Abstract
Introduction:
Although there are many literature examining the possible effects of varicocelectomy on classic semen parameters and recurrence rate, few published articles have examined the effect of conventional laparoscopic varicocelectomy on sperm DNA integrity.
Objectives:
The objective was to evaluate the effect of extensive laparoscopic venous disconnections on the recurrence rate and sperm DNA damage in varicocele patients.
Methods:
Totally, 54 patients with varicocele underwent extensive laparoscopic venous disconnections were assessed by clinical evaluation, duplex scan, semen analysis, and sperm DNA fragmentation assay before surgery and after 6 and 12 months following surgery.
Results:
No intra- or post-operative complications were observed and out of 54 patients preoperatively complained from varicocele 2 (3.7%) patients' have recurrence during the follow-up period for 12 months. Out of 54 patients complaining from male infertility, 14 patients success to get pregnancy after 6 months with pregnancy rates of 25.92% and 22 (40.74%) after 12 months, and 28 patients (51.85%) had a preoperative DNA fragmentation index (DFI) >30%, decreased following surgery below 30% in 19 (35.18%) patients after 6 months, and 11 (20.37%) after 12 months, and the percentage of sperm with DFI > 30% was significantly decreased after 6 and 12 months, respectively (38.4 ± 10.6 vs. 31.3 ± 12.4, [P < 0.001] at 6 months, and 22.9 ± 13.2, [P < 0.001] after 1-year). Other spermatic parameter was significantly improved.
Conclusions:
An extensive laparoscopic venous disconnection was significantly decreasing the recurrence rate, DFI and improving normal semen parameters and fertility.
Keywords: Extensive, infertility, laparoscopic, sperm, varicocele
INTRODUCTION
Varicocele is a state of dilated, elongated, and tortuous veins of the pampiniform plexus of the spermatic cord. Varicoceles typically develop during adolescent and have been found in about 15% of the general male populations and up to 40% of men with primary infertility and 75% of men with secondary infertility.[1]
Surgery is currently the most popular treatment for varicocele patients with signs of abnormal semen, testicular hypotrophy or pain. The recurrences rates following varicocele repair range from 5% to 20% depending upon the technique used. The main causes of high recurrence varicocelectomy are developed collaterals within the interrupted venous drainage system and persistence or progression of uninterrupted pathological venous drainage routes.[2]
Varicocele have been associated with increased levels of reactive oxygen species and decreased seminal antioxidant capacity, increased sperm DNA damage, and defective spermatogenesis in affected patients. Sperm DNA damage, in turn, has been linked to lower rates of spontaneous conception, as well as assisted reproductive pregnancies.[3]
Although there are many literature examining the possible effects of varicocelectomy on classic semen parameters and recurrence rate, few published articles have examined the effect of conventional laparoscopic varicocelectomy on sperm DNA integrity,[4,5,6] which provides an ideal access to treat varicocele due to clear visualization of most of the involved venous systems (internal spermatic vein [ISV], external spermatic vein [ESV], deferential veins) which still have same problem of recurrence. So that we attempt to improve the current approach through extensive laparoscopic venous dissections and study effect of this on sperm DNA damage and recurrence rate.
Aim of the work
The purpose of the current study was to further investigate the possible effects of extensive laparoscopic varicocelectomy on the recurrence rate and sperm DNA damage in a prospective design.
METHODS
This was a prospective study that included 54 patients have varicocele presenting to our hospital from May 2010 to September 2013. All participants had complained of infertility for at least 1-year and 16 complained pain and bad cosmetics appearance. All patients underwent medical history and completing general and genital physical examinations, baseline semen analysis, and a test for sperm DNA fragmentation using a TUNEL assay.
All patients were assessed for serum follicle-stimulating hormone, luteinizing hormone, and testosterone levels and scrotal Doppler ultrasound for diagnosis of varicocele according to visible evidence of reflux on cough or valsalva maneuver, as well as multiplicity and size of the veins. All patients had clinically palpable varicocele and abnormal semen parameters in two or more semen samples were received according to World Health Organization manual 2010.[7]
Patients with evidence of azoospermia, urogenital infections, hypogonadism, systemic or endocrine disease or a history of smoking, alcohol or drug abuse, hormonal treatment were excluded. Participating patients did not receive any medical treatment for infertility during the 6 months before enrollment in the study and during the follow-up period.
