Abstract
Objectives
Healthcare is now routinely delivered by telecommunications-based services in all developed countries and an increasing number of developing countries. Telemedicine is used in many clinical specialities and across numerous healthcare settings, which range from mobile patient-centric applications to complex interactions amongst clinicians in tertiary referral hospital settings. This paper discusses some recent areas of significant development and progress in the field with the purpose of identifying strong trends in both research and practice activities.
Methods
To establish the breadth of new ideas and directions in the field, a review of literature was made by searching PubMed for recent publications including terms (telemedicine OR telehealth) AND (challenge OR direction OR innovation OR new OR novel OR trend), for all searchable categories. 3,433 publications were identified that have appeared since January 1, 2005 (2,172 of these since January 1, 2010), based on a search conducted on June 1, 2015.
Results
The current interest areas in these papers span both synchronous telemedicine, including intensive care, emergency medicine, and mental health, and asynchronous telemedicine, including wound and burns care, dermatology and ophthalmology.
Conclusions
It is concluded that two major drivers of contemporary tele medicine development are a high volume demand for a particular clinical service, and/or a high criticality of need for clinical exper tise to deliver the service. These areas offer promise for further study and enhancement of applicable telemedicine methods and have the potential for large-scale deployments internationally, which would contribute significantly to the advancement of healthcare.
Keywords: Telemedicine, Remote Consultation, Telecommunications, Delivery of Health Care
I. Introduction
This paper discusses some recent areas of significant development and progress in the field of telemedicine, with the purpose of identifying strong trends in both research and practice activities. These areas offer promise for further study and enhancement of applicable telemedicine methods and have the potential for large-scale deployments internationally, which would contribute significantly to the advancement of healthcare. We focus on telemedicine being "the use of telecommunications to diagnose and treat disease and ill-health" due to its specific target of medical applications, rather than the broader field of telehealth, which includes "surveillance, health promotion and public health functions" (http://www.who.int/trade/glossary/story021/en/). Nevertheless, we will first make some general comments about telehealth to provide an overall view of the healthcare systems setting in which to place the reviewed work which follows.
The wide-scale adoption of telehealth dates from the 1990s, but its development in the early stage was constrained by the limited telecommunications infrastructure and the high cost of peripheral devices allowing user access. The twenty-first century has seen an explosion in the availability of these aspects, and telehealth is taking advantage of this situation. Some elements of healthcare are now routinely delivered by telecommunications-based services in all developed countries and an increasing number of developing countries. Telemedicine is used in many clinical specialities and across numerous healthcare settings, which range from mobile patient-centric applications to complex interactions amongst clinicians in tertiary referral hospital settings. A 2009 survey conducted by the World Health Organization (WHO) [1] focused on four specialities, and found that teleradiology was the most common application, practised in 62% of WHO member states which responded to the survey. Telehealth adoption in Europe, the Americas, and South-East Asia was highest, while Africa and the Eastern Mediterranean had the lowest uptake.
Several classification schemes, or taxonomies, have been proposed to describe the context in which telehealth applications are found [2,3]. These generally include at least the three broad characterisations of the relevant clinical speciality concerned, the connectivity technology being used, and the care model being supported. The range of clinical applications has steadily expanded to include more complex and demanding specialities, such as intensive care or emergency medicine. From the technology point of view, the exponential expansion of telecommunications infrastructure is helping to drive new telehealth technologies, especially as broadband becomes ubiquitous. New care models are sometimes a by-product of these technologies, and concepts such as patient centricity and networks of caregivers are emerging as healthcare trends driven at least in part by this technological explosion [4].
A recent report [5] suggested that the global implementation of telehealth, as measured by either number of patients or revenue from services and technology sales, will increase tenfold between 2012 and 2018. This growth is driven largely by the rapid proliferation of mobile and home-based devices, which in turn is driven by the need for the cost-effective management of chronic and aging-related disease. Previous reviews that considered these new areas of telehealth, including the major topic of home monitoring and wearable devices [6], have identified some strong emerging trends in these technologies that will help to drive this continued growth. It is therefore appropriate to examine here the complementary aspects of more traditional telemedicine areas, i.e., telehealth-based activities deployed in mainstream medical settings, to establish a comparable set of trends. For the remainder of this paper, we will adopt the term telemedicine in our discussion to indicate that we are concerned with this particular subset of telehealth.
II. Methods
1. Scope of Telemedicine
A distinction is made widely in telemedicine literature between systems on the basis of the immediacy of the interaction (or response) aspects in the telemedicine service. Synchronous or real-time systems support immediate interaction, or at least response within a timeframe that all participating parties would find an acceptable period for them to wait (typically not more than a few minutes). The major advantage of a synchronous approach is the efficiencies gained by having the opportunity to refine details pertinent to the care episode during the session, by seeking additional information or data, and in many cases providing a clinical decision or advice within the session. The typical video-consultation between a doctor and patient is an example of a synchronous model. Asynchronous or store-and-forward systems decouple the components of the interaction so that they can occur at different times (not usually defined ab initio) at the convenience of the participating parties. This model still allows for multiple component interactions to occur, but the effect of the time separation may add overhead of required refreshing of the episode context during this process. An efficiency gain may nevertheless be obtained in asynchronous services when the telemedicine task does not require to-and-from interactions, and especially when it does not rely on direct interaction with the patient throughout (e.g., telepathology or teleradiology).
The constraints imposed by limited bandwidth availability which prompted the development of asynchronous services have now largely fallen away, so there has been a migration of some of these services to synchronous (or near-synchronous). Where patient interaction with a clinician is necessary, a previous tendency was to prefer synchronous telemedicine, which brings with it an imperative for scheduling or at least recruiting the participants in the same timeslot. In settings where the caregiver is non-clinical (e.g., community or family member), or when routine oversight is applied (e.g., on daily or weekly basis), this requirement can be relaxed to allow surveillance activities to be performed independently in time from patient-carer encounters.
