Abstract
The objective of this study was to investigate the associations between the NICU work environment, quality of care, safety, and patient outcomes. A secondary analysis was conducted of responses of 1247 NICU staff nurses in 171 hospitals to a large nurse survey. Better work environments were associated with higher odds of nurses reporting poor quality, safety and outcomes. Improving the work environment may be a promising strategy to achieve safer settings for at-risk newborns.
Keywords: neonatal intensive care, nursing, quality of care, safety, work environment
Critically ill infants cared for in the neonatal intensive care unit (NICU) are among the most vulnerable patient populations in the hospital. NICU infants are at increased risk for adverse outcomes related to quality and safety, including nosocomial infection and unplanned readmission to the hospital. Nosocomial infection affects nearly 1 in 6 very low birthweight (VLBW) infants,1 doubling the risk of mortality and lengthening the hospital stay.2,3 Central line catheters, which are required for many NICU infants, are a common source of nosocomial infection, which is a perinatal quality standard.4,5 NICU infants also have a relatively high rate of readmission,6 partly due to the complexity of their care needs at discharge.7 Adequate preparation of parents for the infants’ care needs is essential.8 The transition from the highly-controlled intensive care environment, where clinicians are the principal caregivers, to the home setting can be challenging for some families. Common challenges include managing respiratory distress, feeding and growth, and jaundice.7
Despite the unique challenges of caregiving in this setting, little research has explored the organizational context in which NICU care is provided—specifically, the work environment of the clinicians who provide the majority of clinical care. Registered nurses (RNs) are instrumental in achieving multiple care goals, including promoting infant health and clinical stability, maintaining the integrity and cleanliness of central catheters, and preparing families for their role in infant care and successful transition to home. NICU nurses monitor infants for subtle cues and provide timely interventions to prevent the development of morbidity or to prevent further clinical decline if morbidity develops.9
Considerable evidence has linked the work environment to patient outcomes in adult populations;10-13 however, research is limited about NICU work environments and outcomes, particularly related to patient safety and quality of care. Superior nursing work environments as promulgated through achievement of hospital Magnet status are associated with better VLBW infant outcomes, including mortality, nosocomial infection, and severe intraventricular hemorrhage.14 Evidence from 9 NICUs in Canada indicates a link between the work environment, care rationing (ie, nursing care activities omitted for lack of time), and nurse-assessed quality of care.15 A study of 104 US NICUs documented that variation in NICU work environments is associated with breastfeeding support for parents; breast milk is a perinatal quality standard.16,17 Finally, one aspect of the work environment, nurse staffing, has been linked to nosocomial infection in the NICU.2,18 However, none of these studies have integrated the perspectives of NICU RNs who are in a unique position to report on the state of nurse work environments, quality and patient safety in US NICUs.
The objective of this study was to investigate the associations between the NICU work environment and nurse reports of quality of care, safety, and NICU-relevant outcomes related to infection and patient/family readiness for discharge in a large group of US NICUs. These relationships were examined using nurse survey data that were collected in four large, geographically diverse states.
METHODS
This study used a secondary analysis of cross-sectional linked nurse survey and administrative hospital data. The objectives of the parent study were similar to the current study, which assured a congruent conceptual focus of the data. Institutional review board approval was obtained for the study protocol.
Samples and setting
In the parent study, the Multistate Study of Nursing Care and Patient Safety,13 conducted in 2005-2008, large, random samples of RNs licensed in 4 states (Pennsylvania, New Jersey, California, Florida) were surveyed. Respondents reported their employing hospital, yielding nurse survey data about 665 hospitals.13
The present study focuses on the subset of hospitals with a sufficient number of NICU staff nurses to yield reliable NICU-level measures. The nurse inclusion criterion was being a NICU staff nurse. The hospital inclusion criterion was a minimum of 3 NICU staff nurse survey respondents. The minimum number of respondents per nursing unit was consistent with prior work19 and supported by satisfactory aggregate reliability statistics for study measures, as reported below. These criteria yielded samples of 171 hospitals and 1,247 nurses. The average number of nurse respondents per hospital was 7.3. The sample hospitals represent 20% of NICUs nationally, based on authors’ calculations from AHA data on hospitals with nonzero NICU beds.
