Abstract
Against the backdrop of population aging, this paper presents the analysis of need-standardised health care utilization among elderly in India. Based on nationally representative morbidity and health care survey 2004, we demonstrate that the need for health care utilization is indeed pro-poor in nature. However, the actual health care utilization is concentrated among richer sections of the population. Further, the decomposition analysis reveals that income has a very strong role in shifting the distribution of health care away from the poor elderly. The impact of income on utilization is well-demonstrated even at the ecological-level as states with higher per capita incomes have higher elderly health care utilization even as the levels of need-predicted distribution across these states are similar. We also find that the distribution of elderly across social groups and their educational achievements favours the rich and significantly contributes to overall inequality. Nevertheless, contribution of need-related self-assessed health clearly favours pro-poor inequality. In concluding, we argue that to reduce such inequities in health care utilization it is necessary to increase public investments in health care infrastructure including geriatric care particularly in rural areas and underdeveloped regions to enhance access and quality of health care for the elderly.
Keywords: Aged, Health Care, Surveys, Delivery of Health Care, Socioeconomic Factors
INTRODUCTION
The global share of older people (aged 60 yr or over) in world population increased from 9.2 percent in 1990 to 11.7 percent in 2013 and is projected to reach 21.1 per cent by 2050 (1). In absolute terms, the number of older persons (aged 60 yr or over) is expected to more than double, from 841 million people in 2013 to more than 2 billion in 2050. While such remarkable increase in share and number of elderly persons reflects our social, economic and health achievements but it also poses several challenges for countries with inadequate social security and restricted fiscal space for welfare programmes. India is one such country where population aging is emerging as a major concern as both the share and size of elderly population is increasing over time. In 2011, India had an elderly population (aged 60 yr or over) of 104 million constituting about 8.6 per cent of the total population. However, the elderly population is projected to reach 157 million by 2025 and 297 million in 2050 thus constituting for 11 per cent and 18 per cent of the total population, respectively (2). Clearly, aging can have profound impact on social, economic and political processes in the country and therefore concerted research and policy engagements are warranted to address the various dimensions of elderly well-being.
Healthy aging is a fundamental aspect of elderly well-being. The nationally representative morbidity and health care survey of India (3) reports health ailments in about 39 per cent of the elderly population (37 percent and 44 percent in rural and urban areas, respectively). Although, complaints of non-communicable diseases such as hypertension and diabetes are notable but disability-related ailments such as disorders of joints and bones, visual, locomotors and hearing disabilities are among the most commonly reported ailments among the elderly. However, with poor provisioning of geriatric care services in India it is unlikely that all elderly are able to access and utilize health care as per their need. The utilization of health care in accordance with need is a commonly accepted egalitarian principle and is expounded under norms of horizontal and vertical equity (4). While horizontal equity necessitates that "same set of health services, of comparable quality should be made available to all persons with similar health needs, irrespective of socioeconomic status, ability to pay, social or personal background" (5) the complementary norm of vertical equity demands "appropriate unequal treatment of unequals" (6).
It may be noted that these concepts are central to measurement and interpretation of health inequities. For example, need for health care is likely to be greater among older persons than compared to younger ones and can also vary by sex of the person. In fact, health care utilization is significantly influenced by both need and non-need related factors. Variables such as age, gender, and self-assessed health are a few indicators that proxy need for health care utilization, whereas income and education are among the non-need factors that are often correlated with health care utilization. Unlike need-based standardization, adjusting for non-need factors is also critical to estimate the correlation of the confounding variables (need factors) with health conditional on these additional variables. However, several studies provide imprecise description of health inequities by interpreting unstandardised distribution of health and health care utilization (7,8). Therefore, to measure inequity, any observed inequality in health care utilization must be standardized for such differences in need-related factors (6). After standardization, any residual inequality in utilization can be interpreted as horizontal inequity, which could be pro-rich, pro-poor or equally distributed across various socio-economic groups.
Need-standardized health care utilization is interpreted as the distribution that would be expected to be observed, irrespective of differences in the distribution of need factors across non-need factors such as income. Despite such relevance, the issue has remained a neglected aspect in policy research on elderly health and well-being in India or elsewhere. For instance, most of the empirical studies on inequalities in elderly health have primarily discussed the trends, patterns and differentials in ageing cross-classified by social, economic and demographic characteristics (10,11,12,13,14,15). Although, a few have exclusively focused on health status of elderly (8,16,17,18,19,20) but need-standardization was seldom emphasized upon. Clearly, an analysis of need-standardized distribution could inform regarding the magnitude of horizontal inequity in health care utilization across dimensions such as income, education and social groups. Also, information on need-standardized utilization can help to comprehend whether elderly in need are at least able to receive some health care.
With this backdrop, this article aims to examine the need-standardized distribution of health care utilization by elderly in India. It also unravels the magnitude of income-related horizontal equity in elderly health care utilization and argues for better health care coverage for the vulnerable sections of the population. Overall, it is expected that the findings can play a crucial role in creating and assessing policies aimed at eliminating the health care disadvantages among the elderly population. With this motivation, the rest of this article is organized as follows: Section 2 elaborates on the data, variables and methods used for analyzing the actual and need-expected health care distribution. Section 3 presents the key results with specific focus on describing the influence of living arrangement and financial dependence on health care utilization. Section 4 discusses the major findings and its policy implications particularly in the context of universal health care coverage in India. This section also reports some of the limitations and suggestions for further research. Section 5 concludes.
MATERIALS AND METHODS
Nationally representative data from Morbidity and Health Care Survey (60th round) of India is used for the analysis (3). This survey was conducted in 2004 by the National Sample Survey Organisation (NSSO), Ministry of Statistics and Programme Implementation, Government of India and covered a sample of over 73 thousand households (around 47 thousand in rural areas and 26 thousand in urban areas). Key information on aspects of hospitalisation (inpatient) and ambulatory (outpatient) care for a reference period of 365 days and 15 days respectively was collected through this survey. This article analyses the information on about 34,831 elderly (aged 60 and above) persons with focus on utilization of outpatient and inpatient care services in the last 15 days. At the outset, we acknowledge that need for health care is a rather elusive concept with considerable variations in its conception, measurement and interpretation (21,22). However, despite such intricacies, it is plausible to find reasonable information that proxy need for health care. For instance, demographic, health and morbidity status of an individual are most natural alternative (6). Even subjective information such as self-assessed health status can be reliably used to reflect need for health care in India (23). Therefore, 'need' is captured through a set of variables reflecting demographic and health status of the elderly. The analysis also controls for potential non-need factors to estimate the correlation of need variables with health care utilization conditional on these variables. The key non-need variable is wealth status captured through household monthly per capita consumption expenditure (MPCE) quintiles, health insurance, and financial independence of the elderly. In addition, pertinent non-need factors such as education, caste, and place of residence are also included in the analysis. The descriptive statistics of these variables are reported in Table 1.
