Abstract
Introduction:
Prevalence and pattern of acquired syphilis are changing in India in recent years because of good laboratory diagnosis and treatment, but it still remains a major public health problem with significant regional variations.
Aim:
To study the changing trend of acquired syphilis in a Tertiary Care Center of North India.
Subjects and Methods:
Retrospective analysis of all the cases of sexually transmitted infections (STIs) registered in the Skin and VD Department of PGIMS, Rohtak from January 2008 to December 2012 was done. Complete epidemiological, clinical, and investigational data were recorded and analyzed for changing trends in prevalence, pattern and clinical presentations of syphilis.
Observation:
Total of 1462 cases attended the STI clinic from January 2008 to December 2012. A total of 124 patients were venereal diseases research laboratory reactive, of which 33 (2.25%) were false positive cases, and Treponema pallidum hemagglutination was reactive in 91 cases (6.22%). Totally, 91 (6.22%) cases were diagnosed as syphilis. Of 91 cases, 78 (85.71%) were males and 13 (14.29%) were females. Primary syphilis was diagnosed in 21 (13.08%), secondary in 38 (41.76%), and latent in 32 (35.16%) patients. 4 (10.53%) of the secondary syphilis were having asymptomatic rash, 14 (36.84%) had condyloma lata and 17 (44.74%) had genital ulcer with cutaneous rash. Mixed infection was detected in 7 patients. 8 (8.79%) were human immunodeficiency virus positive.
Conclusion:
Although our study indicates a decreasing trend in the prevalence of syphilis in last 5 years, there is a rise in latent syphilis as compared to primary syphilis demanding steps to increase awareness among general population.
Keywords: Acquired syphilis, biological false positive, latent, Treponema pallidum hemagglutination
INTRODUCTION
Syphilis “the great imitator” was defined by Stokes as an infectious disease caused by Treponema pallidum, systemic from the outset, characterized by florid manifestations on the one hand and years of complete asymptomatic latency on the other, capable of involving practically every organ in its course, simulating almost every disease in the field of medicine and surgery, transmissible to the offspring in man, transmissible to certain laboratory animals, and treatable to the point of presumptive cure.[1,2,3] True to the definition, prevalence and clinical patterns of syphilis are changing in India recently because of availability of good laboratory diagnosis and treatment and increased health awareness, but it still remains a major public health problem with significant regional variations. Decreasing prevalence of bacterial sexually transmitted infections (STIs) and an increasing prevalence of viral STIs reflect rampant use of antibiotics and asymptomatic bacterial infections.[4,5,6] There is a dearth of information regarding the epidemiology of STIs in India for many reasons such as stigma and discrimination associated with STIs.[7] The phenomenon of biological false positive (BFP) also merits attention as many infectious and inflammatory diseases could mimic syphilis clinically as well as serologically. Human immunodeficiency virus (HIV) infection alters the clinical manifestations and course of syphilis, and mixed infections are not uncommon. Thus, we did a retrospective clinico-investigative study to analyze the current status of syphilis and to identify the changes in the epidemiological and clinical trends of syphilis over the past 5 years.
SUBJECTS AND METHODS
Clinical records of all the patients who attended the STI clinic of PGIMS, Rohtak from January 2008 to December 2012 constituted the baseline data of this retrospective study. Details of epidemiological features, complete clinical examination, and presence of any other concomitant STI were noted. Venereal diseases research laboratory test (VDRL) and HIV test were done in all patients. VDRL antigen from Institute of Serology, 3, Kyd Street, Calcutta was used throughout the study period. Internal quality control was used by the laboratory as a method for quality assurance. Rapid Test for HIV by SD BIO LINE HIV 1/2 was done in all patients as a screening test; the confirmatory test being Western Blot. The patients who were VDRL reactive were subjected to T. pallidum hemagglutination (TPHA) testing. TPHA test by Omega Diagnostics Immutrep Tpha Kit (sensitivity of 98.5% and specificity of 99.6%) was taken as the confirmatory test for syphilis, the same kit being used throughout 5 years. In patients whose TPHA was negative but VDRL was positive, a repeat VDRL was done. If the repeat VDRL test was positive too and on detailed history and examination, no evidence of syphilis had been detected, it was considered to be a BFP VDRL. If the repeat VDRL test was negative, it was considered as technical false positive (refers to false positive VDRL due to laboratory error). In those cases where the clinical presentation was suggestive of primary chancre but VDRL test was negative, dark field microscopy was done to confirm the diagnosis. The patients of latent stage syphilis were diagnosed due to serological positivity in the spouse of the patient of primary or secondary syphilis (refers to patients who gave a positive history or were suffering from primary or secondary syphilis at that time). A few latent syphilitic cases were detected due to some other reason, e.g., routine serologic testing during pregnancy, passport purpose, or blood transfusion. In all the above cases, TPHA test was done to confirm the diagnosis.
