Abstract
Whether operative treatment for complex proximal humeral fractures (CPHFs) has a greater benefit over non-operative treatment remains controversial. There is no consensus on the optimal treatment in elderly patients with CPHFs. This updated meta-analysis of randomized controlled trials (RCTs) aims to investigate whether operative treatment is superior to non-operative treatment in CPHFs. The authors searched RCTs in the electronic databases (Cochrane Central Register of Controlled Trials, PubMed, EMBASE, Medline, Embase, Springer Link, Web of Knowledge, OVID and Google Scholar) from their establishment to July 2015. Researches on operative and non-operative treatment for CPHFs were selected in this meta-analysis. The quality of all studies was assessed and effective data was pooled for this meta-analysis. Outcome measurements were functional status include constant scores (CS scores) and disabilities of the arm, shoulder and hand scores (DASH scores), total complication rates and healthy-related quality of life. The meta-analysis was performed with software revman 5.3. Nine articles with a total 518 patients (average age 70.93) met inclusion criteria. Patients were followed up for at least 1 year in all the studies. No statistical differences were found between operative and non-operative treatment in CS scores at 12 mo (months) [MD 1.06 95 % CI (−3.51, 5.62)] and 24 mo [MD −0.61 95 % CI (−5.87, 4.65)]. There are also no statistical differences between operative and non-operative treatment in DASH scores at 12 mo [MD −4.51 95 % CI (−13.49, 4.47)] and 24 mo [MD −7.43 95 % CI (−16.14, 1.27)]. Statistical differences were found between operative and non-operative treatment in total complication rates [RR 1.55, 95 % CI (1.24, 1.94)]. Statistical differences in EQ-5D at 24 mo [MD 0.15, 95 % CI (0.05, 0.24)] were found between operative and non-operative treatment but no statistical differences were found in ED-5D at 12 mo [MD 0.08, 95 % CI (−0.01, 0.17)], 15D at 12 mo [MD 0.02, 95 % CI (−0.68, 0.73)] and 15D at 24 mo [MD 0.02, 95 % CI (−0.07, 0.83)]. Operative treatments did not significantly improve the functional outcome and healthy-related quality of life in elderly patients. Instead, Operative treatment for CPHFs led to higher incidence of postoperative complications.
Keywords: Operative, Non-operative treatment, Complex proximal humeral fractures (CPHFs), Meta-analysis, Randomized controlled trials (RCTs)
Background
Proximal humeral fractures are common injuries that comprises 5–6 % of all adult fractures, with the incidence of 63.0/105 per year (Bengner et al. 1988; Baron et al. 1996a, b). It is the third most common fracture after hip and wrist fractures that occur in patients older than 60 years (Roux et al. 2012; Horak and Nilsson 1975; Kannus et al. 1996). The fractures are common in patients older than 60 years especially females. Nearly 85 % proximal humeral fractures are non- or minimally displaced and can be treated conservatively (Roux et al. 2012). Many patients could regain shoulder function with non-operative treatment (Yuksel et al. 2011). The remaining 15 % displaced fractures which are challenge to surgeons can be treated with operative or non-operative treatment (Kim et al. 2012; Handoll and Ollivere 2010). These fractures include 2-part fractures involving the surgical neck, 3- and 4-part fractures which all have poor outcomes and the optimal treatment is still controversial. With recent advancement in technique and implants for fracture fixation (Russo et al. 2013; Lill et al. 2013; Vundelinckx et al. 2012), operative treatment has become increasingly popular for these injuries (Karataglis et al. 2011), including internal fixation (Jost et al. 2013) and humeral head replacement (Cadet and Ahmad 2012), which increased treatment costs for this fracture. While non-operative treatment includes sling immobilization (Yuksel et al. 2011).
To date, meta-analysis comparing conservation with operative treatment for proximal humeral fractures have been available in recent years (Sun et al. 2015; Mao et al. 2014; Jia et al. 2014; Fu et al. 2014; Li et al. 2013). However, they did not improve evidence-based decision making because of lack of RCTs. Recently, several RCTs have investigated whether operative treatment may provide greater benefits than non-operative treatment (Rangan et al. 2015; Fjalestad and Hole 2014; Fjalestad et al. 2010, 2012; Boons et al. 2012; Olerud et al. 2011a, b; Zyto et al. 1997; Stableforth 1984). Whether operative treatment for CPHFs has a greater benefit over non-operative treatment remains controversial. This updated meta-analysis of RCTs aims to investigate whether operative treatment is superior to non-operative treatment in CPHFs.
Methods
Search strategy
The authors conducted a search of the Cochrane Central Register of Controlled Trials, PubMed, EMBASE, MEDLINE, Springer Link, Web of Knowledge, OVID and Google Scholar up to July 2015. No language restriction was made. The search strategy first used Mesh terms [“Shoulder fractures” (Mesh) OR “Proximal Humerus fractures” (Mesh) OR “Proximal Humeral Fractures” (Mesh)] and type of clinical trial (randomized controlled trial) and then a secondary free search was performed using multiple keywords (humer* and fractur* and random*) to ensure inclusion all possible studies. In addition, the reference lists of the included studies were checked for eligible studies.
