Abstract
Acute myocardial infarction (AMI) is a major cause of morbidity and mortality worldwide. The highest risk of fatality occurs within the initial hours of onset of AMI. Thus, early diagnosis of cardiac ischemia is critical for the effective management of patients with AMI. Improper diagnosis of patients with chest pain often leads to inappropriate admission of patients without AMI and vice versa. In addition to clinical history, physical examination, accurate electrocardiogram findings and assessment of cardiac biomarkers have an important role in the early diagnosis of acute ischemia. The present review discusses in detail the various cardiac biomarkers released during the event of an AMI.
Keywords: acute myocardial infarction, electrocardiogram, atherosclerosis, biomarkers
1. Introduction
In the early 1970s, the World Health Organization (WHO) had defined the term myocardial infarction by the presence of 2 of the 3 following characteristics (1,2): i) Symptoms of acute ischemia (chest pain), ii) development of Q waves in electrocardiogram (ECG) and iii) increase of enzymes in the blood [combination of total creatine kinase (CK), CK-myocardial band (MB), aspartate aminotransferase (AST) and lactate dehydrogenase (LDH)]. However, in 1999, the Joint European Society of Cardiology and the American College of Cardiology Committee jointly proposed the new definition for myocardial infarction, emphasizing the importance of sensitive and serological biomarkers for the diagnosis of acute myocardial infarction (AMI), and introduced cardiac troponins (cTn) as the gold standard (3) (Fig. 1).
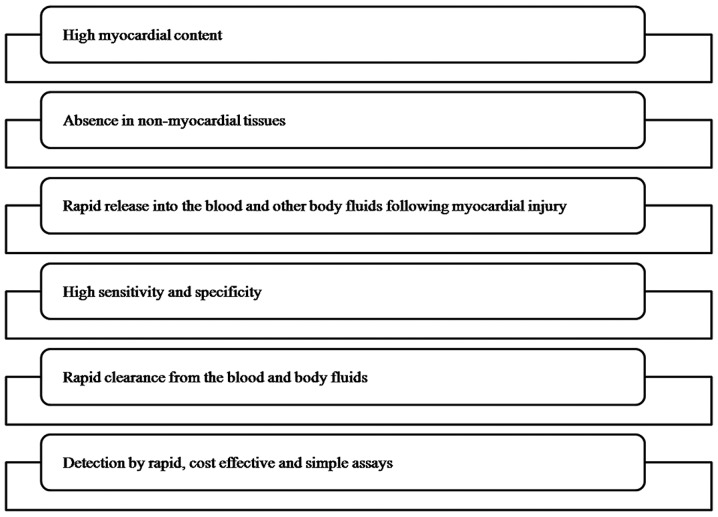
Figure 1.
Characteristics of an ideal cardiac biomarker.
2. Biomarkers of myocardial infarction
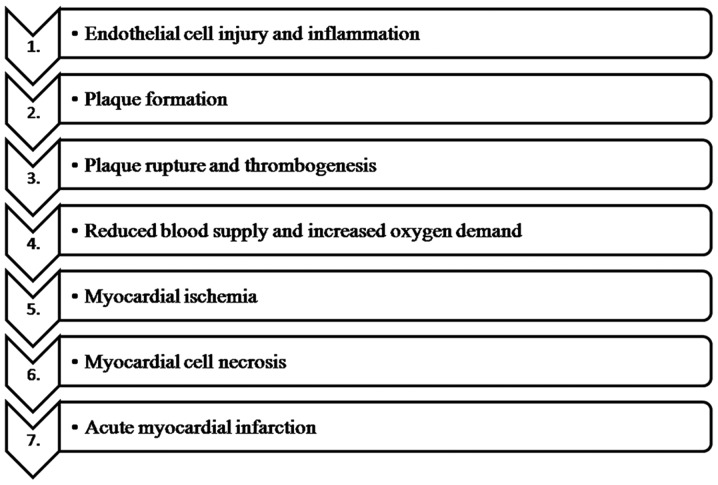
Myocardial infarction is defined as myocardial cell death due to prolonged ischemia (4). Myocardial cell death does not occur immediately following the onset of myocardial ischemia, but occurs ≥6 h. Atherosclerosis is by far the most common cause of myocardial infarction. The major risk factors of atherosclerosis are hyperlipidemia, diabetes, smoking, hypertension, gender and age. Endothelial dysfunction and inflammation have a major role in the initiation of the atherosclerotic plaque formation (5,6). Atherosclerosis is characterized by lipid accumulation in the vessel walls leading to the formation of an atherosclerotic plaque consisting of a central lipid core surrounded by foamy macrophages and smooth muscle cells covered by a fibrous cap (7). Rupture of the fibrous cap leads to communication between the lipid content of the plaque and the blood flowing through the arterial lumen (8). The tissue factor expressed by the macrophages activates the platelets eventually leading to the formation of intraluminal thrombus (9,10). Finally occlusion of the coronary artery by the thrombus reduces the blood supply to the myocardial tissues leading to ischemia and necrosis, eventually causing myocardial infarction (11) (Fig. 2).
