Abstract
Background:
Sexually transmitted infections (STIs) increase the risk of transmission of Human Immunodeficiency Virus (HIV) infection causing immense need to understand the patterns of STIs prevailing in the regions of a country for proper planning and implementation of STI control strategies. Due to the lack of adequate laboratory infrastructure in the country, information regarding the profile of STIs relies essentially on syndromic diagnosis.
Aims and Objectives:
To study the pattern of common STIs and the prevalence of HIV infection in patients attending the STI clinic of a tertiary care hospital in northern part of India using a syndromic approach.
Materials and Methods:
A retrospective analysis of data collected from the clinical records of 2700 patients over a period of 21 months (July 2012 to March 2014) was carried out at the Skin and VD Department of SMS Hospital, Jaipur. Detailed history, demographical data, and clinical features were recorded from all the patients. All patients were tested for HIV by ELISA and rapid plasma reagin. STIs were categorized in different syndromes as depicted by National AIDS Control Organization in the syndromic management of STIs. The data collected was analyzed statistically. The proportions were calculated for various syndromes and disease prevalence.
Results:
The overall most common STI was balanoposthitis, followed by genital herpes, vaginal/cervical discharge, molluscum contagiosum, genital warts, nonherpetic genital ulcer disease, lower abdominal pain, and urethral discharge in decreasing order. Among the study population, 2.55% were found to be HIV-positive.
Conclusion:
Viral STIs such as molluscum contagiosum, herpes genitalis, and condylomata acuminata are on the rise among STI/RTI clinic attendees.
Keywords: HIV, sexually transmitted infections, syndromic approach
INTRODUCTION
Sexually transmitted infections (STIs), including Human Immunodeficiency Virus (HIV), continue to present major health, social, and economic problem in the developing world, leading to considerable morbidity, mortality, and stigma.[1] Unprotected sex with an infected partner is by far the most important risk factor for STI/HIV infection.[2,3] They show various trends in different parts of the country and constitute a major public health problem for both developing and developed countries. STIs increases the risk of transmission of HIV infection causing immense need to understand the patterns of STIs prevailing in the regions of a country for proper planning and implementation of STI control strategies. Due to the lack of adequate laboratory infrastructure in the country, information regarding the profile of STIs relies essentially on syndromic diagnosis. The availability of baseline information on the epidemiology of STIs and other associated risk behaviors remain essential for the designing, implementing, and monitoring successful targeted interventions.
Aims and objectives
To study the pattern of common STIs and prevalence of HIV infection in patients attending the STI clinic of a tertiary care hospital in northern part of India using a syndromic approach.
MATERIALS AND METHODS
A retrospective analysis of data collected from the clinical records of 2700 patients over a period of 21 months (July 2012 to March 2014) was carried out.
The data were collected from individuals attending the STI clinic at the Skin and VD Department of SMS Hospital, Jaipur.
Detailed history, demographical data, and clinical features were recorded from all the patients. All patients were tested for HIV by ELISA/rapid tests as recommended by the National AIDS Control Organization (NACO). STIs were categorized in different syndromes as depicted by NACO in the syndromic management of STIs.[4] The syndromes depicted by NACO were urethral discharge, vaginal discharge, genital ulcer disease herpetic and nonherpetic (GUD-H and GUD-NH), inguinal bubo, lower abdominal pain, scrotal swelling, etc. STIs, which were not included in the syndromic management such as molluscum contagiosum, condyloma acuminata, and balanoposthitis were detected clinically. The data collected was analyzed statistically to know the clinico-epidemiological profile. The proportions were calculated for various syndromes and disease prevalence.
RESULTS
In the study population, 78% (2108/2700) were males, 22% (592/2700) were females with male to female ratio being 3.5:1. The majority of patients attending STI clinic belonged to the age group 25-44 years 57.47% (1552/2701), followed by the 20-24 years 20.7% (559/2700), >44 years 15.84% (428/2700), and <20 years 5.92% (161/2700) [Figure 1].
Figure 1.