RESULTS
Sociodemographic data
A total of 1462 cases attended the STI clinic of PGIMS Rohtak, Haryana from January 2008 to December 2012. Of these, syphilis (91 cases, 6.22%) was found to be the third most common STI after genital warts (514 cases, 35.15%) and herpes simplex infection (493 cases, 33.72%).
As shown in Table 1, the annual distribution of syphilis has showed a decreasing trend from 2008 to 2012 (except an increase from 2008 to 2009) and this decrease was found to be statistically significant (P < 0.001).
Table 1.
Annual distribution and year wise break up of syphilis cases
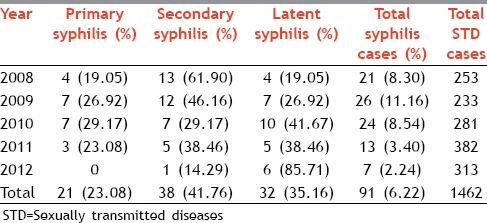
The year wise breakup of primary, secondary, and latent syphilis [Table 1] showed that primary syphilis cases were the least common among all the syphilis cases every year. In 2008 and 2009, secondary syphilis was the most common presentation (61.90% and 46.16% respectively). This difference was most significant in 2008 (P = 0.003). This predominance was substituted by latent syphilis in the later years, that is, 2010-2012 (41.67%, 38.46%, and 85.71%, respectively). In 2012, the incidence of latent syphilis was significantly higher than primary or secondary syphilis (P < 0.001). Overall, secondary syphilis was the most common presentation (41.76%). The change in the trend of primary and secondary syphilis over the years, however, was not statistically significant (P value was 0.61 and 0.11 respectively). But the increase in the incidence of latent syphilis over the last 5 years is statistically significant (P = 0.021).
Of 91 confirmed syphilis cases, 78 were male (85.71%) and 13 (14.29%) were females; the male: female ratio was 6:1. Age of the patients ranged from 18 to 40 years. 41 male patients (52.56%) were married, and of these married patients, 23 patients (56%) gave a history of either pre or extra marital sexual contact. Most of the married females denied any history of pre or extra marital sexual contact (11 cases, 84.62%). 18 males (23.08%) gave a history of visit to commercial sex workers, 3 patients (2 males and one female) (3.30%) gave a history of blood transfusion in the past. 10 male patients (12.82%) were found to be homosexuals.
Agricultural workers (19; 24.36%), students (15; 19.23%), and laborers (9; 11.54%) constituted the majority of patients. Most of the females were housewives (10, 76.92%).
Clinical presentation
The presentations of primary, secondary, and latent syphilis observed in our study is given in Table 2.
Table 2.
Clinical presentation of syphilis
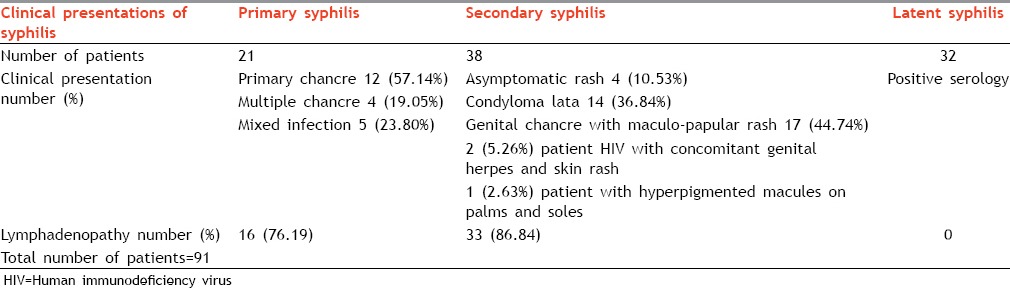
Significantly, 2 patients of secondary syphilis (5.26%) and 4 patients of latent syphilis (12.50%) did not give any history of primary chancre suggesting either syphilis d’emblee or more likely not having noticed the primary lesion due to mild/asymptomatic chancre or hidden chancre, that is, intra meatal or cervical lesion or extragenital lesion.
SEROLOGICAL ASPECTS WITH FALSE POSITIVES
VDRL was reactive in 124 of 1462 STI cases. Of these, 59 cases were symptomatic and 32 cases were asymptomatic. TPHA was reactive in only 91 cases. Thus, 91 (6.22%) cases were diagnosed as confirmed syphilis and 33 (2.25%) cases were considered to be false positives.