Figure 2.
Schematic representation of the pathogenesis of myocardial infarction.
Rapid identification of AMI is mandatory to initiate effective treatment for better prognosis. The newer concept of diagnosis of AMI emphasizes the importance of the 12-lead ECG and the assessment of early cardiac biomarkers since ECG by itself is often inadequate to diagnose AMI (Table I).
Table I.
Biomarkers of myocardial infarction.
| Type | Marker |
|---|---|
| Obsolete | Aspartate aminotransferase |
| Total CK | |
| Lactate dehydrogenase | |
| Established | Troponin T |
| Troponin I | |
| Myocardial fraction of CK | |
| Myoglobin | |
| Emerging | Heart fatty acid-binding protein |
| B-type natriuretic peptide | |
| Ischemia-modified albumin | |
| Pregnancy-associated plasma protein A | |
| Copeptin | |
| Growth differentiation factor-15 |
CK, creatine kinase.
In the year 1954, AST was the first cardiac biomarker to be used. AST is found in the liver, heart, skeletal muscles, brain and kidneys. Due to its lack of specificity to the cardiac tissue it is no longer used for the diagnosis of AMI (12,13). In the year 1959, the total CK level was assessed for AMI, as it was a good indicator of skeletal muscle injury (14). Following this, in the year 1960, LDH was used for diagnosis of AMI (15). Finally in the year 1979, WHO recommended the panel of CK, AST and LDH for the diagnosis of AMI (2).
However, the assessment of the cardiac biomarkers was revolutionized in the year 1980 after the development of immunoassays (16).
3. Inflammatory markers
C-reactive protein (CRP)
CRP is an acute phase protein secreted by the hepatocytes during an inflammatory stimulus (17). In addition to being an inflammatory marker, CRP has a pro-inflammatory effect causing expression of adhesion molecules and inflammatory cells (18). It has been shown that CRP is increased in patients with unstable angina; however, owing to lack of sensitivity and specificity, it cannot be used as a diagnostic marker (19). As a prognostic indicator, high CRP levels have also been associated with poor outcome (20).
Pentraxin 3 (PTX-3)
PTX-3 of the PTX family is a specific marker of vascular inflammation produced by the vascular endothelial cells, vascular smooth muscle cells, macrophages, and neutrophils in response to an inflammatory stimulus (21). The PTX-3 level has been proposed as a prognostic biomarker of adverse outcome in patients with unstable angina pectoris, myocardial infarction and heart failure (22,23). However, as opposed to CRP, PTX-3 predicts advanced atherosclerosis and is more specific for vessel wall inflammation (24).
Interleukin (IL)-6
Another marker of early atherosclerosis is IL-6, which has a major role in the recruitment and activation of inflammatory cells in response to ischemia and further during the reperfusion of the infarcted myocardium (25). In addition, it stimulates the liver to produce the acute phase protein, CRP (26). Thus, an elevated serum level of IL-6 and CRP are associated with the development of atherosclerosis and additionally to the development of type II diabetes in insulin-resistant individuals (27).
4. Plaque destabilization markers
Myeloperoxidase (MPO)
MPO is a metalloproteinase produced by the polymorphonuclear leukocytes and macrophages. It initiates the production of reactive oxygen species that are important for the development of atheroma and plaque rupture (28). Thus, an increased level of MPO is a marker of plaque instability (29). Furthermore, it serves as a predictive marker for future cardiovascular adverse events (30).
Pregnancy-associated plasma protein A (PAPPA)
PAPPA is also a metalloproteinase that has an active role during the rupture of an atherosclerotic plaque (31). It is primarily produced by the syncytiotrophoblasts of the placenta, as well as by the fibroblasts, vascular endothelial cells and vascular smooth muscle cells. In atherosclerosis, it has been associated with plaque progression and instability (32).
Soluble cluster of differentiation 40 ligand (sCD40L)
sCD40L of the tumor necrosis factor-α (TNF-α) family is upregulated on the platelets located in the intraluminal thrombus. The activation of the inflammatory and coagulant pathways during thrombogenesis causes the release of CD40L into the circulation, thus indicating plaque rupture and subsequent myocardial infarction (33).
TNF-α
TNF-α is a pleiotropic cytokine produced by the endothelial cells, smooth muscle cells and macrophages. TNF-α levels are markedly elevated in advanced heart failure (34). The role of TNF-α in atherosclerosis is the production of tissue inhibitors of metalloproteinases by the fibroblasts. Thus, the production of excess amounts of metalloproteinases causes rupture of the atheromatous plaque (35). Additionally, it can stimulate the synthesis of IL-6 by the smooth muscle cells. This confirms the role of TNF-α in the regulation of the inflammatory cascade. Thus, elevated levels of TNF-α are indicative of recurrent non-fatal myocardial infarction or a fatal cardiovascular event (36).