The institutional ethics committee for research approved the study and the surgical procedure was explained to the participants, and signed consent for the surgical procedure was obtained. Extensive laparoscopic varicocelectomy were performed by the same surgeon for all patients in the period from May 2010 to September 2013. Both external and ISVs were ligated and divided, the testicular artery and lymphatic vessels were spared.
All participating patients were asked to revisit the clinic after 3 and 6 months for follow-up clinical symptoms, semen analysis, sperm DNA fragmentation assessment, and scrotal ultrasound examination to check for varicocele recurrence and sperm DNA fragmentation.
Operative procedure
Under general anesthesia, we start with the patient in the supine position and the operating table in the horizontal level. A small subumbilical incision (1 cm) is made and peritoneal insufflation is performed via a Veress needle to a pressure of 15 mmHg. The umbilical trocar-cannula is inserted and the telescope is introduced. During the procedure, the intra-abdominal pressure is reduced to 12 mmHg. The surgeon inspects the abdomen in general, but focuses on the anatomy of the venous drainage of both testes. Two other ports are then introduced; each is midway between the umbilicus and the anterior superior iliac spine, at the lateral border of the rectus abdominis, on one side of the abdomen.
The initial steps in the dissection are similar to those of the classical laparoscopic procedure for varicocele (opening a window in the parietal peritoneum over internal spermatic vessels and dissecting to identify individual vessels). The artery is identified by its visible pulsation. It is isolated to allow the inclusion of all the other vessels within the field in disconnection with more dissection across the axis of the ISV is done and proceeds cephalad to include possible missed accessory veins through mobilization of the sigmoid and descending colon to expose the veins underneath.
As the dissection progresses, the dissected vein bundle becomes longer. It becomes necessary to keep the vein bundle elevated to facilitate its dissection from the surrounding extraperitoneal tissue and to expose communicator veins. As the dissection progresses cephalad, a wide margin of the “venous ablation field” is always maintained (about one inch on each side). Meanwhile, communicator veins (e.g., testiculo-colonic and testiculo-ureteric) continue to appear as they join the ISV. They are either coagulated by diathermy or clipped before they are divided. A minimum of 10 cm of the length of the vein bundle is totally freed.
The usual endpoint is met when the ISV turns deeply to join the renal vein. Clips are applied at this point and caudally at the starting point then the vein bundle between clips is excised and removed outside the abdomen. The ESV is managed by occluding the terminal end of the inferior epigastric vein by clips or diathermy coagulation. All patients were follow-up assessed by: Clinical evaluation, duplex scan, and semen analysis after 3 and 6 months after surgery.
Statistical methods
Differences between pre- and postoperative parameters were estimated by the Wilcoxon signed-rank test. The correlation coefficients between variables were calculated using Spearman's nonparametric method. All analyses were conducted using SPSS 80 for Windows (SPSS Inc., Chicago, IL, USA). All hypothesis testing was two-tailed.P < 0.05 was considered statistically significant.
RESULTS
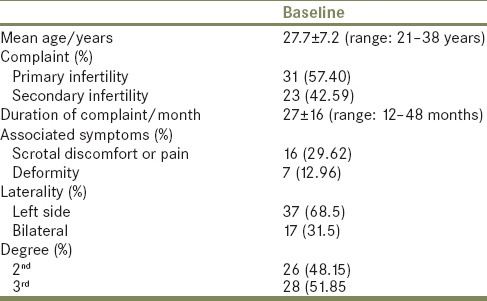
The mean age was 27.7 ± 7.2 years (range: 21–38 years), and the mean duration of complaining was 27 ± 16 months (range: 12–48 months). Varicocele was detected on the left side only in 37 (68.5%) patients and bilaterally in 17 (31.5%) patients. Of the 54 patients included in the study, 31 (57.40%) had primary infertility whereas 23 (42.59%) of them had secondary infertility [Table 1].
Table 1.
Baseline Clinical characteristics of the patients
Operative data
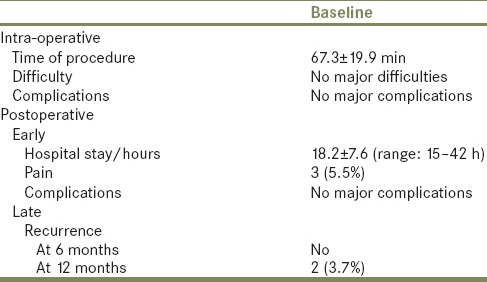
The duration of the procedure ranged between 55 min and 85 min (the mean was 67.3 ± 19.9). No major difficulties were encountered during the procedure, and any degree of bleeding was observed to stain the whole field and reduce the illumination. No major intra-operative complications such as bleeding, bowel injury or others were encountered. No major postoperative complications were observed. Delayed bowel function occurred in 5 patients. Recovery was eventless in most cases. All patients were discharged within 48 h of the procedure [Table 2].
