Abstract
Though many methods of prevention of STI/HIV are available, condoms remain of utmost importance. They have gone a long way from the oiled silk paper used by the Chinese and the hard sheaths made of tortoise- shell used by the Japanese to the latex condoms of today. The breakthrough came when the rubber vulcanization process was invented by Charles Goodyear and eventually the first rubber condom was made. The condom offers maximum protection( more than 90%) against HIV, Hepatitis B virus and N.Gonorrhoea. They also offer protection in scenarios when alternate sexual practices are adapted. The female condom in the only female driven contraceptive method available today. Graphene and Nano lubricated condoms are new in the market and others in futuristic approach may include wearable technology/Technology driven condom and invisible Condoms. Both Correct and Consistent use of condoms needs to be promoted for HIV/STI prevention.
Keywords: Condoms, efficacy, future, history, issues
INTRODUCTION
Though many methods of prevention of sexually transmitted infection (STI)/HIV are available, female empowerment is still a distant dream, behavioral change is not yet on the horizon and vaccines need more encouraging trials. Until that time, condoms remain important armamentaria for STI/HIV prevention.
With the adoption of permanent sterilization and also with the promotion of emergency contraceptive pill, condoms are becoming more important for STI/HIV prevention.
CONDOM HISTORY
Condoms or sheaths are the oldest forms of barrier contraception used by the male.[1] It has been suggested that the Ancient Egyptians were among the first to wear them [Figure 1]. The earliest description of the condom was by the great Italian anatomist Gabriello Fallopio [Figure 2] in 1564, published 2 years after his death. He claimed to have invented a linen sheath made to fit the glans and it was worn for protection against syphilis.
Figure 1.
Egyptian condoms (source: Internet)
Figure 2.

Gabriello Fallopio
Gut condom was invented by English army doctor Colonel Quondam, a physician and Colonel to King Charles 1 (1660-1685). He provided the King with means of preventing illegitimate offsprings and the word condom is probably a corruption of his name. Most authorities have rejected this story. The word condom first appeared in print in 1706 in a poem by Lord Belhaven and then in a book by Daniel Turner in 1717. Ferdy in 1904 proposed a French village of the condom as the source of the word, but a year later he suggested that the Latin word “condus” was the origin. Richter in 1911 proposed a Persian “Kendu” or “Kondu” as the source of the word, which means a long storage vessel made from animal intestine. The Chinese utilized oiled silk paper [Figure 3] and the Japanese used to wear hard sheaths made of tortoise-shell, horn (kabutogata), or fine leather. The original condoms were made from the animal intestine (cecum) of sheep [Figure 4], calves, and goats. The introduction of liquid latex in the mid-1930 made possible greater tensile strength and longer shelf life of 5 years instead of 3 months. In the later 1960's polyurethane was used but due to a high rupture rate, the research was discontinued.
Figure 3.

Silk condoms (Chinese)
Figure 4.

Condom made from animal intestine circa (source: Internet)
Wm E Kruck, of the University of North Carolina, conducted research for the American Dialect Society and in 1981, concluded that the origin of the word is unknown and is definitely not derived from Latin. For the sake of completeness of his research, he included the suggestion of the Playboy Magazine in 1972 in Chicago “Conundrum! A riddle, difficult to put on.” By the 18th century, “the condom,” “preservative machine,” or “armor” as it was variously described had achieved some popularity for its contraceptive as well as its prophylactic functions.
The rubber vulcanization process was invented by Charles Goodyear [Figures 5 and 6] in 1839 and patented in 1844. First, rubber condom was produced in 1855.
Figure 5.

Charles Goodyear
Figure 6.

Goodyear Tyre
The smallest microorganism transmitting a sexually transmitted disease the herpes virus has a diameter of 0.1 Am about 1000 times larger than air or water molecules. There is no evidence of passage of viral particles across the condom membranes in vitro. It is possible that a male or female sheath or both were used in Imperial Rome, but no evidence exists beyond a legend related by Antoninus Libralis (AD 150) in which goats' bladder served as a female sheath.