Table 1. Descriptive statistics of need and non-need variables for elderly, India 2004.
| Variables | Sample (n) | Mean | Std. Dev. | Minimum | Maximum |
|---|---|---|---|---|---|
| Dependent variable | |||||
| Elderly reporting utilization | 34,831 | 0.251 | 0.433 | 0 | 1 |
| Need-related variables | |||||
| Male, 60-65 yr | 34,831 | 0.181 | 0.385 | 0 | 1 |
| 65-70 yr | 34,831 | 0.141 | 0.348 | 0 | 1 |
| 70-75 yr | 34,831 | 0.094 | 0.292 | 0 | 1 |
| 75-80 yr | 34,831 | 0.039 | 0.195 | 0 | 1 |
| 85 yr & above | 34,831 | 0.045 | 0.207 | 0 | 1 |
| Female, 60-65 yr | 34,831 | 0.181 | 0.385 | 0 | 1 |
| 65-70 yr | 34,831 | 0.149 | 0.356 | 0 | 1 |
| 70-75 yr | 34,831 | 0.092 | 0.290 | 0 | 1 |
| 75-80 yr | 34,831 | 0.036 | 0.186 | 0 | 1 |
| 80 yr & above | 34,831 | 0.041 | 0.199 | 0 | 1 |
| Self-assessed health: Poor | 34,831 | 0.227 | 0.419 | 0 | 1 |
| Non-need variables | |||||
| Financially independent | 34,831 | 0.335 | 0.472 | 0 | 1 |
| First MPCE quintile | 34,831 | 0.205 | 0.404 | 0 | 1 |
| Second MPCE quintile | 34,831 | 0.189 | 0.391 | 0 | 1 |
| Middle MPCE quintile | 34,831 | 0.232 | 0.422 | 0 | 1 |
| Fourth MPCE quintile | 34,831 | 0.185 | 0.388 | 0 | 1 |
| Highest MPCE quintile | 34,831 | 0.188 | 0.391 | 0 | 1 |
| Health insurance cover | 34,831 | 0.009 | 0.093 | 0 | 1 |
| Illiterate | 34,831 | 0.658 | 0.474 | 0 | 1 |
| Up to primary education | 34,831 | 0.196 | 0.397 | 0 | 1 |
| Secondary education | 34,831 | 0.103 | 0.303 | 0 | 1 |
| Higher education | 34,831 | 0.044 | 0.204 | 0 | 1 |
| Rural | 34,831 | 0.757 | 0.429 | 0 | 1 |
| Urban | 34,831 | 0.243 | 0.429 | 0 | 1 |
| Scheduled tribe | 34,831 | 0.066 | 0.248 | 0 | 1 |
| Scheduled caste | 34,831 | 0.174 | 0.379 | 0 | 1 |
| Other backward classes | 34,831 | 0.398 | 0.490 | 0 | 1 |
| Other social groups | 34,831 | 0.361 | 0.480 | 0 | 1 |
Regression-based indirect standardization (IS) approach is applied to arrive at need-standardised distribution of health care utilization (6,24,25). This procedure corrects the actual health care utilization distribution by comparing it with the distribution that would be observed if all elderly had their own need status but the same average effects as the entire sample. Since information on health care utilization is dichotomous (yes=1 and No=0) therefore a non-linear (probit) regression is used to describe the relationship between the binary health care utilization variable, yi, with (i=1, 2, ..., n) need (xj) and non-need (zk) variables where (j:1, 2, … m) and (k: 1, 2, … l). This probit specification P(.) is written as follows:
| yi=P(α + ∑jβjxji + ∑kγkzki) + εi |
where α is the regression constant, βj and γk are the respective parameters for variables (xj) and (zk) with εi as the regression residual.
Using the regression parameters, need-standardized utilization (ŷiIS) is obtained as the difference between actual and need-expected utilization (ŷiX) as follows:
| ŷiIS=yi - ŷiX + ŷimean |
Here ŷimean is the mean of the predicted health care utilization. Need-standardized utilization (ŷiIS) is interpreted as the distribution of health care utilization that would be observed, irrespective of differences in the distribution of the need factors across non-need correlates.
Following the descriptive analysis, concentration curve (CC) and concentration index (CI) are computed to discern the horizontal inequity in health care utilization (25). The CC plots the cumulative proportions of the elderly population (ranked by socioeconomic status) on the x-axis against the cumulative proportions of (standardized) health care utilization on y-axis. For interpretative purposes, if the incidence of health care utilization is evenly distributed across socioeconomic spectrum then the concentration curve would coincide with the diagonal (line of equality); if it is concentrated among higher (lower) income groups, then CC lies below (above) the diagonal; and farther the CC from the diagonal, greater would be the magnitude of inequality. In other words, we can find evidence of horizontal inequity if the CC for need-standardized care lies below the diagonal.
Further, horizontal inequity is tested by determining whether the standardised utilization is unequally distributed by across MPCE distribution. In the literature, probably due to poverty concerns, income-related horizontal inequity has received popular attention (24,26,27). This can be ascertained by computing the concentration index (CI) for need-standardised utilization (ŷiIS). CI could be written in many ways including the convenient covariance method (25) as follows:
| CI=2*Covariance(ŷiIS, ri)/ŷimean, |
where ŷiIS is the need-standardized health care utilization variable whose inequality is being measured, ŷimean is its mean, ri is the ith individual's fractional rank in the socioeconomic distribution. CI measures relative inequality and defines equity as a situation where the cumulative proportions of standardised utilization matches with cumulative population shares. Any mismatch between the two sets is defined as inequality. The CI ranges between +1 and -1 with zero depicting no inequality and large positive (negative) values suggesting disproportionately higher concentration of utilization among the rich (poor).
After obtaining estimates of horizontal inequity, it is of interest to probe further into the association of such inequities with key socioeconomic correlates. For this purpose, the computed concentration index for unstandardized health care utilization is decomposed to know the contributions of need and non-need factors. To elaborate, we work with a probit model for health care utilization whereby partial effects evaluated at the means are used as a linear approximation for this nonlinear model (28).
| yi=αm + ∑jβmjxji + ∑kγmkzki) + ui |
where the βmj and γmk are the partial effects of each variable treated as fixed parameters and evaluated at sample means (6). Thereafter, the concentration index can be decomposed into the contribution of each determinant, computed as the product of the explanatory variable's elasticity with respect to the determinant and the latter's concentration index as follows:
| CI=∑j(∑jβmjxmj/ym)Cj + ∑k(∑kγmkzmk/ym)Ck + GCu/ym |
Here an estimate of horizontal inequity can be obtained by subtracting the need contributions in the above decomposition equation from the overall unstandardized CI. It may be noted that because of linear approximation of the relationship this estimate of horizontal inequity will only be similar and not exactly equal to the concentration index for need-standardized utilization. However, the advantage of the approach is that it allows for a detailed analysis of both need and non-need related factors to understand the relative importance of each factor. All the analysis presented here is weighted as per the instructions available in NSSO (2006). The analysis is performed in Stata 10.0 statistical software.
Ethics statement
The present analysis was based on an anonymous public use data set with no identifiable information on the survey participants. The data were obtained from the Morbidity and Health Care Survey 2004 conducted by the National Sample Survey Organization, Government of India.
RESULTS
The findings from the nationally representative survey indicate that two-thirds of the elderly persons in India are aged below 70 yr and mostly reside in rural areas (76%). 66% of the elderly are illiterate whereas only 20% have received education up to primary level (up to 5 yr). The distribution of elderly across various social and religious groups corresponds with the all-India pattern. For instance, 17%, 7%, and 40% of the elderly are affiliated to scheduled caste (SC), scheduled tribes (ST), and other backward classes (OBC) which is similar to their respective share in national population. Elderly are more or less equally distributed across the quintiles of household monthly consumption expenditure (MPCE) for all-India. Most of the elderly reside with their family (12% with spouse only, 45% with spouse and other members, and 32% with children only). However, 40% of the elderly are either widowed or divorced and another 9% are living alone (including as inmate of old age home). Financial dependency is a major concern as only one-third of the elderly are self-dependent and nine percent are supported by spouse. One-half of the elderly fully or partly rely on children for economic support whereas a few depend on grandchildren (2%) and other relatives/non-relatives (4%).