2. Literature Search
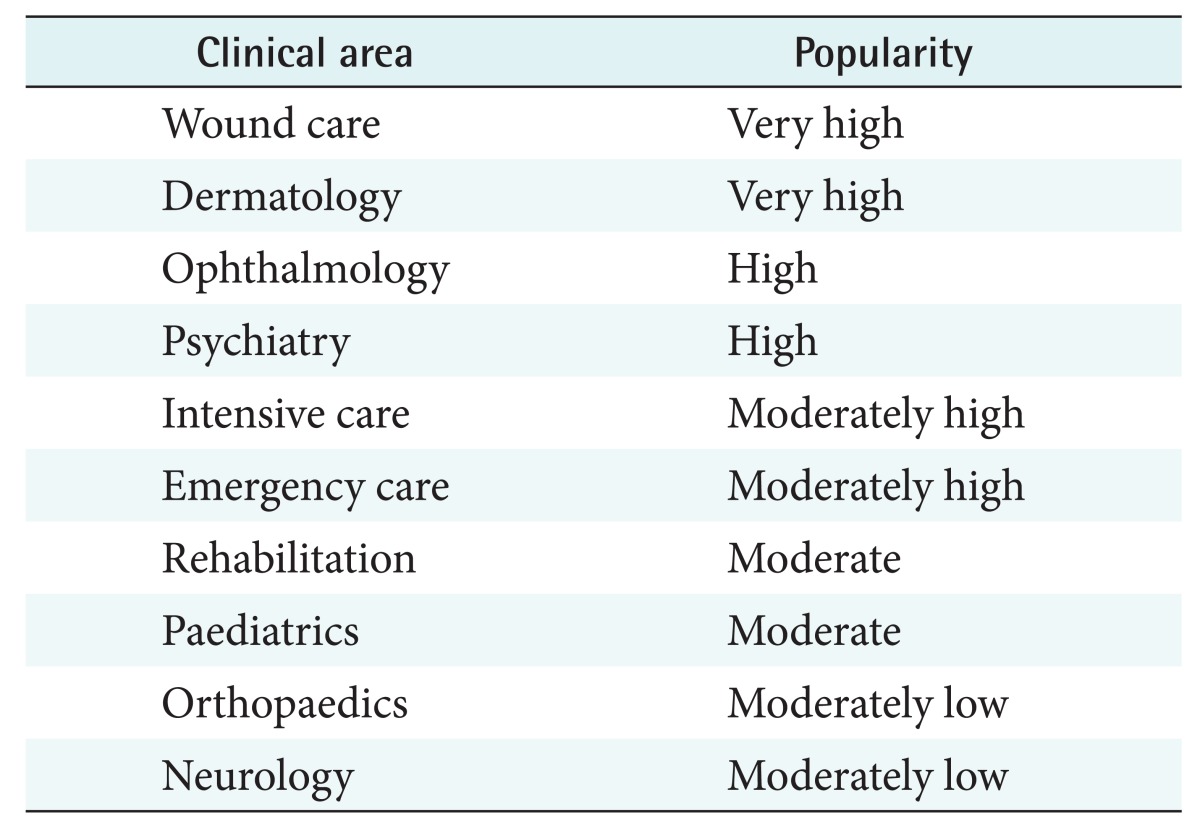
To establish the breadth of new ideas and directions in the realm of telemedicine, a review of literature was made by searching PubMed for recent publications including terms (telemedicine OR telehealth) AND (challenge OR direction OR innovation OR new OR novel OR trend), for all searchable categories. 3,433 publications were identified that have appeared since January 1, 2005 (2,172 of these since January 1, 2010), based on a search conducted on June 1, 2015. A simple keyword analysis of those deemed most relevant to telemedicine showed that numerous clinical areas were addressed, but far fewer technologies. Table 1 summarizes the main clinical areas covered, ranked by decreasing popularity in terms of the number of publications returned by the search.
Table 1. Clinical areas for recent telemedicine innovation.
Because of the broad range of telemedicine applications, a comprehensive review of the entire field is beyond the scope of this paper. Instead we will highlight a few important applications, based on the literature search results described above, that illustrate the current best practice and further development directions. As mentioned earlier, the extremely rapid growth in home and mobile-based applications will not be further discussed here. We also have not considered applications that are peripheral to mainstream medicine, such as educational or administrative services. For convenience, we have grouped our selected applications into the areas of synchronous and asynchronous telemedicine.
III. Results
1. Synchronous Telemedicine
Early telemedicine developments were popularised around the 'teleconsultation' model of delivering healthcare despite a physically separated clinician and patient. This practice has become widespread, and the associated behavioural and technical issues have been well documented [7]. Economic analyses have shown that cost effectiveness of synchronous telemedicine vary widely according to the delivery setting [8]. Contemporary directions in synchronous telemedicine are now addressing less obvious and less simplistic areas, where high impact clinical benefits can be obtained at the expense of more complex interactivity and a more sophisticated technical environment. The three examples given below offer different perspectives on this observation.
1) Intensive care
Telemedicine and medical informatics have, to a large extent, evolved independently of one another, with telemedicine having a focus on synchronous activity, while informatics has a focus on patient data. Although convergence of these disciplines has been seen as inevitable, few telemedicine applications reflect the rich data space increasingly associated with each patient.
One telemedicine application that exemplifies the combination of time-critical interaction with substantial data is intensive care. While intensive care units exist in most hospitals, there is a worldwide shortage of intensive care specialists (intensivists). For example, in the United States, it is estimated [9] that there are approximately 4,000 intensivists to staff the 4,000 adult intensive care units (ICUs) in the nation. Smaller ICUs must consequently operate without round-the-clock intensivist support, below critical mass in either patient load or staffing numbers. Movement of patients to larger facilities is resource-intensive and highly disruptive to both patients and their families.