Table 2.
Operative assessments and postoperative follow-up
Follow-up
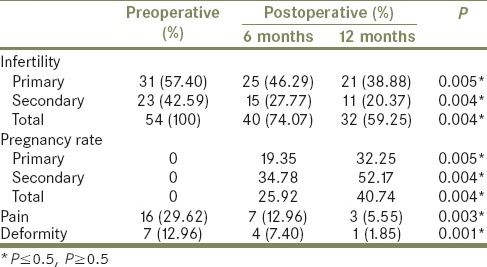
During follow-up period at 6 and 12 months, out of 54 patients complaining from male infertility, 14 patients success to get pregnancy after 6 months with pregnancy rates of 25.92% and 22 (40.74%) after 12 months. Pregnancy rate was 19.35% and 32.25% in patients with primary infertility and 34.78% and 52.17% in patients with secondary infertility after 6 and 12 months, respectively.
In regard to associated symptoms, 13 patients out of 16 patients (81.25%) was complaining with scrotal discomfort or pain had complete resolution of their symptoms; and 3 patients (18.75%) still have pain and 1 patients out of 7 (14.28%) have residual deformity, none of the patients developed hydrocele and 2 patients had recurrence only detecting by Doppler ultrasound examination at 12 months [Table 3].
Table 3.
Characteristics of postoperative follow-up patient's complaints
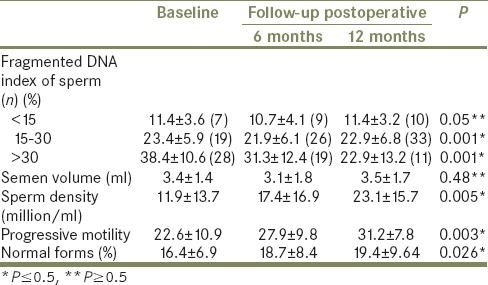
There was a positive correlation between the sperm DNA fragmentation index (DFI) and the duration of complaining (r = 0.42,P < 0.05), sperm density (r = 0.51,P < 0.05), and sperm motility (r = 0.47,P < 0.05), but there was no correlation between the sperm DFI and the percentage of sperm with sperm's normal forms (r = 0.12,P > 0.05). Of 54 patients, 28 patients (51.85%) had a preoperative DFI > 30%, decreased following surgery below 30% in 19 (35.18%) patients after 6 months, and 11 (20.37%) after 12 months, and the percentage of sperm with DFI > 30% was significantly decreased after 6 and 12 months, respectively (38.4 ± 10.6 vs. 31.3 ± 12.4, (P < 0.001) at 6 months, and 22.9 ± 13.2, (P < 0.001) after 1-year) [Table 4].
Table 4.
Baseline seminal laboratory assessments and postoperative follow-up
DISCUSSION
Regardless of the exact etiological mechanism, venous reflux is a constant feature in varicocele, which is observed in all clinical cases and becomes more frequent and more serious with time, results in testicular damage so that the majority of current surgical approaches to varicocele share one basic principle: “Interruption of pathological incompetent and refluxing venous drainage route of the testes to divert venous drainage to competent routes.”[8]
There are many factors contribute to recurrence of varicocele including, incomplete elimination of the refluxing venous channels at the time of surgery and/or development of collaterals after elimination of the original source of reflux. The first one may be due to technically ineffective interruption, or missing one of ISV, which is less frequently a single vein and reported to cause 50% of the recurrences after surgery.[9] Not only but the ESV was also reported to account for 20% of the cases of varicocele recurrence.[10]
Normally, communicator's venous channels connect the ISV with the neighboring plexuses. They include testiculo-ureteric, testiculo-colonic, testiculo-renal, and testiculo-testicular veins. The connections of the ISV with ureteral and colonic plexuses, as well as the contralateral ISV play an important role in recurrence. Following simple interruption of the ISV develop collateral channels that restore the reversed flow to caudal segment of ISV by passing site of interruption and employing neighboring plexuses as colonic, renal, ureteral or contralateral testicular venous bridges. This mechanism was reported in 18% of cases of recurrence.[9]
In our study, recurrence factors were abolished by excision of a long segment of the ISV and clearing all significant communicator veins. Dissection of the ISV for a long distance and exposing a wide area across its course allow visual identification of communicator veins and their ablation by coagulation or clips. This procedure was planned to widen the narrow pressure front as well and discourages re-communication.
