Abstract
Background
Gastrojejunocolic fistula (GJCF) is a late and severe complication of a stomal ulcer after gastrojejunostomy, which develops as a result of inadequate resection of stomach or incomplete vagotomy. The occurrence of perforation in a GJCF is even more a rare complication because long evolution time or latent period is required for its appearance. Patients with this condition usually present with diarrhea, weight loss, feculent vomiting, under-nutrition and features of peritonitis that require immediate surgical intervention.
Case presentation
We described two cases of gastrojejunocolic fistula in men aged 60 and 40, first cases of gastrojejunocolic fistula seen in our referral hospital and in the whole region following more than a decade after gastrojejunostomy. Both patients initially presented with watery diarrhea, vomiting of fecal materials, poor appetite and weight loss. Upper GI series or barium enema studies allowed a conclusive diagnosis to be made. Both patients underwent one-stage en bloc resection, and their postoperative course and outcome was one cure and one death.
Conclusion
As it is rare phenomenon, high clinical suspicion is very important in the diagnosis of GJCF on patients who manifest with chronic diarrhea, vomiting of fecal matter, abdominal pain and features of malnutrition. Careful preoperative preparation is mandatory before any type of surgical procedure is carried out. Pre-operative nutritional status should be evaluated in patients undergoing corrective surgery. Adequate resection of the stomach after Gastrojejunostomy and complete vagotomy is important to prevention development of GJCF.
Keywords: Gastrojejunocolic fistulas, Gastrojejunostomy, Post-surgical, Northern Ethiopia
Highlights
-
•
High Nasal carriage of Staphylococcus aureus.
-
•
Vancomycin, Gentamicin and Ceftriaxone were 100% effective.
-
•
Isolated bacteria showed high resistance to penicillin and Ampicillin.
-
•
Low MRSA prevalence arte.
-
•
Food handlers should train on personal hygiene.
1. Introduction
Gastrojejunocolic fistula (GJCF) is a rare and late complication of gastrojejunostomy applied for recurrent peptic ulcer disease [1]. It was thought to be induced by a stomal ulcer, due to inadequate gastrectomy or incomplete vagotomy [1], [2]. The symptoms in these situations include upper abdominal pain, weight loss, diarrhea, gastrointestinal bleeding, and fecal vomiting [3]. These patients are cachectic and dehydrated, with labs showing malnutrition. Barium upper gastrointestinal series (UGIS), gastroscopy, and colonoscopy are used for diagnosis [1]. Although the occurrence of GJCF has decreased remarkably as a result of better treatment, the modern management of this condition and the generally accepted surgical treatment strategies must be discussed. Although the occurrence of GJCF has decreased remarkably as a result of better treatment, the modern management of this condition and the generally accepted surgical treatment strategies must be discussed [4].
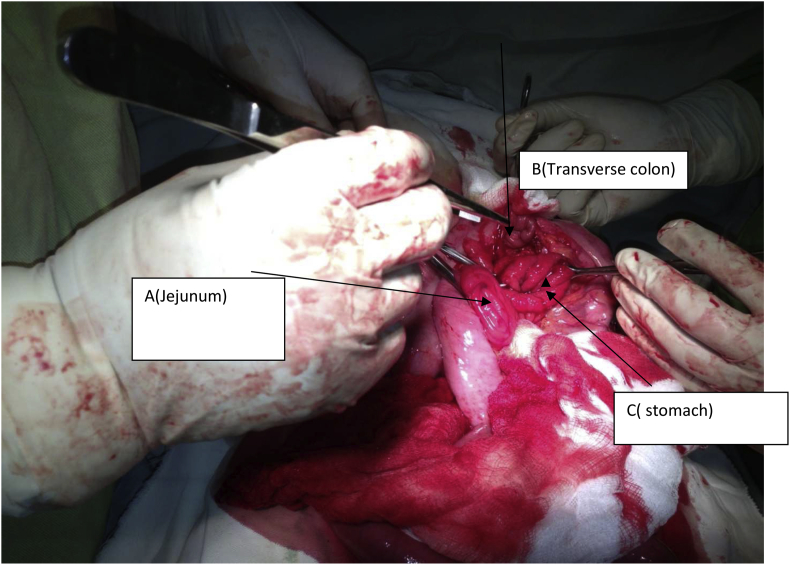
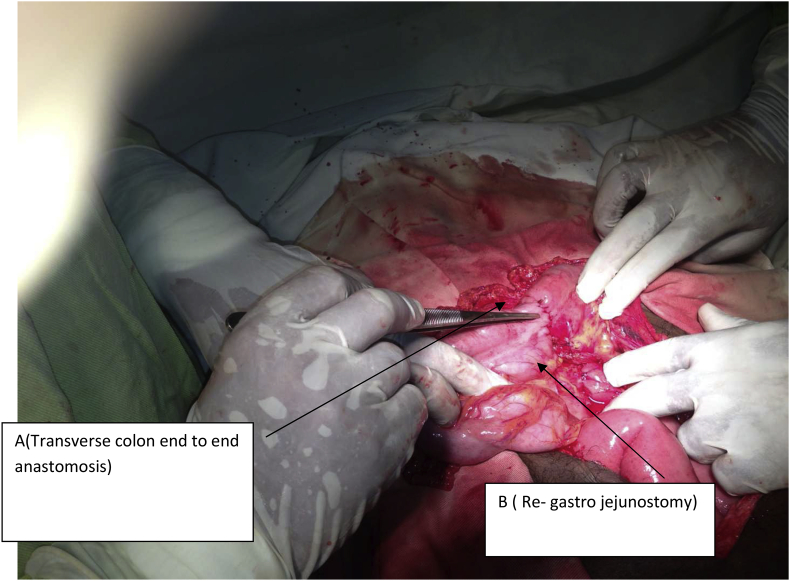
In this report, we described two cases of GJCF fistula in patients of 60 and 40 years men and review the literature relevant to their diagnosis and management (Fig. 1, Fig. 2).