Of the 33 false positives, repeat VDRL was negative in 10 patients indicating technical false positives. The remaining 23 patients who showed repeat VDRL positivity were considered to be BFP (1.57%). Respective percentages of BFP's and the associated clinical entities are given in pie diagram [Figure 1].
Figure 1.
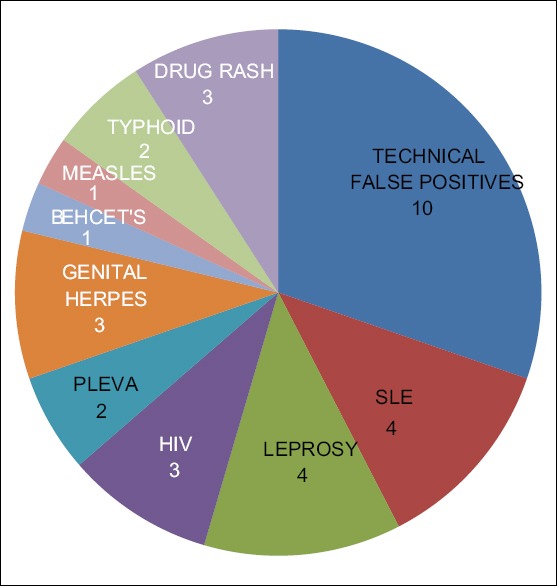
Pie diagram showing biological false positives
VDRL titer ranged from 1:8 to 1:128 in primary syphilis, and 1:32 to 1:256 in secondary and latent syphilis.
HIV seropositivity was seen in 8 patients (8.79%). These included 2 cases of secondary syphilis with concomitant genital herpes, 2 cases with multiple large primary chancres, 1 case with condyloma lata, 2 cases with mixed chancres, and 1 case was with latent syphilis.
DISCUSSION
The socioepidemiological parameters of STIs are dynamic and have seen a definite change over the years. In our study, viral STIs such as genital warts (514 cases, 35.15%) cases were most prevalent, followed by Herpes simplex infection (493 cases, 33.72%) and syphilis (91 cases, 6.22%). This is in accordance with the previous studies on the epidemiological trends of STIs.[8,9,10] The increase in viral STIs may be attributed to greater self-reporting by patients, an apparent increase due to indiscriminate use of broad-spectrum antibiotics which reduces the incidence of bacterial infections, effectiveness of syndromic approach of treatment, and up gradation of health services at the primary level.[8] Viral infections are dominating the Sexually transmitted diseases (STD) world today, but syphilis has maintained its constant prevalence rate.[10] Various studies have shown a rise in the prevalence of syphilis in recent years in India[11] as well as in the Western countries.[12] The annual distribution of syphilis cases showed an increase in incidence from 2008 to 2009; but since then, it has been showing a decreasing trend till December 2012. This decrease in trend of annual syphilis cases from 2008 to 2012 was found to be statistically significant (P < 0.001), unlike the previous studies where the prevalence rate over the years was constant.[10,13] This could be mainly because of ubiquitous use of over the counter antibiotics for every illness.; other contributing factors being condom usage, better reporting of cases, self-awareness and effectiveness of syndromic approach of treatment, which reduce all STIs in general.
In our study, the incidence of primary syphilis increased from 2008 to 2010 but decreased in 2011 and 2012. This change in the trend of primary syphilis over the years, however, was not statistically significant (P = 0.61). The incidence of secondary syphilis has been decreasing from 2008 to 2012 (61.90-14.29%) except a small blip in 2011 (38.46%) (P = 0.11). One peculiar and important finding was the increasing incidence of latent syphilis cases from 19.05% in 2008 to 85.71% in 2012. The increase in the incidence of latent syphilis over the last 5 years is statistically significant (P = 0.021).
The year wise break up of primary, secondary, and latent syphilis showed that primary syphilis cases were the least common among all the syphilis cases every year. In 2008 and 2009, secondary syphilis was the most common presentation (61.90% and 46.16% respectively). This predominance was substituted by latent syphilis in the later years, that is, 2010-2012. In 2012, the incidence of latent syphilis was significantly higher than primary or secondary syphilis (P < 0.001). This is a new finding and has not been adequately highlighted in earlier studies in the literature. This rising trend in latent syphilis cases may be due to increased chance reporting as a result of stricter blood screening protocols, passport documentation, or antenatal checkup in pregnancy (due to increase in the number of hospital deliveries).