5. Myocardial necrosis markers
Troponins
The troponins are a complex of 3 protein subunits, namely troponin C, troponin T and troponin I, located on the thin filaments of the skeletal and cardiac muscle fibers. Troponin C is the calcium-binding component, troponin T is the tropomyosin-binding component and troponin I is the inhibitory component. As the isoforms of troponin C is identical in the skeletal and cardiac muscle, troponin C is not extremely specific for myocardial injury (37,38). The isoforms of troponin T and troponin I differ in the skeletal and the cardiac muscle, and thus are extremely specific for cardiac tissue necrosis (39). Troponin T is present chiefly in the bound form to the contractile elements of the myocardial cells; however, it is also present free in the cytoplasm. Troponin T exhibits a dual release initially of the cytoplasmic component and later of the bound component (40). Troponin I is extremely specific for the cardiac muscle and has not been isolated from the skeletal muscle. This absolute specificity makes it an ideal marker of myocardial injury (41). They are released into the circulation 6–8 h after myocardial injury, peak at 12–24 h and remain elevated for 7–10 days (42). The only disadvantage of cTn is the late clearance that makes it difficult to identify a recurrent myocardial infarction.
Myoglobin (MYO)
MYO is a small cytoplasmic oxygen-binding protein found in the skeletal as well as the cardiac muscle. It is released extremely early into the serum, 1 h after the onset of myocardial injury, peaks at 4–12 h and returns to baseline values immediately (43,44). The major disadvantage of MYO is the lack of specificity to the cardiac tissue due to the presence of large amounts of MYO in the skeletal muscle (45). The levels of MYO can therefore not be used as a single diagnostic marker, but in conjunction with the troponins or CK-MB. Thus, serum levels of MYO can be used to rule out, rather than diagnose, myocardial infarction (46).
CK and CK-MB
CK was first indicated as a cardiac biomarker in the year 1979. CK is an enzyme that is found primarily in the cardiac muscle and skeletal muscle. This enzyme has 3 isoenzymes: MM, MB and BB. CK-MM is the skeletal muscle fraction, CK-MB is the cardiac muscle fraction and CK-BB is the brain fraction of the total CK (47). Previously, the total CK was assessed for myocardial infarction. However, as the total CK contains 95% of the CK-MM fraction, recent concepts have proposed the use of the relative index score (RI) as follows (48).
The CK-MB rises in the serum at 4–9 h after the onset of chest pain, peaks ~24 h and returns to baseline values at 48–72 h. The one advantage of CK-MB over the troponins is the early clearance that helps in the detection of reinfarction. Thus, the serum level of troponin along with the level of the CK-MB fraction is assessed for the diagnosis of myocardial infarction (49).
Heart fatty acid-binding protein (H-FABP)
H-FABP is a small cytosolic low molecular weight protein found in the cardiac tissues that are responsible for the transport of fatty acids from the plasma membrane to sites of β-oxidation in mitochondria and peroxisomes, and to the endoplasmic reticulum for lipid synthesis (50). It is chiefly present in the myocardium and, to a lesser extent, in the brain, kidney and skeletal muscle. H-FABP is released extremely early into the serum following myocyte rupture (51). An increased concentration of H-FABP appears as early as 30 min after myocardial injury, peaks at 6–8 h and returns to baseline levels at ~24 h (52). Additionally, H-FABP can be used as a predictive biomarker of mortality following acute coronary syndrome (ACS) (53).
B-type natriuretic peptide (BNP)
BNP is a neurohormone released from the cardiac cells. Studies have shown that elevated BNP is a predictive marker of death and heart failure. However, they are not useful for the diagnosis of AMI (54).
Ischemia-modified albumin (IMA)
Under ischemic conditions, the level of IMA in the blood is significantly increased, thus aiding in the diagnosis of acute ischemia prior to the onset of myocardial necrosis (55). The measurement of IMA is enabled by the binding of the cobalt to the damaged N-terminus of the albumin. The increase in IMA levels occurs immediately after the onset of ischemia and returns to baseline values within 6–12 h, thus enabling early identification of ischemia (56).
Growth-differentiation factor-15 (GDF-15)
GDF-15 is a member of the transforming growth factor-β family of cytokines that is primarily expressed by the placenta; however, under abnormal conditions, it can be expressed by various tissues (57). During cardiac ischemia, the level of GDF-15 is increased favoring diagnosis of ACS (58). However, owing to its lack of specificity, it can be used as a predictive marker of mortality rather than a diagnostic marker following ACS (59).
Copeptin
Copeptin, the C-terminal portion of provasopressin is cosecreted with vasopressin. Copeptin is secreted extremely early in the course of an AMI from the pituitary (60). Copeptin levels are significantly increased within minutes in patients with AMI. Thus, copeptin can be used as a diagnostic and prognostic marker of myocardial injury (61).
F2 isoprostanes
F2 isoprostanes are products of arachidonic acid metabolism. During atherosclerosis, the F2 isoprostanes are secreted by a variety of cells including the monocytes. Studies have shown that the F2 isoprostane level is increased in the urine of patients with unstable angina. Additionally, it can be used as a predictive marker of complications in non-fatal myocardial infarction, development of heart failure and fatality (62).