Measures
The outcome and explanatory variables were measured from nurse survey questions and tools described below.
Nurse-reported quality of care, safety and patient outcomes
Nurses rated the overall quality of care provided on their unit using a 4-point scale (poor to excellent), an item validated with outcomes from administrative patient data.20 Reponses of poor or fair were classified as poor quality of care. Nurses reported an overall safety grade for their unit from A (excellent) to F (failing), using an item from the Agency for Healthcare Research and Quality's hospital survey on patient safety culture.21 Responses of C, D, and F were classified as poor safety grade. Nurses reported the frequency of central line associated blood stream infection on a 7-item scale (“never” to “every day”). Responses of a few times a month or more frequent were classified as frequent. Nurses reported their confidence in the ability of their patients to manage their care at discharge using a 4-point scale (very to not at all). For this study, these assessments were interpreted as reflecting parental ability to care for the infant at discharge. Some nurses (18%) considered this query not applicable, likely because the patients were infants. The not applicable responses were omitted. Responses of somewhat and not at all confident were classified as not confident.
Work environment
The work environment was measured by the Practice Environment Scale of the Nursing Work Index (PES-NWI).22 This 31-item validated tool has been endorsed by the National Quality Forum since 2004 and is used extensively worldwide.23-25 For each item, the nurse responds to the query “to what extent do you agree the item is present in your current job?” with 4 response options (strongly disagree to strongly agree). Higher scores indicate a workplace supportive of professional nursing practice.22 The PES-NWI comprises 5 subscales representing the domains: Nurse Participation in Hospital Affairs, Nursing Foundations for Quality of Care, Nurse Manager Ability, Leadership and Support of Nurses, Staffing and Resource Adequacy, and Collegial Nurse-Physician Relations. Subscales items are averaged to compute a subscale score. A composite is the average of subscale scores.
To measure the work environment at the aggregate level, the intraclass correlation coefficient (ICC [1,k]) should be at least .60.26 Using responses of at least 3 nurses, the ICC of 4 of the 5 PES-NWI subscales exceeded this criterion and the fifth was considered satisfactory at .58. Hospitals were classified into 3 categories using methods described previously.27,28 Hospitals with average subscale scores above the sample median for 4 or 5 subscales were classified as having better environments, for 2 or 3 subscales as having mixed environments, and for 0 or 1 subscale as having poor environments.
Covariates
NICU nurse staffing was computed as the average number of patients cared for on the last shift among nurses reporting from 1 to 6 patients on their last shift. Nurses with 0 or more than 6 patients (n = 42; 3%) were excluded to retain nurses providing direct patient care and omit nurses in roles such as charge or resource nurse. Nurse age, sex, education and experience were used to describe the sample. The following hospital characteristics, obtained from the AHA Annual Survey database, were used to describe the sample or as controls in regression models: number of hospital acute care beds, teaching status, technology status, and number of neonatal intensive plus intermediate care beds. The number of NICU beds was missing for one-third of hospitals. Teaching status was classified based on the resident to bed ratio: none, less than 1:4 (minor), and 1:4 or greater (major). Hospitals with the capability for open heart surgery and/or organ transplantation were classified as high technology. Additionally, NICUs were classified into levels of care II, IIIa, and IIIb using the American Academy of Pediatrics (AAP) classification system.29 Data on classification level were provided by the Vermont Oxford Network, a voluntary NICU quality collaborative. NICU level of care was not available for the one-fourth of sample NICUs not in the network.