Eligibility criteria
Studies were considered acceptable according to the following criteria: (1) complex displaced proximal humeral fractures; (2) operative treatment vs non-operative treatment; (3) functional outcomes, complications or healthy-related quality of life were described; and (4) randomized controlled trial study design. Studies were excluded if they (1) were abstracts, letters, or meeting proceedings; (2) had repeated data; or (3) enrolled patients with multi-trauma or patients undergoing surgery for a revision, infection, or nonunion or malunion.
Data extraction
The eligible studies were reviewed and all appropriate data were extracted by two authors (LX, YC) independently. The extracted data included general demographic characteristics, functional outcomes, complications and healthy-related quality of life.
Study quality assessment
The risk of bias of each study was independently assessed by two authors (FD, ZGZ), in accordance with the Cochrane risk of bias tool, which defines nine aspects: (1) random sequence generation (selection bias); (2) allocation concealment (selection bias); (3) blinding of participants (performance bias); (4) blinding of treatment providers (performance bias); (5) blinding of outcome assessors (detection bias); (6) intention to treat (attrition bias); (7) selective reporting (reporting bias); (8) comparable study groups; and (9) other bias. A qualification of risk of bias, including low risk, unclear risk, or high risk, was provided. The final qualification for each study was determined by consensus among three authors (LX, YC, and DMX).
Statistical analysis
Statistical analysis was performed with revman 5.3 software (Cochrane Collaboration, Oxford, UK) for outcome measures. The outcomes were function outcome (CS scores; DASH scores; ASES; OSS and SF-12), complications (total complications rates; the rate of additional surgery; infection; avascular necrosis; osteoarthritis; nerve injury; nonunion; impingement and re-displacement) and healthy-related quality of life (EQ-5D, 15D). Continuous variables and dichotomous data were analyzed with mean difference (MD) and relative risk (RR), both with 95 % confidence interval (CI), respectively. Statistical heterogeneity was assessed by the I2 statistics. Fixed-effects model was used when the heterogeneity was negligible (I2 < 50 %). Otherwise a random-effects model was adopted. To define sources of heterogeneity, subgroup analyses based on internal fixation and arthroplasty were defined during the analysis design phase. Publication bias was tested by funnel plots when possible. P < 0.05 was considered statistically significant.
Results
Study selection and characteristics
Figure 1 illustrates the study flow. The initial search identified 190 references. After duplicate references were removed and the titles, abstracts, and contents of the full text were examined, 9 articles included 7 RCTs were included in the meta-analysis (Rangan et al. 2015; Fjalestad and Hole 2014; Fjalestad et al. 2010, 2012; Boons et al. 2012; Olerud et al. 2011a, b; Zyto et al. 1997; Stableforth 1984). Table 1 shows the general characteristics of the 9 included articles. A total of 518 patients (average age 70.93) with CPHFs were included in this study. Mean age ranged from 65.6 to 79.9. The percentage of female patients ranged from 75 to 96 %. The studies followed patients for periods of 12–60 mo, and the rate of patient follow-up ranged from 72.5–98 %.
Fig. 1.
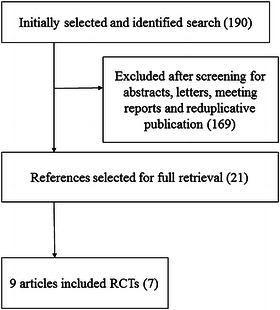
Flow diagram of literature search
Table 1.
Characteristics of included studies (O operative, N non-opreative)
| Study | Mean age (O/N) | No. (O/N) | % Female (O/N) | Follow-up (mo) | Rate of follow-up |
|---|---|---|---|---|---|
| Rangan et al. (2015) | 67.42/66.12 | 114/117 | 77.6/76.0 | 24 | 86 |
| Boons et al. (2012) | 79.9/76.4 | 25/25 | 92/96 | 24 | 94 |
| Fjalestad et al. (2010, 2012); Fjalestad and Hole (2014) | 72.2/73.1 | 25/25 | 80/94 | 12 | 98.0 |
| Olerud et al. (2011a, b) | 72.9/74.9 | 30/30 | 80/83 | 24 | 88.3 |
| Olerud et al. (2011a, b) | 75.8/77.5 | 27/28 | 85/86 | 24 | 89.1 |
| Stableforth (1984) | 65.6/70.1 | 16/16 | 75/81.3 | 6–48 | 93.8 |
| Zyto et al. (1997) | 73/75 | 20/20 | 90/85 | 36–60 | 72.5 |
Study quality
Figure 2 shows the quality of the RCTs as independently assessed by two authors (LX, YC). Six studies were single-center studies and one study was multi-center study. five studies were judged as having used sufficient allocation concealment. Only one study used closed envelopes without reporting adequate safeguards. Only one study was reported to have blinded the outcome assessors. Six studies reported a proper intention-to-treat analysis and clearly stated interventions. The comparability of baseline characteristics was generally acceptable.