Where some local intensivist support is available, this can be supplemented by video consultation between the smaller ICU and larger units located in major hospitals. This provided the impetus for the ECHONET project, conducted by Australia's Commonwealth Scientific and Industrial Research Organisation between two centres in Tasmania [10]. Portable telemedicine units were deployed in one city-based ICU and one partially-staffed ICU in a rural centre. As well as bedside diagnostic procedures, such as live echocardiography, the system supported a number of interactions across the two ICUs, ranging from ward rounds to decision support for patients in the rural hospital. High levels of satisfaction were recorded for the ability of the system to integrate a number of activities closely across the two geographically-separated sites. Other benefits included enhanced training opportunities and reduced stress for staff in the rural ICU.
An increasingly common scenario for ICU telemedicine is the effective outsourcing of all specialist intensivist activities to a major centre linked by telemedicine to client ICUs. Medical staff members in the peripheral ICUs are qualified to care for patients and perform hands-on procedures, but the patients are effectively managed by intensivists located in the control centre. This model is exemplified by the eICU, currently marketed by Philips. Intensivists may inspect the vital signs (including historical records) of any ICU patients and visually examine patients by cameras, which are remotely controlled by the specialist and are sometimes incorporated in completely robotically-controlled mobile units. The system can also be programmed to generate an alarm when a particular adverse data combination is detected.
Such systems are now deployed widely in the United States and are considered a highly effective way to deliver such specialist services. A recent review [11] showed that among 25 studies, most showed some reduction in mortality following the introduction of the eICU, although the actual reduction exhibited a high variation across different projects. Many implementations demonstrated reduction in stress and 'burnout' experienced by staff members who have to care for ICU patients without peer support.
A rich and structured data stream provides opportunities for telemedicine systems to incorporate intelligent decision support. This is especially useful in environments in which large amounts of data are created continuously, and decisions need to be made in a time-critical setting. If telemedicine systems continue to converge with information management systems, the incorporation of such 'smarts' may become increasingly common features of such systems.
2) Emergency medicine
An area of recent expansion in the use of telemedicine is emergency medicine. A typical scenario is that a patient is admitted to the emergency department of a rural hospital staffed by generalist physicians who may require specialist advice on the management of the patient. This is one of the most challenging situations for telemedicine, due mainly to the time-criticality of the decision-making (achieving treatment within the 'golden hour' since trauma) and the complete impossibility of scheduling such consultations. The information space is dense, and new information may be generated during the consultation. Telemedicine consultations need to be undertaken at the point of care in busy emergency departments by staff who are working under stressful conditions with a high level of patient focus. Information presented to the specialist can include multiscale views of the room and patient, vital signs, medical images, and interviews with all participants, including the patient and his/her family.
One solution to this problem was the virtual critical care unit, developed jointly by Australia's Commonwealth Scientific and Industrial Research Organisation and Sydney West Area Health Service in the early 2000s [12,13]. Using a user-centred design approach, a multi-camera broadband system linked a rural emergency department to a major tertiary referral hospital. The system was able to demonstrate improved decision-making for patient-management, especially for those patients in the 'middle' levels of trauma severity, where local management could be enhanced through specialist participation [14]. A similar project in Arizona, USA connected a level 1 trauma centre in Tucson to five rural hospitals with minimal specialist support [15]. Although the sample size was too small for detailed analysis, the authors reported considerable savings in the cost of transporting patients.
The widespread availability of wireless broadband has made it possible to connect ambulances directly to specialist centres, moving the timing of triage to before presentation in an emergency department, although the requirement for widespread wireless coverage effectively limits such applications to urban areas. A recent study of 838 ambulance-transported patients in Korea (of whom 188 were subject to in-ambulance monitoring) demonstrated that the choice of the treating hospital could be improved if physicians were made aware of continuous monitoring of vital signs [16].
A success story within emergency telemedicine has been the use of telemedicine in acute stroke care, sometimes referred to as 'telestroke'. Thrombolytic drugs, if delivered within a strict post-stroke time window, have demonstrated a high rate of reversal of many of the long-term effects of stroke. However, there is risk to the patient if these drugs are administered when stroke is not indicated, and the assessment involves CT scans, blood tests, and an assessment of the patient's neurological function. The neurological specialists qualified to make the decision on drug administration are sparsely distributed outside major cities in most countries with advanced healthcare systems, but recently their expertise has been increasingly exploited using telemedicine.
This application is highly time-critical (the delay limit for drug administration as about four hours from stroke onset) and requires the transmission of a variety of information types (including CT scans) as well as an interactive examination of the patient. There have been several large-scale demonstrations of the efficacy of this technique. As an example, in the TeleMedical Project for Integrative Stroke Care (TEMPiS) in Bavaria, Germany, between February 2003 and December 2012, 54,804 strokes and transient ischemic attacks were treated in 15 regional hospitals, and 31,864 teleconsultations were performed. Intravenous thrombolysis was applied to 3,331 of these stroke cases. The median onset-to-treatment time was reduced from 150 to 120 minutes, and door-to-needle time was reduced from 80 to 40 minutes [17].
3) Mental health
As telemedicine incorporates an increasing diversity of technologies, a correspondingly wider range of clinical scenarios can be supported. One clinical speciality that illustrates this, possibly more than any other, is mental health, which in the context of telemedicine is often referred to as telepsychiatry or telemental health.
Mental health is an increasing challenge for health systems worldwide. The World Health Organization [18] has estimated that 450 million people are affected by mental or behavioural disorders worldwide, and five of the ten leading causes of disability and premature death are associated with psychiatric conditions. The potentially fatal effects of depression and other mental conditions can be prevented or greatly attenuated with timely intervention, but this is difficult to implement, due to such factors as limitations in access to providers [19]. Most recently, the time-critical nature of some telemental health interventions has prompted innovation in this long-established field.
Generally, consultation in mental health takes the form of an interview between a practitioner and a patient, but conducting such consultations can sometimes be difficult without telemedicine technologies. Specialists and patients are often separated by large distances, there can be a stigma attached to attending facilities, and delayed intervention can lead to deterioration in a patient's condition. Many such consultations need to take place in locations with limited access to appropriate clinical specialists, such as prisons and emergency departments of hospitals. There is a stigma attached to seeking treatment for mental conditions, which creates further barriers between patients and those who can offer treatment.