Analysis
To describe the hospital and NICU nursing characteristics, and the outcome and explanatory variables, central tendencies and percent distributions are presented. Differences in the 4 outcomes across hospital work environment subgroups were tested using analysis of variance. The effect of work environment on the likelihood of nurses reporting poor quality and safety outcomes was examined using logistic regression models. These models accounted for clustering of nurses within hospitals by adjusting the standard errors using the Huber-White sandwich estimator. Adjusted models included controls for NICU-level nurse staffing, state, hospital size, teaching, and technology status. Sensitivity analyses were conducted in the subsamples of hospitals with complete data on NICU beds (n = 138) and NICU classification (n = 130), which would be appropriate control variables. To test robustness of results, analyses were replicated in the subsample of 112 hospitals with at least 5 NICU nurses. The regression results were essentially identical in direction, magnitude, and significance to the results from the original sample. We report the results from the original sample, which reflects a larger fraction of US NICUs. All analyses were performed using Stata software version 13.0.30
RESULTS
The majority of sample hospitals had 250 or more beds (76%), were classified as teaching hospitals (66%), and had high-technology capabilities (68%). The average NICU in the sample had 28 beds (SD = 19, n = 138). All descriptive statistics are reported in the aggregate (ie, NICU-level). On average, nurses cared for 2.6 patients on their last shift (NICU-level SD = 0.58) and had 10.9 years of RN experience on their current unit (NICU-level SD = 4.4 years). Almost half (49%) of nurses held a BSN or higher (SD across NICUs = 23%). The average NICU-level PES-NWI composite score was 2.88 (range across NICUs 1.93 to 3.79; SD across NICUs = .32). The scores differed significantly in the 3 subgroups: 3.19 in better environments; 2.86 in mixed; and 2.54 in poor (P < .001).
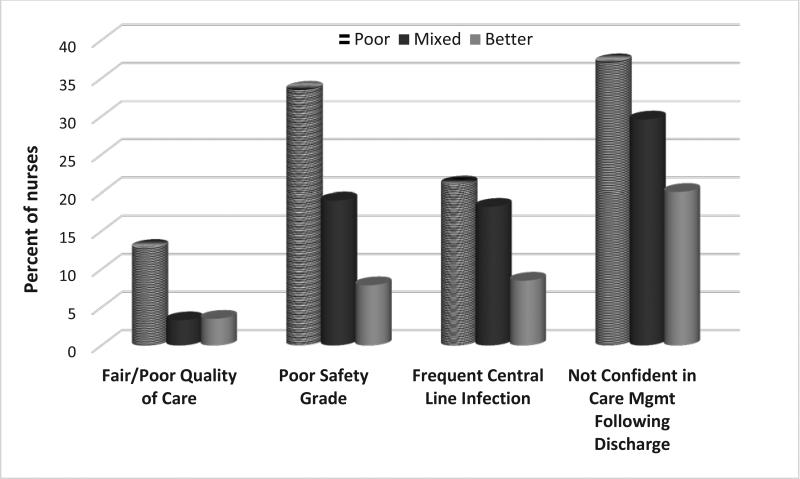
Overall, 6% of nurses reported fair/poor quality of care overall on their unit, while 20% gave their unit a poor grade on patient safety. Frequent central line infections (occurring once a month or more) were reported by 16% of nurses. More than one-quarter (29%) reported that they were not confident in parents’ ability to manage their infant's care after discharge. Differences in these outcomes were observed by work environment types, with decreasing percentages of nurses reporting poor quality and safety outcomes as the work environment improved (Figure 1). For example, one-third of nurses in poor practice environments (34%) gave their unit a poor safety grade, compared to 19% in mixed environments, and 8% in better environments (p<0.001). Similar patterns were observed for the other 3 outcomes, all of which were statistically significant.
Figure 1.