6. Salivary biomarkers associated with myocardial necrosis
Saliva offers an easy, simple and non-invasive screening procedure for various systemic diseases. Whole saliva contains constituents from serum, gingival crevicular fluid and oral mucosal transudate making it a valuable diagnostic tool. Salivary markers of acute myocardial infarction include MYO, CRP, MPO, CK-MB and cTn, which when used in combination with an ECG, shows a positive correlation in patients when compared to healthy controls (63). The salivary MYO levels were found to be significantly higher within 48 h of onset of chest pain in AMI patients and correlated positively with its serum concentration (64). In a study performed by Miller et al (65), the salivary concentrations of CRP, TNF-α, matrix metalloproteinase-9 (MMP-9) and MPO were significantly higher in patients with AMI and correlated positively with the serum concentrations. Studies reveal that salivary soluble intracellular adhesion molecule 1 is significantly elevated in AMI patients; however, levels of salivary sCD40L were significantly lowered in AMI patients. In a study performed by Foley et al (66), salivary levels of troponin I and CRP correlated with the serum levels in patients with myocardial injury. Additionally, levels of MMP-9 and MPO in saliva correlated with its serum levels (67). Thus, these studies suggest that saliva can be used as an alternative to serum in the diagnosis of myocardial infarction (68).
7. Conclusion
The analysis of cardiac biomarkers has become the frontline diagnostic tools for AMI, and has greatly enabled the clinicians in the rapid diagnosis and prompt treatment planning, thereby reducing the mortality rate to a great extent. However, the future of cardiac biomarkers will follow the analysis of a panel of markers for the diagnosis and prognosis of myocardial infarction.
Abbreviations
- AMI
acute myocardial infarction
- AST
aspartate aminotransferase
- CK
creatine kinase
- LDH
lactate dehydrogenase
- CRP
C-reactive protein
- PTX-3
pentraxin 3
- MPO
myeloperoxidase
- PAPPA
pregnancy-associated plasma protein A
- TNF-α
tumor necrosis factor-α
- CK-MB
creatine kinase myocardial band
- H-FABP
heart fatty acid-binding protein
- BNP
B-type natriuretic peptide
- IMA
ischemia-modified albumin
- GDF-15
growth-differentiation factor-15
- ACS
acute coronary syndrome
- MYO
myoglobin
- MMP-9
matrix metalloproteinase-9
References
- 1.World Health Organization (WHO) working group, corp-author. The establishment of ischaemic heart disease registers (report of the fifth working group) WHO Reg Publ Eur Ser, Copenhagen. 1972;821(suppl 5) [Google Scholar]
- 2.Task force, corp-author. Nomenclature and criteria for diagnosis of ischemic heart disease. Report of the Joint International Society and Federation of Cardiology/World Health Organization task force on standardization of clinical nomenclature. Circulation. 1979;59:607–609. doi: 10.1161/01.CIR.59.3.607. [DOI] [PubMed] [Google Scholar]
- 3.Alpert JS, Thygesen K, Antman E, et al. Myocardial infarction redefined - a consensus document of The Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction. J Am Coll Cardiol. 2000;36:959–969. doi: 10.1016/S0735-1097(00)00804-4. [DOI] [PubMed] [Google Scholar]
- 4.Jennings RB, Reimer KA. Factors involved in salvaging ischemic myocardium: Effect of reperfusion of arterial blood. Circulation. 1983;68:I25–I36. [PubMed] [Google Scholar]
- 5.Cunningham KS, Gotlieb AI. The role of shear stress in the pathogenesis of atherosclerosis. Lab Invest. 2005;85:9–23. doi: 10.1038/labinvest.3700299. [DOI] [PubMed] [Google Scholar]
- 6.Libby P, Ridker PM, Maseri A. Inflammation and atherosclerosis. Circulation. 2002;105:1135–1143. doi: 10.1161/hc0902.104353. [DOI] [PubMed] [Google Scholar]
- 7.Watanabe T, Tokunaga O, Fan JL, Shimokama T. Atherosclerosis and macrophages. Acta Pathol Jpn. 1989;39:473–486. doi: 10.1111/j.1440-1827.1989.tb01513.x. [DOI] [PubMed] [Google Scholar]