TYPES OF CONDOMS
Three types of condom materials used include natural materials, latex rubber, and plastic. Natural condoms are an effective barrier against sperm and bacterial STDs but do not protect against viral organisms such as HIV, which are smaller than bacteria. Natural condoms allow the transfer of body heat between partners. Latex condoms are less porous than natural condoms and hence form a more effective barrier that can block smaller organisms, such as HIV. They reduce heat transfer that may contribute to reduce sexual pleasure. Plastic or polyurethane condoms are under development. They provide an effective barrier against HIV as well as bacterial STDs while at the same time allowing better transfer of heat. They are thinner than latex condoms and increase sensitivity. However, plastic condoms are more expensive than latex condoms and less flexible so more lubrication may be needed.
Condoms are made in different lengths and widths. Different manufacturers produce varying sizes. There is no standard length for condoms, and they are increasingly made in a range of sizes. The width of a condom also varies. Some condoms have a slightly smaller width to give a closer fit while others will be slightly larger.
PROTECTION
Typical use (both incorrect and inconsistent use) of the male condom has a failure rate of approximately 14%.[2] Efficacy is 97% with perfect use (correct and consistent use) and 86% with typical use.[2] They confer full protection only in conditions causing urethral discharge. In conditions such as syphilitic chancre, condyloma acuminate, and giant herpetic ulcer, only parts covered by a condom are protected. A condom chancre is a penile chancre close to the radix penis which is an area beyond the protection of a condom.
PROTECTIVE EFFICACY OF CONDOM IN DIFFERENT SEXUALLY TRANSMITTED INFECTIONS
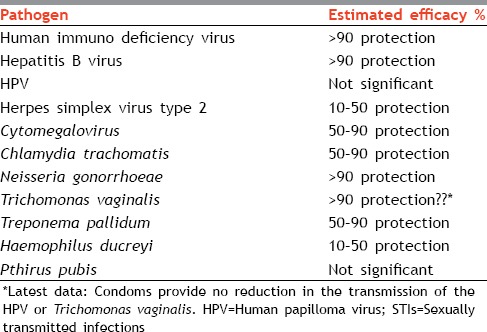
The protective value of condom is variable. It is less protective against, currently, more prevalent infections such as human papillomavirus (HPV) and herpes simplex virus (HSV). The part not covered by a condom can act as a portal of entry/exit for microorganisms [Table 1].
Table 1.
Protective efficacy of condom in different STIs
Bacterial sexually transmitted infections
The male condom offers more than 90% protection against Neisseria gonorrhoeae, 50-90% protection against Chlamydia trachomatis as well as Treponema pallidum, and 10-50% protection against Haemophilus ducreyi. Two cross-sectional and one case-control study showed 49-75% reduction in risk of gonorrhea.[3] A case-control study in STD clinic in Seattle showed 33% risk reduction of chlamydial infections with consistent condom use.[3] In another prospective study, none of the men using condom developed chlamydial infections as compared to 6.3% among nonusers syphilis transmission is reduced 29% for typical use.[4] It is reduced 50-71% when condoms are used 100% of the time correctly.
Viral sexually transmitted infection
The male condom offers more than 90% protection against HIV and Hepatitis B virus, 50-90% protection against Cytomegalovirus (CMV), and 10-50% protection against HSV-2. HIV transmission is reduced by approximately 85% when condoms are used 100% of the time correctly. Hepatitis B transmission is reduced by approximately 90%. Genital herpes transmission is reduced by approximately 40%. Protection conferred against HPV is not significant. Condoms provide no reduction in the transmission of the HPV. HPV colonized in anogenital canal with potential of transmission due to viral shedding even when the person is asymptomatic.
Trichomonas vaginitis
It is claimed to provide more than 90% protection against Trichomonas vaginitis, but the latest reports are controversial. Statistically significant reduction in trichomonas infection (30%) was reported with condom use.[3]
Protection conferred against Pthirus pubis is not significant.
CONDOMS AND ALTERNATIVE SEXUAL PRACTICES
A prospective study of pharyngeal gonorrhea and inconsistent condom use for oral sex among female brothel-based sex workers in Singapore by Wong et al showed that the prevalence of consistent condom use for oral sex was 70.4% compared to 96.8% for vaginal sex. Sex workers with inconsistent condom use for oral sex were 17.1 times more likely than consistent condom users to develop pharyngeal gonorrhea.[5]
Worldwide, men who have sex with men (MSM) are 18 times more likely to be infected with HIV than the general population.[6] The HIV epidemic has begun to stabilize in many countries, but it still continues to affect MSM disproportionately. Unprotected anal sex is the main cause of the HIV epidemic among this population.