Percent of nurses reporting NICU quality and safety outcomes by work environment category
Fair/Poor Quality of Care: Nurse Rating of quality of nursing care delivered to patients as fair or poor (n= 1237)
Poor Safety Grade: Nurse rating of unit safety as acceptable, poor, or failing (n = 1242)
Frequent Central Line Infection: Nurse rating of frequent central line infection as a few times a month or more (n = 1194)
Not Confident in Discharge Care: Nurse rating of patient ability to manage care at discharge as somewhat or not at all confident (n = 1017)
Table 1 presents the results of the adjusted logistic regression analyses that estimated the effect of work environment on the 4 nurse-reported quality and safety outcomes. In the better environments, compared to the poor environments, nurses were 66% less likely to report fair/poor quality of care on their unit, 80% less likely to report poor safety grade, 68% less likely to report frequent central line infections and 51% less likely to report poor confidence in parents’ ability to manage their infant's care after discharge (all p<0.001). The sensitivity analyses in the two subsamples with complete data on number of NICU beds and NICU AAP classification yielded odds ratios with the same direction and significance as the full sample but smaller effect sizes.
Table 1.
Odds ratios estimating the effect of work environment on nurse-reported NICU quality and safety outcomes
| Adjusted |
|||
|---|---|---|---|
| NICU Outcome | OR | (95% CI) | P |
| Fair/Poor Quality of Care (n = 1237) | |||
| Poor Environment (reference) | |||
| Mixed Environment | 0.32 | 0.17-0.59 | <.001 |
| Better Environment | 0.34 | 0.20-0.59 | <.001 |
| Poor Safety Grade (n = 1242) | |||
| Poor Environment (reference) | |||
| Mixed Environment | 0.58 | 0.39-0.86 | .007 |
| Better Environment | 0.20 | 0.13-0.31 | <.001 |
| Frequent Central Line Infection a few times a month or more (n = 1194) | |||
| Poor Environment (reference) | |||
| Mixed Environment | 0.89 | 0.49-1.61 | .693 |
| Better Environment | 0.32 | 0.18-0.58 | <.001 |
| Not confident in care management following discharge (n = 1017) | |||
| Poor Environment (reference) | |||
| Mixed Environment | 0.84 | 0.60-1.19 | .326 |
| Better Environment | 0.49 | 0.33-0.72 | <.001 |
Note: OR=odds ratio, CI=confidence interval, NICU = Neonatal Intensive Care Unit. Models control for staffing and hospital characteristics (hospital state, teaching status, technology status, and size).
The n varies for each outcome (n=1017 to 1242) due to different response rates.
DISCUSSION
Our results provide strong evidence that environments supportive of professional nursing practice are linked to the well-being of critically ill infants. Significantly fewer nurses (about one-quarter the number) in the better NICU work environments say that quality or safety is poor compared to the poor environments. Our multivariable analyses show that these nurses were 51 to 80% less likely to report poor quality and safety than nurses in the poor environments, controlling for nurse staffing and other hospital characteristics. These large effects suggest that the variation in nurses’ practice environments warrant the attention of nursing, medical, and hospital leaders to achieve safer, optimal care quality for these infants.
Infections in this population are an ongoing concern due to the health risks, including higher mortality and the longer hospital stays that infections require. NICUs routinely track infections due to their grave consequences. Central line infections were reported as frequent by 16% of NICU staff nurses. In the better environments, less than half as many nurses reported frequent infections (9%) as compared to the poorest environments (21%). While life threatening, these infections can be prevented by the implementation of evidence-based actions, enforced by policy and unit leadership. These actions include appropriate hand hygiene and central line care practices which can dramatically reduce nosocomial infections.31,32
Transition home in this population is particularly complex, given the developmental needs of NICU newborns and parents. The successful preparation of families for discharge entails an organizational context that supports expert nursing care. In addition to surveillance of the infant, nurses also assess parents’ engagement with their newborn, their newborn care, and parenting capabilities.33 We found that nearly 4 in 10 nurses working in poor environments were not confident that parents could manage their infant's care after discharge. However, in the better work environments, this fraction was significantly lower (1 in 5), indicating parents are better prepared for the transition to home. Our results align with those of the study of missed nursing care in nine Canadian NICUs, which showed that the care domains most strongly affected by the work environment were discharge planning and parental teaching.15 Together, this evidence suggests that poor work environments thwart the completion of required nursing care in these domains and consequently parents may not be adequately prepared to manage the infant's needs upon discharge.