Fig. 2.
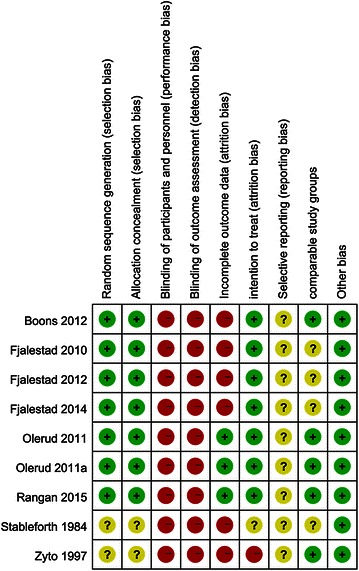
Risk of bias summary. Abbreviations: +, low risk; ?, unclear risk; −, high risk
Outcomes
Functional outcome
CS and DASH scores were the most commonly used to assess functional outcome of patients with displaced proximal humeral fractures. CS scores were mentioned in 6 studies and DASH scores were mentioned in two studies. No statistical differences were found between operative and non-operative treatment in CS scores at 12 mo [MD 1.06 95 % CI (−3.51, 5.62)] (Fig. 3) and 24 mo [MD −0.61 95 % CI (−5.87, 4.65)] (Fig. 4), There are no statistical differences between operative and non-operative treatment in DASH scores at 12 mo [MD −4.51 95 % CI (−13.49, 4.47)] (Fig. 5) and 24 mo (MD −7.43 95 % CI (−16.14, 1.27)] (Fig. 6), Other functional outcomes (ASES, OSS and SF-12) have no statistical differences between operative and non-operative treatment either (Table 2).
Fig. 3.
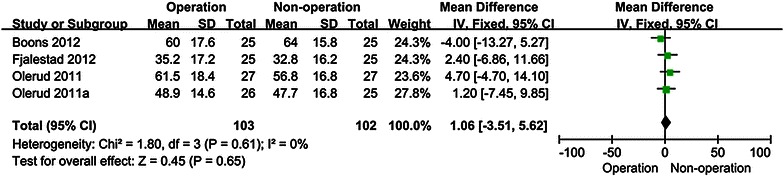
Forest plot for constant scores at 12 mo
Fig. 4.
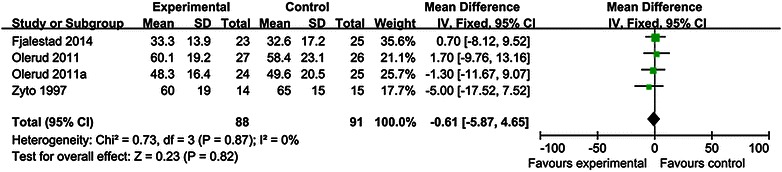
Forest plot for constant scores at 24 mo
Fig. 5.
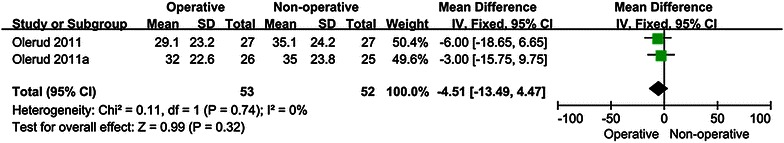
Forest plot for DASH scores at 12 mo
Fig. 6.
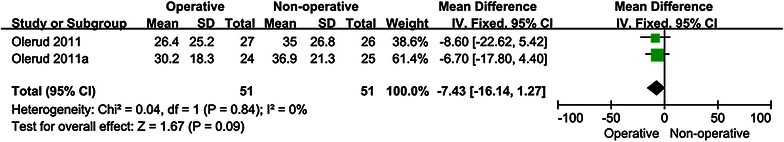
Forest plot for DASH scores at 24 mo
Table 2.
Functional status outcome (NA not available)
| Outcome | Studies | No. of patients (O/N) | MD (95 % CI) | P for MD | I2 | P for heterogeneity |
|---|---|---|---|---|---|---|
| ASES score at 6 mo | 1 | 23/25 | 0.10 (−3.66, 3.86) | 0.96 | NA | NA |
| ASES score at 12 mo | 1 | 23/25 | −0.70 (−4.52, 3.12) | 0.72 | NA | NA |
| OSS | 1 | 114/117 | 0.75 (−1.45, 2.95) | 0.50 | NA | NA |
| SF-12 physical component score | 1 | 111/115 | 2.00 (−1.00, 5.00) | 0.19 | NA | NA |
| SF-12 mental component score | 1 | 111/115 | −1.00 (−3.87, 1.87) | 0.49 | NA | NA |
Complications
Total complications rates [RR 1.55, 95 % CI (1.24, 1.94)] have statistical differences between operative and non-operative treatment (Fig. 7). All the complication reported were summarized in Table 3. Six articles that included 497 patients provided data on the rate of additional surgery. The rate of additional surgery was significantly higher in the operative group compared with the non-operative group [RR 1.91, 95 % CI (1.06, 3.45); Table 3]. No statistical differences were seen in the rates of infection; avascular necrosis; osteoarthritis; nerve injury; nonunion; impingement or re-displacement between operative and non-operative treatment (Table 3).