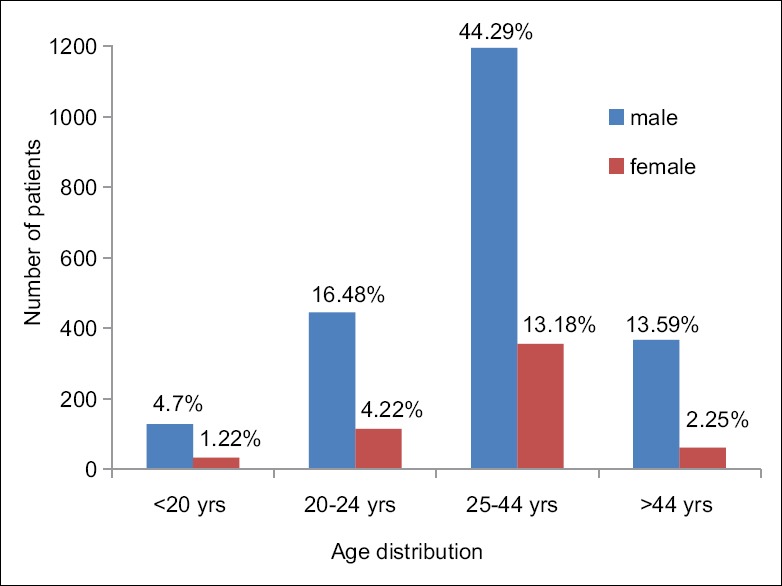
Demographic profile
The overall most common STI was balanoposthitis (39.62%) followed by genital herpes (17.5%), vaginal/cervical discharge (13.4%), genital molluscum (11.74%), genital warts (10.77%), GUD-NH (4.59%), lower abdominal pain (2.66%), and urethral discharge (2.55%) in decreasing order. There were no cases of inguinal bubos [Figure 2].
Figure 2.
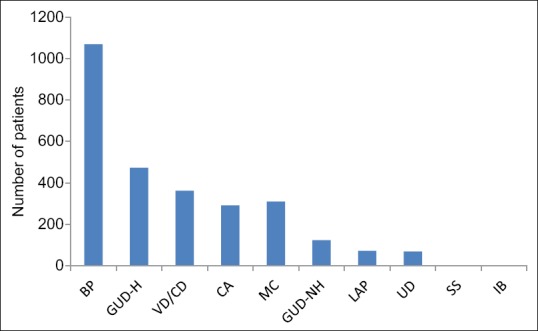
Graph showing diagnosis in the 2700 study cases. Balanoposthitis = BP; genital ulcer disease herpetic = GUD-H; vaginal/ cervical discharge = VD/CD; anogenital warts = CA; molluscum contagiosum = MC; genital ulcer disease nonherpetic = GUD-NH; lower abdominal pain = LAP; urethral discharge = UD; scrotal swelling = SS; inguinal bubo = IB
Among the male patients, balanoposthitis 50.75% (1070/2108) was the most common STI, followed by GUD-H 19.87% (419/2108), condyloma acuminata 12.28% (259/2108), and molluscum contagiosum 9% (190/2108).
In the females, the most common STI was combination of cervical and vaginal discharge 61.04% (362/593) followed by molluscum contagiosum 20.2% (120/593), GUD-H 9.1% (54/593), and condyloma acuminata 5.3% (32/593).
Of the 4.59% (123/2700) patients of GUD-NH, 62.6% (77/123) patients were rapid plasma reagin (RPR) positive with 56 males and 21 female patients.
Among the study population, 2.55% (69/2700) were found to be HIV-positive, in which 84% (58/69) were males and 16% (11/69) were females [Figures 3 and 4].
Figure 3.
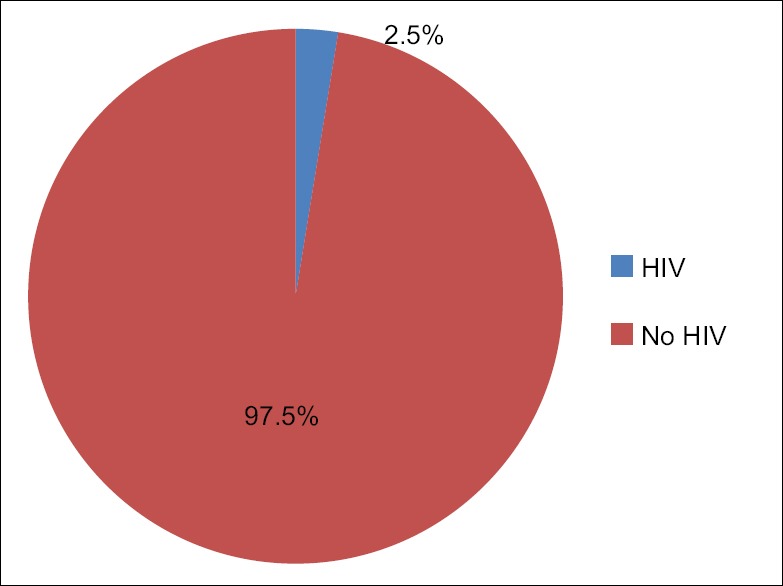
Pie chart showing prevalence of HIV positivity among the STI patients
Figure 4.