Exactly how better work environments support NICU safety and quality outcomes is an area ripe for research. Better work environments may support evidence-based infection prevention practices and quality improvement initiatives that are nurse driven. Better work environments may support nurses to increase parental visitation and participation in infant care and decision making34-36, which may facilitate infant health and smoother transition to home, as well as greater parent confidence and satisfaction with care.8,37 Research that reveals the mechanisms linking environments to outcomes would bolster management motivation and efforts to improve environments.
Our findings are consistent with a similar study linking the nurse work environment to health care–associated infections in adult critical care.12 The mean work environment rating (i.e., the PES-NWI composite score) in this NICU sample (2.88) is almost 2/3 SD higher than that reported in adult critical care settings (2.68), but lower than reported in a 2008 study of 104 Vermont Oxford Network NICUs nationally16: (3.06; range 2.42 to 3.97), which may reflect better environments of NICUs that have the motivation and capacity to participate in a NICU quality collaborative. A composite of 2.88 indicates that NICU nurses tend toward a response of “agree” (3.00) but not “strongly agree” (4.00) that organizational traits supportive of professional practice are present. Notably, the NICUs in this sample exhibited a wide range of composite scores from 1.93 to 3.79, demonstrating the potential for improvement.
Our results support the conclusions of the World Health Organization's World Alliance for Patient Safety38 and Institute of Medicine39 that the organizational context of care is as, or possibly more, important than the actions of individual providers in keeping patients safe. Hospitals can and do improve their work environments over time, and those that succeed experience improved outcomes.40 One approach to improving the work environment is to use nationally endorsed measures to identify areas of work environment weakness. Benchmarking databases like the National Database of Nursing Quality Indicators provide comparisons to peer institutions to assist in these efforts. NICU managers could motivate improvements by comparing the quality of their work environment and the rates of poor outcomes from evidence presented here. Pursuing Magnet hospital designation is a hospital-wide approach to improving work environments.41,42
Limitations
The necessity of using cross-sectional data limits causal inference, which points to the need to study changes in work environments over time and their impact. The safety orientation of the NICU has increased since the data were generated in 2005-2008. However, the differences across hospitals in NICU work environments and outcomes have been documented in more recent data,43 suggesting that these relationships persist. Specifically, data from the same work environment instrument from 104 NICUs nationally in 2008 demonstrate that NICUs with poorer work environments have higher rates of nosocomial infection.43 The sample NICUs are located in 4 large states, and although there is little reason to think that NICU care differs across these states, we included state dummy variables to take any state differences into account. Data on actual infection rates were not available to corroborate nurse reports, although previous research has shown that nurse reports of quality are accurate predictors of mortality rates and other patient outcomes.20 Research linking NICU environments to patient outcomes would bolster this nurse-report-based evidence, as has been demonstrated in adult critical care.12,44 NICU level of care data, according to the American Academy of Pediatrics classification, were incomplete, which limited our ability to fully account for patient acuity. Sensitivity analyses that were conducted on subsamples with complete data for NICU beds and AAP classification yielded similar results to those presented in this paper.
CONCLUSIONS
Quality and safety vary considerably across US NICUs and the nurse work environment appears to be a key organizational factor that underlies NICU outcomes. The essential component of neonatal intensive care for infants at high risk of poor outcomes is professional nursing care in environments that enable nurses to provide high-quality care to infants and their parents. As shown in our study, there is plenty of room for improvement in NICU work environments, patient safety, and quality of care. NICU staff nurses are best positioned to work with their managers to identify and address safety weaknesses as well as parental preparation for transition to home. Improving work environments may be a promising strategy for substantially improving the outcomes of some of the most vulnerable patients in our hospitals.
Acknowledgments
Funding Support: This research was funded by grants to the Center for Health Outcomes and Policy Research from the National Institute of Nursing Research (T32-NR-007104 and R01-NR-004513, L. Aiken, PI) and Pennsylvania Hospital.
Footnotes
The authors declare no conflict of interest.