Fig. 1.
Intraoperative acquired photograph showing involvement of the stomach, jejunum and transverse colon in a fistulous communication.
Fig. 2.
Intraoperative acquired photograph showing gastrojejunostomy and end-to-end transvers colon anastomosis.
In the late 1930s, since patients with GJCF fistula were usually malnourished, operative mortality and morbidity were high; as a result, a two-stage or three-stage procedure was recommended [5].
In this report, we describe two cases of GJCF fistula in patients of 60 and 40 years men and review the literature relevant to their diagnosis and management.
2. Case reports
2.1. Case one
This is a 60 years old male admitted to our hospital in October 2014 after he presented with 1year and 6 months history of dull aching post prandial epigastric pain with no radiation to any site. Since a year prior to his presentation he experienced passage of loose stool (4–5 times per day). Since four months prior to his admission he experienced halitosis and vomiting of fecal matter. He lost appetite and has significant un-quantified weight loss. He underwent abdominal surgery 13 years back for the complaint of repeated vomiting of ingested matter after long history of dyspepsia (the operating surgeon remembered the procedure and it was Truncal vagotomy + Gastrojejunostomy for Gastric outlet obstruction).
At admission he was emaciated (BMI = 15), slightly pale conjunctiva and supra umbilical surgical scar. There was no pertinent finding in the other systems. He was investigated with stool examination, complete blood count, serum electrolytes and albumin, blood group and RH, abdominal X-ray, ultrasound, ECG and RBS. Hemoglobin was 9 g/dl, albumin 2.9 g/dl and blood group B + ve. Other investigations were within the normal range. Upper gastrointestinal endoscopy results revealed no active ulcer but scarred area. Patient was properly resuscitated and nutritional build up with total parental nutrition (TPN) and bowel rest for three weeks was done. Elective surgical exploration was performed through the previous incision and the intraoperative finding was gastrojejunocolic fistula. It was difficult to revise the completeness of the vagal trunk due to severe adhesion in the area of the abdominal esophagus.
The site of communication was resected in block and re-gastrojejunostomy and end-to-end anastomosis of the transverse colon done. Histologic examination of the resected specimen found no evidence of active ulcer or malignant transformation. The postoperative course in hospital was successful and the patient was discharged on the seventh postoperative day with proton pump inhibitor. He was on monthly follow up for the first three months and then after every six months has gained weight and his BMI raised to 20.
2.2. Case two
A 40 year old gentle man visited our referral hospital in June 2012 was presented with mild dull aching epigastric pain of one-year duration. Six months prior to his presentation he experienced repeated vomiting of feculent matter and diarrhea (6–7 times per day). He lost his appetite and about 25 kg weight over the last year. He was operated five times before 15 years for complications of peptic ulcer disease (first for perforated peptic ulcer disease, second operation for leaked Grahams Patch in the same week of the first operation, third operation ten years later for Gastric outlet obstruction, fourth and fifth are the current surgeries for GJCF and anastomosis leak). On physical examination he was emaciated with pale conjunctiva, there were multiple healed surgical scars on his abdomen. There was no pertinent finding on the other systems.
On investigation he was mildly anemic (hemoglobin = 9 g/dl), albumin was 2.61 g/dl and his coagulation profile was PTT 48 s and INR was 2.5. Barium meal showed passage of the contrast to the transvers colon through a fistulous tract; Upper gastrointestinal endoscopy revealed no active ulcer but scarred area. Serum electrolytes were within the normal range. After proper resuscitation with ringers lactate, normal saline, Vitamin K supplementation, nutritional build up with TPN and bowel rest of three weeks, he was explored on elective bases through the previous supra umbilical mid line surgical incision and the intraoperative finding was GJCF. posterior vagus was intact which can be evidence for high acid secretion.