Fig. 7.
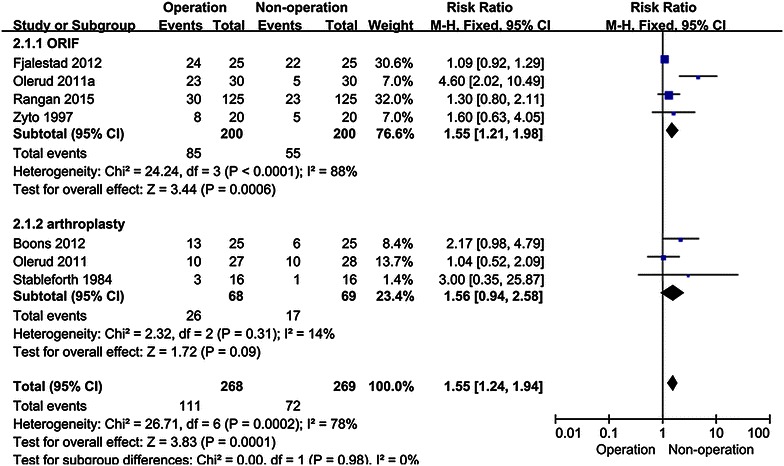
Forest plot for total complications rates
Table 3.
Total complication reported
| Outcome | No. of trials | No. of patients (O/N) | RR (95 % CI) | P for RR | I2 (%) | P for heterogeneity |
|---|---|---|---|---|---|---|
| Additional surgery rate | Boons et al. (2012) Fjalestad et al. (2012) Olerud et al. (2011a, b) Rangan et al. (2015) Stableforth (1984) |
248/249 | 1.91 (1.06, 3.45) | 0.03 | 13 | 0.33 |
| Mortality | Boons et al. (2012) Fjalestad et al. (2012) Rangan et al. (2015) Stableforth (1984) |
191/191 | 2.07 (0.88, 4.83) | 0.09 | 0 | 0.94 |
| Infection | Fjalestad et al. (2012) Olerud et al. (2011a, b) Rangan et al. (2015) Zyto et al. (1997) |
213/216 | 5.05 (0.90, 28.35) | 0.07 | 0 | 1.00 |
| Avascular necrosis | Fjalestad et al. (2012) Olerud et al. (2011a, b) Rangan et al. (2015) Zyto et al. (1997) Boons et al. (2012) |
252/253 | 0.82 (0.38, 1.77) | 0.61 | 16 | 0.31 |
| Osteoarthritis | Fjalestad et al. (2010) Zyto et al. (1997) |
41/41 | 1.34 (0.37, 4.82) | 0.66 | 13 | 0.28 |
| Nerve injury | Fjalestad et al. (2012) Rangan et al. (2015) |
148/150 | 1.57 (0.65, 3.79) | 0.32 | 0 | 0.38 |
| Nonunion | Fjalestad et al. (2012) Olerud et al. (2011a, b) Rangan et al. (2015) Zyto et al. (1997) |
189/191 | 0.38 (0.11, 1.26) | 0.11 | 10 | 0.34 |
| Impingement | Olerud et al. (2011a) Rangan et al. (2015) |
149/150 | 1.02 (0.15, 7.05) | 0.98 | 0 | 0.33 |
| Redisplacement | Fjalestad et al. (2012) Olerud et al. (2011a) Zyto et al. (1997) |
38/40 | 0.53 (0.10, 2.78) | 0.45 | 48 | 0.16 |
Healthy-related quality of life
Only the differences in EQ-5D at 24 mo [MD 0.15, 95 % CI (0.05, 0.24)] were found between operative and non-operative treatment and no statistical differences were found in ED-5D at 12 mo [MD 0.08, 95 % CI (−0.01, 0.17)], 15D at 12 mo [MD 0.02, 95 % CI (−0.68, 0.73)] and 15D at 24 mo [MD 0.02, 95 % CI (−0.07, 0.83)] (Table 4).
Table 4.
Health-related quality of life
| Outcome | Study | No. of patients (O/N) | MD (95 % CI) | P for MD | I2 | P for heterogeneity |
|---|---|---|---|---|---|---|
| EQ-5D at 12 mo | Olerud et al. (2011a, b) | 53/52 | 0.08 (−0.01, 0.17) | 0.10 | 0 % | 0.83 |
| EQ-5D at 24 mo | Olerud et al. (2011a, b) | 51/51 | 0.15 (0.05, 0.24) | 0.004 | 0 % | 0.65 |
| 15D at 12 mo | Fjalestad et al. (2012) | 23/25 | 0.02 (−0.03, 0.07) | 0.44 | NA | NA |
| 15D at 24 mo | Fjalestad et al. (2012) | 23/25 | 0.02 (−0.78, 0.83) | 0.95 | NA | NA |
Sensitivity analysis
Due to the high heterogeneity in the above analysis, we performed subgroup analysis in the meta-analysis based on different surgical treatments. A sensitivity analysis was also conducted by removing one study at a time. We found that no article substantially influenced the results in this analysis.