In addition to this, 5-10% of world's population engages itself in anal sex. A number of studies conducted over the past quarter century have found that people who reported consistent condom use reduced their risk of HIV transmission during anal sex by 70-87 percent.[7] Currently, available condoms do offer protection in scenarios when alternate sexual practices are adapted.
A California-based company is hoping to revolutionize protective barriers by introducing the Origami Condom (company website), the first dedicated condom for receptive anal intercourse. Their three condom types are currently under the clinical testing and are expected to come in the market by 2015, but already the prototype has received much attention.
ISSUES WITH CONDOM USE
Condom use errors include late application, early removal, slipping off during sex, and reuse of condoms.
In a study by Topping et al titled “A comparison of condom use errors and problems for heterosexual anal and vaginal intercourse,” prevalence of condom use errors and similar problems regardless of intercourse type was evaluated. Anal intercourse was more likely to report using water-based (P < 0.001) and oil-based (P = 0.037) lubricant and to remove condoms before sex was finished (P < 0.001). Condom use promotion programs designed for heterosexual adults are needed that address condom use errors.[8] In a study by Crosby et al titled “Condom use errors and problems: A study of high-risk young Black men residing in 3 Southern US cities,” it was observed that condom use errors and problems were common with some of the critical errors occurring in >1 of every 5 young black men.[9] In another study by Lang et al regarding Predictors of condom errors among sex workers in Armenia' observed condom use errors in 78.0% of participants.[10]
Factors associated with condom use errors are number of clients, higher frequency of condom application on clients by female sex worker, greater perceived barriers to condom use, elevated depressive symptomatology, and having sex while drinking alcohol.
A study by Crosby et al titled “Slips, breaks and falls: Condom errors and problems reported by men attending an STD clinic” observed that 19% of cases were associated with “fit and feel” problems, 15% involved breakage, 14% involved lost erection, 9% associated with lost erection while application, 8% involved slippage during withdrawal, and 7% involved slippage during sex. None of these summative variables (total errors, total problems or total of errors and problems) were significantly associated with age, minority status or whether men indicated they had ever been taught how to use condoms.[11]
Latex allergy
It is of two types. Immediate reaction, which is a type I reaction (anaphylaxis), and delayed hypersensitivity reaction, which is a type IV reaction. Symptoms include urticaria or skin rash/hives, itching, cough, watery eyes, sneezing, running nose, chest tightness, shortness of breath, wheezing, confusion, low blood pressure, and dizziness. It has been reported in spouses as well. Alternatives to latex condoms include synthetic condoms, made of polyurethane, or natural membrane condoms (made from lamb intestine).
Determinants of condom use
Approximately, 85% and 69% women from urban and rural areas, respectively had heard of a condom. Currently, 9.8 urban and 3.2% rural married women are condom users. It was also observed that among sexually active unmarried population, 72.4% women and 98% men used condom. It may be because of accessibilities, availability, policies, and political influence that affect the prevalence of condom use. This apparent variation may be due to the use of condom primarily for pregnancy prevention in the north and for HIV prevention in the south.[12]
REASONS FOR USING CONDOMS
The reason for choosing condoms over other spacing family planning methods is the fear of side effects of other modern spacing methods. The most common reason for discontinuing oral pills and intrauterine devices within 1 year of beginning their use was concerns with side effects or health concerns.[12]
REASONS FOR NOT USING CONDOM
The most significant barriers such as lack of privacy in stores and social stigma were associated with condom use. The reported problems related to not using condom include not accepted by sexual partner, perceived ineffectiveness, less comfort, lack of sexual satisfaction with condoms, husband's alcohol use, depression, anxiety, and not available at that instant.[12]
Further, female sterilization is the dominant family planning method in India. Couples in whom either the husband or wife has been sterilized may not be motivated to use condoms. They perceive that asking for use of the condom indicates the infidelity or having multiple partners.
FEMALE CONDOM
Females are vulnerable to STIs because of biological and socioeconomic factors. They are not able to negotiate for safe sex particularly for the use of the male condom. Hence, the need of the hour is female driven protective devices.
The female condom is made up of prelubricated polyurethane sheath which covers introitus in toto. It is effective as a contraceptive as well as protective against HIV/STI with the efficacy of 95% with perfect use and 79% with typical use.[2] However, it is less accessible, costly, and not easily available. It has less acceptability as insertion is difficult with nonacceptance by the male partner. It is difficult to procure and difficult to use more so in the Indian context where female literacy is low. Potential for re-use of the female condom must not be overlooked.