In our study, most of the patients were males. This might be due to higher social stigma of reporting to STI clinics in females. The majority of patients were in age group of 18-40 years as has been seen in other studies also[10] and is mainly because of high sexual activity in this age group.
Agricultural workers (19, 24.36%), students (15, 19.23%), and laborers (9, 11.54%) constituted the majority of patients. Most of the females were housewives (10, 76.92%). In another study on the epidemiological profile of STDs conducted in the same center,[9] occupational profile of the patients was found to be more or less similar to our study. This conforms to the rural and agricultural background of the patients in the state of Haryana.
Primary syphilis presented most commonly as the classical single indurated, painless genital chancre in 12 cases (57.14%). A significant percentage presented as mixed chancre and multiple chancres (23.80% and 19.10% respectively). This assumes special importance in the HIV era. Herpes genitalis (9.52%) was the most common presentation accompanying primary chancre in a mixed pattern. This is in accordance with an earlier study[10] and reinforces the fact that a detailed clinical examination and serological investigations are mandatory in all genital ulcer patients so that syphilitic lesions are not missed among the multiple herpetic erosions.
In secondary syphilis, patients presented most commonly with “itchy maculo-papular rash with concomitant primary chancre” in 17 cases (44.74%). This may be due to inadequate treatment in primary stage or faster progression of primary to secondary stage. This was followed by condyloma lata in 36.84% cases. This is in agreement with the findings in other studies.[10,13] It indicates increasing trend of indulgence in abnormal sexual practices such as oro-genital and peno-anal contact. It also indicates increased bacterial load and infectivity of the patients.
In patients of syphilis who were co-infected with HIV, clinical presentations were varied and included secondary syphilis with concomitant genital herpes, multiple large primary chancres, and mixed chancres. These presentations may thus point toward an immune deficient state. Pustular syphilis, reported in another similar study,[10] was not seen in our study. This indicates that syphilis in HIV may have myriad presentations and thus, HIV serology should always be carried out in all patients with suspicion of a STI.
Significantly, 2 patients of secondary syphilis (5.26%) and 4 patients of latent syphilis (12.50%) did not give any history of primary chancre suggesting either syphilis d’emblee or more likely not having noticed the primary lesion due to mild/asymptomatic chancre or hidden chancre, that is, intra meatal or cervical lesion or extragenital lesion. The unwillingness to report the primary lesion due to fear or shame is also a possibility. Hence, firm steps should be taken to increase social awareness for early reporting of the condition.
Serological features
VDRL was reactive in 124 cases out of 1462 STI cases. Out of these, TPHA was reactive in only 91 cases (true positives). Of the 33 false positives, 10 patients were technical false positives. In all the other cases which were BFPs (1.57%) (typhoid with rose spots, lepromatous leprosy, systemic lupus erythematosus, drug rash, HIV, etc.), there may have been nonspecific immune stimulation leading to false serological response to cardiolipin antigen and clinically they mimicked primary or secondary syphilis. In a previous study by Bala et al,[14] the prevalence of BFP reactivity was 0.2% (9/5785).In a Nagpur-based study by Tankhiwale and Naikwade,[15] the proportion of BFP cases was 0.47% (61/13008). The percentage of BFP reactors in the general population was 0.59% in a study from Jamaica.[16] In another study of Saudi Arabia, BFP reactors were detected in 0.5% of the total sera examined (30/6684).[17] The slightly higher percentage of BFP reactors in our study could be attributed to a smaller sample size as compared to the previously mentioned studies. This indicates that depending on the clinical presentation, all cases of VDRL positivity should necessarily undergo TPHA testing whenever possible to rule out false positives. In a previous study by Ray et al,[18] it was shown that TPHA is negative in 25% of the primary syphilis cases and also that there is no significant diagnostic titer for syphilis.[14] Thus, every case with clinical presentation of chancre even with a low VDRL titer should be substantiated with dark field microscopy to avoid misdiagnosis as nonsyphilitic cases.