Telemental health services need to be tailored for an extremely diverse group of patients, with corresponding subspecialities among providers. Specific patient categories including paediatric, adolescent, and geriatric groups, often require different clinical approaches and, in the telemedicine setting, different technologies. For example, while the basic mental health consultation is an interview between clinician and patient, the ease of access provided by telemedicine can allow a single 50-minute consultation to be replaced by two or three shorter interviews [20]. Scheduling difficulties for both patient and clinician can be eased through the use of asynchronous consultations [19]. Standard interviews can be conducted through semi-specialist clinicians and reviewed by the specialist before evidence-based treatment is recommended. The record of the interview becomes part of the patient's record and facilitates reviews of the patients' progress over time.
The need to supply timely and sometimes frequent contact between clinician and patient is met by implementing home-based telemental health (HBTMH) using the improved communications infrastructure present in many homes. A recent review paper [21] pointed out a number of benefits of HBTMH, including better adherence to appointments and medication, overcoming social isolation, access to contextual information such as the patient's home situation, improved patient and practitioner safety, and removal of the fears of stigma attached to attending a mental health clinic. There appears to be little or no reduction in effectiveness compared with face-to-face consultations.
The relative immediacy of HBTMH is further enhanced through the use of mobile devices. The ability to interact with a patient at virtually any time or place makes mobile devices especially useful in delivering mental health care. Furthermore, such devices can support a high degree of self-management, and are especially well received by such groups as adolescents. A contemporary review [22] lists a number of activities in mental illness management facilitated through mHealth. Pre-treatment applications include educating patients before treatment and reaching groups who are reluctant to access in-person services. During treatment, patients can receive location-dependent information and advice, as well as instructions and distractions for dealing with minor crises. In addition, such devices enable checking of adherence to 'homework' regimes, symptom self-monitoring, administration of therapy via automated 'apps', and scheduling of interviews at very short notice. Post-therapy, many conditions require ongoing coaching and encouragement, which can be delivered by mobile apps as the patient steps down from the more intensive stage of treatment.
2. Asynchronous Telemedicine
The predominant characteristic of asynchronous telemedicine is a time separation between one phase of the process and another. Whether for reasons of efficiency or to overcome resource constraints, the net effect of this separation is that poor availability of a scarce physical or human resource is overcome by careful management of the capture, storage, and transmission of information to accommodate that situation. In the examples considered here, various technical issues arise, and various organisational solutions are adopted, demonstrating that both of these aspects are still significant factors in need of further attention if such solutions are to be developed.
1) Wound care
Clinical management of wounds makes up a substantial fraction of day care and outpatient clinic activities in the acute sector, and it imposes a burden on home or aged care and outreach nursing activities. The need to inspect the patient's condition approximately daily leads to significant workload and expense, while the benefits of personalizing the treatment of the patient and achieving faster or better recovery can be substantial. Situations in which telemedicine has been reported recently as being used innovatively for wound care include postoperative wound management, trauma and accidental injury patients, burns, diabetes and other degenerative diseases, pressure sores and ulcers, skin and subcutaneous procedures [23,24].
The basic telemedicine approach in such situations has been the acquiring of digital images or video, which are presented either in real time or by store-and-forward to a clinician, who advises on the best treatment given the patient's treatment history and the appearance of the wound. The effectiveness of the approach depends closely on the quality and acquisition characteristics of the imagery. Technical aspects, such as image resolution, focus, and depth-of-field, as well as lighting, position of camera relative to the subject, and colour, are all important to ensure that there is enough information for accurate clinical assessment and judgement. These aspects are seldom systematized sufficiently in clinical situations to allow reliable control of the variability and prediction of outcomes [25,26]. Furthermore, due to the widespread availability of personal communication devices with inbuilt cameras, which allow ad hoc practices to emerge, the development of appropriate guidelines is imperative [27].
An advantage noted in telewoundcare research has been the ease with which additional expert opinion for assessment and treatment can be accessed by patients and carers through simple imaging approaches. This enables timely and informed clinical decisions, which can be important due to the wide range of conditions and severities possible. High levels of agreement (at least 80%) between experts have been reported for this approach in primary care [28] and nursing home [29] settings. More complex telewoundcare management situations, such as pressure ulcers involving multiple carers, have also been shown to be comparable with conventional practice [30].
An area of wound care that has been in recent focus is the care of burns and related trauma situations. A driver for the use of telemedicine in these situations is a decrease in the number of specialist burns units, while in many cases transportation of the patient to a specialist site is undesirable. High levels of agreement between experts have been reported [31] for telemedicine, whereas referring physicians tended to make more pessimistic assessments. Studies in UK [32] and USA [33] suggest that routine institutional teleburn treatment management is feasible.
2) Teledermatology
Teledermatology for the assessment of skin conditions is a challenging area in telemedicine due to the highly varied and specific nature of many types of conditions, distinguished by very subtle appearance features which demand careful visual inspection and experienced professional judgements. At the same time, the comparative scarcity of dermatologists makes it a natural candidate for an asynchronous telemedicine service; indeed this demand has also prompted the emergence of synchronous services in some settings where a real-time decision would be advantageous. A recent study of teledermatology programs in the United States observed that sustainability of services in the study period since 2003 had depended strongly on volume of case throughput [34]. In Australia, a national online consultation and educational service known as TeleDerm has operated for the past decade, providing asynchronous case advice with a 24-hour turn-around [35].
Adoption of teledermatology (including teledermatoscopy) has been widespread compared with other areas in telemedicine, driven by the availability of numerous commercial products to acquire and analyze imagery [36], by the user satisfaction and positive attitude of dermatologists towards its uptake [37], and by the substantial evidence of its clinical effectiveness [38,39,40]. It can also offer improvements in healthcare in settings with a substantial remote area population like Australia [41], and in developing world situations where population size limits access to health services, like India [42]. A strong body of literature exists describing numerous aspects of teledermatology [43].