Table 2 shows the actual (unstandardized), need-predicted and need-standardized distribution for the probability of an elderly reporting at least one visit to a doctor in the last 15 days prior to the survey. These probabilities are reported by gender, education, MPCE class, social group and place of residence. It is noted that actual observed utilization is greater among educated, richer and advantaged social groups. For example, compared to illiterates, elderly persons with higher education have reported 15 per cent higher health care utilization. Similarly, for those in the lowest MPCE quintile, the probability of reporting utilization is 9.2 percent lower than would be expected on average given their need, whereas the highest MPCE quintile report a probability of utilization that is 15.6 percent higher than expected. Such wide differences between actual and need expected utilization is also noted across social groups and in urban areas.
Table 2. Distribution (in %) of actual (unstandardized), need-predicted and need-standardized health care utilization in previous 15 days, India 2004.
| Parameters | Actual | Need-predicted | Difference | Need-standardized |
|---|---|---|---|---|
| Gender | ||||
| Female | 25.1 (0.008) | 24.6 (0.002) | 0.5 (0.007) | 24.6 (0.007) |
| Male | 25.1 (0.008) | 23.7 (0.002) | 1.4 (0.007) | 25.5 (0.007) |
| Education | ||||
| Illiterate | 21.4 (0.006) | 24.7 (0.002) | -3.2 (0.006) | 20.9 (0.006) |
| Up to primary education | 30.9 (0.013) | 23.9 (0.003) | 7.0 (0.012) | 31.1 (0.012) |
| Secondary education | 32.7 (0.018) | 22.4 (0.004) | 10.4 (0.018) | 34.5 (0.018) |
| Higher education | 35.6 (0.028) | 21.9 (0.005) | 13.7 (0.027) | 37.9 (0.027) |
| MPCE quintile | ||||
| Lowest | 15.9 (0.010) | 25.2 (0.003) | -9.2 (0.010) | 14.9 (0.010) |
| Second | 20.8 (0.011) | 24.6 (0.003) | -3.8 (0.011) | 20.4 (0.011) |
| Middle | 22.7 (0.011) | 24.1 (0.003) | -1.5 (0.010) | 22.7 (0.010) |
| Fourth | 28.4 (0.013) | 23.5 (0.003) | 5.0 (0.012) | 29.1 (0.012) |
| Highest | 38.9 (0.014) | 23.4 (0.003) | 15.6 (0.013) | 39.7 (0.013) |
| Social group | ||||
| Scheduled tribe | 12.3 (0.016) | 22.8 (0.005) | -10.6 (0.015) | 13.6 (0.015) |
| Scheduled caste | 21.2 (0.012) | 24.7 (0.003) | -3.5 (0.012) | 20.7 (0.012) |
| Other backward classes | 23.1 (0.008) | 24.2 (0.002) | -1.1 (0.008) | 23.0 (0.008) |
| Others | 31.4 (0.009) | 24.1 (0.002) | 7.3 (0.009) | 31.5 (0.009) |
| Place of residence | ||||
| Rural | 22.6 (0.006) | 24.3 (0.002) | -1.7 (0.006) | 22.5 (0.006) |
| Urban | 32.6 (0.012) | 23.7 (0.003) | 9.0 (0.011) | 33.1 (0.011) |
| All India | 25.1 (0.005) | 24.2 (0.001) | 0.9 (0.005) | 25.1 (0.005) |
Standard errors in parenthesis.
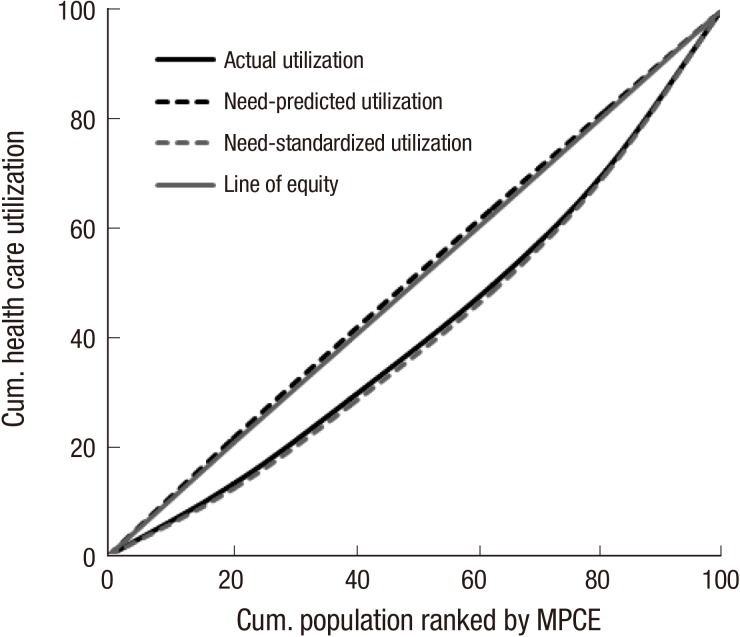
However, this utilization profile is unstandardized and does not account for varying need profile of the elderly population across these socioeconomic groups. In fact, the need-predicted distribution of health care utilization is noted to favour poor and vulnerable socioeconomic groups suggesting that these groups have greater unmet need for health care (Fig. 1). It is therefore observed that the need-standardized distribution shows even greater bias favouring the rich, educated and the advantaged social groups. As described above, the need-standardized utilization is interpreted as the distribution of health care utilization that would be observed, irrespective of differences in the distribution of the need factors across non-need correlates. This need-standardized distribution also indicates presence of inequities in health care utilization across income, education and social groups.
Fig. 1. Distribution (in %) of actual (unstandardized), need-predicted and need-standardized health care utilization in previous 15 days by MPCE quintiles, India 2004.
Fig. 2 shows the actual (unstandardized) and need-standardized distribution of health care utilization by major Indian states. It is immediately discernible that Jharkhand (9.4 percent) has the lowest actual health care utilization among elderly whereas Kerala reports the highest utilization (53.3 percent). As such, most of the states with low per capita incomes have low health care utilization, particularly among the poorer households. This can be noted from Table 3 which reports MPCE quintile specific distribution of actual and need-standardised distribution. The highest actual utilization probability of 61.3 percent is reported by elderly population belonging to the richest MPCE quintile in Kerala. In most of the states the need-standardized utilization is higher than unstandardised utilization thus indicating possible horizontal inequities in health care utilization. Also, this suggests that if need-related factors where distributed more equally across non-need factors such as income and education then the actual utilization would have increased across most of the states.
Fig. 2. Distribution (in %) of actual (unstandardized) and need-standardized health care utilization in previous 15 days, Major Indian states 2004.
Table 3. Distribution (in %) of actual (unstandardized) and need-standardized health care utilization in previous 15 days by MPCE quintiles, Major Indian states 2004.