- 8.Virmani R, Kolodgie FD, Burke AP, Finn AV, Gold HK, Tulenko TN, Wrenn SP, Narula J. Atherosclerotic plaque progression and vulnerability to rupture: Angiogenesis as a source of intraplaque hemorrhage. Arterioscler Thromb Vasc Biol. 2005;25:2054–2061. doi: 10.1161/01.ATV.0000178991.71605.18. [DOI] [PubMed] [Google Scholar]
- 9.Butenas S, Undas A, Gissel MT, Szuldrzynski K, Zmudka K, Mann KG. Factor XIa and tissue factor activity in patients with coronary artery disease. Thromb Haemost. 2008;99:142–149. doi: 10.1160/TH07-08-0499. [DOI] [PubMed] [Google Scholar]
- 10.Furie B, Furie BC. Mechanisms of thrombus formation. N Engl J Med. 2008;359:938–949. doi: 10.1056/NEJMra0801082. [DOI] [PubMed] [Google Scholar]
- 11.Kawai C. Pathogenesis of acute myocardial infarction. Novel regulatory systems of bioactive substances in the vessel wall. Circulation. 1994;90:1033–1043. doi: 10.1161/01.CIR.90.2.1033. [DOI] [PubMed] [Google Scholar]
- 12.Dolci A, Panteghini M. The exciting story of cardiac biomarkers: From retrospective detection to gold diagnostic standard for acute myocardial infarction and more. Clin Chim Acta. 2006;369:179–187. doi: 10.1016/j.cca.2006.02.042. [DOI] [PubMed] [Google Scholar]
- 13.Ladenson JH. A personal history of markers of myocyte injury (myocardial infarction) Clin Chim Acta. 2007;381:3–8. doi: 10.1016/j.cca.2007.02.039. [DOI] [PubMed] [Google Scholar]
- 14.Ruzich RS. Cardiac enzymes. How to use serial determinations to confirm acute myocardial infarction. Postgrad Med. 1992;92(92):85–89. doi: 10.1080/00325481.1992.11701533. [DOI] [PubMed] [Google Scholar]
- 15.Lee TH, Goldman L. Serum enzyme assays in the diagnosis of acute myocardial infarction. Recommendations based on a quantitative analysis. Ann Intern Med. 1986;105:221–233. doi: 10.7326/0003-4819-105-2-221. [DOI] [PubMed] [Google Scholar]
- 16.Imteyaz Ahmad M, Neera Sharma. Biomarkers in acute myocardial infarction. J Clin Exp Cardiolog. 2012;3:11. [Google Scholar]
- 17.DeServi S, Mariani M, Mariani G, Mazzone A. C-reactive protein increase in unstable coronary disease cause or effect? J Am Coll Cardiol. 2005;46:1496–1502. doi: 10.1016/j.jacc.2005.05.083. [DOI] [PubMed] [Google Scholar]
- 18.Lindahl B, Toss H, Siegbahn A, Venge P, Wallentin L. Markers of myocardial damage and inflammation in relation to long-term mortality in unstable coronary artery disease. FRISC Study Group. Fragmin during Instability in Coronary Artery Disease. N Engl J Med. 2000;343:1139–1147. doi: 10.1056/NEJM200010193431602. [DOI] [PubMed] [Google Scholar]
- 19.Duffy JR, Salerno M. New blood test to measure heart attack risk: C-reactive protein. J Cardiovasc Nurs. 2004;19:425–429. doi: 10.1097/00005082-200411000-00016. [DOI] [PubMed] [Google Scholar]
- 20.deWinter RJ, Bholasingh R, Lijmer JG, Koster RW, Gorgels JP, Schouten Y, Hoek FJ, Sanders GT. Independent prognostic value of C-reactive protein and troponin I in patients with unstable angina or non-Q-wave myocardial infarction. Cardiovasc Res. 1999;42:240–245. doi: 10.1016/S0008-6363(99)00018-8. [DOI] [PubMed] [Google Scholar]
- 21.Inoue K, Sugiyama A, Reid PC, Ito Y, Miyauchi K, Mukai S, Sagara M, Miyamoto K, Satoh H, Kohno I, et al. Establishment of a high sensitivity plasma assay for human pentraxin3 as a marker for unstable angina pectoris. Arterioscler Thromb Vasc Biol. 2007;27:161–167. doi: 10.1161/01.ATV.0000252126.48375.d5. [DOI] [PubMed] [Google Scholar]
- 22.Latini R, Maggioni AP, Peri G, Gonzini L, Lucci D, Mocarelli P, Vago L, Pasqualini F, Signorini S, Soldateschi D, et al. Lipid Assessment Trial Italian Network (LATIN) Investigators: Prognostic significance of the long pentraxin PTX3 in acute myocardial infarction. Circulation. 2004;110:2349–2354. doi: 10.1161/01.CIR.0000145167.30987.2E. [DOI] [PubMed] [Google Scholar]
- 23.Suzuki S, Takeishi Y, Niizeki T, Koyama Y, Kitahara T, Sasaki T, Sagara M, Kubota I. Pentraxin 3, a new marker for vascular inflammation, predicts adverse clinical outcomes in patients with heart failure. Am Heart J. 2008;155:75–81. doi: 10.1016/j.ahj.2007.08.013. [DOI] [PubMed] [Google Scholar]