References
- 1.Horbar JD, Carpenter JH, Badger GJ, et al. Mortality and neonatal morbidity among infants 501 to 1500 grams from 2000 to 2009. Pediatrics. 2012;129(6):1019–1026. doi: 10.1542/peds.2011-3028. [DOI] [PubMed] [Google Scholar]
- 2.Rogowski J, Staiger D, Patrick T, Horbar J, Kenny MJ, Lake E. Nurse staffing and NICU infection rates. JAMA Pediatr. 2013;167(5):444–450. doi: 10.1001/jamapediatrics.2013.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Payne N, Carpenter J, Badger G, Horbar J, Rogowski J. Marginal increase in cost and excess length of stay associated with nosocomial bloodstream infections in surviving very low birth weight infants. Pediatrics. 2004;114(2):348–355. doi: 10.1542/peds.114.2.348. [DOI] [PubMed] [Google Scholar]
- 4.The Joint Commission Performance Measure PC-04: Health Care-Associated Bloodstream Infections in Newborns. Specifications Manual for Joint Commission National Quality Measures (v2014A1) 2014 https://manual.jointcommission.org/releases/TJC2014A1/MIF0169.html.
- 5.National Quality Forum Neonatal Blood Stream Infection Rate (NQI #3) 2013 http://www.qualityforum.org/QPS/00478.
- 6.Escobar GJ, McCormick MC, Zupancic JAF, et al. Unstudied infants: outcomes of moderately premature infants in the neonatal intensive care unit. Arch Dis Child Fetal Neonatal Ed. 2006;91(4):F238–F244. doi: 10.1136/adc.2005.087031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.American Academy of Pediatrics - American Committee on Fetus and Newborn Hospital Discharge of the High-Risk Neonate. Pediatrics. 2008;122(5):1119–1126. doi: 10.1542/peds.2008-2174. [DOI] [PubMed] [Google Scholar]
- 8.Griffin T, Abraham M. Transition to home from the newborn intensive care unit: applying the principles of family-centered care to the discharge process. J Perinat Neonatal Nurs. 2006;20(3):243–249. doi: 10.1097/00005237-200607000-00012. [DOI] [PubMed] [Google Scholar]
- 9.Cricco-Lizza R. Everyday nursing practice values in the NICU and their reflection on breastfeeding promotion. Qual Health Res. 2011;21(3):399–409. doi: 10.1177/1049732310379239. [DOI] [PubMed] [Google Scholar]
- 10.Friese CR, Lake ET, Aiken LH, Silber J, Sochalski JA. Hospital nurse practice environments and outcomes for surgical oncology patients. Health Serv Res. 2008;43(4):1145–1163. doi: 10.1111/j.1475-6773.2007.00825.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Aiken LH, Clarke SP, Sloane DM, Lake ET, Cheney T. Effects of hospital care environments on patient mortality and nursing outcomes. J Nurs Adm. 2008;38(5):223–229. doi: 10.1097/01.NNA.0000312773.42352.d7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kelly D, Kutney-Lee A, Lake ET, Aiken LH. The critical care work environment and nurse-reported health care-associated infections. Am J Crit Care. 2013 Nov;22(6):482–488. doi: 10.4037/ajcc2013298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Aiken LH, Cimiotti JP, Sloane DM, Smith HL, Flynn L, Neff D. The effects of nurse staffing and nurse education on patient deaths in hospitals with different nurse work environments. Med Care. 2011;49(12):1047–1053. doi: 10.1097/MLR.0b013e3182330b6e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lake ET, Staiger D, Horbar J, et al. Association between hospital recognition for nursing excellence and outcomes of very low birth weight infants. JAMA. 2012;307(16):1709–1716. doi: 10.1001/jama.2012.504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rochefort CM, Clarke SP. Nurses’ work environments, care rationing, job outcomes, and quality of care on neonatal units. J Adv Nurs. 2010;66(10):2213–2224. doi: 10.1111/j.1365-2648.2010.05376.x. [DOI] [PubMed] [Google Scholar]
- 16.Hallowell SG, Spatz DL, Hanlon AL, Rogowski JA, Lake ET. Characteristics of the NICU work environment associated with breastfeeding support. Adv Neonatal Care. 2014;14(4):290–300. doi: 10.1097/ANC.0000000000000102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.The Joint Commission Performance Measure PC-05: Exclusive Breast Milk Feeding Considering Mother's Choice. Specifications Manual for Joint Commission National Quality Measures (v2014A1) 2014 https://manual.jointcommission.org/releases/TJC2014A1/MIF0170.html.