The site of communication was dismantled, distal gastrectomy, truncal vagotomy, segmental resection of the jejunum and transverse colon and Roux-en-Y reconstruction was done. Truncal vagotomy was done because during the pre operative counseling patient was reluctant to take proton pump inhibitors for long period of time and preferred vagotomy rather. Patient was haemo-dynamically unstable postoperatively and developed anastomotic leak on his 5th post operative day for which he was re-explored and reanastomosis was done but he died after 4 days of re-exploration due to sepsis.
3. Discussion
Gastrojejunocolic fistula (GJCF) is a late and uncommon postoperatively complication of gastrojejunostomy mainly caused by insufficient resection of the stomach, incomplete vagotomy, retained antrum after gastrectomy and a long afferent loop may lead to the development of a stomal ulcer, which induces this disease recurrent [1], [2].
Due to severe diarrhea, vomiting, less intensive care absences of H2-blockers and proton pump inhibitors mortality and morbidity of patients with GJCF fistula in the late 1930s was very high. Hence, a two-stage or three-stage procedure was recommended to manage cases [5], [6], [7], [8]. This trend of high mortality rate of patients however; was decreased due to the recent advances in parenteral nutritional support and intensive care. Hence, it was recommended a one-stage resection to be performed [9].
Besides, due to the treatment of peptic ulcers with H2 receptor antagonists, proton pump inhibitors and eradication of Helicobacter pylori, the incidence of such fistulas has been recently decreased dramatically [10], [11]. However, since the fistula can develop one to 20 years after gastrectomy [5], it is still an important and the contribution of previous surgery should not be overlooked. Factors, such as smoking, use of non steroidal anti inflammatory agents, alcohol use and chronic anticoagulation can also lead to postoperative marginal ulceration which in turn lead to GJCF [12], [13], [14].
In our cases even if both patients were severely malnourished during admission, proper resuscitation and stabilization was first done, then a single stage en bloc resection was carried out. Diagnosis of a GJCF fistula is straightforward with high clinical suspicions. Marshall and Knud-Hansen and Chung et al. have described the triad of symptoms associated with a GJC fistula as diarrhea, weight loss, and eructation of fecal-smelling gas [3], [5]. These symptoms were also seen in our cases where both had vomiting of fecal-matter, diarrhea, weight loss and poor appetite.
GJCF fistulae suspected patients may be confirmed using an upper GI series or water-soluble contrast enema. Barium enema which has been found by Thoeny et al. [12] has 95% sensitivity for making the diagnosis of GJCF as compared with 27% sensitivity with X-ray film series of the upper GI tract. In both of our cases, upper GI series confirmed the diagnosis by showing passage of Barium meal contrast from the stomach to the jejunum and transverse colon.
The role of endoscopy in establishing the diagnosis of GJCF by excluding other GI disease has been mentioned. Hence recommendations were given that simultaneous examination using gastroscopy and colonoscopy are useful in the diagnosis of GJCF [13]. In our cases, both gastroscopy and colonoscopy were not able to detect the fistulae initially. These results indicate that endoscopy negative findings are insufficient to rule out the diagnosis of GJCF fistulae. Tissue biopsy was done and showed no malignant features in both cases.
Despite inadequate surgery, resulting from gastroenterostomy, inadequate gastric resection, or incomplete vagotomy is the main reason for GJCF, stomach ulcers are also reported to cause an early formation of GJCF [14]. In our cases however, endoscopy results showed no active ulcer formation in both patients.
Management of GJCF is always essential and comprises en bloc resection of the fistula (revision of gastrectomy), partial resection of the jejunum and the colon, which involves the fistulous communication and restoration of continuity of the digestive tract. Better medical treatment at the phase of stomal ulcer with proton pump inhibitor and Helicobacter pylori eradication do also play great role in prevention of the disease. However, treatments directed only toward the fistula is inadequate unless the ulcer diathesis is also corrected.
4. Conclusion
Gastrojejunocolic fistulas are rare and late case mainly develops as a result of inadequate resection of the stomach or incomplete vagotomy in the past. Therefore, the potential contribution of previous surgery is often overlooked. Hence, high clinical suspicion should be done in the diagnosis of patients who manifest chronic diarrhea, vomiting of fecal matter, abdominal pain and features of malnutrition. Upper GI series with small bowel follow-through or water-soluble contrast enema study were found confirmatory diagnostic tool. Negative findings on endoscopy do not rule out the diagnosis of a GJCF. One-stage en bloc resection is feasible if the patient's general condition is good or can be maintained during a time of bowel rest with TPN. Treatment directed only toward the fistula is inadequate unless the ulcer diathesis is also corrected.