One of the most active areas for teledermatology development and deployment has been in skin cancer screening, diagnosis, and treatment management [44]. It is accepted by many authors that the performance of teledermatology in this area is below that of direct clinical inspection, with typical reported accuracy of diagnosis rates of around 80%, e.g., [45]. Recognition of potential melanoma and carcinoma from transmitted images was shown to have high sensitivity (98%) but low specificity (43%) [46], resulting in excessive referrals. A subsequent study reported that teledermatology was overall inferior to clinical dermatology in diagnostic accuracy [47]. It remains challenging to improve on this performance and so reduce the extent of unnecessary follow-up clinical consultations.
Despite its reliance on the quality of image acquisition technology, teledermatology is deemed to be a good candidate for mobile services based on the use of tablet computers and smartphones, and several recent papers have discussed this aspect especially in the context of skin cancer screening. The appeal of the simplicity and universality of this solution [48] and its suitability for transfer of dermoscope imagery [49] make it appealing, and it has been claimed that accuracy of 81% is achievable [50], consistent with conventional teledermatology. Cautionary commentary has also appeared suggesting that results obtained with publicly available smartphone dermatology applications may be highly variable and unreliable [51]. This suggests that further study is warranted in this new technology arena, and perhaps certification or accreditation processes should be instituted for mobile software products that have clinical usage.
3) Teleophthalmology
Diseases and other conditions affecting the eye have a substantial impact on the quality of life of the individuals affected, especially as many left undiagnosed and untreated can experience deterioration in eyesight and even blindness. Especially in remote areas and developing countries, the loss of productivity and opportunities due to diminished vision could be avoided by the provision of regular, frequent eye care. While teleophthalmology generally requires specialised imaging equipment, it is non-invasive and not reliant on direct clinical expertise in the image acquisition process, which makes it easier to achieve cost-effectiveness in large-scale population-wide circumstances.
A major application area for teleophthalmology is diabetic retinopathy, often in a setting of repeated screening of diabetes patients for signs of deterioration. Its clinical efficacy has been established [52] and more recently, analysis of its economic viability has been undertaken [53,54]. The development of an open-source system, EyePACS [55], supporting diabetic retinopathy as well as other ocular disorders on a variety of platforms, has encouraged widespread adoption of the telemedicine approach [56].
Other promising applications for teleophthalmology involve the support of public health screening programmes for ocular health. Fundamental acuity testing has been seen as a suitable candidate for remote delivery using computer-based tools [57], and it has been shown to deliver performance comparable to that of human testers [58]. Other applications reported to be suitable for telemedicine include blurred vision [59] and degenerative eye diseases [60]. Recent interest has been shown in using smartphones in place of specialised equipment where feasible [61].
IV. Conclusion
In 2015, we are seeing telemedicine evolve from a technology-driven novelty to an essential component of healthcare delivery in a number of specialities and fields. This is increasingly based on the utility of the applications rather than response to a technology push, and there is increasing demand for system-wide implementations rather than further unsustainable and unscalable pilots. In this paper, we have reviewed a number of clinical application areas, and two trends which are immediately apparent are implementations which demonstrate:
1) High volume, in which it is increasingly difficult to physically co-locate the patient and their associated data on the one hand, and the expertise to deal with that data on the other. Such co-location can occur in time as well as in space, which will continue to create demand for asynchronous telemedicine, as discussed in Section III of this paper. Increasing pressure on health systems to deliver high-quality healthcare within strict financial constraints will drive this trend to leverage healthcare resources more effectively.
2) High criticality applications, where specialist expertise needs to be made available at the point of care within a very strict time frame. This is exemplified in emergency telemedicine, but it is also true of some mobile and home-based applications, such as telemental health, where patient-initiated contact with a health professional can avert potentially disastrous deterioration of the patient's condition.
In most developed countries, the increasing availability of reliable broadband communications and user interface devices has effectively removed the cost and availability of this technology as a barrier to the uptake of telemedicine. One consequence has been the ability to provide telemedicine on a wide variety of delivery devices. For example, specialist consultation services may be delivered through high definition videoconferencing or through mobile phones. Increased use of wireless communication is permitting telemedicine to be used more easily at the point of care rather than in a videoconferencing setting. Telemedicine interactions may be performed at a patient's bedside in an emergency department, in an ambulance, or even at the location of a trauma. Such applications are especially valuable when patients cannot be moved easily. It also makes telemedicine more likely to be used in time-critical applications, such as the treatment of stroke.
Telemedicine is now working in a richer information space than in the 1990s. Telemedicine systems are often coupled with peripheral devices, such as ophthalmoscopes, and even camera-based systems are making use of multiple views, some of which can be high definition. A range of multidimensional medical images (such as 3D CT or real-time ultrasound) might also need to be transmitted as part of the telemedicine consultation. Of course, the data space associated with a patient extends beyond the information transmitted as part of the telemedicine consultation. Health informatics has evolved largely independently of telemedicine, but telemedicine systems are already evolving to work in an environment of complex digital information. This is especially true of intensive care applications, where current and previous vital signs records form part of the information space for each patient. The distinction between the telemedicine consultation and the patient record is already blurred in telepsychiatry, but the convergence of telemedicine and medical informatics is likely to make this distinction even less relevant in the future.
As alluded to earlier in this paper, telemedicine is likely to evolve with developments associated with three 'dimensions' of the telemedicine space: technology, clinical applications, and care models. Telemedicine has tended to follow fixed models of care, based either on replicating conventional care delivery methods (e.g., videoconferencing replacing face to face live consultations) or introducing new methods (e.g., home-based patient health status monitoring). One recent trend has been the evolution of hybrid models of care derived by changing some aspects of the telemedicine solution to introduce a significant variation. Examples include store-and-forward teleconsultations, and telerehabilitation therapy in the home. Another trend has been the adoption of telemedicine on a greater scale by certain clinical disciplines, such as critical and emergency care, or chronic disease management. Often, this recent adoption has been due to the development of a new technological solution (e.g., storage and rapid backend processing of large datasets) that makes this practical.