- 18.Cimiotti JP, Haas J, Saiman L, Larson EL. Impact of staffing on bloodstream infections in the neonatal intensive care unit. Arch Pediatr Adolesc Med. 2006;160(8):832–836. doi: 10.1001/archpedi.160.8.832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hanrahan NP. Measuring inpatient psychiatric environments: psychometric properties of the practice environment scale-nursing work index (PES-NWI). Int J Psychiatr Nurs Res. 2007;12(3):1521–1527. [PubMed] [Google Scholar]
- 20.McHugh MD, Stimpfel AW. Nurse reported quality of care: A measure of hospital quality. Res Nurs Health. 2012;35(6):566–575. doi: 10.1002/nur.21503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sorra J, Nieva V. Hospital Survey on Patient Safety Culture. Agency for Healthcare Research and Quality; Rockville: 2004. [September 10, 2013]. (Prepared by Westat, Rockville, MD, under contract No. 290-96-0004). http://www.ahrq.gov/qual/patientsafetyculture/hospcult.pdf. [Google Scholar]
- 22.Lake ET. Development of the practice environment scale of the nursing work index. Res Nurs Health. 2002;25(3):176–188. doi: 10.1002/nur.10032. [DOI] [PubMed] [Google Scholar]
- 23.National Quality Forum [July 21, 2014];Practice Environment Scale - Nursing Work Index (PES-NWI) (composite and five subscales) 2014 http://www.qualityforum.org/QPS/0206.
- 24.Aiken LH, Sloane DM, Bruyneel L, Van den Heede K, Sermeus W. Nurses’ reports of working conditions and hospital quality of care in 12 countries in Europe. Int J Nurs Stud. 2013;50(2):143–153. doi: 10.1016/j.ijnurstu.2012.11.009. [DOI] [PubMed] [Google Scholar]
- 25.Warshawsky NE, Havens DS. Global use of the practice environment scale of the nursing work index. Nurs Res. 2010;60(1):17–31. doi: 10.1097/NNR.0b013e3181ffa79c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Glick WH. Conceptualizing and measuring organizational and psychological climate: Pitfalls in multilevel research. Acad Manage Rev. 1985;10(3):601–616. [Google Scholar]
- 27.Aiken LH, Sloane DM, Clarke S, et al. Importance of work environments on hospital outcomes in nine countries. Int J Qual Health Care. 2011 May;11:2011. doi: 10.1093/intqhc/mzr022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Liu K, You L-M, Chen S-X, et al. The relationship between hospital work environment and nurse outcomes in Guangdong, China: A nurse questionnaire survey. J Clin Nurs. 2012 doi: 10.1111/j.1365-2702.2011.03991.x. no-no. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.American Academy of Pediatrics Levels of Neonatal Care. Pediatrics. 2004;114(5):1341–1347. doi: 10.1542/peds.2004-1697. [DOI] [PubMed] [Google Scholar]
- 30.StataCorp . Stata/IC 13.1 for Windows. College Station, TX: 2014. [Google Scholar]
- 31.Larson EL, Cimiotti J, Haas J, et al. Effect of antiseptic handwashing vs alcohol sanitizer on health care–associated infections in neonatal intensive care units. Arch Pediatr Adolesc Med. 2005;159(4):377–383. doi: 10.1001/archpedi.159.4.377. [DOI] [PubMed] [Google Scholar]
- 32.Rosenthal VDMD, Dueñas LMD, Sobreyra-Oropeza MMD, et al. Findings of the International Nosocomial Infection Control Consortium (INICC), Part III: Effectiveness of a multidimensional infection control approach to reduce central line–associated bloodstream infections in the neonatal intensive care units of 4 developing countries. Infect Control Hosp Epidemiol. 2013;34(3):229–237. doi: 10.1086/669511. [DOI] [PubMed] [Google Scholar]
