Abstract
We describe the global status of measles control and elimination, including surveillance and vaccination coverage data provided by the World Health Organization (WHO). Since 2000, two doses of measles vaccine (MCV2) became recommended globally and the achievement of high vaccination coverage has led to dramatic decrease in the measles incidence. Our finding indicates that, in the Western Pacific Region (WPR), substantial progress has been made to control measles transmission in some countries; however, the measles virus continues to circulate, causing outbreaks. The Republic of Korea (ROK) experienced a series of resurgence of measles due to the importation and healthcare-associated transmission in infants, however overall incidence and surveillance indicators met the WHO criteria for measles elimination. The ROK was verified to be measles-free along with Australia, Mongolia, and Macau, China in 2014. One of the effective elimination activities was the establishment of solid keep-up vaccination system in school settings. The lessons learnt from the measles elimination activities in Korea may contribute to enhancing the surveillance schemes and strengthening of vaccination programs in member countries and areas of WPR.
Keywords: Measles, Korea, Western Pacific Region, Elimination, Surveillance
BACKGROUND
Measles is a highly contagious disease that infected almost all vulnerable populations during the pre-vaccination era, with the case fatality rate ranging 3%-15% in the developing countries (1). The transmission occurs through droplets or aerosols and results in secondary attack rate of more than 70%-80% in susceptible populations (2). Measles is potentially eradicable because humans are the only reservoir to the virus, a sensitive and specific diagnostic tool is available, and an effective vaccine is available (3).
The vaccines play a key role in the elimination of measles. It is estimated that one dose of measles vaccine confers at least 95% effectiveness in preventing clinical measles and 92% effectiveness in preventing secondary cases among household contacts (4). The highly transmissible measles records basic reproduction number of greater than 10, therefore the vaccination coverage of more than 95% is necessary to achieve effective herd protection from the vaccines (5). Current strategies for the global eradication of measles include achieving high vaccination coverage coupled with epidemiological and laboratory surveillance. The two-dose measles vaccination program is now being recommended globally, however, the implementation is challenging in countries with limited health resources. The weak health systems hinder the key components in routine vaccination services: stable vaccine procurement, maintenance of cold-chain, and effective vaccination delivery. To overcome these challenges, various vaccination strategies have played a role for attaining adequate vaccination coverage and stopping endemic transmission of the measles virus in the community (6,7).
In the World Health Organization (WHO) Western Pacific Region Office (WPR), substantial progress has been made to control and interrupt measles transmission (8). However, the measles virus continues to circulate causing outbreaks in the WPR countries, potentially due to limited success in achieving universally high vaccination rates at the sub-national level. In this report, we aimed to provide perspectives in measles elimination, with sharing the experiences from the Republic of Korea, to intensify efforts to close gaps in population immunity of measles with the WPR member states and regions.
GLOBAL MEASLES ELIMINATION ACTIVITIES
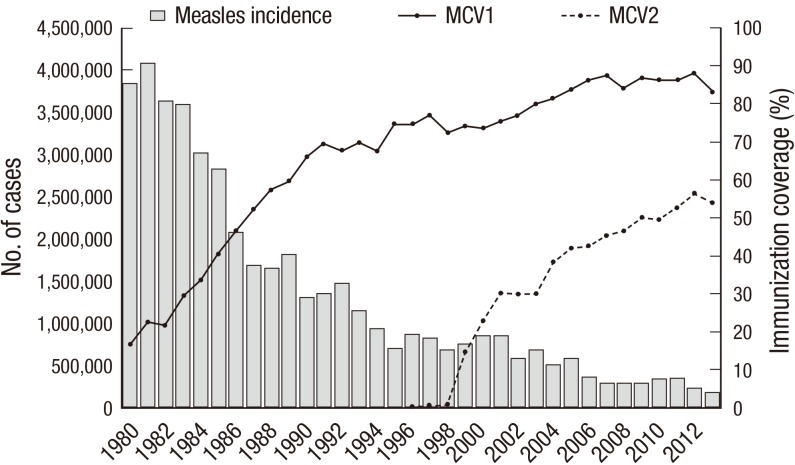
The measles-containing vaccines (MCV) have been used routinely in many countries, employing different schedules and doses for nearly 50 yr. Strengthening of the measles vaccination activities dates back to the 1974, when the WHO has initiated the Expanded Program on Vaccination (EPI), aiming to develop and support the increase of vaccination coverage (9). However, the global vaccination coverage in the 1980s was low, less than 60%, and consequently measles continued to prevail causing more than 2 million cases per year. In the late 1980s, following the World Health Assembly's resolution to reduce measles morbidity by 90% and mortality by 95% and the World Summit for Children's implementation to target vaccination coverage among 90% of children, the measles cases decreased to 1-1.5 million annual cases in the 1990s (10). In 2000, the WHO and the United Nations Children's Fund (UNICEF) have recommended the two doses of measles vaccine (MCV2) in every child. Globally, the achievement of high vaccination coverage of the first and second doses of MCV has led to dramatic decrease in the measles incidence (Fig. 1).