More broadly, telemedicine has the potential to both catalyze and benefit from the introduction of new care models. Many of the barriers to telemedicine expansion lie in this domain rather than technology, which has, if anything, outpaced telemedicine applications [62]. Discussions of future healthcare models often focus on the concept of 'patient centricity', and the expansion of telehealth into self-management and home and mobile-based applications will certainly form part of this trend. As healthcare models evolve, telemedicine is more likely to fulfil a role in transforming healthcare by increasing the capacity for clinical professionals to interact with patients and carers.
Footnotes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
References
- 1.World Health Organisation. Telemedicine: opportunities and developments in member states. Geneva, Switzerland: World Health Organisation; 2010. [Google Scholar]
- 2.Tulu B, Chatterjee S, Maheshwari M. Telemedicine taxonomy: a classification tool. Telemed J E Health. 2007;13(3):349–358. doi: 10.1089/tmj.2006.0055. [DOI] [PubMed] [Google Scholar]
- 3.Bashshur R, Shannon G, Krupinski E, Grigsby J. The taxonomy of telemedicine. Telemed J E Health. 2011;17(6):484–494. doi: 10.1089/tmj.2011.0103. [DOI] [PubMed] [Google Scholar]
- 4.Li J, Wilson LS. Telehealth trends and the challenge for infrastructure. Telemed J E Health. 2013;19(10):772–779. doi: 10.1089/tmj.2012.0324. [DOI] [PubMed] [Google Scholar]
- 5.Caswell W. Global telehealth market to expand 10x by 2018 [Internet] [place unknown]: Modern Health Talk; 2014. [cited at 2015 Mar 20]. Available from: http://www.mhealthtalk.com/global-telehealth-market-to-expand-10x-by-2018/#more-7937. [Google Scholar]
- 6.Marschollek M, Gietzelt M, Schulze M, Kohlmann M, Song B, Wolf KH. Wearable sensors in healthcare and sensor-enhanced health information systems: all our tomorrows? Healthc Inform Res. 2012;18(2):97–104. doi: 10.4258/hir.2012.18.2.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fatehi F, Armfield NR, Dimitrijevic M, Gray LC. Technical aspects of clinical videoconferencing: a large scale review of the literature. J Telemed Telecare. 2015;21(3):160–166. doi: 10.1177/1357633X15571999. [DOI] [PubMed] [Google Scholar]
- 8.Wade VA, Karnon J, Elshaug AG, Hiller JE. A systematic review of economic analyses of telehealth services using real time video communication. BMC Health Serv Res. 2010;10:233. doi: 10.1186/1472-6963-10-233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ahn Y, Jasmer RM, Shaughnessy T. Perspectives on the electronic ICU. ICU Dir. 2012;3(2):64–69. [Google Scholar]
- 10.Hansen SK, Wilson LS, Roberson T. Applying an integrated approach to the design, implementation and evaluation of a telemedicine system. J Int Soc Telemed eHealth. 2013;1(1):19–29. [Google Scholar]
- 11.Kumar S, Merchant S, Reynolds R. Tele-ICU: efficacy and cost-effectiveness of remotely managing critical care. Perspect Health Inf Manag. 2013;10:1f. [PMC free article] [PubMed] [Google Scholar]
- 12.Li J, Wilson LS, Qiao RY, Percival T, Krumm-Heller A, Stapleton S, et al. Development of a broadband telehealth system for critical care: process and lessons learned. Telemed J E Health. 2006;12(5):552–560. doi: 10.1089/tmj.2006.12.552. [DOI] [PubMed] [Google Scholar]
- 13.Wilson LS, Stevenson DR, Cregan P. Telehealth on advanced networks. Telemed J E Health. 2010;16(1):69–79. doi: 10.1089/tmj.2009.0079. [DOI] [PubMed] [Google Scholar]
- 14.Westbrook JI, Coiera EW, Brear M, Stapleton S, Rob MI, Murphy M, et al. Impact of an ultrabroadband emergency department telemedicine system on the care of acutely ill patients and clinicians' work. Med J Aust. 2008;188(12):704–708. doi: 10.5694/j.1326-5377.2008.tb01850.x. [DOI] [PubMed] [Google Scholar]
- 15.Latifi R, Hadeed GJ, Rhee P, O'Keeffe T, Friese RS, Wynne JL, et al. Initial experiences and outcomes of telepresence in the management of trauma and emergency surgical patients. Am J Surg. 2009;198(6):905–910. doi: 10.1016/j.amjsurg.2009.08.011. [DOI] [PubMed] [Google Scholar]
- 16.Kim YK, Kim KY, Lee KH, Kim SC, Kim H, Hwang SO, et al. Clinical outcomes on real-time telemetry system in developing emergency medical service system. Telemed J E Health. 2011;17(4):247–253. doi: 10.1089/tmj.2010.0152. [DOI] [PubMed] [Google Scholar]
- 17.Muller-Barna P, Hubert GJ, Boy S, Bogdahn U, Wiedmann S, Heuschmann PU, et al. TeleStroke units serving as a model of care in rural areas: 10-year experience of the TeleMedical project for integrative stroke care. Stroke. 2014;45(9):2739–2744. doi: 10.1161/STROKEAHA.114.006141. [DOI] [PubMed] [Google Scholar]
- 18.World Health Organization. Prevention of mental disorders: effective interventions and policy options [Internet] Geneva, Switzerland: World Health Organization; 2004. [cited at 2015 Apr 3]. Available from: http://www.who.int/mental_health/evidence/en/prevention_of_mental_disorders_sr.pdf. [Google Scholar]