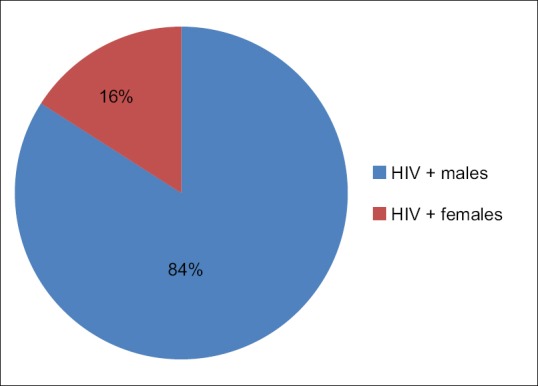
Pie chart showing male and female distribution among HIV positivity patients
DISCUSSION
Sexually transmitted diseases (STDs) are a global health problem of great magnitude. The pattern of STDs differs from country to country and from region to region, especially in large countries such as India.
STI have a tremendous impact on public health. They are responsible for a significant proportion of infertility in both sex, morbidity, economic loss to the family, and increased susceptibility to HIV infection. STI are a major contributor to fetal deaths, abortions, and the delivery of low birth weight babies.[5] STI is not only a medical problem but also causes significant social stigma. Early diagnosis and appropriate treatment will definitely curb the transmission of HIV/AIDS. To achieve this, syndromic approach to STI management came into effect.[6,7] It is an approach where the health care providers diagnose and treat patients on the basis of signs and symptoms (syndrome) rather than specific STIs.
In the present study, males accounted for 78% cases, females were 22% (M: F = 3.5:1), which was almost similar to the north eastern study where males constituted 75.45% and females constituted 24.24% (M: F = 3.09:1).[8] The most common STI was balanoposthitis (39.62%) majority of which were fungal in origin, followed by genital herpes (17.5%), vaginal/cervical discharge (13.4%), genital molluscum (11.74%), genital warts (10.77%), GUD-NH (4.59%), lower abdominal pain (2.66%), and urethral discharge (2.55%) in decreasing order. There were no cases of inguinal bubo. This was in contrast to the north eastern study and study conducted at medical college Trivandrum. In the eastern study, GUD-H (38.1%) was the most common, followed by vaginal/cervical discharge (18.6%), urethral discharge (13.8%), and molluscum contagiosum (4.7%)[8] while in study at Trivandrum, the commonest STD was syphilis, followed by herpes genitalis and condyloma acuminata. HIV was detected in 3.2% of the patients.[9]
Our data compared well with a previous study at a regional STD center in New Delhi were changing trends of the profile of STIs and HIV seropositivity over a 15-year period were analyzed.[10] The STI profile and HIV seropositivity were compared between 1990 and 1993, 1994-1997, 1998-2001, and 2002-2004.[11] Similar to our study, that is, the viral STIs such as molluscum contagiosum, GUD-H, condyloma acuminata, etc., were much more prominent than the bacterial STIs such as urethral discharge and GUD-NH which were more prominent in our institution 10 years back.
In the present study, the prevalence of HIV among STI patients was 2.55% (males - 84%, females - 16%) with male to female ratio being 3.5:1 which was in concordance with the epidemiological analysis of reported AIDS cases where disease is common in males than females, ratio being 3:1.[12] and with the national average (2.5%) as per recent NACO estimates.[13]
There was a wide variation for seropositivity for HIV among STI patients, 8.21% in Zamzachin et al,[14] study, 9.62% in Jaiswal et al,[15] study, 17.2% in Saikia et al,[16] study, and 10.3% in Choudhry et al,[17] study. The prevalence rate in Punjab is 0.32%[18] and 4.2% in the eastern study.[8] This difference could be attributed to the high prevalence of HIV infection and intravenous drug abuse in the North-eastern part of India.
RPR reactivity was seen in 12.8% of the total ulcerative STI patients, which is contrary to the reports of Vora et al, [ 10] and Mewada et al,[19] where the incidence of VDRL reactivity was 19.41% and 53.3%, respectively.
HIV and STIs are perfect examples of epidemiologic synergy as they are core transmitters of each other. The presence of multiple STIs is a risk factor for increased rate of transmission of HIV. This can be controlled by promoting the strategies to reduce high-risk behavior, encouraging condom use, strengthening STI clinics and family health awareness programs, and imparting sex education and awareness regarding STI/HIV among the masses and vulnerable population.