| States | Lowest | Second | Middle | Fourth | Highest | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Actual | IS* | Actual | IS | Actual | IS | Actual | IS | Actual | IS | |
| Andhra Pradesh | 22.0 | 20.7 | 24.4 | 23.3 | 30.6 | 30.9 | 35.7 | 35.4 | 49.1 | 48.9 |
| Assam | 22.8 | 21.1 | 36.2 | 36.2 | 27.7 | 27.8 | 33.7 | 36.5 | 35.4 | 35.9 |
| Bihar | 8.0 | 7.9 | 15.4 | 14.4 | 19.1 | 20.1 | 16.9 | 16.9 | 18.7 | 20.2 |
| Chhattisgarh | 11.5 | 12.7 | 9.5 | 13.0 | 12.5 | 12.0 | 16.8 | 16.4 | 33.0 | 32.8 |
| Gujarat | 16.0 | 17.6 | 24.8 | 27.2 | 22.1 | 24.3 | 28.1 | 30.7 | 29.4 | 32.2 |
| Haryana | 17.2 | 16.9 | 19.6 | 21.3 | 13.6 | 14.4 | 21.5 | 23.8 | 32.3 | 32.4 |
| Himachal Pradesh | 21.7 | 20.1 | 21.9 | 22.9 | 21.7 | 23.3 | 26.6 | 28.8 | 36.4 | 37.4 |
| Jammu & Kashmir | 36.5 | 34.5 | 18.5 | 19.2 | 20.1 | 19.8 | 24.2 | 23.0 | 26.4 | 24.4 |
| Jharkhand | 3.8 | 0.6 | 13.1 | 12.0 | 7.8 | 8.1 | 16.0 | 18.0 | 17.9 | 19.0 |
| Karnataka | 11.1 | 12.6 | 19.3 | 18.5 | 15.7 | 16.5 | 19.0 | 20.8 | 32.4 | 34.9 |
| Kerala | 54.4 | 48.0 | 44.2 | 39.0 | 50.0 | 44.9 | 51.4 | 48.1 | 61.3 | 59.1 |
| Madhya Pradesh | 13.9 | 11.8 | 15.5 | 17.2 | 19.7 | 19.2 | 22.1 | 23.6 | 33.3 | 33.5 |
| Maharashtra | 18.4 | 18.7 | 27.4 | 27.8 | 26.4 | 27.2 | 30.2 | 31.9 | 45.6 | 47.2 |
| Orissa | 10.3 | 9.3 | 10.4 | 8.6 | 12.5 | 10.3 | 17.2 | 14.4 | 16.0 | 18.1 |
| Punjab | 5.3 | 4.1 | 24.3 | 23.6 | 25.8 | 28.4 | 32.6 | 33.4 | 42.2 | 42.7 |
| Rajasthan | 9.9 | 9.5 | 11.7 | 10.7 | 10.3 | 10.3 | 18.8 | 19.5 | 31.1 | 31.2 |
| Tamil Nadu | 20.9 | 22.1 | 17.0 | 18.4 | 18.1 | 21.4 | 27.2 | 30.0 | 34.9 | 38.0 |
| Uttar Pradesh | 19.1 | 17.1 | 19.9 | 19.5 | 19.1 | 19.0 | 25.5 | 26.0 | 32.4 | 32.6 |
| Uttaranchal | 3.9 | 9.3 | 1.3 | 3.6 | 15.1 | 14.8 | 14.4 | 12.8 | 28.9 | 32.5 |
| West Bengal | 24.5 | 20.9 | 30.5 | 26.9 | 33.0 | 29.5 | 36.0 | 35.4 | 43.8 | 42.3 |
Standard errors are not reported here due to space constraints. *IS refers to indirectly standardized estimates of health care utilization.
In Fig. 3, we plot the concentration curves (CC) for actual, need-predicted and need-standardized utilization for all-India. The CC for actual utilization lies below the diagonal (line of equity) and has a pro-rich bias indicating presence of significant income-related inequalities in elderly health care utilization in India. Although, the CC need-predicted utilization lies very close to the line of equity but it displays a marginal pro-poor bias in the distribution of need-predicted health care utilization. Consequently, the CC for need-standardised distribution shows even greater pro-rich bias in health care utilization. The concentration index (CI) values for the corresponding CCs for all-India are reported in the last row of Table 4. The (unstandardised) concentration index value of 0.172 (standard error: 0.008) further confirms a pro-rich distribution of health care utilization. The need-expected CI value of -0.016 (std. err. 0.002) informs that the need-expected distribution of health care utilization should have been more equal with a marginal pro-poor bias. Finally, the CI for need-standardised health care utilization also referred to as the horizontal inequity index is computed to be 0.188 (std. err. 0.008) indicating that income-related inequality in utilization is pro-rich. Alternatively, a similar value of horizontal inequity index is obtained as the difference between the CI for unstandardised (0.172) and need-expected (-0.016) utilization reported above. A positive horizontal inequity index confirms the pro-rich bias signifying income-related inequalities in health care utilization.
Fig. 3. Distribution of actual (unstandardized), need-predicted and need-standardized health care utilization in previous 15 days by MPCE quintiles, India 2004.
Table 4. Concentration index for actual (unstandardized), need predicted and need-standardized health care utilization in previous 15 days, major Indian states 2004.
| States | CI Unstandardized (std. err.) | CI Need-predicted (std. err.) | Horizontal inequity CI Need-standardized (std. err.) |
|---|---|---|---|
| Andhra Pradesh | 0.169 (0.025) | -0.010 (0.008) | 0.180 (0.024) |
| Assam | 0.034 (0.041) | -0.034 (0.012) | 0.060 (0.037) |
| Bihar | 0.164 (0.048) | -0.006 (0.009) | 0.175 (0.047) |
| Chhattisgarh | 0.103 (0.074) | -0.010 (0.014) | 0.109 (0.064) |
| Gujarat | 0.088 (0.039) | -0.008 (0.008) | 0.086 (0.036) |
| Haryana | 0.147 (0.050) | -0.002 (0.012) | 0.142 (0.045) |
| Himachal Pradesh | 0.119 (0.044) | -0.012 (0.011) | 0.123 (0.040) |
| Jammu & Kashmir | 0.032 (0.062) | 0.008 (0.018) | 0.025 (0.064) |
| Jharkhand | 0.250 (0.072) | -0.045 (0.015) | 0.408 (0.113) |
| Karnataka | 0.176 (0.041) | -0.017 (0.009) | 0.186 (0.039) |
| Kerala | 0.052 (0.015) | -0.031 (0.007) | 0.074 (0.015) |
| Madhya Pradesh | 0.130 (0.043) | -0.022 (0.009) | 0.161 (0.042) |
| Maharashtra | 0.165 (0.024) | -0.014 (0.007) | 0.170 (0.022) |
| Odisha | 0.074 (0.060) | 0.014 (0.009) | 0.049 (0.068) |
| Punjab | 0.146 (0.036) | 0.007 (0.011) | 0.138 (0.033) |
| Rajasthan | 0.219 (0.048) | -0.011 (0.009) | 0.237 (0.049) |
| Tamil Nadu | 0.144 (0.029) | -0.016 (0.006) | 0.143 (0.026) |
| Uttar Pradesh | 0.094 (0.024) | -0.018 (0.006) | 0.117 (0.023) |
| Uttarakhand | 0.382 (0.083) | 0.024 (0.016) | 0.308 (0.072) |
| West Bengal | 0.109 (0.023) | -0.023 (0.007) | 0.137 (0.024) |
| All India | 0.172 (0.008) | -0.016 (0.002) | 0.188 (0.008) |
Table 4 also reports the state-wise concentration index for unstandardized, need-predicted and need-standardised elderly health care utilization. Without exception, actual health care utilization in all the states has a pro-rich bias. The magnitude of such income-related inequalities are very high in Uttarakhand (CI: 0.382), Jharkhand (CI: 0.250) and Rajasthan (CI: 0.219). Interestingly, as noted by the negative CI values, in most of the states the need-predicted distribution has a significant pro-poor bias indicating that elderly from poorer households are expected to be in greater need for health care utilization. The pro-poor bias is marginally higher in case of Jharkhand (CI: -0.045) and Kerala (CI: -0.031). The CI for need-standardised distribution or the horizontal inequity index is therefore significantly positive for all the states. These figures also informs that the magnitude of horizontal inequity is comparatively higher in Jharkhand (CI: 0.408), Uttarakhand (CI: 0.308) and Rajasthan (CI: 0.237). Thus this state-wise analysis presents the extent to which standardized use is unequally distributed across income. Similarly, Table A1 and Table A2 in the appendix also confirm of significant horizontal inequities that manifest along the dimension of educational and social groups.