Disadvantages of the female condom are that they are relatively more expensive with more mechanical problems than the male condom, insertion and removal difficulties, penetration difficulties, dissatisfaction in the fit and feel of condom during intercourse, breakage and slippage of condom, and pain during intercourse.
A study by Vijayakumar et al titled “A review of female-condom effectiveness: Patterns of use and impact on protected sex acts and STI incidence” indicated strongly the benefits of female-condom use in increasing protected sex acts and decreases in STI incidence with the introduction of the female condom.[13] Female condom is more accessible to women who are less likely to use other dual protection methods. In another study “Female condom and male condom failure rate among women at high risk of sexually transmitted diseases,” women with high-risk sexual activity were studied. Breakage was less common for female condoms than for male condoms, but the slippage was more common for the female condoms than for male condoms. From first use to more than15 uses, combined failure rate fell from 20% to 1.2% for female condoms and 9%-2.3% for male condoms.[14]
The relative risk of acquiring gonorrhea infection among women using a diaphragm with spermicide is half the risk of women whose male partners used condoms. In addition, the pelvic inflammatory disease was less for diaphragm users than for condom users. The female condom has been shown in vitro to be impermeable to HIV and CMV and in one clinical trial to prevent to trichomoniasis infection. The most striking feature of the female condom is that it gives women the means to protect themselves from STDs without relying on partner cooperation. Many women do have the leverage in sexual encounters to negotiate the use of male condom due to culturally sanctioned male dominance in relationships.[15]
The first-generation female condom (FC1®), manufactured by the Female Health Company (FHC), was a silicone-lubricated polyurethane sheath with flexible rings at each end to aid insertion into the vagina and hold the condom in place. It has been replaced by FHC's second-generation product, the FC2®. The FC2® has the same design and dimensions as the FC1® but is made of nitrile rubber, synthetic latex.[16] The VA w.o.w.® or “Reddy” female condom, manufactured by MedTech Products Ltd., of India, is made of natural rubber latex, comes prelubricated with silicone, has a triangular outer frame, and uses a sponge to secure the condom in the vagina. The Cupid™ female condom, manufactured by Cupid Ltd., India, is made of natural rubber latex, comes prelubricated with silicone, has an octagonal outer frame, and uses a sponge to hold the condom in place in the vagina. The woman's condom, manufactured by Dahua Medical Apparatus Company of Shanghai, China, is made of thin polyurethane film. The pouch folded into a capsule that quickly dissolves after insertion in the vagina. Once the capsule dissolves, the condom unfolds, releasing four foam shapes that cling lightly inside the vagina and hold the condom in place. The Phoenurse female condom, manufactured by Tianjin Condombao Medical Polyurethane Tech. Co. Ltd., is made of polyurethane, has an inner ring to hold the condom in place, comes prelubricated with a water-based lubricant, and is packaged with an insertion tool, sanitary towel, and disposable bag.[17]
FUTURE PERSPECTIVE
Graphene condoms are made of an extremely thin-but-strong layer of crystalline carbon, so that they can be thinner than current latex offerings and also conduct heat better. The nano-lubricated condom contains a coating of super-hydrophilic nanoparticles (ultra-thin layer of trapped water). The coating is created using nanofabrication technology and promises to be a more resilient form of lubricant than what we use today. Other futuristic approach includes Wearable technology/technology driven condom and invisible Condoms. Invisible condoms consist of a gel that hardens upon increased temperature after insertion into the vagina or rectum. In the laboratory, it has been shown to block HIV and HSV effectively. The barrier breaks down and liquefies after several hours. As of 2005, the invisible condom is in the clinical trial phase and has not yet been approved for use. Furthermore, a condom treated with an erectogenic compound is developed in 2005. The drug-treated condom is intended to help the wearer maintain his erection, which should also help reduce slippage.