Fig. 1. Global number of reported measles cases and estimate of the first and second doses of measles immunization coverage, 1980-2013. MCV, measles containing vaccine.
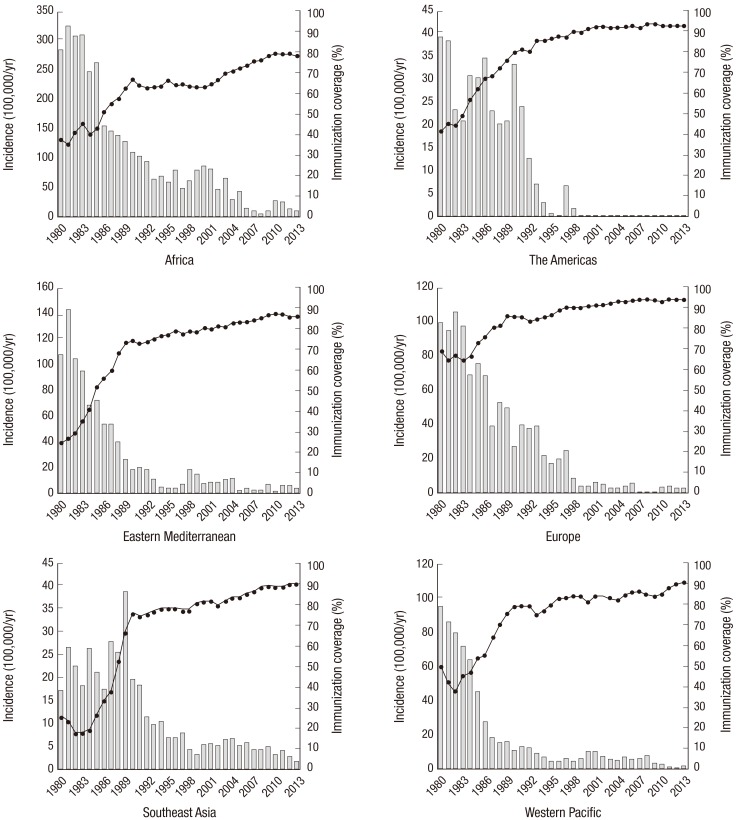
However, concerns have been raised over the apparent discrepancies between coverage rates in the WHO Regions. The Regions of Americas and Europe, with their steady increase in the vaccination coverage since 1980, have reached MCV1 coverage of more than 90% in the 1990s, and sustained low incidence of measles in the 2000s (Fig. 2). The increase in MCV1 coverage in Regions of Eastern Mediterranean and Western Pacific were noted in 1980s, but less than 90% coverage in the 1990s led to ongoing transmission of the virus in their Regions. In the Regions of Africa and Southeast Asia, there were significant reduction in overall incidence rates; however, the Region's most remote and hard-to-reach population are still vulnerable to transmission and outbreak of measles due to poor access to vaccines.
Fig. 2. Measles incidence rate per 100,000 population/year and estimate of the first dose of measles vaccination coverage by WHO Region, 1980-2013. WHO, World Health Organization; incidence, reported case per 100,000 population per year; bar represent incidence rate, line represent immunization coverage.
ELIMINATION OF MEASLES IN THE REGION OF AMERICAS
In 2002, the Region of Americas became the first WHO region to interrupt measles transmission, and several lessons have been learned from their experiences. Innovative measles vaccination strategies were implemented in the Region since 1990s. The strategies aimed to rapidly interrupt the measles transmission by performing mass vaccination campaigns, namely "catch-up", "mop-up", and "follow-up", and to maintain high population immunity by providing adequate vaccination coverage to each successive birth cohorts through routine vaccination services (11). The "catch-up" vaccination campaign is a one-time mass vaccination campaign conducted for a defined age group (usually children aged 9 months to 14 yr). After the "catch-up" campaign was conducted, there were portions of the population with inadequate vaccination coverage; therefore a "mop-up" campaign was conducted to increase vaccination in areas of low coverage. Because the vaccine is not 100% effective and the measles virus is highly transmissible, the accumulation of susceptible population over time may result in on-going transmission of the virus; therefore, a "follow-up" vaccination campaign was conducted every 2-5 yr periodically to increase the population immunity.