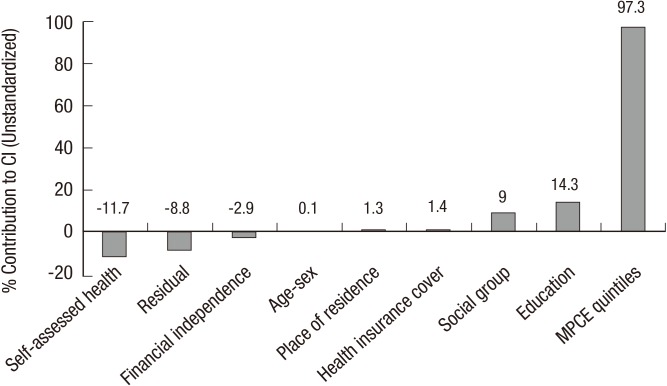
Finally, we decompose the concentration index for elderly health care utilization in India. The decomposition allows us to understand the relative importance of each variable and its distribution in magnifying horizontal inequity. Given the nature of data, we have estimated the probability of health care utilization by using a probit model. In this case, we make a linear approximation to the model using the partial effects evaluated at sample means. The detailed decomposition results are presented in Table 5. The partial effects estimated at sample means bear expected signs. For instance, the demographic (age and sex interactions) variables show that health care utilization increases with age but it declines after reaching higher ages of 85 and above. Also, elderly reporting poor self-assessed health have 25 percent higher probability of health care utilization. Non-need factors also share expected associations. For instance, income has a positive impact on health care utilization with greater marginal effects associated with elderly from richest MPCE quintiles. Similarly, education also has a favourable impact on health care utilization whereas elderly belonging to backward and disadvantaged social groups are likely to have lower health care utilization. The elasticities associated with each of these need and non-need factors is also presented. In case of need-related variables, self-assessed health is relatively elastic and indicates over 23 percent increase in chances of utilization if elderly report poor health. In case of non-need factors, income has the highest elasticity and thus is a major determinant of elderly health care utilization. Interestingly, primary education is found to have greater elasticity than other educational categories. The concentration index for each of the explanatory variables are also reported and shows a pro-poor bias (negative CI values) in case of need-related factors whereas greater pro-rich inequalities (positive CI values) are noted for non-need factors.
Table 5. Probit model based contributions to Concentration index (unstandardized) and horizontal inequity index for health care utilization in previous 15 days, India 2004.
| Variables | Partial effects | 95% Conf. | Int. | Elasticity | CI (x/z) | Cont. to CI | % Cont. |
|---|---|---|---|---|---|---|---|
| Need factors | |||||||
| Male, 65-70 yr | 0.026 | 0.025 | 0.026 | 0.015 | -0.019 | -0.0003 | -0.2 |
| 70-75 yr | 0.038 | 0.038 | 0.039 | 0.014 | 0.009 | 0.0001 | 0.1 |
| 75-80 yr | 0.060 | 0.060 | 0.061 | 0.009 | 0.050 | 0.0005 | 0.3 |
| 85 yr & above | -0.019 | -0.020 | -0.019 | -0.003 | 0.041 | -0.0001 | -0.1 |
| Female, 60-65 yr | -0.001 | -0.001 | 0.000 | -0.001 | -0.022 | 0.0000 | 0.0 |
| 65-70 yr | 0.006 | 0.006 | 0.007 | 0.004 | -0.031 | -0.0001 | -0.1 |
| 70-75 yr | 0.043 | 0.043 | 0.044 | 0.016 | -0.004 | -0.0001 | 0.0 |
| 75-80 yr | 0.026 | 0.026 | 0.027 | 0.004 | 0.074 | 0.0003 | 0.2 |
| 80 yr & above | -0.008 | -0.009 | -0.008 | -0.001 | 0.094 | -0.0001 | -0.1 |
| Self-assessed health: Poor | 0.254 | 0.254 | 0.255 | 0.230 | -0.088 | -0.0202 | -11.7 |
| Subtotal (Need) | -0.0200 | -11.6 | |||||
| Non-need factors | |||||||
| Financially independent | -0.041 | -0.041 | -0.041 | -0.054 | 0.091 | -0.0050 | -2.9 |
| Second MPCE quintile | 0.061 | 0.060 | 0.061 | 0.046 | -0.436 | -0.0198 | -11.5 |
| Middle MPCE quintile | 0.078 | 0.077 | 0.078 | 0.072 | -0.077 | -0.0056 | -3.2 |
| Fourth MPCE quintile | 0.142 | 0.141 | 0.142 | 0.105 | 0.384 | 0.0402 | 23.3 |
| Highest MPCE quintile | 0.225 | 0.225 | 0.226 | 0.169 | 0.903 | 0.1528 | 88.7 |
| Health insurance cover | 0.101 | 0.100 | 0.102 | 0.004 | 0.701 | 0.0025 | 1.4 |
| Up to primary education | 0.065 | 0.065 | 0.065 | 0.051 | 0.137 | 0.0070 | 4.0 |
| Secondary education | 0.060 | 0.060 | 0.061 | 0.025 | 0.429 | 0.0106 | 6.1 |
| Higher education | 0.052 | 0.051 | 0.053 | 0.009 | 0.785 | 0.0071 | 4.1 |
| Urban | 0.004 | 0.004 | 0.005 | 0.004 | 0.535 | 0.0023 | 1.3 |
| Scheduled tribe | -0.101 | -0.102 | -0.101 | -0.027 | -0.239 | 0.0064 | 3.7 |
| Scheduled caste | -0.036 | -0.037 | -0.036 | -0.025 | -0.195 | 0.0049 | 2.9 |
| Other backward classes | -0.031 | -0.031 | -0.031 | -0.049 | -0.085 | 0.0042 | 2.4 |
| Subtotal (Non-need) | 0.2075 | 120.4 | |||||
| Residual | -0.0152 | -8.8 | |||||
| CI (Unstandardized) | 0.1723 | 100.0 | |||||
| Horizontal inequity index | 0.1923 |
All the partial effects are significant at 99 percent. Pseudo R2=0.0903; Unweighted N=34,831.
The contribution of each of these variables to the unstandardized concentration index is reported in the last two columns of the table (also see Fig. 4). These contributions are obtained as the product of the explanatory variable's elasticity with respect to the determinant and the latter's concentration index. Overall, the contribution of need-related variables is negative indicating that if utilization were determined by need alone, it would be pro-poor. The aggregate contribution of all non-need factors is 11.6 percent of the unstandardized concentration index. In fact, all of this contribution is due to only one variable of self-rated health as other need variables (age and sex) have low elasticity and are more or less equally distributed across income quintiles. Interestingly, the pro-poor push rendered by the need variables is more than offset by the direct effect of non-need factors including income, education and social groups. In fact, if need were distributed equally, the direct effect of these non-need factors would produce a concentration index 20.4 percent greater than the observed CI for unstandardized utilization.
Fig. 4. Contributions (in %) to concentration index for health care utilization in last-15 days, India 2004.
The decomposition results also facilitate estimation of horizontal inequity as it can be obtained by subtracting the need contributions (-0.020) in the decomposition from the overall unstandardized CI (0.172). Thus the horizontal inequity index yields a value of 0.192. It may be noted that this estimate of horizontal inequity marginally differs from the estimate of 0.188 that is reported in Table 3 and is caused due to assumed linear approximation for the probit model. However, it is reassuring that the difference is negligible as compared to possible anomalies associated with some nonlinear models (6,29). Nevertheless, both the techniques of estimating horizontal inequity indicate that for given need, elderly belonging to the better-off sections of the society have greater utilization of health care services in India. The analysis also establishes that the assumption of greater concentration of illness among the poor is justified though the need-predicted concentration is relatively lower than expected.
