Sir,
Bowenoid papulosis (BP) is caused by human papilloma virus (HPV) characterized by papular lesions on the genitalia in the sexually active age group. Although it generally runs a benign course with spontaneous regression within several months, sometimes it can turn malignant. Histopathology reveals characteristic dysplastic changes. We describe a case with lesions on the pubic area and penis.
A 41-year-old male presented with asymptomatic lesions over the pubic region for past 8-10 months. He was married for the past 15 years with a history of single unprotected premarital sexual contact with a known person. Multiple hyperpigmented papules, some verrucous, were present over the pubic region and shaft of penis Figure 1. A diagnosis of BP was considered. Biopsy of the papule showed acanthotic epidermis Figure 2 and mild dysplastic features with anisonucleosis, nuclear enlargement, and increased mitosis [Figure 3] with mild dermal perivascular infiltrate. DNA-polymerase chain reaction (PCR) markers for HPV strains 16 and 18 were negative. The patient was treated with 5% imiquimod cream.
Figure 1.

Bowenoid papulosis on the genitalia
Figure 2.
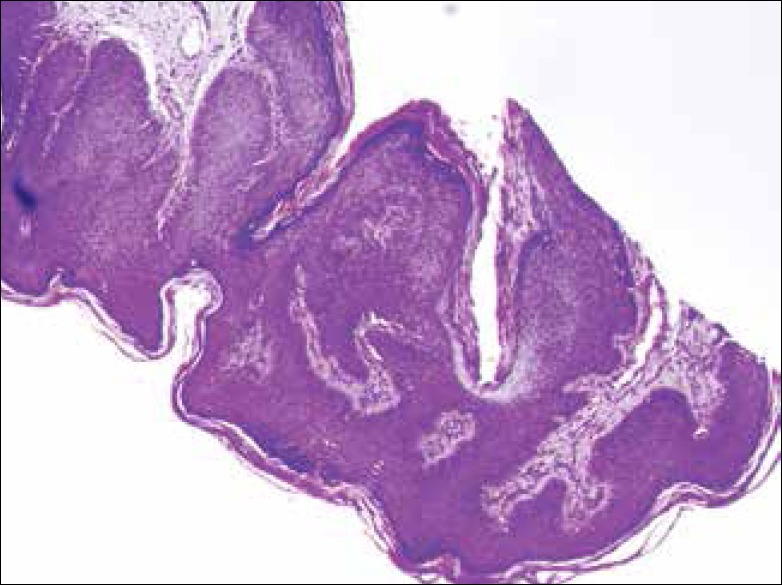
Papillomatous and acanthotic stratified squamous epithelium (H and E, ×40)
Figure 3.
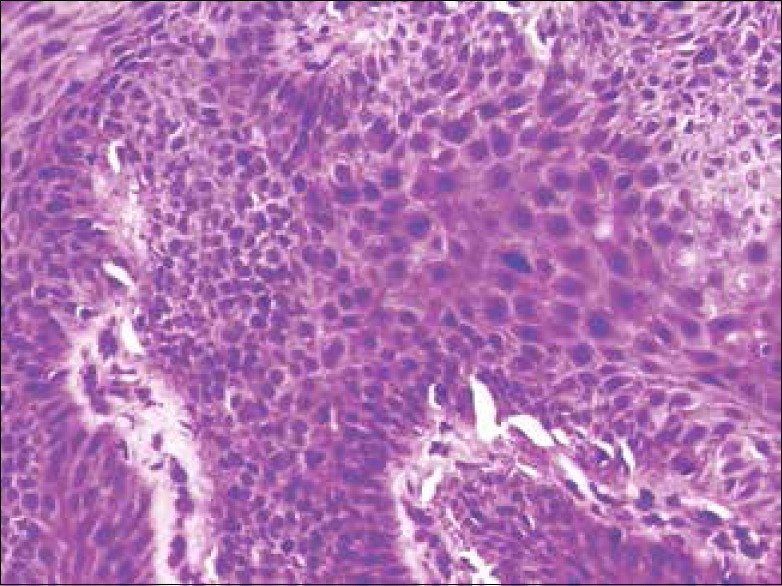
Photomicrograph showing dysplastic squamous epithelium (H and E, ×200)
BP was first described by Lloyd but described as an entity by Kopf et al Although HPV 16 is considered as the causative agent other HPV serotypes such as 18, 31, 33, 39, and 52 have also been implicated of which 16, 18, and 33 are the most oncogenic strains.[1] However in our patient, PCR for HPV was negative.
Clinically the lesions are pigmented ranging in size from 0.2 to 3 mm resembling persistent warts. The most frequent sites affected are the penis and vulva but sometimes other areas such as oral, periungual, and neck[2] may be involved. In females, it is referred to as multifocal vulvar intraepithelial neoplasia. Lesions should be differentiated from genital warts, lichen planus, molluscum contagiosum, seborrheic keratosis, and Bowen's disease. BP is considered as a transitional stage between genital warts and squamous carcinoma in situ. The multiplicity of lesions and the younger age differentiate it from Bowen's disease. As in condyloma acuminatum, increased expression of PPAR - gamma and COX-2 receptors has been demonstrated in BP too.[3] Histologic differentiation of BP from Bowen's disease may be difficult, sometimes impossible. The classical histopathological features include full thickness epidermal atypia, loss of architecture, intact basement membrane with koilocytotic, dyskeratotic cells, and metaphase mitoses.[4]
The natural history of the disease is not well known. It usually runs a long course but spontaneously resolves. Transformation to invasive carcinoma is rare occurring in <1% of cases, especially in immunocompromised.[5] Treatment should be conservative using modalities such as electrofulguration, cryotherapy, scissors excision, topical application of 5-fluoruracil or 5% imiquimod, intralesional recombinant alpha - 2 interferon, photodynamic therapy, and CO2 laser vaporization.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Yoneta A, Yamashita T, Jin HY, Iwasawa A, Kondo S, Jimbow K. Development of squamous cell carcinoma by two high-risk human papillomaviruses (HPVs), a novel HPV-67 and HPV-31 from bowenoid papulosis. Br J Dermatol. 2000;143:604–8. doi: 10.1111/j.1365-2133.2000.03718.x. [DOI] [PubMed] [Google Scholar]
- 2.Johnson TM, Saluja A, Fader D, Blum D, Cotton J, Wang TS, et al. Isolated extragenital bowenoid papulosis of the neck. J Am Acad Dermatol. 1999;41(5 Pt 2):867–70. doi: 10.1016/s0190-9622(99)70355-5. [DOI] [PubMed] [Google Scholar]
- 3.Ni J, Zhang YZ, Xue SL. The expressions of PPAR-gamma, COX-2 in the lesions of patients with condyloma acuminatum and bowenoid papulosis. Sichuan Da Xue Xue Bao Yi Xue Ban. 2009;40:439–41. [PubMed] [Google Scholar]
- 4.Weedon D, Strutton G. Skin Pathology. 2nd ed. London: Churchill Livingstone; 2002. Viral diseases; p. 705. [Google Scholar]
- 5.von Krogh G, Horenblas S. Diagnosis and clinical presentation of premalignant lesions of the penis. Scand J Urol Nephrol Suppl. 2000;(Suppl. 205):201–14. doi: 10.1080/00365590050509931. [DOI] [PubMed] [Google Scholar]