Between 1989 and 1995, a total of 39 out of 41 countries in the Region of Americas have conducted catch-up campaigns and periodic follow-up campaigns every four years (12). All children aged 9 months to 14 yr, irrespective of previous vaccination history, have been vaccinated within a short period of time. Since there may still remain pockets of population with limited access to catch-up campaign, the special vaccination or mop-up campaign were carried out in areas to increase their level of immunity. The catch-up and mop-up campaigns resulted in a rapid increase in population immunity, and contributed in overall reduction of measles incidence in the Region. After the initial catch-up campaign, strengthening of routine vaccination services to "keep-up" at least 95% of each birth cohorts at 12-15 months of age was conducted. And to ensure the adequate herd immunity among children, the "follow-up" vaccination campaigns had been conducted. These vaccination strategies were accompanied by the improvements in virologic and epidemiologic surveillance schemes.
The implementation of the vaccination strategies in the Region of Americas has resulted in reduction of measles incidence as depicted in Fig. 2. The number of measles cases declined to 537 in 2001; more than 99% lower than previously reported in 1990. Among all WHO Regions, the Americas accounted for 6.6% (185,793 out of 2,794,053) during 1980-1991, while the proportion decreased to 2.6% in 1992-2003, and to 0.1% in 2004-2013. Between the three periods, the incidence rates in the Region of Americas have decreased by 90% and 99%, respectively (Fig. 2, Table 1).
Table 1. Time trend in the estimated incidence of measles by WHO region.
| WHO region | Estimated incidence per year, n (%) | ||
|---|---|---|---|
| 1980-1991 | 1992-2003 | 2004-2013 | |
| Africa | 914,461 (32.7) | 425,588 (49.2) | 165,650 (44.2) |
| The Americas | 185,793 (6.6) | 22,202 (2.6) | 273 (0.1) |
| Eastern Mediterranean | 212,790 (7.6) | 47,875 (5.5) | 28,619 (7.6) |
| Europe | 584,591 (20.9) | 141,656 (16.4) | 26,653 (7.1) |
| Southeast Asia | 267,540 (9.6) | 101,956 (11.8) | 75,104 (20.0) |
| Western Pacific | 628,878 (22.5) | 126,133 (14.6) | 78,602 (21.0) |
| Total | 2,794,053 | 865,409 | 374,900 |
WHO, World Health Organization; incidence, reported case.
WESTERN PACIFIC REGION AND THE ELIMINATION GAP
Since the 1960s, many countries and areas of the WPR have included MCVs as a part of their routine vaccination program (13,14). By 1990s, all member states have included measles vaccine, usually in the form of monovalent vaccine, and in Guam, Hong Kong, Palau, and Singapore, it is given in the form of measles-mumps-rubella (MMR) vaccine. MCV2 was first implemented in American Samoa, New Zealand, Palau, and Samoa. As the poliomyelitis eradication activities have led to strengthening of routine immunization system, it also contributed to increase of measles vaccination coverage in Cambodia, China, Lao PDR, the Philippines, and Vietnam (15). During the national immunization days for poliomyelitis eradication in the Philippines, supplementary measles and tetanus toxoid vaccines were also given to all children between 9 and 59 months of age (16). By 2003, the introduction of measles immunization programs in WPR countries has resulted in dramatic decreases in morbidity and mortality attributable to measles. In Pacific islands, Australia, Mongolia, and Korea, experiences indicate that elimination can be achieved in countries with diverse geography, populations, and measles epidemiology (13). Between 1980 and 1991, the estimated annual incidence in the WPR was 628,878 cases, which accounted for 22.5% of the global incidence (Table 1). The number of cases per year from 1992 to 2003 decreased to 126,133 cases, and further down to 78,602 cases in 2004-2013.
The strategy used in the WPR in 1990-1995 was to "control" measles; in 1996-2002, was to "accelerate control", and from 2003 to now, "elimination" (17). In 2005, the 37 countries of the WPR established a goal to eliminate measles in the region by 2012. The strategies included (1) high vaccination coverage (≥95%) with a first and second dose of measles-containing vaccine (MCV2) through routine vaccination or catch-up and follow-up supplementary immunization activities (SIAs); and enhanced case-based epidemiological surveillance in conjunction with laboratory monitoring to identify measles virus genotype. By 2009, 21 of 37 countries and areas had ≥90% coverage with a first dose of measles vaccine. Between 2009 and 2012, the incidence has reached a record low, with decline by 82.6% from 34.0 to 5.9 cases per million (18).