DISCUSSION AND CONCLUSION
It is widely acknowledged that health inequity and health inequalities are two related but distinct concepts. The latter is an empirical construct referring to differences in health status between different groups whereas the former is a normative concern focusing on those inequalities that are judged to be unjust or unfair because they result from socially derived processes (30,31,32). Despite such conceptual understanding, most of the studies fail to provide an apt description of health distribution and instead (unknowingly) confuse interpretation of health inequalities with health inequities (33). Particularly, studies on elderly health and health care seldom appreciate such intricacies (8,34). It is obvious that with increasing age there would be a greater need for health care. However, such age-related differences (or any need-related differences) cannot be simply identified as health inequities. In fact, a few studies explicitly identify it as a problem related to data availability and interpretation of health inequities (9). In this context, this study contributes by providing the analysis of need-standardised health care utilization by elderly in India.
The results confirm that income-related inequities and inequalities in health care utilization are a prominent concern for elderly well-being. In particular, results reveal of huge socioeconomic inequalities in health care utilization that favours the rich and the advantaged sections of the elderly population. While it is suggested that any distribution of health care that is not pro-poor reflects horizontal inequity (9) but it may be noted that the magnitude of such inequities can be higher than what is observed through unstandardized analysis. In fact, in the Indian context the reports of any ailments during the last 15 days (prior to the survey) also display a pro-rich bias and require need-standardization. For instance, only 22.6 percent of the elderly in lowest MPCE quintile report of ailing during the last 15 days as compared to 43.2 percent from the highest quintile. The concentration index value for such reporting is 0.123 (0.109, 0.136). Clearly, not only utilization but also reporting of ailments displays a pro-rich bias whereas it is expected that sickness will be concentrated among the poorer sections.
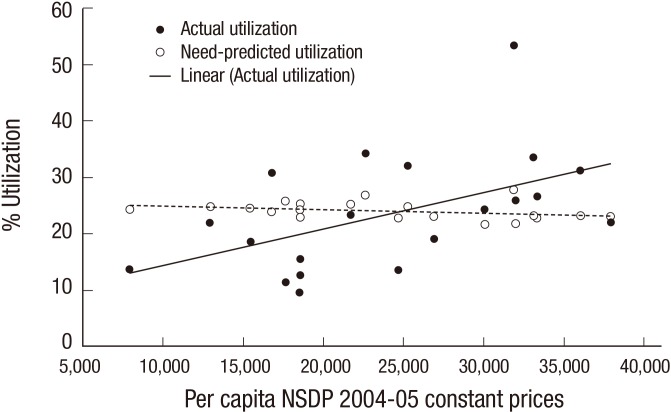
This study effectively demonstrates that the need for health care utilization is indeed pro-poor in nature. Also, with a CI value of -0.015 (-0.019, -0.011), we find that the need-predicted distribution of ailing is pro-poor in nature. Given such pro-poor nature of need-distribution, it is no surprise that the need-standardized distribution of health care utilization reveals an even greater magnitude of inequity than compared to the unstandardized estimates. The decomposition analysis reveals that income has a very strong role in shifting the distribution away from the poor. The distribution of elderly across social groups and their educational achievements also favour the rich and significantly contribute to overall inequality. Although, contribution of age-sex related factors to overall inequality is more or less negligible but poor self-assessed health clearly favours pro-poor inequality. Urban residency and health insurance also have a small role in engendering income-related inequality in health care utilization. The impact of income on utilization is well-demonstrated even at the macro-level. For example, Fig. 5 shows that states with higher per capita net state domestic product (PCNSDP) tend to have higher elderly health care utilization even as the need-predicted distribution across these states is more or less similar (or marginally in favour of poorer states).
Fig. 5. Association of actual utilization and need-predicted utilization with state per capita NSDP, Indian states 2004.
To some extent, India's experience is similar to that of Mexico where insurance is a major driver of pro-rich inequalities in health care utilization (35). This situation of non-need driven health care utilization is a major concern for India and it is likely that this problem is not unique to elderly population but also is common among non-elderly persons. This is in sharp contrast to the experience of countries such as Brazil and the United States where need-standardized health care utilization is found to be pro-poor in nature (26,27). In fact, in Brazil health care utilization is becoming more equal over time and much of these improvements are associated with better health policies. Clearly, India has to learn from the policies and approaches from several other countries and should display greater socio-political willingness to achieve health equity.
To reduce such inequities it is necessary to increase public investments in health care infrastructure including geriatric care particularly in rural areas and underdeveloped regions to enhance access and quality of care. Since horizontal inequity is rampant along the dimensions of gender, education and caste therefore utilization by females, illiterates and lower caste (SC, ST and OBC) should be improved through strategies and approaches bearing a non-discriminatory social outlook. This also implies targeting contextual effects that have direct relevance for elderly well-being and cannot be discussed in isolation with structural factors including economic history, infrastructure and socio-political background. In this regard, expansion of the formal sector and policies for elderly social security provisions are key areas for engagement in an expanding market economy with huge informal sector (36).
It is worrisome to note that elderly population in India does not have adequate insurance provisions. Although, in recent years the coverage of insured population may have increased due to several national (such as Rashtriya Swasthya Bima Yojana) and subnational policy initiatives (such as Arogyashree Scheme) but high out of pocket health care expenditure in the private sector remains a formidable concern. Besides, it increases the risk of catastrophic health care expenditure even among better-off households which therefore may refrain from investing in elderly health (37). Moreover, utilization above expected profile (over-medicalisation) may have implications for costs and resource allocations but amidst highly privatised tertiary care sector this issue has not received adequate policy attention. Clearly, all such determinants can intensify health inequalities whereby a majority of the elderly population may fail to enjoy the good health that is biologically possible. In view of such intricacies, strengthening policies for universal health care coverage is a pragmatic way forward to enhance elderly well-being.
Also, with demographic and epidemiological transition, it is necessary to increase awareness among the vulnerable social groups and enhance their capacity to assess health care needs related to non-communicable diseases. Specifically, the role of information campaigns increases manifold because of massive illiteracy among elderly and other disadvantaged socioeconomic groups. Such initiatives, however, should be accompanied by expansion of the public health sector through nation-wide health care programmes. Even though the National Rural Health Mission (NRHM) has improved the supply side situation in the last decade but specific institutional provisions for geriatric care are warranted. In this regard, notable efforts by the Indian system of medicine, Non-Governmental Organizations (NGOs), and Accredited Social Health Activists (ASHAs) as visible under NRHM offers vital insights for envisioning strategies to promote 'healthy ageing'. Presumably, improvements in recruitment and retention policies for human resources (specialists, doctors and community health workers) would also constitute one component of the solutions. However, so far there are no encouraging signs that would signify preparedness or policy intention to enhance elderly well-being (36).
In concluding, three limitations are worth highlighting. First, it must be noted that the analysis assumes that vertical equity norm is satisfied and that the quality and quantity of care received by elderly is in accordance with their need. However, there can be considerable violation of the equity norms as several elderly persons can perhaps receive inadequate health care for various reasons. Second, the estimates of horizontal inequity are sensitive to the need variables included in the analysis. In this regard, it is important that scope for using better proxy variables for analyzing need-standardized health care utilization. It is also worthwhile to note that the estimates could differ with the type of linear approximation of the nonlinear model and deserves further research attention. Third, the available data for ageing research in India is often a byproduct of health surveys with different motivations (such as reproductive health or health care expenditure) and provides limited information to proxy need for health care. Hence, it would be useful to entail a 'symptoms approach' consisting of non-technical questions about health status and medical care to understand health care need (38). Needless to say, quality data and information can go a long way in supporting policy research and policy decisions for elderly well-being.
ACKNOWLEDGMENTS
Joe W is thankful to the Lown Scholars Program of Harvard T H Chan School of Public Health for research support. Joe W and Rudra S are thankful to Udaya Shankar Mishra for helpful discussions on the subject matter of the paper. Joe W also thanks Abhishek for excellent research assistance. Usual disclaimer applies.