- 24.Knoflach M, Kiechl S, Mantovani A, Cuccovillo I, Bottazzi B, Xu Q, Xiao Q, Gasperi A, Mayr A, Kehrer M, et al. Pentraxin-3 as a marker of advanced atherosclerosis results from the Bruneck, ARMY and ARFY Studies. PLoS One. 2012;7:e31474. doi: 10.1371/journal.pone.0031474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Karpiński L, Płaksej R, Kosmala W, Witkowska M. Serum levels of interleukin-6, interleukin-10 and C-reactive protein in relation to left ventricular function in patients with myocardial infarction treated with primary angioplasty. Kardiol Pol. 2008;66:1279–1285. [PubMed] [Google Scholar]
- 26.Baumann H, Gauldie J. Regulation of hepatic acute phase plasma protein genes by hepatocyte stimulating factors and other mediators of inflammation. Mol Biol Med. 1990;7:147–159. [PubMed] [Google Scholar]
- 27.Pradhan AD, Manson JE, Rifai N, Buring JE, Ridker PM. C-Reactive protein, Interleukin-6 and risk of developing type 2 diabetes mellitus. JAMA. 2001;286:327–334. doi: 10.1001/jama.286.3.327. [DOI] [PubMed] [Google Scholar]
- 28.Khan SQ, Kelly D, Quinn P, Davies JE, Ng LL. Myeloperoxidase aids prognostication together with N-terminal pro-B-type natriuretic peptide in high-risk patients with acute ST elevation myocardial infarction. Heart. 2007;93:826–831. doi: 10.1136/hrt.2006.091041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wang J, Zhang S, Jin Y, Qin G, Yu L, Zhang J. Elevated levels of platelet-monocyte aggregates and related circulating biomarkers in patients with acute coronary syndrome. Int J Cardiol. 2007;115:361–365. doi: 10.1016/j.ijcard.2006.03.019. [DOI] [PubMed] [Google Scholar]
- 30.Cavusoglu E, Ruwende C, Eng C, Chopra V, Yanamadala S, Clark LT, Pinsky DJ, Marmur JD. Usefulness of baseline plasma myeloperoxidase levels as an independent predictor of myocardial infarction at two years in patients presenting with acute coronary syndrome. Am J Cardiol. 2007;99:1364–1368. doi: 10.1016/j.amjcard.2006.12.060. [DOI] [PubMed] [Google Scholar]
- 31.BayesGenis A, Conover CA, Overgaard MT, Bailey KR, Christiansen M, Holmes DR, Jr, Virmani R, Oxvig C, Schwartz RS. Pregnancy-associated plasma protein A as a marker of acute coronary syndromes. N Engl J Med. 2001;345:1022–1029. doi: 10.1056/NEJMoa003147. [DOI] [PubMed] [Google Scholar]
- 32.Lund J, Qin QP, Ilva T, Nikus K, Eskola M, Porela P, Kokkala S, Pulkki K, Pettersson K, Voipio-Pulkki LM. Pregnancy-associated plasma protein A: A biomarker in acute ST-elevation myocardial infarction (STEMI) Ann Med. 2006;38:221–228. doi: 10.1080/07853890500525883. [DOI] [PubMed] [Google Scholar]
- 33.Heeschen C, Dimmeler S, Hamm CW, van den Brand MJ, Boersma E, Zeiher AM, Simoons ML. CAPTURE Study Investigators: Soluble CD40 ligand in acute coronary syndromes. N Engl J Med. 2003;348:1104–1111. doi: 10.1056/NEJMoa022600. [DOI] [PubMed] [Google Scholar]
- 34.Levine B, Kalman J, Mayer L, Fillit HM, Packer M. Elevated circulating levels of tumor necrosis factor in severe chronic heart failure. N Engl J Med. 1990;323:236–241. doi: 10.1056/NEJM199007263230405. [DOI] [PubMed] [Google Scholar]
- 35.Shingu M, Nagai Y, Isayama T, Naono T, Nobunaga M, Nagai Y. The effects of cytokines on metalloproteinase inhibitors (TIMP) and collagenase production by human chondrocytes and TIMP production by synovial cells and endothelial cells. Clin Exp Immunol. 1993;94:145–149. doi: 10.1111/j.1365-2249.1993.tb05992.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ridker PM, Rifai N, Pfeffer M, Sacks F, Lepage S, Braunwald E. Elevation of tumor necrosis factor-alpha and increased risk of recurrent coronary events after myocardial infarction. Circulation. 2000;101:2149–2153. doi: 10.1161/01.CIR.101.18.2149. [DOI] [PubMed] [Google Scholar]
- 37.Lewandrowski K, Chen A, Januzzi J. Cardiac markers for myocardial infarction. A brief review. Am J Clin Pathol. 2002;118(Suppl 1):S93–S99. doi: 10.1309/3EK7-YVV9-228C-E1XT. [DOI] [PubMed] [Google Scholar]
- 38.Ruseva A. Laboratory diagnosis of acute myocardial infarction. Trakia J Sci. 2005;3:8–14. [Google Scholar]
- 39.Apple FS. Tissue specificity of cardiac troponin I, cardiac troponin T and creatine kinase-MB. Clin Chim Acta. 1999;284:151–159. doi: 10.1016/S0009-8981(99)00077-7. [DOI] [PubMed] [Google Scholar]