Although the countries and areas in the WPR experience an overall decrease in burden of measles, there were large numbers of cases continue in several countries. The WHO-led intensified vaccination efforts focused on Cambodia, Laos, Papua New Guinea, and Vietnam at first, yet, China and Japan, the most populous two countries accounting 80% of the region's population, were not included (19). In 2008, a total of 131,441 measles cases (98.4 per million population) were reported from China and 11,015 cases (86.1 per million population) from Japan (20). In China, although the incidence of measles decreased from 9.95 in 2008 to 0.46 in 2012, however increased in 2013 by 1.96, potentially due to immunity gaps between birth cohorts (21). In Japan, the regular vaccination schedule has been changed to two-dose schedule since 2006, however there were still estimated 5-10 thousands measles cases and 50 measles death annually (22). The outbreaks were also reported in distant countries: in Marshall Islands in 2003, Fiji in 2006, and Australia in 2006 (23). In Vietnam, although supplementary immunization activities were conducted in 2002-2003, there were outbreak of 7,948 measles cases (93 per million population) reported from 60 of 63 provinces in 2008-2010 (24).
By late 2000s, more intensified efforts by WPR countries became necessary to achieve the 2012 goal. From 1996 to 2009, 235 million children and adolescents received vaccines during a total of 94 immunization campaigns (17). By 2009, 21 of 37 WPR countries and areas had ≥90% coverage with MCV1; 32 countries and areas provided MCV2 with 94% coverage. Since 2010, there are ongoing activities of measles supplementary vaccination with or without conjunction with oral polio vaccine campaign: 2010 in China, Federated States of Micronesia, Papua New Guinea, Tuvalu, Vietnam; 2011 in Cambodia, Laos, the Philippines; 2012 in Papua New Guinea, Solomon, Mongolia. In 2010, the largest supplemental immunization activity in history was conducted in China, with over 103 million children vaccinated (25). Although the elimination goal of measles from WPR was not achieved, elimination was achieved in 25 of 37 countries as of 2012, including Korea, Pacific Island countries, Australia, Hong Kong and Macau (26). In addition, there was resurgence of measles transmission in 2013 and 2014, particularly in China, the Philippines, Vietnam and Papua New Guinea.
In China, routine immunization of MCV1 and MCV2 were established in 1978 and 1985, respectively (27). The supplementary immunization activities were conducted in 2004, 2008, 2010, and 2011-2013, while since 2005, school entry requirement for MCV2 was implemented. The number of measles cases decreased from 5,000-25,000 between 2007-2010 to less than 3,000 in 2011-2012, however in 2014, 33,831 cases were reported by May 31 2014, which was increased by 97% compared to that during the same period in 2013. In the Philippines, supplementary immunization activities were conducted every 3-4 yr, however the coverage rate was not high and uniform enough (19). Serious major disasters from 2012 to 2013 damaged immunization service infrastructure, which may have caused an outbreak of 2,956 cases in 2013 and 10,712 cases by April 2014. In Vietnam, supplementary immunization activities were conducted in 2002-2003, 2004, 2006, 2007, 2008, 2010, and 2011-2013 targeting various age groups and regions (27). From May 2013 to 2014, measles outbreak of more than 6,000 patients occurred, potentially affected by declined MCV2 coverage due to the shortage of vaccines. The largest measles-rubella immunization campaign had launched targeting 23 million children aged 1-14 yr in 2014. In Papua New Guinea, the supplementary immunization was given every 2 yr, and covered approximately 80%-85% of coverage rate. However, the largest outbreak since 2005-2006 occurred in 2013-2014, resulting in 1,251 cases by June 2014 (27). The investigation revealed that 35% of cases between 6 months to 5 yr did not receive a MCV1 in routine immunization.
EXPERIENCE IN THE REPUBLIC OF KOREA
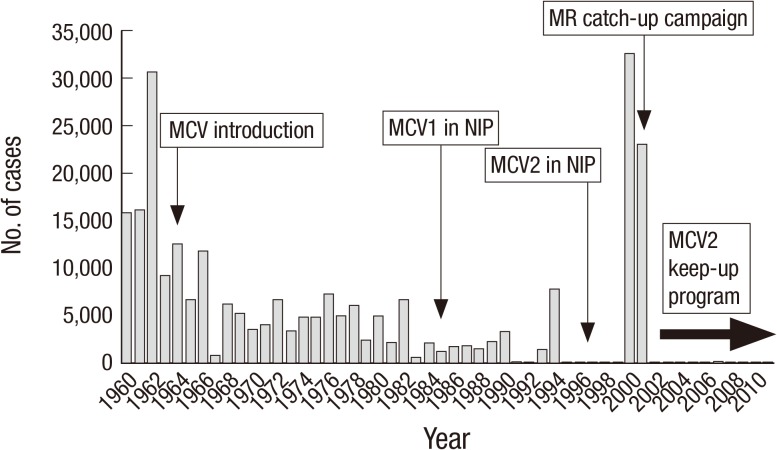
In the Republic of Korea, the annual number of notified cases has declined after the introduction of MCV in 1965, and further down to 1,000-1,800. The MCV1 was included in the National Immunization Program (NIP) in 1985, and MCV2 became recommended by Korean Society of Pediatrics since 1997 (Fig. 3) (28). However in 2000-2001, a nationwide epidemic of measles with more than 50,000 reported cases prompted the government to implement the Five Year Measles Elimination Program that included a catch-up vaccination program targeting population with 8-16 yr of age; a keep-up program that required all children entering first grade elementary school to present a certificate of second dose of MCV vaccination (Table 2) (29).