Appendix Table A1
Distribution (in %) of actual (unstandardized) and need-standardized health care utilization in previous 15 days by social groups, major Indian states 2004.
| States | Scheduled tribe | Scheduled caste | Other backward classes | Others | ||||
|---|---|---|---|---|---|---|---|---|
| Actual | IS* | Actual | IS | Actual | IS | Actual | IS | |
| Andhra Pradesh | 19.9 | 20.5 | 27.0 | 25.5 | 29.9 | 29.4 | 39.9 | 39.7 |
| Assam | 23.3 | 23.8 | 20.8 | 20.9 | 31.4 | 32.2 | 34.0 | 34.2 |
| Bihar | 3.6 | -5.4 | 15.1 | 13.9 | 11.7 | 12.2 | 16.9 | 17.0 |
| Chhattisgarh | 8.1 | 10.9 | 25.3 | 22.9 | 11.1 | 12.5 | 30.2 | 27.8 |
| Gujarat | 11.0 | 12.8 | 31.8 | 32.7 | 22.0 | 24.6 | 31.6 | 34.6 |
| Haryana | 0.0 | 7.7 | 16.3 | 15.5 | 25.3 | 27.1 | 22.2 | 23.6 |
| Himachal Pradesh | 20.0 | 21.8 | 20.4 | 22.9 | 28.7 | 28.7 | 29.3 | 30.3 |
| Jammu & Kashmir | 4.8 | 5.0 | 16.7 | 12.0 | 25.9 | 27.9 | 24.7 | 24.5 |
| Jharkhand | 6.7 | 8.5 | 3.3 | -0.2 | 9.6 | 7.5 | 15.3 | 16.2 |
| Karnataka | 21.3 | 23.6 | 9.7 | 9.2 | 19.0 | 20.4 | 21.1 | 22.4 |
| Kerala | 35.2 | 36.7 | 48.6 | 43.4 | 53.9 | 49.3 | 33.7 | 37.0 |
| Madhya Pradesh | 10.3 | 10.3 | 18.0 | 17.3 | 18.9 | 19.0 | 23.7 | 23.1 |
| Maharashtra | 20.3 | 21.7 | 16.6 | 16.5 | 24.7 | 25.9 | 40.7 | 41.8 |
| Orissa | 6.8 | 6.8 | 12.9 | 11.2 | 12.5 | 10.9 | 12.7 | 10.7 |
| Punjab | 0.0 | 5.9 | 30.2 | 30.7 | 26.8 | 28.5 | 37.8 | 38.8 |
| Rajasthan | 7.2 | 9.3 | 10.5 | 10.5 | 16.1 | 15.4 | 20.5 | 20.6 |
| Tamil Nadu | 0.6 | 2.8 | 17.8 | 20.5 | 25.3 | 27.8 | 17.9 | 16.4 |
| Uttar Pradesh | 6.5 | 11.1 | 21.2 | 21.1 | 20.6 | 19.3 | 24.8 | 25.4 |
| Uttaranchal | 24.5 | 30.7 | 14.5 | 18.2 | 5.0 | 7.2 | 14.3 | 15.2 |
| West Bengal | 15.0 | 16.3 | 30.5 | 28.2 | 30.7 | 26.5 | 36.5 | 33.8 |
Standard errors are not reported here due to space constraints. *IS refers to indirectly standardized estimates of health care utilization.
Appendix Table A2
Distribution (in %) of actual (unstandardized) and need-standardized health care utilization in previous 15 days by education, major Indian states 2004.
| States | Illiterate | Up to primary | Up to secondary | Higher | ||||
|---|---|---|---|---|---|---|---|---|
| Actual | IS* | Actual | IS | Actual | IS | Actual | IS | |
| Andhra Pradesh | 26.6 | 25.9 | 46.1 | 46.7 | 48.4 | 47.3 | 53.9 | 52.9 |
| Assam | 31.5 | 31.0 | 32.1 | 33.7 | 19.2 | 19.0 | 32.5 | 35.3 |
| Bihar | 13.1 | 12.4 | 12.7 | 13.2 | 17.6 | 20.4 | 13.1 | 15.9 |
| Chhattisgarh | 11.9 | 13.3 | 11.8 | 14.6 | 6.3 | 1.4 | 37.9 | 33.2 |
| Gujarat | 23.0 | 25.0 | 30.7 | 34.0 | 27.1 | 29.1 | 36.3 | 41.1 |
| Haryana | 21.5 | 22.1 | 24.5 | 26.5 | 21.9 | 25.4 | 20.0 | 22.7 |
| Himachal Pradesh | 24.5 | 25.1 | 29.7 | 32.1 | 33.1 | 37.1 | 37.3 | 43.5 |
| Jammu & Kashmir | 23.4 | 21.5 | 29.7 | 30.2 | 17.3 | 21.4 | 23.6 | 25.8 |
| Jharkhand | 7.8 | 6.5 | 4.3 | 2.3 | 22.9 | 25.8 | 14.9 | 14.6 |
| Karnataka | 15.4 | 16.0 | 25.6 | 26.6 | 21.7 | 25.4 | 44.2 | 46.1 |
| Kerala | 52.0 | 45.2 | 54.9 | 51.4 | 51.7 | 51.6 | 53.4 | 54.2 |
| Madhya Pradesh | 16.4 | 15.8 | 25.0 | 25.9 | 25.1 | 26.3 | 23.5 | 24.8 |
| Maharashtra | 27.9 | 28.4 | 31.4 | 32.0 | 38.2 | 40.9 | 44.1 | 48.0 |
| Orissa | 10.6 | 8.5 | 12.3 | 12.1 | 18.5 | 18.6 | 7.5 | 13.4 |
| Punjab | 33.4 | 33.4 | 35.4 | 37.6 | 35.4 | 38.6 | 19.0 | 25.4 |
| Rajasthan | 13.6 | 13.3 | 19.9 | 20.7 | 21.1 | 21.3 | 34.1 | 33.8 |
| Tamil Nadu | 18.5 | 20.8 | 30.9 | 33.6 | 38.6 | 42.3 | 31.2 | 35.1 |
| Uttar Pradesh | 21.0 | 19.9 | 21.0 | 21.9 | 27.5 | 29.0 | 31.3 | 33.8 |
| Uttaranchal | 12.0 | 12.6 | 9.0 | 10.7 | 18.8 | 22.2 | 30.9 | 36.8 |
| West Bengal | 30.2 | 26.7 | 36.3 | 33.1 | 37.8 | 37.6 | 45.5 | 46.8 |
Standard errors are not reported here due to space constraints. *IS refers to indirectly standardized estimates of health care utilization.
Footnotes
AUTHOR CONTRIBUTION: Design of the study: Joe W, Rudra S, Subramanian SV. Data analysis: Joe W, Rudra S. Writing the first draft: Joe W, Rudra S. Revision of manuscript: Joe W, Rudra S, Subramanian SV. Approval of final manuscript: all authors.