Publication bias
The publication bias was evaluated by a funnel plot. The funnel plot shapes showed no obvious evidence of a symmetry. The results suggested that publication bias was not evident in this meta-analysis.
Discussion
According to the Neer classification (Neer 1970a, b), the decision regarding the treatment of proximal humeral fractures is dependent on whether the four anatomical segments of the proximal humeral (the humeral head, shaft, and greater and lesser tubercles) are fractured or displaced. In our paper, CPHFs mean proximal humeral fractures excluding non- or minimally displaced proximal humeral fractures. CPHFs have poor outcomes and the optimal treatment is still controversial. There are several kinds of surgical methods for patients with CPHFs, including steosynthesis, hemiarthroplasty and reverse shoulder arthroplasty (Murray et al. 2011). Whether surgical methods could help to resume the painless range of motion and good shoulder function, thereby allow for rapid return to work and previous level of activity is still unclear. We performed this updated meta-analysis concerning the comparison of operative and non-operative treatment for the CPHFs. This meta-analysis was based on 7 RCTs in 9 articles (Rangan et al. 2015; Fjalestad and Hole 2014; Fjalestad et al. 2010, 2012; Boons et al. 2012; Olerud et al. 2011a, b; Zyto et al. 1997; Stableforth 1984). In this study, we compared the efficiency and safety of surgical and conservative interventions for CPHFs in elderly patients. The results of this meta-analysis indicated that surgical intervention only improved the ED-5D at 24 mo but suffered more complications. Meanwhile, no statistical differences were observed in CS scores, DASH scores, ED-5D at 12 mo and 15D.
Function outcome was a major clinical evaluation in all studies. Various measures have been developed to assess shoulder and arm disability. The measures can contain either self-reported or performance-based assessments or a combination of both. Among all these measure, the CS score is a widely accepted functional score of shoulder joint in the world (Constant and Murley 1987; Conboy et al. 1996; Rocourt et al. 2008). No statistical difference was detected with respect to CS score in our meta-analysis. The DASH score is a measurement of upper-extremity disability and symptoms (Hudak et al. 1996). There was also no statistical difference with regard to DASH score between two groups in our findings. Other functional outcomes (ASES, OSS and SF-12) have no statistical differences between operative and non-operative treatment either. Based on these outcomes, our analysis shows that operative treatment has no significant benefit on shoulder and arm functional recovery compared to non-operative treatment.
Total complications events in operative group were more common than that in conservative group especially the postoperative complications such as penetration of implant into joint rate, metalwork problem. For patients with operative treatment, the incidence of additional surgery is higher. This higher incidence of additional surgery in operative group may be associated with surgical expertise (Namdari et al. 2012). These complications could be minimized by improved operative techniques (Owsley and Gorczyca 2008; Egol et al. 2008). All deaths mentioned in this article were unrelated with interventions, thus, no statistically differences were found between operative and non-operative treatment in mortality. Some of these complication (infection; avascular necrosis; osteoarthritis; nerve injury; nonunion; impingement or re-displacement) may occur in both operative and non-operative treatment, and no statistical differences were found between operative and non-operative treatment in these complication.
Healthy-related quality of life in patients treated with operative treatment outperformed that with conservative treatments for EQ-5D at 24 mo, while no statistical differences in ED-5D at 12 mo, 15D at 12 mo and 15D at 24 mo (Table 4). While the number of studies included is limited. Only Olerud et al. (2011a, b) reported that hemiarthroplasty can improve EQ-5D at 24 mo, so more well designed, high quality RCTs are needed. All of these results indicate that neither operative nor non-operative treatment can achieve ideal clinical results, and operative treatment might fail to show a clinical benefit compared with non-operative treatment.
Although this meta-analysis was performed with the best available evidence presently, some unavoidable weaknesses earned to be noted. First, although we used multiple search strategies and available databases to include all possible studies, publication bias may be unavoidable. Second, the number of studies included is small. More well designed, high quality RCTs are needed. Furthermore, the types of operative or non-operative treatment in studies were varied and the follow-up periods in studies ranged largely from 1 year to several years. In addition, the variety of outcome measures limits the authors’ ability to combine outcomes and make definitive conclusions.
Although some limitations were unavoidable, this study has some merits. First, the search style based on the computer and manual search ensures a complete inclusion of relevant studies. Secondly, no significant heterogeneity was observed in most variables. Last, all the studies in this meta-analysis were RCTs.
