] [Google Scholar]
- 25.Callahan CM, Unverzagt FW, Hui SL, Perkins AJ, Hendrie HC. Six-item screener to identify cognitive impairment among potential subjects for clinical research. Med Care. 2002;40:771–781. doi: 10.1097/00005650-200209000-00007. [DOI] [PubMed] [Google Scholar]
- 26.Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Centers for Disease Control and Prevention. Measuring Healthy Days. Atlanta, Georgia: CDC; 2000. [Accessed October 15, 2015]. http://www.cdc.gov/hrqol/pdfs/mhd.pdf. [Google Scholar]
- 28.Cornoni-Huntley J, Brock DB, Ostfeld A, Taylor JO, Wallace RB. Established populations for epidemiological Studies of the elderly Resource Data Book. Washington, DC: U.S. Department of Health and Human Services; 1986. Rep. No. NIH Publication No. 86–2443. [Google Scholar]
- 29.Pearlin LI, Mullan JT, Semple SJ, Skaff MM. Caregiving and the stress process: an overview of concepts and their measures. Gerontologist. 1990;30:583–594. doi: 10.1093/geront/30.5.583. [DOI] [PubMed] [Google Scholar]
- 30.Williams LS, Bakas T, Brizendine E, Plue L, Tu W, Hendrie H, et al. How valid are family proxy assessments of stroke patients’ health-related quality of life? Stroke. 2006;37:2081–2085. doi: 10.1161/01.STR.0000230583.10311.9f. [DOI] [PubMed] [Google Scholar]
- 31.American Heart Association American Stroke Association. Caring for stroke survivors. [Accessed October 15, 2015];Stroke Connection Special Edition. 2010 Krames Patient Education #50-1682. Updated version #50-1699 at https://www.kramesstore.com/OA_HTML/ibeSpringSearchResults_kra.jsp?q=50-1682&ksw001_kswp=OOMAL0WynM_RJgYPjj9waXrJ:S&ksw001_kswp_pses=ZGEEE7D8846BAA57167EE5F7FCF0C4DD8F67543AA034625EC6715051EF6B60530E6640276CC8FB89186C8762EFE1147D01B552E4081BA583B8BCE548B405144C44.
- 32.Bakas T, Farran CJ, Austin JK, Given BA, Johnson EA, Williams LS. Content validity and satisfaction with a stroke caregiver intervention program. J Nurs Scholarship. 2009;41:368–375. doi: 10.1111/j.1547-5069.2009.01282.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bakas T, Farran CJ, Austin JK, Given BA, Johnson EA, Williams LS. Stroke caregiver outcomes from the Telephone Assessment and Skill-Building Kit (TASK) Top Stroke Rehabil. 2009;16:105–121. doi: 10.1310/tsr1602-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Borrelli B, Sepinwall D, Ernst D, Bellg AJ, Czajkowski S, Breger R, et al. A new tool to assess treatment fidelity and evaluation of treatment fidelity across 10 years of health behavior research. J Consult Clin Psych. 2005;73:852–860. doi: 10.1037/0022-006X.73.5.852. [DOI] [PubMed] [Google Scholar]
- 35.McLennon SM, Hancock RD, Redelman K, Scarton LJ, Riley E, Sweeney B, et al. Comparing treatment fidelity between study arms of a randomized controlled clinical trial for stroke family caregivers. [Accessed October 15, 2015];Clin Rehabil. doi: 10.1177/0269215515585134. published online ahead of print May 7, 2015. http://cre.sagepub.com/content/early/2015/05/05/0269215515585134.full.pdf+html. [DOI] [PMC free article] [PubMed]
- 36.Cameron JI, Naglie G, Silver FL, Gignac MAM. Stroke family caregivers’ support needs change across the care continuum: a qualitative study using the timing it right framework. Disabil Rehabil. 2013;34:315–324. doi: 10.3109/09638288.2012.691937. [DOI] [PubMed] [Google Scholar]
- 37.Cameron JI, Tsoi C, Marsella A. Optimising stroke systems of care by enhancing transitions across care environments. Stroke. 2008;39:2637–2643. doi: 10.1161/STROKEAHA.107.501064. [DOI] [PubMed] [Google Scholar]
- 38.SAS Institute Inc. What’s New in SAS® 9.4. Cary, NC: SAS Institute Inc; 2013. [Google Scholar]
- 39.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap) – a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Allison PD. Change scores as dependent variables in regression analysis. Sociological Methodology. 1990;20:93–114. [Google Scholar]
- 41.Fitzmaurice GM, Laird NM, Ware JH. Applied Longitudinal Analysis. 2. Hoboken, New Jersey: John Wiley & Sons; 2004. [Google Scholar]
- 42.Kalra L, Evans A, Perez I, Melbourn A, Patel A, Knapp M, et al. Training carers of stroke patients: randomised controlled trial. BMJ. 2004;328:1099. doi: 10.1136/bmj.328.7448.1099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.King RB, Hartke RJ, Houle T, Lee J, Herring G, Alexander-Peterson BS, et al. A problem solving early intervention for stroke caregivers: one year follow up. Rehabil Nurs. 2012;37:231–243. doi: 10.1002/rnj.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mant J, Carter J, Wade DT, Winner S. Family support for stroke: a randomized controlled trial. Lancet. 2000;356:808–813. doi: 10.1016/S0140-6736(00)02655-6. [DOI] [PubMed] [Google Scholar]
- 45.Grant JS, Elliott TR, Weaver M, Bartolucci AA, Giger JN. Telephone intervention with family caregivers of stroke survivors after rehabilitation. Stroke. 2002;33:2060–2065. doi: 10.1161/01.str.0000020711.38824.e3. [DOI] [PubMed] [Google Scholar]
- 46.Pettinari CJ, Jessopp L. “Your ears become your eyes”: managing the absence of visibility in NHS Direct. J Adv Nurs. 2001;36:668–675. doi: 10.1046/j.1365-2648.2001.02031.x. [DOI] [PubMed] [Google Scholar]
- 47.Chi N, Demiris D. A systematic review of telehealth tools and interventions to support family caregivers. Journal of Telemedicine and Telecare. 2015;21:37–44. doi: 10.1177/1357633X14562734. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.