Fig. 3. Change in the incidence of measles in the Republic of Korea, 1960-2012.
Table 2. Measles timeline in the Republic of Korea, 1965-2014.
| Timeline | Events |
|---|---|
| 1965 | Introduction monovalent vaccine (MCV1) |
| Early 1980 | Introduction of MMR (12-15 months of age) |
| 1983 | Introduction of MMR into NIP |
| 1989-1990 | Outbreak of 5,809 cases |
| 1993-1994 | Outbreak of 9,386 cases |
| 1997 | Recommendation of MCV2 by Korean Society of Pediatrics (4-6 yr of age) |
| 2000-2001 | Outbreak of 52,897 cases |
| 2001-2006 | Five-Year Measles Elimination Program |
| (1) Catch-up campaign (5.8 million) | |
| (2) Keep-up program (School entrance, 0.5-0.7 million annually) | |
| (3) Enhanced surveillance (Case-based & laboratory) | |
| 2006 | Declaration of measles elimination (< 1 case/million population) |
| 2006 | Outbreak of 15 cases (Kindergarten) |
| 2007 | Outbreak of 180 cases (Nosocomial transmission) |
| 2010 | Outbreak of 93 cases (Junior high school) |
| 2011 | Outbreak of 32 cases (Gyeongnam Province) |
| 2014 | WHO verification of measles elimination |
| : 2008-2013; 0.93 cases/million population | |
| : Average of 47.5 confirmed annual measles cases |
The recommendation of MCV2 in 1997 without NIP may have posed insufficient population immunity level to prevent the 2000-2001 epidemic because of low MCV2 coverage rate (30). In 2000, the estimated MCV1 and MCV2 coverages were 86.2% and 37.7% respectively among 14,032 children selected for national survey (31). Therefore, a strong mandatory MCV2 vaccination among children such as entering elementary school became in need. The early system involved passive reporting from doctors to issue certificate of MCV2 vaccination to the parents or guardians and demonstrated adequate validity. In a survey of doctors, 59.5% of the certificates depended on the medical records of clinic, 13.5% was immunization booklets, 23.7% was re-immunizations, 1.9% was confirmation of record of other clinics, and 1.4% was parents' statements or requests without evidence (32). A randomized survey in 2010 revealed an increase of vaccination coverage of 98.3% for MCV1 and 66.1% for MCV2 (33). The recent introduction of electronic registry of all vaccination records in Korea may further improve the MCV2 coverage and validity of the coverage data (34).
The routine surveillance of measles in Korea involves a passive reporting of clinically diagnosed cases. The case-based surveillance with laboratory confirmation should be conducted in all patients with fever, measles-like rash and one of cough, coryza and conjunctivitis, and the collection of serum and throat swab specimens became mandatory. In 2006, the active laboratory-based surveillance was established, which involved mandatory reports from sentinel laboratories to the Korea Centers for Disease Control and Prevention (KCDC) (35). When the KCDC receives direct notification from sentinel laboratories, the investigation team immediately starts an investigation of each case. To enhance the human resource capacities of immunization, the Field Management Training Program (FMTP) was established to train annually the health workers of more than 250 public health centers located across the country.
After implementation and improvement of the program, a number of annual reported cases have declined to less than one case per million persons, and Korea became the first nation in Western Pacific to declare the elimination in 2006. Between 2002 and 2005, a decrease in measles incidence was noted, whereas cyclical increases were noted from 2006 to 2011. Most cases were in the age groups 0-23 months and 12-17 yr (36). The two unexpected outbreaks of measles that occurred during 2006 in a kindergarten in Incheon, and during 2007 in which cases that were mostly nosocomial transmission (37,38). In 2010, an outbreak occurred in a junior high school that included 74 vaccine-modified measles cases with limited symptoms that resembled measles (39).
Although Korea experienced a series of resurgence of measles due to importation and healthcare-associated transmission in infants, the overall incidence and surveillance indicators met the WHO criteria for measles elimination. Following the Third Annual Meeting of the Regional Verification Commission for Measles Elimination in the Western Pacific Region in March 2014, Korea, Australia, Mongolia, and Macau China were verified to be measles-free for the first time since the criteria for measles-free verification were established in the region.