The early results of this technique were impressive and may contribute to improve the outcome of varicocele surgery and decrease the recurrence rate. The incidence of varicocele recurrence following surgical repair varies from 1% to 35%, depends upon the type of procedure performed. The recurrence rate was 1–15%, 5–15%, 5–20%, and 7–25% in microscopic inguinal, retroperitoneal, conventional inguinal laparoscopic, and balloon technique, respectively.[11] Our recurrence rate at extensive laparoscopic varicocelectomy was 3.7% at 12 months after varicocelectomy.
Increasing evidence that varicocele ligation improves semen quality and pregnancy rates. However, the bulk of these data come from retrospective and poor controlled study. Although numerous observational study have documented higher pregnancy rates following varicocelectomy versus observation only two randomized controlled studies have been performed in the last 2 years. Abdel-Meguid et al.,[12] randomized 145 men with minimal varicocele to microsurgical varicocelectomy or observation, and reported significantly improved semen parameter and high spontaneous pregnancy rate versus control groups (33% vs. 14%), Mansour et al.,[13] similarly reported higher pregnancy rate in 136 men randomized to varicocelectomy versus conservative management (44% vs. 19%). in present study, patients showed higher sperm density, progressive motility, and normal form (P < 0.05) and out of 54 patients was complaining of male infertility, 14 patients' success to get pregnancy after 6 months with pregnancy rates of 25.92% and 22 (40.74%) after 12 months after extensive laparoscopic varicocelectomy.
The results of our study demonstrated that 28 patients (51.85%) had a preoperative DFI > 30%, decreased following surgery below 30% in 19 (35.18%) patients after 6 months, and 11 (20.37%) after 12 months, and the percentage of sperm with DFI > 30% was significantly decreased after 6 and 12 months, respectively (38.4 ± 10.6 vs. 31.3 ± 12.4, (P < 0.001) at 6 months, and 22.9 ± 13.2, (P < 0.001) after 1-year). Our results are agreements with several recent studies [14,15,16] have documented beneficial effect of varicocelectomy on sperm DNA quality.
In a prospective study of 81 infertile men who underwent microscopic varicocelectomy Ghazi and Abdelfattah,[14] reported significant decrease DFI 6 months after surgery, 18 patients showed preoperative fragmentation index > 30% and after varicocelectomy 16 of them showed DFI < 30%. Similar finding has been reported by Zini et al.,[17] have noted that significant post-varicocelectomy improvements in DFI decreased from18% before surgery to 10% and 7% at 4 and 6 months after surgery, respectively).
The association between DFI and pregnancy was explored by Smit et al.,[18] in 49 infertile men, the authors reported significant decrease DNA fragmentation after surgery from 35.2% to 30.2% after varicocelectomy and 37% of couple patient conceive spontaneously and 24% achieve pregnancy with assisted reproductive technique and the mean postoperative DNA fragmentation was significantly higher in couple that did not conceive spontaneously or through in vitro fertilization/intra-cytoplasmic sperm injection. In contrast to Baker et al.,[19] did not find the difference in the mean postoperative DFI in couple, who were able to achieve pregnancy compare to couples that reported no pregnancy.
Our finding that sperm DNA fragmentation decreased below this threshold 30% in 9 patients out of 28 patients (32.14%) after 6 months following extensive laparoscopic venous dissection had preoperative DNA fragmentation > 30% in agree with other report by others [20,21] however, there were several limitations in this current study as the total number of patients were too small to draw definitive conclusion and lack of control groups.
The current study is the first prospective study to demonstrate the effect of extensive laparoscopic varicocelectomy on sperm DNA damage using the TUNEL assay. The outcome of our study was comparable with recently published meta-analysis studies,[21,22] that showed the incidence of pregnancy rate was significantly higher in microsurgical varicocelectomy (39.1%) with low incidence of recurrence (1.05%) than conventional open and laparoscopic varicocelectomy. Our findings were supporting the previously published literature that both extensive laparoscopic and microsurgical varicocelectomy have similar predictive values for DNA fragmentation, varicocele recurrence and improve pregnancy rate.