Conclusion
For CPHFs, current limited studies suggest that operative treatments did not significantly improve the functional outcome and healthy-related quality of life. Instead, Operative treatment for CPHFs led to higher incidence of postoperative complications. Based on the results of this meta-analysis, both treatment can achieve a similar effect on CPHFs, but operative treatment may increase the rate of total complication. Large, definitive RCTs are needed. Fortunately, such RCTs have already been designed (Launonen et al. 2012; Den Hartog et al. 2010; Handoll et al. 2009; Brorson et al. 2009).
Authors’ contributions
DX designed the study; LX and FD searched relevant studies and abstracted the data; ZZ and YC analyzed and interpreted the data; LX and FD wrote the manuscript and DX approved the final version of the manuscript. All authors read and approved the final manuscript.
Acknowledgements
We are very grateful to Dr. Xiao Zhihong for language editing.
Competing interests
The authors declare that they have no competing interests. No organization sponsored the research.
Abbreviations
- CPHFs
Complex proximal humeral fractures
- RCTs
Randomized controlled trials
- CS
Constant
- DASH
Disabilities of the arm, shoulder and hand
- mo
Months
- MD
Mean difference
- RR
Relative risk
- CI
Confidence interval
Contributor Information
Lin Xie, Email: lin_xie2014@163.com.
Fan Ding, Email: 295511@qq.com.
Zhigang Zhao, Email: 317363525@qq.com.
Yan Chen, Email: shrrng0@gmail.com.
Danmou Xing, Phone: +8618051183772, Email: dorisjiang667@163.com.
References
- Baron JA, Barrett JA, Karagas MR. The epidemiology of peripheral fractures. Bone. 1996;18(3):S209–S213. doi: 10.1016/8756-3282(95)00504-8. [DOI] [PubMed] [Google Scholar]
- Baron JA, Karagas M, Barrett J, Kniffin W, Malenka D, Mayor M, Keller RB (1996b) Basic epidemiology of fractures of the upper and lower limb among Americans over 65 years of age. Epidemiology 7(6):612–618. doi:10.1097/00001648-199611000-00008 [DOI] [PubMed]
- Bengner U, Johnell O, Redlundjohnell I. Changes in the incidence of fracture of the upper end of the humerus during a 30-year period. A study of 2125 fractures. Clin Orthop Relat R. 1988;231:179–182. [PubMed] [Google Scholar]
- Boons HW, Goosen JH, van Grinsven S, van Susante JL, van Loon CJ. Hemiarthroplasty for humeral four-part fractures for patients 65 years and older: a randomized controlled trial. Clin Orthop Relat R. 2012;470(12):3483–3491. doi: 10.1007/s11999-012-2531-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brorson S, Olsen BS, Frich LH, Jensen SL, Johannsen HV, Sorensen AK, Hrobjartsson A. Effect of osteosynthesis, primary hemiarthroplasty, and non-surgical management for displaced four-part fractures of the proximal humerus in elderly: a multi-centre, randomised clinical trial. Trials. 2009;10:51. doi: 10.1186/1745-6215-10-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cadet ER, Ahmad CS. Hemiarthroplasty for three- and four-part proximal humerus fractures. J Am Acad Orthop Sur. 2012;20(1):17–27. doi: 10.5435/JAAOS-20-01-017. [DOI] [PubMed] [Google Scholar]
- Conboy VB, Morris RW, Kiss J, Carr AJ. An evaluation of the Constant-Murley shoulder assessment. J Bone Jt Surg Br. 1996;78B(2):229–232. [PubMed] [Google Scholar]
- Constant CR, Murley AHG. A clinical method of functional assessment of the shoulder. Clin Orthop Relat R. 1987;214:160–164. [PubMed] [Google Scholar]
- Den Hartog D, Van Lieshout EM, Tuinebreijer WE, Polinder S, Van Beeck EF, Breederveld RS, Bronkhorst MW, Eerenberg JP, Rhemrev S, Roerdink WH, Schraa G, Van der Vis HM, Van Thiel TP, Patka P, Nijs S, Schep NW. Primary hemiarthroplasty versus conservative treatment for comminuted fractures of the proximal humerus in the elderly (ProCon): a multicenter randomized controlled trial. BMC Musculoskelet Disord. 2010;11:97. doi: 10.1186/1471-2474-11-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egol KA, Ong CC, Walsh M, Dazrawi LM, Tejwani NC, Zuckerman JD. Early complications in proximal humerus fractures (OTA types 11) treated with locked plates. J Orthop Trauma. 2008;22(3):159–164. doi: 10.1097/BOT.0b013e318169ef2a. [DOI] [PubMed] [Google Scholar]
- Fjalestad T, Hole MO. Displaced proximal humeral fractures: operative versus non-operative treatment—a 2-year extension of a randomized controlled trial. Eur J Orthop Surg Traumatol. 2014;24(7):1067–1073. doi: 10.1007/s00590-013-1403-y. [DOI] [PubMed] [Google Scholar]