Thus, the epidemiological trends of syphilis have changed over the years. Latent syphilis is on the rise and is becoming more common than primary or secondary syphilis. The possibility of BFPs should alert the physician about alternate diagnosis and prompts the confirmation of VDRL tests by TPHA whenever possible. Awareness and health care seeking behavior have to be promoted among the public especially women. The importance of such studies thus lies in monitoring the epidemiologic trends of disease and facilitates better prevention and control measures.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Morton RS. The treponematoses. In: Rook A, Wilikinson DS, Ebling FJ, Champion RH, editors. Textbook of Dermatology. 4th ed. London: Blackwell; 1986. pp. 839–83. [Google Scholar]
- 2.Thin RN. Early syphilis in the adult. In: Holmes KK, Mardh PA, Sparling PF, Wiesner PJ, editors. Sexually Transmitted Diseases. 2nd ed. New York: McGraw-Hill; 1990. pp. 221–30. [Google Scholar]
- 3.Sanchez M, Luger AF. Syphilis. In: Fitzpatric TB, Eisen AZ, Wolff K, Freedberg IM, Austen FK, editors. Dermatology in General Medicine. 4th ed. New York: McGraw-Hill; 1993. pp. 2703–43. [Google Scholar]
- 4.Garnett GP, Bowden FJ. Epidemiology and control and curable sexually transmitted diseases: Opportunities and problems. Sex Transm Dis. 2000;27:588–99. doi: 10.1097/00007435-200011000-00007. [DOI] [PubMed] [Google Scholar]
- 5.Kretzschmar M, van Duynhoven YT, Severijnen AJ. Modeling prevention strategies for gonorrhea and Chlamydia using stochastic network simulations. Am J Epidemiol. 1996;144:306–17. doi: 10.1093/oxfordjournals.aje.a008926. [DOI] [PubMed] [Google Scholar]
- 6.Bowden FJ, Garnett GP. The epidemiology and control of Trichomonas vaginalis: Parameterising and analyzing a mathematical model. Sex Transm Infect. 2000;76:248–56. doi: 10.1136/sti.76.4.248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Choudhry S, Ramachandran VG, Das S, Bhattacharya SN, Mogha NS. Pattern of sexually transmitted infections and performance of syndromic management against etiological diagnosis in patients attending the sexually transmitted infection clinic of a tertiary care hospital. Indian J Sex Transm Dis. 2010;31:104–8. doi: 10.4103/2589-0557.74998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dhawan J, Khandpur S. Emerging trends in viral sexually transmitted infections in India. Indian J Dermatol Venereol Leprol. 2009;75:561–5. doi: 10.4103/0378-6323.57715. [DOI] [PubMed] [Google Scholar]
- 9.Jain VK, Dayal S, Aggarwal K, Jain S. Changing trends of sexually transmitted diseases at Rohtak. Indian J Sex Transm Dis. 2008;29:23–5. [Google Scholar]
- 10.Jain A, Mendiratta V, Chander R. Current status of acquired syphilis: A hospital-based 5-year study. Indian J Sex Transm Dis. 2012;33:32–4. doi: 10.4103/2589-0557.93814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ray K, Bala M, Gupta SM, Khunger N, Puri P, Muralidhar S, et al. Changing trends in sexually transmitted disease in a regional STD centre in north India. Indian J Med Res. 2006;124:559–68. [PubMed] [Google Scholar]
- 12.Schumacher CM, Ellen J, Rompalo AM. Changes in demographics and risk behaviors of persons with early syphilis depending on epidemic phase. Sex Transm Dis. 2008;35:190–6. doi: 10.1097/OLQ.0b013e31815a88b0. [DOI] [PubMed] [Google Scholar]
- 13.Kar HK. Incidence of secondary syphilis on rise and need for a separate flow chart for its syndromic management. Indian J Sex Transm Dis. 2004;25:70. [Google Scholar]
- 14.Bala M, Toor A, Malhotra M, Kakran M, Muralidhar S, Ramesh V. Evaluation of the usefulness of Treponema pallidum hemagglutination test in the diagnosis of syphilis in weak reactive Venereal Disease Research Laboratory sera. Indian J Sex Transm Dis. 2012;33:102–6. doi: 10.4103/2589-0557.102117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tankhiwale SS, Naikwade SR. Seroprevalence of syphilis and biologically false positive cases in a tertiary care center. Indian J Dermatol Venereol Leprol. 2014;80:340–1. doi: 10.4103/0378-6323.136911. Tankhiwale SS, Naikwade SR. Seroprevalence of syphilis and biologically false positive cases in a tertiary care center. Indian J Dermatol Venereol Leprol 2014;80:340-1. [DOI] [PubMed] [Google Scholar]
- 16.Smikle MF, James OB, Prabhakar P. Biological false positive serological tests for syphilis in the Jamaican population. Genitourin Med. 1990;66:76–8. doi: 10.1136/sti.66.2.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hossain A. Serological tests for syphilis in Saudi Arabia. Genitourin Med. 1986;62:293–7. doi: 10.1136/sti.62.5.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ray K, Latha R, Sachdeva KG, Ganguly DD, Bhargava NC. Screening and confirmation of syphilis by serology - A five year experience. Indian J Sex Transm Dis. 1991;12:47–50. [Google Scholar]