Ethical approval
We only the consent of the patients, hence no ethical issue was needed as it is case reports.
Sources of funding
No fund was needed as it is case report which is part of the routine activities.
Authors' contributions
Girmay Hagos Araaya (principal investigator and conceived that it has to be published to the scientific community), Kibrom Gebresilasie , Weldehawaria Weldu did the patient management and write literature reviews. Araya Gebreyesus Wasihun prepared the manuscript for publication. All authors read and approved the final manuscript.
Conflicts of interest
Authors declare that there is no any conflict of interest.
Guarantor
Araya Gebreyesus Wasihun (Assistant professor of microbiology)
E-mail araya13e25@gmail.com
Consent
Written informed consent was obtained from the patients for publication of these case reports and taking the images.
References
- 1.Takemura M., Hamano G., Nishioka T., Takii M., Mayumi K., Ikebe T. One-stage laparoscopic-assisted resection of gastrojejunocolic fistula after gastrojejunostomy for duodenal ulcer: a case report. J. Med. Case Rep. 2011;5:543. doi: 10.1186/1752-1947-5-543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Takemura M., Hamano G., Nishioka T., Takii M., Mayumi K., Ikebe T. One-stage laparoscopic-assisted resection of gastrojejunocolic fistula after gastrojejunostomy for duodenal ulcer: a case report. J. Med. Case Rep. 2011;5:543. doi: 10.1186/1752-1947-5-543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chung D.P., Li R.S., Leong H.T. Diagnosis and current management of gastrojejunocolic fistula. Hong Kong Med. J. 2001;7:439–441. [PubMed] [Google Scholar]
- 4.Kim H.K., Jee S.Y. Gastrojejuno-colic fistula after gastrojejunostomy. J. Korean Surg. Soc. 2013;84(4):252–255. doi: 10.4174/jkss.2013.84.4.252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marshall S.F. A plan for the surgical management of gastrojejunocolic fistula. Ann. Surg. 1945;121:620–633. doi: 10.1097/00000658-194505000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Eyskens E., Van Moer E., Vanderstighelen Y. Gastrocolic and gastrojejunocolic fistulas. 6 cases. Acta Chir. Belg. 1985;85(5):287–292. [PubMed] [Google Scholar]
- 7.Mathewson C., Jr. Preliminary coloctomy in the management of gastrocolic and gastrojejunocolicnfistulae. Ann. Surg. 1941;114:1004–1010. doi: 10.1097/00000658-194112000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tseng H.C., Lee C.H., Wu C.W., Lui W.Y., P'eng F.K. Gastrocolic, duodenocolic & gastrojejunocolic fistulas report of 16 cases. Taiwan Yi Xue Hui Za Zhi. 1985;84(5):609–615. [PubMed] [Google Scholar]
- 9.Cody J.H., DiVincenti F.C., Cowick D.R., Mahanes J.R. Gastrocolic and gastrojejunocolic fistulae: report of twelve cases and review of the literature. Ann. Surg. 1975;181(3):376–380. doi: 10.1097/00000658-197503000-00021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ohta M., Konno H., Tanaka T., Baba M., Kamiya K., Mitsuoka H., Unno N., Sugimura H., Nakamura S. Gastrojejunocolic fistula after gastrectomy with Billroth II reconstruction: report of a case. Surg. Today. 2002;32:367–370. doi: 10.1007/s005950200054. [DOI] [PubMed] [Google Scholar]
- 11.Kece C., Dalgic T., Nadir I., Baydar B., Nessar G., Ozdil B., Bostanci E.B. Current diagnosis and management of gastrojejunocolic fistula. Case Rep. Gastroenterol. 2010;4(2):173–177. doi: 10.1159/000314048. Thoeny RH, Hodson JR, Scudamore HH: The roentgenologic diagnosis of gastrocolic tract and gastrojejunocolic fistulas. Am J Roentgenol Radium Ther Nucl Med 1960, 83:876-881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jacobs D.O., Robinson M.K. Morbid obesity and operations for morbid obesity. In: Zinner M.J., Ashley S.W., editors. Maingot's Abdominal Operations. 11th ed. Appleton & Lange; New York: 2007. p. 472. [Google Scholar]
- 13.Capella J.F., Capella R.F. Gastro-gastric fistulas and marginal ulcers in gastric bypass procedures for weight reduction. Obes. Surg. 1999;9:22–27. doi: 10.1381/096089299765553674. [DOI] [PubMed] [Google Scholar]
- 14.Lee Y.T., Sung J.J., Choi C.L. Ulcer recurrence after gastric surgery: is Helicobacter pylori the culprit? Am. J. Gastrolenterol. 1998;93:928–931. doi: 10.1111/j.1572-0241.1998.00279.x. [DOI] [PubMed] [Google Scholar]