One of the keys to effectively control measles in Korea was the establishment of routine immunization of 2 dose before entrance to elementary school. As the population immunity reaches threshold to interrupt measles transmission among traditionally high risk group for measles infection, there are eventual shift in age from pre-school aged children to school aged children (40,41). Targeting school-aged children for school-based mass vaccination campaign therefore is a rational approach for attaining adequate population immunity and to interrupt measles transmission in high risk population. Moreover, a policy requiring measles vaccination certificate when entering schools have been successful in ensuring high vaccination coverage rate (42). The policy was also effective in decreasing measles incidence as observed in the United States, where the measles incidence was lower in states that had mandatory requirements for MCV2 at school entrance (43).
FUTURE PERSPECTIVES
As the smallpox was eradicated globally in 1980, marking the first time that humans have removed an infectious disease, this triumph should be replicated in the case of measles and other vaccine-preventable diseases. Yet, evaluation of the ongoing resurgence of measles in the Korea has been helpful in understanding the reasons for continued disease occurrence in the countries and areas of WPR. Reports from most outbreaks were caused by non-vaccinated or under-vaccinated population, importation, and weak surveillance system. The continued occurrence of measles demonstrates that the virus continues to circulate around the globe, albeit at low levels of incidence in the Regions of America and Korea. The recent adoption of two-dose vaccination strategy by China and Japan may contribute to the dramatic reduction of measles cases in the WPR. Because not all countries in the WPR have solid health infrastructure and system, continuous supplementary vaccination activities including keep-up, follow-up, and mop-up strategies would be necessary. Full investigation of remaining measles cases, including confirmation of genotypes and documentation of epidemiological assessment, would provide additional opportunities for prevention. At present, most cases of measles in the WPR occur in preschool-aged children and in unvaccinated or partially vaccinated children aged 1-2 yr old. These observations reinforce the need to ensure universal and timely vaccination against measles in the WPR, and sharing the experiences from Korea would be helpful to other member states and areas.
Footnotes
DISCLOSURE: No optential conflicts of interest are declared.
AUTHOR CONTRIBUTION: Study design: Lee JK. Writing: Choe YJ. Revision of the manuscript: all authors. Supervision and interpretation of data: Jee Y, Oh MD. Approval of final manuscript: all authors.
References
- 1.Cutts FT, Henderson RH, Clements CJ, Chen RT, Patriarca PA. Principles of measles control. Bull World Health Organ. 1991;69:1–7. [PMC free article] [PubMed] [Google Scholar]
- 2.Narain JP, Khare S, Rana SR, Banerjee KB. Epidemic measles in an isolated unvaccinated population, India. Int J Epidemiol. 1989;18:952–958. doi: 10.1093/ije/18.4.952. [DOI] [PubMed] [Google Scholar]
- 3.Knobler S, Lederberg J, Pray LA Institute of Medicine (US) Forum on Emerging Infections. Considerations for viral disease eradication lessons learned and future strategies: workshop summary. Washington, DC: National Academy Press; 2002. [PubMed] [Google Scholar]
- 4.Demicheli V, Rivetti A, Debalini MG, Di Pietrantonj C. Vaccines for measles, mumps and rubella in children. Cochrane Database Syst Rev. 2012;2:CD004407. doi: 10.1002/14651858.CD004407.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.van Boven M, Kretzschmar M, Wallinga J, O'Neill PD, Wichmann O, Hahné S. Estimation of measles vaccine efficacy and critical vaccination coverage in a highly vaccinated population. J R Soc Interface. 2010;7:1537–1544. doi: 10.1098/rsif.2010.0086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gidding HF. The impact of Australia's measles control programme over the past decade. Epidemiol Infect. 2005;133:99–105. doi: 10.1017/s0950268804003073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bonanni P, Bechini A, Boccalini S, Peruzzi M, Tiscione E, Boncompagni G, Mannelli F, Salmaso S, Filia A, Ciofi degli Atti M. Progress in Italy in control and elimination of measles and congenital rubella. Vaccine. 2007;25:3105–3110. doi: 10.1016/j.vaccine.2007.01.019. [DOI] [PubMed] [Google Scholar]