- 33.Gooding JS, Cooper LG, Blaine AI, Franck LS, Howse JL, Berns SD. Family support and family-centered care in the neonatal intensive care unit: origins, advances, impact. Paper presented at: Seminars in Perinatology. 2011 doi: 10.1053/j.semperi.2010.10.004. [DOI] [PubMed] [Google Scholar]
- 34.Melnyk BM, Feinstein NF, Alpert-Gillis L, et al. Reducing premature infants' length of stay and improving parents’ mental health outcomes with the Creating Opportunities for Parent Empowerment (COPE) neonatal intensive care unit program: a randomized, controlled trial. Pediatrics. 2006;118(5):e1414–e1427. doi: 10.1542/peds.2005-2580. [DOI] [PubMed] [Google Scholar]
- 35.Reynolds LC, Duncan MM, Smith GC, et al. Parental presence and holding in the neonatal intensive care unit and associations with early neurobehavior. J Perinatol. 2013;33(8):636–641. doi: 10.1038/jp.2013.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dunn MS, Reilly MC, Johnston AM, Hoopes RD, Abraham MR. Development and dissemination of potentially better practices for the provision of family-centered care in neonatology: the family-centered care map. Pediatrics. 2006;118(Supplement 2):S95–S107. doi: 10.1542/peds.2006-0913F. [DOI] [PubMed] [Google Scholar]
- 37.Sneath N. Discharge teaching in the NICU: are parents prepared? An integrative review of parents' perceptions. Neonatal Netw. 2009;28(4):237–246. doi: 10.1891/0730-0832.28.4.237. [DOI] [PubMed] [Google Scholar]
- 38.World Health Organization Global priorities for patient safety research. 2009 doi: 10.1136/bmj.b1775. [DOI] [PubMed] [Google Scholar]
- 39.Institute of Medicine . Keeping Patients Safe: Transforming the Work Environment of Nurses. The National Academies Press; Washington, DC: 2003. [PubMed] [Google Scholar]
- 40.Kutney-Lee A, Wu ES, Sloane DM, Aiken LH. Effect of changes in hospital nurse work environments and nurse job outcomes: An analysis of panel data. Int J Nurs Stud. 2013;50(2):195–201. doi: 10.1016/j.ijnurstu.2012.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.McHugh MD, Kelly LA, Smith HL, Wu ES, Vanak J, Aiken LH. Lower mortality in Magnet hospitals. Med Care. 2012;51(5):382–888. doi: 10.1097/MLR.0b013e3182726cc5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kelly LA, McHugh MD, Aiken LH. Nurse Outcomes in Magnet® and Non-Magnet Hospitals. J Nurs Adm. 2011;41(10):428–433. doi: 10.1097/NNA.0b013e31822eddbc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lake ET, Staiger D, Patrick T, Horbar J, Kenny MJ, Rogowski J. Disparities in perinatal quality outcomes for very low birth weight infants in neonatal intensive care. Health Serv Res. 2014 doi: 10.1111/1475-6773.12225. EarlyView September 22, 2014. http://onlinelibrary.wiley.com/doi/10.1111/1475-6773.12225/abstract. [DOI] [PMC free article] [PubMed]
- 44.Kelly DM, Kutney-Lee A, McHugh MD, Sloane DM, Aiken LH. Impact of critical care nursing on 30-day mortality of mechanically ventilated older adults*. Crit Care Med. 2014 May;42(5):1089–1095. doi: 10.1097/CCM.0000000000000127. [DOI] [PMC free article] [PubMed] [Google Scholar]