- 19.Yellowlees P, Odor A, Patrice K, Parish MB, Nafiz N, Iosif AM, et al. Disruptive innovation: the future of healthcare? Telemed J E Health. 2011;17(3):231–234. doi: 10.1089/tmj.2010.0130. [DOI] [PubMed] [Google Scholar]
- 20.Mohr DC. Telemental health: reflections on how to move the field forward. Clin Psychol Sci Pract. 2009;16(3):343–347. [Google Scholar]
- 21.Pruitt LD, Luxton DD, Shore P. Additional clinical benefits of home-based telemental health treatments. Prof Psychol Res Pr. 2014;45(5):340–346. [Google Scholar]
- 22.Price M, Yuen EK, Goetter EM, Herbert JD, Forman EM, Acierno R, et al. mHealth: a mechanism to deliver more accessible, more effective mental health care. Clin Psychol Psychother. 2014;21(5):427–436. doi: 10.1002/cpp.1855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gray LC, Armfield NR, Smith AC. Telemedicine for wound care: current practice and future potential. Wound Pract Res. 2010;18(4):158–163. [Google Scholar]
- 24.Chanussot-Deprez C, Contreras-Ruiz J. Telemedicine in wound care: a review. Adv Skin Wound Care. 2013;26(2):78–82. doi: 10.1097/01.ASW.0000426717.59326.5f. [DOI] [PubMed] [Google Scholar]
- 25.Hasselberg M, Beer N, Blom L, Wallis LA, Laflamme L. Image-based medical expert teleconsultation in acute care of injuries: a systematic review of effects on information accuracy, diagnostic validity, clinical outcome, and user satisfaction. PLoS One. 2014;9(6):e98539. doi: 10.1371/journal.pone.0098539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Santamaria N, Kapp S. TeleWound care: providing remote wound assessment and treatment in the home care setting: current status and future directions. Smart Homecare Technol TeleHealth. 2013;1:35–41. [Google Scholar]
- 27.Canadian Agency for Drugs and Technologies in Health. Personal wireless device use for wound care consultation: a review of safety, clinical benefits and guidelines. Ottawa, Canada: Canadian Agency for Drugs and Technologies in Health; 2014. [PubMed] [Google Scholar]
- 28.Chen CH, Young TH, Huang CH, Chang HH, Chen CL, Chien HF, et al. Patient-centered wound teleconsultation for cutaneous wounds: a feasibility study. Ann Plast Surg. 2014;72(2):220–224. doi: 10.1097/SAP.0000000000000031. [DOI] [PubMed] [Google Scholar]
- 29.Vowden K, Vowden P. A pilot study on the potential of remote support to enhance wound care for nursinghome patients. J Wound Care. 2013;22(9):481–488. doi: 10.12968/jowc.2013.22.9.481. [DOI] [PubMed] [Google Scholar]
- 30.Stern A, Mitsakakis N, Paulden M, Alibhai S, Wong J, Tomlinson G, et al. Pressure ulcer multidisciplinary teams via telemedicine: a pragmatic cluster randomized stepped wedge trial in long term care. BMC Health Serv Res. 2014;14:83. doi: 10.1186/1472-6963-14-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Saffle JR, Edelman L, Theurer L, Morris SE, Cochran A. Telemedicine evaluation of acute burns is accurate and cost-effective. J Trauma. 2009;67(2):358–365. doi: 10.1097/TA.0b013e3181ae9b02. [DOI] [PubMed] [Google Scholar]
- 32.Wallace DL, Hussain A, Khan N, Wilson YT. A systematic review of the evidence for telemedicine in burn care: with a UK perspective. Burns. 2012;38(4):465–480. doi: 10.1016/j.burns.2011.09.024. [DOI] [PubMed] [Google Scholar]
- 33.Holt B, Faraklas I, Theurer L, Cochran A, Saffle JR. Telemedicine use among burn centers in the United States: a survey. J Burn Care Res. 2012;33(1):157–162. doi: 10.1097/BCR.0b013e31823d0b68. [DOI] [PubMed] [Google Scholar]
- 34.Armstrong AW, Wu J, Kovarik CL, Goldyne ME, Oh DH, McKoy KC, et al. State of teledermatology programs in the United States. J Am Acad Dermatol. 2012;67(5):939–944. doi: 10.1016/j.jaad.2012.02.019. [DOI] [PubMed] [Google Scholar]
- 35.Muir J. Telehealth: the specialist perspective. Aust Fam Physician. 2014;43(12):828–830. [PubMed] [Google Scholar]
- 36.Massone C, Wurm EM, Hofmann-Wellenhof R, Soyer HP. Teledermatology: an update. Semin Cutan Med Surg. 2008;27(1):101–105. doi: 10.1016/j.sder.2007.12.002. [DOI] [PubMed] [Google Scholar]
- 37.Whited JD. Teledermatology research review. Int J Dermatol. 2006;45(3):220–229. doi: 10.1111/j.1365-4632.2004.02427.x. [DOI] [PubMed] [Google Scholar]
- 38.Levin YS, Warshaw EM. Teledermatology: a review of reliability and accuracy of diagnosis and management. Dermatol Clin. 2009;27(2):163–176. doi: 10.1016/j.det.2008.11.012. [DOI] [PubMed] [Google Scholar]
- 39.Vrucinic Z, Jankovic A, Miladinovic M, Gocev D, Bojanic P, Kacarevic R. Evaluation of clinical diagnosis with "store and forward" teledermatology. Acta Med Median. 2010;49(4):23–30. [Google Scholar]
- 40.Warshaw EM, Gravely AA, Nelson DB. Accuracy of teledermatology/teledermoscopy and clinic-based dermatology for specific categories of skin neoplasms. J Am Acad Dermatol. 2010;63(2):348–352. doi: 10.1016/j.jaad.2009.10.037. [DOI] [PubMed] [Google Scholar]
- 41.Muir J, Lucas L. Tele-dermatology in Australia. Stud Health Technol Inform. 2008;131:245–253. [PubMed] [Google Scholar]