- Fjalestad T, Hole MO, Jorgensen JJ, Stromsoe K, Kristiansen IS. Health and cost consequences of surgical versus conservative treatment for a comminuted proximal humeral fracture in elderly patients. Injury. 2010;41(6):599–605. doi: 10.1016/j.injury.2009.10.056. [DOI] [PubMed] [Google Scholar]
- Fjalestad T, Hole MO, Hovden IA, Blucher J, Stromsoe K. Surgical treatment with an angular stable plate for complex displaced proximal humeral fractures in elderly patients: a randomized controlled trial. J Orthop Trauma. 2012;26(2):98–106. doi: 10.1097/BOT.0b013e31821c2e15. [DOI] [PubMed] [Google Scholar]
- Fu T, Xia C, Li Z, Wu H. Surgical versus conservative treatment for displaced proximal humeral fractures in elderly patients: a meta-analysis. Int J Clin Exp Med. 2014;7(12):4607–4615. [PMC free article] [PubMed] [Google Scholar]
- Handoll HHG, Ollivere BJ (2010) Interventions for treating proximal humeral fractures in adults. Cochrane Database Syst Rev (12). doi:10.1002/14651858.CD000434.pub2 [DOI] [PubMed]
- Handoll H, Brealey S, Rangan A, Torgerson D, Dennis L, Armstrong A, Chuang LH, Cross B, Dumville J, Gardner S, Goodchild L, Hamilton S, Hewitt C, Madhok R, Maffulli N, Micklewright L, Wadsworth V, Wallace A, Williams J, Worthy G. Protocol for the ProFHER (PROximal Fracture of the Humerus: evaluation by Randomisation) trial: a pragmatic multi-centre randomised controlled trial of surgical versus non-surgical treatment for proximal fracture of the humerus in adults. BMC Musculoskelet Disord. 2009;10:140. doi: 10.1186/1471-2474-10-140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horak J, Nilsson BE. Epidemiology of fracture of the upper end of the humerus. Clin Orthop Relat R. 1975;112:250–253. doi: 10.1097/00003086-197510000-00032. [DOI] [PubMed] [Google Scholar]
- Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder, and head) Am J Ind Med. 1996;29(6):602–608. doi: 10.1002/(SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- Jia Z, Li W, Qin Y, Li H, Wang D, Zhang C, He Q, Ruan D. Operative versus nonoperative treatment for complex proximal humeral fractures: a meta-analysis of randomized controlled trials. Orthopedics. 2014;37(6):e543–e551. doi: 10.3928/01477447-20140528-54. [DOI] [PubMed] [Google Scholar]
- Jost B, Spross C, Grehn H, Gerber C. Locking plate fixation of fractures of the proximal humerus: analysis of complications, revision strategies and outcome. J Shoulder Elbow Surg. 2013;22(4):542–549. doi: 10.1016/j.jse.2012.06.008. [DOI] [PubMed] [Google Scholar]
- Kannus P, Palvanen M, Niemi S, Parkkari J, Jarvinen M, Vuori I. Increasing number and incidence of osteoporotic fractures of the proximal humerus in elderly people. Br Med J. 1996;313(7064):1051–1052. doi: 10.1136/bmj.313.7064.1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karataglis D, Stavridis SI, Petsatodis G, Papadopoulos P, Christodoulou A. New trends in fixation of proximal humeral fractures: a review. Injury. 2011;42(4):330–338. doi: 10.1016/j.injury.2010.10.016. [DOI] [PubMed] [Google Scholar]
- Kim SH, Szabo RM, Marder RA. Epidemiology of humerus fractures in the united states: nationwide emergency department sample, 2008. Arthritis Care Res (Hoboken) 2012;64(3):407–414. doi: 10.1002/acr.21563. [DOI] [PubMed] [Google Scholar]
- Launonen AP, Lepola V, Flinkkila T, Strandberg N, Ojanpera J, Rissanen P, Malmivaara A, Mattila VM, Elo P, Viljakka T, Laitinen M. Conservative treatment, plate fixation, or prosthesis for proximal humeral fracture. A prospective randomized study. BMC Musculoskelet Disord. 2012;13:167. doi: 10.1186/1471-2474-13-167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y, Zhao L, Zhu L, Li J, Chen A. Internal fixation versus nonoperative treatment for displaced 3-part or 4-part proximal humeral fractures in elderly patients: a meta-analysis of randomized controlled trials. PLoS One. 2013;8(9):e75464. doi: 10.1371/journal.pone.0075464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lill H, Katthagen C, Jensen G, Voigt C. Arthroscopic fracture management in proximal humeral fractures. Der Unfallchirurg. 2013;116(4):296–304. doi: 10.1007/s00113-012-2345-2. [DOI] [PubMed] [Google Scholar]