CONCLUSION
Our study showed that the most common presenting complaint of the patients was balanoposthitis (39.62%) followed by genital herpes (17.5%), vaginal/cervical discharge (13.4%), genital molluscum (11.74%), genital warts (10.77%), GUD-NH (4.59%), lower abdominal pain (2.66%), and urethral discharge (2.55%) in decreasing order. Viral STIs such as molluscum contagiosum, herpes genitalis, and condylomata acuminata are on the rise among STI/RTI clinic attendees due to the occurrence of asymptomatic shedding, partial treatment or modified course of the bacterial STDs, thereby leading to apparent reduction in the total number of cases of STDs attending STD clinics, as well as a decrease in the proportion of bacterial to viral STDs.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Marfatia YS, Sharma A, Joshipura SP. Overview of sexually transmitted diseases. In: Valia RG, Valia AR, editors. IADVL Textbook of Dermatology. 3rd ed. Vol. 59. Mumbai: Bhalani Publishing House; 2008. pp. 1766–78. [Google Scholar]
- 2.Aral S, Over M, Manhart L, Holmes KK. Sexually transmitted infections. In: Jamison D, Evans D, Alleyne G, Jha P, Breman J, Measham A, editors. Disease Control Priorities in Developing Countries. Washington D.C: World Bank and Oxford University Press; 2006. pp. 311–30. [PubMed] [Google Scholar]
- 3.UNAIDS AIDS Epidemic Update. Geneva: UNAIDS; 2005. [Google Scholar]
- 4.Operational Guidelines for Programme Managers and Service Providers for Strengthening STI/RTI Services, National AIDS Control Organization, Ministry of Health and Family Welfare. New Delhi: Government of India; 2007. p. 18. [Google Scholar]
- 5.STDs and Pregnancy - CDC Fact Sheet. Center for Disease Control. 2008. [Last accessed on 2009 Aug 23]. Available from: http://www.cdc.gov/std/pregnancy/STD Factact.Pregnancy.htm .
- 6.WHO. Guidelines for the Management of Sexually Transmitted Infection 2001. WHO Site: WHO/HIV_AIDS/2001.01, WHO/RHR/01.10. 2001 [Google Scholar]
- 7.National Guidelines on Prevention, Management and Control of Reproductive Tract Infections, Maternal Health Division NACO, Ministry of Health and Family Welfare. New Delhi: Government of India; 2007. [Google Scholar]
- 8.Sarkar S, Shrimal A, Choudhury SR. Pattern of sexually transmitted infections: A profile from a sexually transmitted infections clinic of a tertiary care hospital of eastern India. Ann Med Health Sci Res. 2013;3:206–9. doi: 10.4103/2141-9248.113663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nair TG, Asha LK, Leelakumari PV. An epidemiological study of sexually transmitted diseases. Indian J Dermatol Venereol Leprol. 2000;66:69–72. [PubMed] [Google Scholar]
- 10.Vora R, Anjaneyan G, Doctor C, Gupta R. Clinico- epidemiological study of sexually transmitted infections in males at a rural-based tertiary care center. Indian J Sex Transm Dis. 2011;32:86–9. doi: 10.4103/2589-0557.85410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Narayanan B. A retrospective study of the pattern of sexually transmitted diseases during a ten-year period. Indian J Dermatol Venereol Leprol. 2005;71:333–7. doi: 10.4103/0378-6323.16784. [DOI] [PubMed] [Google Scholar]
- 12.Lal S. Surveillance of HIV/AIDS. Indian J Community Med. 2003;27:6–9. [Google Scholar]
- 13.NACO. Department of AIDS Control-Ministry of Health and Family Welfare. Current Epidemiological Situations of HIV/AIDS. Annual Report. 2009-2010. [Last accessed on 2011 Aug 13]. Available from: http://www.naco.gov.in/upload/REPORTS/NACO_AR_English%202009-10.pdf .
- 14.Zamzachin G, Singh NB, Devi TB. STD trends in regional institute of medical sciences, Manipur. Indian J Dermatol Venereol Leprol. 2003;69:151–3. [PubMed] [Google Scholar]
- 15.Jaiswal AK, Banerjee S, Matety AR, Grover S. Changing trends in sexually transmitted diseases in North Eastern India. Indian J Dermatol Venereol Leprol. 2002;68:65–6. [PubMed] [Google Scholar]
- 16.Saikia L, Nath R, Deuori T, Mahanta J. Sexually transmitted diseases in Assam: An experience in a tertiary care referral hospital. Indian J Dermatol Venereol Leprol. 2009;75:329. doi: 10.4103/0378-6323.51245. [DOI] [PubMed] [Google Scholar]
- 17.Choudhry S, Ramachandran VG, Das S, Bhattacharya SN, Mogha NS. Characterization of patients with multiple sexually transmitted infections: A hospital-based survey. Indian J Sex Transm Dis. 2010;31:87–91. doi: 10.4103/2589-0557.74978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Punjab State AIDS Control Society. Overview of HIV/AIDS in Punjab (Till July 2012) [Last cited on 2012 Aug 22]. Available from: http://www.punjabsacs.org/OverViewHIV.aspx .
- 19.Mewada B, Kotia N, Marfatia YS. Role of VDRL in syndromic management of sexually transmitted diseases. Indian J Sex Transm Dis. 2000;21:38–40. [Google Scholar]