- 42.Thomas J, Kumar P. The scope of teledermatology in India. Indian Dermatol Online J. 2013;4(2):82–89. doi: 10.4103/2229-5178.110579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Warshaw EM, Hillman YJ, Greer NL, Hagel EM, Mac-Donald R, Rutks IR, et al. Teledermatology for diagnosis and management of skin conditions: a systematic review. J Am Acad Dermatol. 2011;64(4):759–772. doi: 10.1016/j.jaad.2010.08.026. [DOI] [PubMed] [Google Scholar]
- 44.Mahendran R, Goodfield MJ, Sheehan-Dare RA. An evaluation of the role of a store-and-forward teledermatology system in skin cancer diagnosis and management. Clin Exp Dermatol. 2005;30(3):209–214. doi: 10.1111/j.1365-2230.2005.01735.x. [DOI] [PubMed] [Google Scholar]
- 45.Moreno-Ramirez D, Ferrandiz L, Bernal AP, Duran RC, Martin JJ, Camacho F. Teledermatology as a filtering system in pigmented lesion clinics. J Telemed Telecare. 2005;11(6):298–303. doi: 10.1258/1357633054893364. [DOI] [PubMed] [Google Scholar]
- 46.Bowns IR, Collins K, Walters SJ, McDonagh AJ. Telemedicine in dermatology: a randomised controlled trial. Health Technol Assess. 2006;10(43):iii–iv. ix–xi, 1–39. doi: 10.3310/hta10430. [DOI] [PubMed] [Google Scholar]
- 47.Warshaw EM, Lederle FA, Grill JP, Gravely AA, Bangerter AK, Fortier LA, et al. Accuracy of teledermatology for pigmented neoplasms. J Am Acad Dermatol. 2009;61(5):753–765. doi: 10.1016/j.jaad.2009.04.032. [DOI] [PubMed] [Google Scholar]
- 48.Massone C, Brunasso AM, Campbell TM, Soyer HP. Mobile teledermoscopy: melanoma diagnosis by one click? Semin Cutan Med Surg. 2009;28(3):203–205. doi: 10.1016/j.sder.2009.06.002. [DOI] [PubMed] [Google Scholar]
- 49.Kroemer S, Fruhauf J, Campbell TM, Massone C, Schwantzer G, Soyer HP, et al. Mobile teledermatology for skin tumour screening: diagnostic accuracy of clinical and dermoscopic image tele-evaluation using cellular phones. Br J Dermatol. 2011;164(5):973–979. doi: 10.1111/j.1365-2133.2011.10208.x. [DOI] [PubMed] [Google Scholar]
- 50.Lamel SA, Haldeman KM, Ely H, Kovarik CL, Pak H, Armstrong AW. Application of mobile teledermatology for skin cancer screening. J Am Acad Dermatol. 2012;67(4):576–581. doi: 10.1016/j.jaad.2011.11.957. [DOI] [PubMed] [Google Scholar]
- 51.Wolf JA, Moreau JF, Akilov O, Patton T, English JC, 3rd, Ho J, et al. Diagnostic inaccuracy of smartphone applications for melanoma detection. JAMA Dermatol. 2013;149(4):422–426. doi: 10.1001/jamadermatol.2013.2382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Whited JD. Accuracy and reliability of teleophthalmology for diagnosing diabetic retinopathy and macular edema: a review of the literature. Diabetes Technol Ther. 2006;8(1):102–111. doi: 10.1089/dia.2006.8.102. [DOI] [PubMed] [Google Scholar]
- 53.Jones S, Edwards RT. Diabetic retinopathy screening: a systematic review of the economic evidence. Diabet Med. 2010;27(3):249–256. doi: 10.1111/j.1464-5491.2009.02870.x. [DOI] [PubMed] [Google Scholar]
- 54.Chasan JE, Delaune B, Maa AY, Lynch MG. Effect of a teleretinal screening program on eye care use and resources. JAMA Ophthalmol. 2014;132(9):1045–1051. doi: 10.1001/jamaophthalmol.2014.1051. [DOI] [PubMed] [Google Scholar]
- 55.Cuadros J, Sim I. EyePACS: an open source clinical communication system for eye care. Stud Health Technol Inform. 2004;107(Pt 1):207–211. [PubMed] [Google Scholar]
- 56.Cuadros J, Bresnick G. EyePACS: an adaptable telemedicine system for diabetic retinopathy screening. J Diabetes Sci Technol. 2009;3(3):509–516. doi: 10.1177/193229680900300315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kumar S, Bulsara M, Yogesan K. Automated determination of distance visual acuity: towards teleophthalmology services. Clin Exp Optom. 2008;91(6):545–550. doi: 10.1111/j.1444-0938.2008.00267.x. [DOI] [PubMed] [Google Scholar]
- 58.Srinivasan K, Ramesh SV, Babu N, Sanker N, Ray A, Karuna SM. Efficacy of a remote based computerised visual acuity measurement. Br J Ophthalmol. 2012;96(7):987–990. doi: 10.1136/bjophthalmol-2012-301751. [DOI] [PubMed] [Google Scholar]
- 59.Tan JC, Poh EW, Srinivasan S, Lim TH. A pilot trial of tele-ophthalmology for diagnosis of chronic blurred vision. J Telemed Telecare. 2013;19(2):65–69. doi: 10.1177/1357633x13476233. [DOI] [PubMed] [Google Scholar]
- 60.Maa AY, Evans C, DeLaune WR, Patel PS, Lynch MG. A novel tele-eye protocol for ocular disease detection and access to eye care services. Telemed J E Health. 2014;20(4):318–323. doi: 10.1089/tmj.2013.0185. [DOI] [PubMed] [Google Scholar]
- 61.Zvornicanin E, Zvornicanin J, Hadziefendic B. The use of smart phones in ophthalmology. Acta Inform Med. 2014;22(3):206–209. doi: 10.5455/aim.2014.22.206-209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Jang-Jaccard J, Nepal S, Alem L, Li J. Barriers for delivering telehealth in rural australia: a review based on Australian trials and studies. Telemed J E Health. 2014;20(5):496–504. doi: 10.1089/tmj.2013.0189. [DOI] [PubMed] [Google Scholar]