- 8.Perry RT, Gacic-Dobo M, Dabbagh A, Mulders MN, Strebel PM, Okwo-Bele JM, Rota PA, Goodson JL Centers for Disease Control and Prevention (CDC) Progress toward regional measles elimination: worldwide, 2000-2013. MMWR Morb Mortal Wkly Rep. 2014;63:1034–1038. [PMC free article] [PubMed] [Google Scholar]
- 9.Keja K, Chan C, Hayden G, Henderson RH. Expanded programme on immunization. World Health Stat Q. 1988;41:59–63. [PubMed] [Google Scholar]
- 10.From the Centers for Disease Control and Prevention. Progress toward global measles control and elimination, 1990-1996. JAMA. 1997;278:1396–1397. doi: 10.1001/jama.1997.03550170026011. [DOI] [PubMed] [Google Scholar]
- 11.de Quadros CA, Hersh BS, Nogueira AC, Carrasco PA, da Silveira CM. Measles eradication: experience in the Americas. Bull World Health Organ. 1998;76:47–52. [PMC free article] [PubMed] [Google Scholar]
- 12.de Quadros CA, Izurieta H, Carrasco P, Brana M, Tambini G. Progress toward measles eradication in the region of the Americas. J Infect Dis. 2003;187:S102–S110. doi: 10.1086/368032. [DOI] [PubMed] [Google Scholar]
- 13.McFarland JW, Mansoor OD, Yang B. Accelerated measles control in the Western Pacific region. J Infect Dis. 2003;187:S246–S251. doi: 10.1086/368039. [DOI] [PubMed] [Google Scholar]
- 14.Expanded programme on immunization (EPI) immunization schedules in the WHO Western Pacific Region, 1995. Wkly Epidemiol Rec. 1996;71:133–137. [PubMed] [Google Scholar]
- 15.Aylward RB, Bilous J, Tangermann RH, Sanders R, Maher C, Sato Y, Omi S. Strengthening routine immunization services in the Western Pacific through the eradication of poliomyelitis. J Infect Dis. 1997;175:S268–S271. doi: 10.1093/infdis/175.supplement_1.s268. [DOI] [PubMed] [Google Scholar]
- 16.Tangermann RH, Costales M, Flavier J. Poliomyelitis eradication and its impact on primary health care in the Philippines. J Infect Dis. 1997;175:S272–S276. doi: 10.1093/infdis/175.supplement_1.s272. [DOI] [PubMed] [Google Scholar]
- 17.Sniadack DH, Mendoza-Aldana J, Jee Y, Bayutas B, Lorenzo-Mariano KM. Progress and challenges for measles elimination by 2012 in the Western Pacific Region. J Infect Dis. 2011;204:S439–S446. doi: 10.1093/infdis/jir148. [DOI] [PubMed] [Google Scholar]
- 18.Progress towards measles elimination in the Western Pacific Region, 2009-2012. Wkly Epidemiol Rec. 2013;88:233–240. [PubMed] [Google Scholar]
- 19.Masuno K, Shibuya K. Measles elimination: lack of progress in the Western Pacific Region. Lancet. 2009;373:1008. doi: 10.1016/S0140-6736(09)60608-5. [DOI] [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention (CDC) Progress toward the 2012 measles elimination goal: Western Pacific Region, 1990-2008. MMWR Morb Mortal Wkly Rep. 2009;58:669–673. [PubMed] [Google Scholar]
- 21.Ma C, Hao L, Zhang Y, Su Q, Rodewald L, An Z, Yu W, Ma J, Wen N, Wang H, et al. Monitoring progress towards the elimination of measles in China: an analysis of measles surveillance data. Bull World Health Organ. 2014;92:340–347. doi: 10.2471/BLT.13.130195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Numazaki K. Current problems of measles control in Japan and Western Pacific Region. Vaccine. 2007;25:3101–3104. doi: 10.1016/j.vaccine.2007.01.105. [DOI] [PubMed] [Google Scholar]
- 23.Centers for Disease Control and Prevention (CDC) Measles outbreak and response: Fiji, February-May 2006. MMWR Morb Mortal Wkly Rep. 2006;55:963–966. [PubMed] [Google Scholar]
- 24.Sniadack DH, Mendoza-Aldana J, Huyen DT, Van TT, Cuong NV, Olive JM, Toda K, Hien NT. Epidemiology of a measles epidemic in Vietnam 2008-2010. J Infect Dis. 2011;204:S476–S482. doi: 10.1093/infdis/jir092. [DOI] [PubMed] [Google Scholar]
- 25.Centers for Disease Control and Prevention (CDC) Progress in global measles control, 2000-2010. MMWR Morb Mortal Wkly Rep. 2012;61:73–78. [PubMed] [Google Scholar]