- 40.Katus HA, Remppis A, Scheffold T, Diederich KW, Kuebler W. Intracellular compartmentation of cardiac troponin T and its release kinetics in patients with reperfused and nonreperfused myocardial infarction. Am J Cardiol. 1991;67:1360–1367. doi: 10.1016/0002-9149(91)90466-X. [DOI] [PubMed] [Google Scholar]
- 41.Higgins JP, Higgins JA. Elevation of cardiac troponin I indicates more than myocardial ischemia. Clin Invest Med. 2003;26:133–147. [PubMed] [Google Scholar]
- 42.Tucker JF, Collins RA, Anderson AJ, Hauser J, Kalas J, Apple FS. Early diagnostic efficiency of cardiac troponin I and Troponin T for acute myocardial infarction. Acad Emerg Med. 1997;4:13–21. doi: 10.1111/j.1553-2712.1997.tb03637.x. [DOI] [PubMed] [Google Scholar]
- 43.Mair J, ArtnerDworzak E, Lechleitner P, Morass B, Smidt J, Wagner I, Dienstl F, Puschendorf B. Early diagnosis of acute myocardial infarction by a newly developed rapid immunoturbidimetric assay for myoglobin. Br Heart J. 1992;68:462–468. doi: 10.1136/hrt.68.11.462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Vaidya HC. Myoglobin: An early biochemical marker for the diagnosis of acute myocardial infarction. J Clin Immunoass. 1994;17:35–39. [Google Scholar]
- 45.Mair J, Morandell D, Genser N, Lechleitner P, Dienstl F, Puschendorf B. Equivalent early sensitivities of myoglobin, creatine kinase MB mass, creatine kinase isoform ratios, and cardiac troponins I and T for acute myocardial infarction. Clin Chem. 1995;41:1266–1272. [PubMed] [Google Scholar]
- 46.Gibler WB, Gibler CD, Weinshenker E, Abbottsmith C, Hedges JR, Barsan WG, Sperling M, Chen IW, Embry S, Kereiakes D. Myoglobin as an early indicator of acute myocardial infarction. Ann Emerg Med. 1987;16:851–856. doi: 10.1016/S0196-0644(87)80521-8. [DOI] [PubMed] [Google Scholar]
- 47.Bloomberg DJ, Kimber WD, Burke MD. Creatine kinase isoenzymes. Predictive value in the early diagnosis of acute myocardial infarction. Am J Med. 1975;59:464–469. doi: 10.1016/0002-9343(75)90253-3. [DOI] [PubMed] [Google Scholar]
- 48.Wu AH, Wang XM, Gornet TG, OrdonezLlanos J. Creatine kinase MB isoforms in patients with skeletal muscle injury: Ramifications for early detection of acute myocardial infarction. Clin Chem. 1992;38:2396–2400. [PubMed] [Google Scholar]
- 49.Gerhardt W, Katus H, Ravkilde J, et al. S-troponin T in suspected ischemic myocardial injury compared with mass and catalytic concentrations of S-creatine kinase isoenzyme MB. Clin Chem. 1991;37:1405–1411. [PubMed] [Google Scholar]
- 50.Chan D, Ng LL. Biomarkers in acute myocardial infarction. BMC Med. 2010;8:34. doi: 10.1186/1741-7015-8-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Haltern G, Peiniger S, Bufe A, Reiss G, Gülker H, Scheffold T. Comparison of usefulness of heart-type fatty acid binding protein versus cardiac troponin T for diagnosis of acute myocardial infarction. Am J Cardiol. 2010;105:1–9. doi: 10.1016/j.amjcard.2009.08.645. [DOI] [PubMed] [Google Scholar]
- 52.Mad P, Domanovits H, Fazelnia C, Stiassny K, Russmüller G, Cseh A, Sodeck G, Binder T, Christ G, Szekeres T, et al. Human heart-type fatty-acid-binding protein as a point-of-care test in the early diagnosis of acute myocardial infarction. QJM. 2007;100:203–210. doi: 10.1093/qjmed/hcm007. [DOI] [PubMed] [Google Scholar]
- 53.Ruzgar O, Bilge AK, Bugra Z, Umman S, Yilmaz E, Ozben B, Umman B, Meric M. The use of human heart-type fatty acid-binding protein as an early diagnostic biochemical marker of myocardial necrosis in patients with acute coronary syndrome, and its comparison with troponin-T and creatine kinase-myocardial band. Heart Vessels. 2006;21:309–314. doi: 10.1007/s00380-006-0908-2. [DOI] [PubMed] [Google Scholar]
- 54.Morrow DA, de Lemos JA, Sabatine MS, et al. Evaluation of B-type natriuretic peptide for risk assessment in unstable angina/non-ST-elevation myocardial infarction: B-type natriuretic peptide and prognosis in TACTICS-TIMI 18. J Am Coll Cardiol. 2003;41:1264–1272. doi: 10.1016/S0735-1097(03)00168-2. [DOI] [PubMed] [Google Scholar]