References
- 1.United Nations. World population ageing 2013. ST/ESA/SER.A/348. New York: Department of Economic and Social Affairs, Population Division; 2013. [Google Scholar]
- 2.Giridhar G, Sathyanarayana K, Kumar S, James K, Alam M. Population ageing in India. Delhi: Cambridge University Press; 2014. [Google Scholar]
- 3.National Sample Survey Organisation. Morbidity health care and the condition of aged: report no 507. New Delhi: Ministry of Statistics and Programme Implementation; 2006. [Google Scholar]
- 4.Wagstaff A, van Doorslaer E. Equity in health care finance and delivery. In: Culyer AJ, Newhouse JP, editors. Handbook of Health Economics (1B) Amsterdam: Elsevier; 2000. pp. 1803–1862. [Google Scholar]
- 5.High Level Expert Group (HLEG) High level expert group report on universal health coverage for India. New Delhi: Planning Commission; 2011. [PMC free article] [PubMed] [Google Scholar]
- 6.O'Donnell O, van Doorslaer E, Wagstaff A, Lindelow M. Analysing health equity using household survey data: a guide to techniques and their implementation. Washington, DC: The World Bank; 2008. [Google Scholar]
- 7.Mukherjee S, Levesque JF. Changing inequalities in Utilisation of inpatient care in rural india: evidence from the NSS. Econ Polit Wkly. 2010;45:85. [Google Scholar]
- 8.Goli S, Singh L, Jain K, Pou L. Socioeconomic determinants of health inequalities among the older population in India: a decomposition analysis. J Cross Cult Gerontol. 2014;29:353–369. doi: 10.1007/s10823-014-9251-8. [DOI] [PubMed] [Google Scholar]
- 9.O'Donnell O, van Doorslaer E, Rannan-Eliya RP, Somanathan A, Adhikari SR, Akkazieva B, Harbianto D, Garg CC, Hanvoravongchai P, Herrin AN, et al. Who pays for health care in Asia? J Health Econ. 2008;27:460–475. doi: 10.1016/j.jhealeco.2007.08.005. [DOI] [PubMed] [Google Scholar]
- 10.Sathyanarayana KM, Kumar S, James KS. Living arrangements of elderly in India: policy and programmatic implications. New Delhi: United Nations Population Fund; 2012. [Google Scholar]
- 11.Bongaarts J, Zimmer Z. Living arrangements of older adults in the developing world: an analysis of demographic and health survey household surveys. J Gerontol B Psychol Sci Soc Sci. 2002;57:S145–S157. doi: 10.1093/geronb/57.3.s145. [DOI] [PubMed] [Google Scholar]
- 12.Rajan SI, Mishra U, Sarma P. Living arrangements among the Indian elderly. Hong Kong J Gerontol. 1995;9:20–28. [Google Scholar]
- 13.Gupta I, Sankar D. Health of the elderly in India: a multivariate analysis. J Health Popul Dev Countries. 2003;24:1–11. [Google Scholar]
- 14.Rajan SI, Kumar S. Living arrangements among Indian elderly: new evidence from national family health survey. Econ Polit Wkly. 2003;38:75–80. [Google Scholar]
- 15.Rajan SI, Mathew ET. India. In: Irudaya Rajan S, editor. Social security for the elderly : experiences from South Asia. New Delhi: Routledge; 2008. pp. 39–106. [Google Scholar]
- 16.Alam M. Ageing in India: socio-economic and health dimensions. New Delhi: Academic Foundation; 2006. [Google Scholar]
- 17.Alam M, Karan A. Elderly health in India: dimension, differentials and determinants, BKPAI Working Paper No. 3. New Delhi: United Nations Population Fund (UNFPA); 2011. [Google Scholar]
- 18.Siva Raju S. Health status of the urban elderly: a medico-social study. Delhi: B. R. Publishing Co; 2002. [Google Scholar]
- 19.Mini GK. Socioeconomic and demographic diversity in the health status of elderly people in a transitional society, Kerala, India. J Biosoc Sci. 2009;41:457–467. doi: 10.1017/S0021932008003003. [DOI] [PubMed] [Google Scholar]
- 20.Agrawal S. Effect of living arrangement on the health status of elderly in India. Asian Popul Stud. 2012;8:87–101. doi: 10.1080/17441730.2012.646842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Culyer AJ. Need: the idea won't do--but we still need it. Soc Sci Med. 1995;40:727–730. doi: 10.1016/0277-9536(94)00307-f. [DOI] [PubMed] [Google Scholar]
- 22.Culyer AJ, Wagstaff A. Equity and equality in health and health care. J Health Econ. 1993;12:431–457. doi: 10.1016/0167-6296(93)90004-x. [DOI] [PubMed] [Google Scholar]
- 23.Subramanian SV, Subramanyam MA, Selvaraj S, Kawachi I. Are self-reports of health and morbidities in developing countries misleading? Evidence from India. Soc Sci Med. 2009;68:260–265. doi: 10.1016/j.socscimed.2008.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.van Doorslaer E, Wagstaff A, van der Burg H, Christiansen T, De Graeve D, Duchesne I, Gerdtham UG, Gerfin M, Geurts J, Gross L, et al. Equity in the delivery of health care in Europe and the US. J Health Econ. 2000;19:553–583. doi: 10.1016/s0167-6296(00)00050-3. [DOI] [PubMed] [Google Scholar]
- 25.Wagstaff A, Paci P, van Doorslaer E. On the measurement of inequalities in health. Soc Sci Med. 1991;33:545–557. doi: 10.1016/0277-9536(91)90212-u. [DOI] [PubMed] [Google Scholar]
- 26.Shin H, Kim J. Differences in income-related inequality and horizontal inequity in ambulatory care use between rural and non-rural areas: using the 1998-2001 US National Health Interview Survey data. Int J Equity Health. 2010;9:17. doi: 10.1186/1475-9276-9-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Macinko J, Lima-Costa MF. Horizontal equity in health care utilization in Brazil, 1998-2008. Int J Equity Health. 2012;11:33. doi: 10.1186/1475-9276-11-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.van Doorslaer E, Koolman X, Jones AM. Explaining income-related inequalities in doctor utilisation in Europe. Health Econ. 2004;13:629–647. doi: 10.1002/hec.919. [DOI] [PubMed] [Google Scholar]
- 29.Gravelle H. Measuring income related inequality in health: standardisation and the partial concentration index. Health Econ. 2003;12:803–819. doi: 10.1002/hec.813. [DOI] [PubMed] [Google Scholar]
- 30.Balarajan Y, Selvaraj S, Subramanian SV. Health care and equity in India. Lancet. 2011;377:505–515. doi: 10.1016/S0140-6736(10)61894-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kawachi I, Subramanian SV, Almeida-Filho N. A glossary for health inequalities. J Epidemiol Community Health. 2002;56:647–652. doi: 10.1136/jech.56.9.647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Whitehead M. The concepts and principles of equity and health, document EUR/ICP/RPD/414. Copenhagen: WHO Regional Office for Europe; [Google Scholar]
- 33.Lu JF, Leung GM, Kwon S, Tin KY, Van Doorslaer E, O'Donnell O. Horizontal equity in health care utilization evidence from three high-income Asian economies. Soc Sci Med. 2007;64:199–212. doi: 10.1016/j.socscimed.2006.08.033. [DOI] [PubMed] [Google Scholar]
- 34.Chen B, Mahal A. Measuring the health of the Indian elderly: evidence from National Sample Survey data. Popul Health Metr. 2010;8:30. doi: 10.1186/1478-7954-8-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Maurer J. Assessing horizontal equity in medication treatment among elderly Mexicans: which socioeconomic determinants matter most? Health Econ. 2008;17:1153–1169. doi: 10.1002/hec.1313. [DOI] [PubMed] [Google Scholar]
- 36.Singh J. Elderly and lonely. Down to Earth 2014. Thursday 15 May 2014. [accessed on 15 June 2015]. Available at http://www.downtoearth.org.in/coverage/elderly-lonely-44173.
- 37.Joe W. Distressed financing of household out-of-pocket health care payments in India: incidence and correlates. Health Policy Plan. 2015;30:728–741. doi: 10.1093/heapol/czu050. [DOI] [PubMed] [Google Scholar]
- 38.Hoffer CR, Schuler EA. Measurement of health needs and health care. Am Sociol Rev. 1948;13:719–724. [Google Scholar]