- 26.Centers for Disease Control and Prevention (CDC) Progress toward measles elimination: Western Pacific Region, 2009-2012. MMWR Morb Mortal Wkly Rep. 2013;62:443–447. [PMC free article] [PubMed] [Google Scholar]
- 27.World Health Organization. The 23th meeting of technical advisory group meeting, Western Pacific Region; 2014 Jun 17-20. Geneva: World Health Organization; 2014. [Google Scholar]
- 28.Choe YJ, Bae GR. Current status of measles in the Republic of Korea: an overview of case-based and seroepidemiological surveillance scheme. Korean J Pediatr. 2012;55:455–461. doi: 10.3345/kjp.2012.55.12.455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bae GR, Choe YJ, Go UY, Kim YI, Lee JK. Economic analysis of measles elimination program in the Republic of Korea, 2001: a cost benefit analysis study. Vaccine. 2013;31:2661–2666. doi: 10.1016/j.vaccine.2013.04.014. [DOI] [PubMed] [Google Scholar]
- 30.Centers for Disease Control and Prevention (CDC) Elimination of measles: South Korea, 2001-2006. MMWR Morb Mortal Wkly Rep. 2007;56:304–307. [PubMed] [Google Scholar]
- 31.Korea Centers for Disease Control and Prevention. Nationwide vaccination coverage level: conceptual methodology and survey. Cheongju: Korea Centers for Disease Control and Prevention; 2009. [Google Scholar]
- 32.Lee K, Kim H, Shin E, Kim Y, Chang S, Choi J. Validity of measles immunization certificates submitted upon enrollment in an elementary school in Korea. J Prev Med Public Health. 2009;42:104–108. doi: 10.3961/jpmph.2009.42.2.104. [DOI] [PubMed] [Google Scholar]
- 33.Choe YJ, Yang JJ, Park SK, Choi EH, Lee HJ. Comparative estimation of coverage between national immunization program vaccines and non-NIP vaccines in Korea. J Korean Med Sci. 2013;28:1283–1288. doi: 10.3346/jkms.2013.28.9.1283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lee YK, Kwon Y, Kim DW, Song KM, Cho H, Kim CH, Go UY, Bae GR, Lee JK. 2009-2010 novel influenza A (H1N1) vaccination coverage in the Republic of Korea. Am J Infect Control. 2012;40:481–483. doi: 10.1016/j.ajic.2011.05.015. [DOI] [PubMed] [Google Scholar]
- 35.Choe YJ, Eom HS, Bae GR, Cho SI. Timely measles surveillance in the Republic of Korea, 2002-2009: impact of sentinel laboratory surveillance. J Med Virol. 2014;86:322–328. doi: 10.1002/jmv.23710. [DOI] [PubMed] [Google Scholar]
- 36.Choe YJ, Park YJ, Eom HS, Kim ES, Bae GR, Lee JK. Epidemiological features and surveillance performance of measles in the Republic of Korea, 2002-2011. Jpn J Infect Dis. 2013;66:290–294. doi: 10.7883/yoken.66.290. [DOI] [PubMed] [Google Scholar]
- 37.Choi WS, Sniadack DH, Jee Y, Go UY, So JS, Cho H, Bae GR, Lee DH, Kim K, Yoon HS, et al. Outbreak of measles in the Republic of Korea, 2007: importance of nosocomial transmission. J Infect Dis. 2011;204:S483–S490. doi: 10.1093/infdis/jir087. [DOI] [PubMed] [Google Scholar]
- 38.So JS, Go UY, Lee DH, Park KS, Lee JK. Epidemiological investigation of a measles outbreak in a preschool in Incheon, Korea, 2006. J Prev Med Public Health. 2008;41:153–158. doi: 10.3961/jpmph.2008.41.3.153. [DOI] [PubMed] [Google Scholar]
- 39.Choe YJ, Hu JK, Song KM, Cho H, Yoon HS, Kim ST, Lee HJ, Kim K, Bae GR, Lee JK. Evaluation of an expanded case definition for vaccine-modified measles in a school outbreak in South Korea in 2010. Jpn J Infect Dis. 2012;65:371–375. doi: 10.7883/yoken.65.371. [DOI] [PubMed] [Google Scholar]
- 40.Lau YL, Chow CB, Leung TH. Changing epidemiology of measles in Hong Kong from 1961 to 1990: impact of a measles vaccination program. J Infect Dis. 1992;165:1111–1115. doi: 10.1093/infdis/165.6.1111. [DOI] [PubMed] [Google Scholar]
- 41.Cullen RM, Walker WJ. Measles epidemics 1949-91: the impact of mass immunisation in New Zealand. N Z Med J. 1996;109:400–402. [PubMed] [Google Scholar]
- 42.Robbins KB, Brandling-Bennett D, Hinman AR. Low measles incidence: association with enforcement of school immunization laws. Am J Public Health. 1981;71:270–274. doi: 10.2105/ajph.71.3.270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Thomas A, Xu D, Wooten K, Morrow B, Redd S. Timing and effectiveness of requirements for a second dose of measles vaccine. Pediatr Infect Dis J. 1999;18:266–270. doi: 10.1097/00006454-199903000-00012. [DOI] [PubMed] [Google Scholar]