- 55.Mastella AK, Moresco RN, da Silva DB, Becker AM, Duarte MM, Giovelli LL, da Silva SH, Rossato L, Moretto MB, da Silva JE. Evaluation of ischemia-modified albumin in myocardial infarction and prostatic diseases. Biomed Pharmacother. 2009;63:762–766. doi: 10.1016/j.biopha.2008.12.002. [DOI] [PubMed] [Google Scholar]
- 56.Hjortshøj S, Dethlefsen C, Kristensen SR, Ravkilde J. Kinetics of ischaemia modified albumin during ongoing severe myocardial ischaemia. Clin Chim Acta. 2009;403:114–120. doi: 10.1016/j.cca.2009.01.033. [DOI] [PubMed] [Google Scholar]
- 57.Xu J, Kimball TR, Lorenz JN, Brown DA, Bauskin AR, Klevitsky R, Hewett TE, Breit SN, Molkentin JD. GDF15/MIC-1 functions as a protective and antihypertrophic factor released from the myocardium in association with SMAD protein activation. Circ Res. 2006;98:342–350. doi: 10.1161/01.RES.0000202804.84885.d0. [DOI] [PubMed] [Google Scholar]
- 58.Kempf T, Sinning JM, Quint A, Bickel C, Sinning C, Wild PS, Schnabel R, Lubos E, Rupprecht HJ, Münzel T, et al. Growth-differentiation factor-15 for risk stratification in patients with stable and unstable coronary heart disease: Results from the AtheroGene study. Circ Cardiovasc Genet. 2009;2:286–292. doi: 10.1161/CIRCGENETICS.108.824870. [DOI] [PubMed] [Google Scholar]
- 59.Kempf T, Björklund E, Olofsson S, Lindahl B, Allhoff T, Peter T, Tongers J, Wollert KC, Wallentin L. Growth-differentiation factor-15 improves risk stratification in ST-segment elevation myocardial infarction. Eur Heart J. 2007;28:2858–2865. doi: 10.1093/eurheartj/ehm465. [DOI] [PubMed] [Google Scholar]
- 60.Voors AA, von Haehling S, Anker SD, Hillege HL, Struck J, Hartmann O, Bergmann A, Squire I, van Veldhuisen DJ, Dickstein K. OPTIMAAL Investigators: C-terminal provasopressin (copeptin) is a strong prognostic marker in patients with heart failure after an acute myocardial infarction: Results from the OPTIMAAL study. Eur Heart J. 2009;30:1187–1194. doi: 10.1093/eurheartj/ehp098. [DOI] [PubMed] [Google Scholar]
- 61.Reichlin T, Hochholzer W, Stelzig C, Laule K, Freidank H, et al. Incremental value of copeptin for rapid rule out of acute myocardial. J Am Coll Cardiol. 2009;54:60–68. doi: 10.1016/j.jacc.2009.01.076. [DOI] [PubMed] [Google Scholar]
- 62.LeLeiko RM, Vaccari CS, Sola S, Merchant N, Nagamia SH, Thoenes M, Khan BV. Usefulness of elevations in serum choline and free F2)-isoprostane to predict 30-day cardiovascular outcomes in patients with acute coronary syndrome. Am J Cardiol. 2009;104:638–643. doi: 10.1016/j.amjcard.2009.04.047. [DOI] [PubMed] [Google Scholar]
- 63.Malathi N, Mythili S, Vasanthi HR. Salivary Diagnostics: A brief review. ISRN Dent. 2014;2014:158786. doi: 10.1155/2014/158786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Floriano PN, Christodoulides N, Miller CS, Ebersole JL, Spertus J, Rose BG, Kinane DF, Novak MJ, Steinhubl S, Acosta S, et al. Use of saliva-based nano-biochip tests for acute myocardial infarction at the point of care: A feasibility study. Clin Chem. 2009;55:1530–1538. doi: 10.1373/clinchem.2008.117713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Miller CS, Foley JD, Bailey AL, Campell CL, Humphries RL, Christodoulides N, Floriano PN, Simmons G, Bhagwandin B, Jacobson JW, et al. Current developments in salivary diagnostics. Biomarkers Med. 2010;4:171–189. doi: 10.2217/bmm.09.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Foley JD, III, Sneed JD, Steinhubl SR, Kolasa JR, Ebersole JL, Lin Y, Kryscio RJ, McDevitt JT, Campbell CL, Miller CS. Salivary biomarkers associated with myocardial necrosis: Results from an alcohol septal ablation model. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;114:616–623. doi: 10.1016/j.oooo.2012.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Möckel M, Danne O, Müller R, Vollert JO, Müller C, Lueders C, Störk T, Frei U, Koenig W, Dietz R, et al. Development of an optimized multimarker strategy for early risk assessment of patients with acute coronary syndromes. Clin Chim Acta. 2008;393:103–109. doi: 10.1016/j.cca.2008.03.022. [DOI] [PubMed] [Google Scholar]
- 68.Wood FO, de Lemos JA. Sorting through new biomarkers. Curr Cardiol Rep. 2008;10:319–326. doi: 10.1007/s11886-008-0051-z. [DOI] [PubMed] [Google Scholar]