CONCLUSION
Condoms have come a long way from the oiled silk paper used by the Chinese, and the sheaths of tortoise shell used by the Japanese to the latex condoms of today.[18] The protective efficacy of the condoms is different for STIs, the highest being against HIV, Hepatitis B, and N. gonorrhoeae (more than 90%). Protection against currently prevalent STIs such as HPV and HSV is comparatively less. For HPV protection offered is not significant and it is 10-50% for HSV. Currently, available condoms also offer protection when alternate sexual practices are adapted. Certain issues with condom use include condom use errors such as late application, early removal, slipping and latex allergy. Female condoms are the only available female driven devices and offer considerable protection against the different STIs. Graphene condoms and Nano lubricated condoms represent the future of condoms. In the wish list, there is all in one condom which is coated with spermicides and microbicides, having similar protection for different mucosa. Both correct and consistent use of condoms is necessary for STI and HIV prevention and is, in the true sense, the need of the hour.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Youssef H. The history of the condom. J R Soc Med. 1993;86:226–8. doi: 10.1177/014107689308600415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Trussel J. In: Contraceptive Technology. 20th ed. Hatcher, editor. 2011. Adapted from WHO 2007-2013. [Google Scholar]
- 3.Workshop Summary: Scientific Evidence on Condom Effectiveness for Sexually Transmitted Disease (STD) Prevention. Hyatt Dulles Airport Herndon. Virginia: 2000. [Google Scholar]
- 4.Holmes KK, Levine R, Weaver M. Effectiveness of condoms in preventing sexually transmitted infections. Bull World Health Organ. 2004;82:454–61. [PMC free article] [PubMed] [Google Scholar]
- 5.Wong ML, Chan RK. A prospective study of pharyngeal gonorrhoea and inconsistent condom use for oral sex among female brothel-based sex workers in Singapore. Int J STD AIDS. 1999;10:595–9. doi: 10.1258/0956462991914726. [DOI] [PubMed] [Google Scholar]
- 6.Beyrer C, Baral SD, van Griensven F, Goodreau SM, Chariyalertsak S, Wirtz AL, et al. Global epidemiology of HIV infection in men who have sex with men. Lancet. 2012;380:367–77. doi: 10.1016/S0140-6736(12)60821-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Smith D, et al. Condom Efficacy by Consistency of Use among MSM: US. 20th Conference on Retroviruses and Opportunistic Infections; Atlanta. 2013. Abstract 32. [Google Scholar]
- 8.Topping AA, Milhausen RR, Graham CA, Sanders SA, Yarber WL, Crosby RA. A comparison of condom use errors and problems for heterosexual anal and vaginal intercourse. Int J STD AIDS. 2011;22:204–8. doi: 10.1258/ijsa.2011.010259. [DOI] [PubMed] [Google Scholar]
- 9.Crosby RA, Milhausen RR, Sanders SA, Graham CA, Yarber WL. Condom use errors and problems: A study of high-risk young black men residing in three Southern US cities. Int J STD AIDS. 2014;25:943–8. doi: 10.1177/0956462414526707. [DOI] [PubMed] [Google Scholar]
- 10.Lang DL, Salazar LF, Diclemente RJ, Markosyan K, Darbinyan N. Predictors of condom errors among sex workers in Armenia. Int J STD AIDS. 2011;22:126–30. doi: 10.1258/ijsa.2009.009418. [DOI] [PubMed] [Google Scholar]
- 11.Crosby R, Yarber WL, Sanders SA, Graham CA, Arno JN. Slips, breaks and ‘falls’: Condom errors and problems reported by men attending an STD clinic. Int J STD AIDS. 2008;19:90–3. doi: 10.1258/ijsa.2007.007103. [DOI] [PubMed] [Google Scholar]
- 12.Donta B, Begum S, Naik DD. Acceptability of male condom: An Indian scenario. Indian J Med Res. 2014;140(Suppl):S152–6. [PMC free article] [PubMed] [Google Scholar]
- 13.Vijayakumar G, Mabude Z, Smit J, Beksinska M, Lurie M. A review of female-condom effectiveness: Patterns of use and impact on protected sex acts and STI incidence. Int J STD AIDS. 2006;17:652–9. doi: 10.1258/095646206780071036. [DOI] [PubMed] [Google Scholar]
- 14.Vaalappel T, et al. Female condom and sexual transmission. Vol. 32. THS; 2005. pp. 35–43. [Google Scholar]
- 15.Mcollete JD. The female condom - Where method and user effectiveness meet. Stanford Med Stud Clin J [Google Scholar]
- 16.Female Health Company (FHC) Chicago: FHC; 2011. 2010 Annual Report: Working for the Health of Women Worldwide. [Google Scholar]
- 17.Global Campaign for Microbicides: Female Condom. Available from: http://www.global.campaign.org/female.condom.htm .
- 18.Cates W., Jr The NIH condom report: The glass is 90% full. Fam Plann Perspect. 2001;33:231–3. [PubMed] [Google Scholar]