- Mao Z, Zhang L, Zhang L, Zeng X, Chen S, Liu D, Zhou Z, Tang P. Operative versus nonoperative treatment in complex proximal humeral fractures. Orthopedics. 2014;37(5):e410–e419. doi: 10.3928/01477447-20140430-50. [DOI] [PubMed] [Google Scholar]
- Murray IR, Amin AK, White TO, Robinson CM. Proximal humeral fractures: current concepts in classification, treatment and outcomes. J Bone Jt Surg Br. 2011;93(1):1–11. doi: 10.1302/0301-620X.93B1.25702. [DOI] [PubMed] [Google Scholar]
- Namdari S, Lipman AJ, Ricchetti ET, Tjoumakaris FP, Huffman GR, Mehta S. Fixation strategies to prevent screw cut-out and malreduction in proximal humeral fracture fixation. Clin Orthop Surg. 2012;4(4):321–324. doi: 10.4055/cios.2012.4.4.321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neer CS. Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Jt Surg Am. 1970;52(6):1077–1089. [PubMed] [Google Scholar]
- Neer CS. Displaced proximal humeral fractures. II. Treatment of three-part and four-part displacement. J Bone Jt Surg Am. 1970;52(6):1090–10103. [PubMed] [Google Scholar]
- Olerud P, Ahrengart L, Ponzer S, Saving J, Tidermark J. Hemiarthroplasty versus nonoperative treatment of displaced 4-part proximal humeral fractures in elderly patients: a randomized controlled trial. J Shoulder Elbow Surg. 2011;20(7):1025–1033. doi: 10.1016/j.jse.2011.04.016. [DOI] [PubMed] [Google Scholar]
- Olerud P, Ahrengart L, Ponzer S, Saving J, Tidermark J. Internal fixation versus nonoperative treatment of displaced 3-part proximal humeral fractures in elderly patients: a randomized controlled trial. J Shoulder Elbow Surg. 2011;20(5):747–755. doi: 10.1016/j.jse.2010.12.018. [DOI] [PubMed] [Google Scholar]
- Owsley KC, Gorczyca JT. Fracture displacement and screw cutout after open reduction and locked plate fixation of proximal humeral fractures [corrected] J Bone Jt Surg Am. 2008;90(2):233–240. doi: 10.2106/JBJS.F.01351. [DOI] [PubMed] [Google Scholar]
- Rangan A, Handoll H, Brealey S, Jefferson L, Keding A, Martin BC, Goodchild L, Chuang LH, Hewitt C, Torgerson D, Collaborators PT. Surgical vs nonsurgical treatment of adults with displaced fractures of the proximal humerus: the PROFHER randomized clinical trial. JAMA. 2015;313(10):1037–1047. doi: 10.1001/jama.2015.1629. [DOI] [PubMed] [Google Scholar]
- Rocourt MHH, Radlinger L, Kalberer F, Sanavi S, Schmid NS, Leunig M, Hertel R. Evaluation of intratester and intertester reliability of the Constant-Murley shoulder assessment. J Shoulder Elbow Surg. 2008;17(2):364–369. doi: 10.1016/j.jse.2007.06.024. [DOI] [PubMed] [Google Scholar]
- Roux A, Decroocq L, El Batti S, Bonnevialle N, Moineau G, Trojani C, Boileau P, de Peretti F. Epidemiology of proximal humerus fractures managed in a trauma center. Orthop Traumatol Surg Res. 2012;98(6):715–719. doi: 10.1016/j.otsr.2012.05.013. [DOI] [PubMed] [Google Scholar]
- Russo R, Cautiero F, Ciccarelli M, Lombardi LV. Reconstruction of unstable, complex proximal humeral fractures with the da Vinci cage: surgical technique and outcome at 2 to 6 years. J Shoulder Elbow Surg. 2013;22(3):422–431. doi: 10.1016/j.jse.2012.04.010. [DOI] [PubMed] [Google Scholar]
- Stableforth PG. Four-part fractures of the neck of the humerus. J Bone Jt Surg Br. 1984;66(1):104–108. doi: 10.1302/0301-620X.66B1.6693466. [DOI] [PubMed] [Google Scholar]
- Sun Y, Li L, Dai J, Wang T. Treatment of complex proximal humeral fracture: plate and tension band fixation versus conservative therapy. Int J Clin Exp Med. 2015;8(5):7143–7151. [PMC free article] [PubMed] [Google Scholar]
- Vundelinckx BJ, Dierickx CA, Bruckers L, Dierickx CH. Functional and radiographic medium-term outcome evaluation of the Humerus Block, a minimally invasive operative technique for proximal humeral fractures. J Shoulder Elbow Surg. 2012;21(9):1197–1206. doi: 10.1016/j.jse.2011.07.029. [DOI] [PubMed] [Google Scholar]
- Yuksel HY, Yilmaz S, Aksahin E, Celebi L, Muratli HH, Bicimoglu A. The results of nonoperative treatment for three- and four-part fractures of the proximal humerus in low-demand patients. J Orthop Trauma. 2011;25(10):588–595. doi: 10.1097/BOT.0b013e318210ea56. [DOI] [PubMed] [Google Scholar]
- Zyto K, Ahrengart L, Sperber A, Tornkvist H. Treatment of displaced proximal humeral fractures in elderly patients. J Bone Jt Surg Br. 1997;79(3):412–417. doi: 10.1302/0301-620X.79B3.7419. [DOI] [PubMed] [Google Scholar]