CONCLUSIONS
Extensive laparoscopic venous disconnections significantly decreasing recurrence rate, DFI, and improving normal semen parameters and fertility.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Kim ED, Leibman BB, Grinblat DM, Lipshultz LI. Varicocele repair improves semen parameters in azoospermic men with spermatogenic failure. J Urol. 1999;162:737–40. doi: 10.1097/00005392-199909010-00031. [DOI] [PubMed] [Google Scholar]
- 2.Beck EM, Schlegel PN, Goldstein M. Intraoperative varicocele anatomy: A macroscopic and microscopic study. J Urol. 1992;148:1190–4. doi: 10.1016/s0022-5347(17)36857-x. [DOI] [PubMed] [Google Scholar]
- 3.Giwercman A, Lindstedt L, Larsson M, Bungum M, Spano M, Levine RJ, et al. Sperm chromatin structure assay as an independent predictor of fertility in vivo: A case-control study. Int J Androl. 2010;33:e221–7. doi: 10.1111/j.1365-2605.2009.00995.x. [DOI] [PubMed] [Google Scholar]
- 4.Will MA, Swain J, Fode M, Sonksen J, Christman GM, Ohl D. The great debate: Varicocele treatment and impact on fertility. Fertil Steril. 2011;95:841–52. doi: 10.1016/j.fertnstert.2011.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Blumer CG, Fariello RM, Restelli AE, Spaine DM, Bertolla RP, Cedenho AP. Sperm nuclear DNA fragmentation and mitochondrial activity in men with varicocele. Fertil Steril. 2008;90:1716–22. doi: 10.1016/j.fertnstert.2007.09.007. [DOI] [PubMed] [Google Scholar]
- 6.Moskovtsev SI, Lecker I, Mullen JB, Jarvi K, Willis J, White J, et al. Cause-specific treatment in patients with high sperm DNA damage resulted in significant DNA improvement. Syst Biol Reprod Med. 2009;55:109–15. doi: 10.1080/19396360902787944. [DOI] [PubMed] [Google Scholar]
- 7.Cooper TG, Noonan E, von Eckardstein S, Auger J, Baker HW, Behre HM, et al. World Health Organization reference values for human semen characteristics. Hum Reprod Update. 2010;16:231–45. doi: 10.1093/humupd/dmp048. [DOI] [PubMed] [Google Scholar]
- 8.Campobasso P. Blue venography in adolescent varicocelectomy: A modified surgical approach. J Pediatr Surg. 1997;32:1298–301. doi: 10.1016/s0022-3468(97)90306-7. [DOI] [PubMed] [Google Scholar]
- 9.Sze DY, Kao JS, Frisoli JK, McCallum SW, Kennedy WA, 2nd, Razavi MK. Persistent and recurrent postsurgical varicoceles: Venographic anatomy and treatment with N-butyl cyanoacrylate embolization. J Vasc Interv Radiol. 2008;19:539–45. doi: 10.1016/j.jvir.2007.11.009. [DOI] [PubMed] [Google Scholar]
- 10.Coolsaet BL. The varicocele syndrome: Venography determining the optimal level for surgical management. J Urol. 1980;124:833–9. doi: 10.1016/s0022-5347(17)55688-8. [DOI] [PubMed] [Google Scholar]
- 11.Cayan S, Shavakhabov S, Kadioglu A. Treatment of palpable varicocele in infertile men: A meta-analysis to define the best technique. J Androl. 2009;30:33–40. doi: 10.2164/jandrol.108.005967. [DOI] [PubMed] [Google Scholar]
- 12.Abdel-Meguid TA, Al-Sayyad A, Tayib A, Farsi HM. Does varicocele repair improve male infertility. An evidence-based perspective from a randomized, controlled trial? Eur Urol. 2011;59:455–61. doi: 10.1016/j.eururo.2010.12.008. [DOI] [PubMed] [Google Scholar]
- 13.Mansour Ghanaie M, Asgari SA, Dadrass N, Allahkhah A, Iran-Pour E, Safarinejad MR. Effects of varicocele repair on spontaneous first trimester miscarriage: A randomized clinical trial. Urol J. 2012;9:505–13. [PubMed] [Google Scholar]
- 14.Ghazi S, Abdelfattah H. Effect of microsurgical varicocelectomy on sperm DNA fragmentation in infertile men. Middle East Fertil Soc J. 2011;16:149–53. [Google Scholar]
- 15.Smit M, Dohle GR, Hop WC, Wildhagen MF, Weber RF, Romijn JC. Clinical correlates of the biological variation of sperm DNA fragmentation in infertile men attending an andrology outpatient clinic. Int J Androl. 2007;30:48–55. doi: 10.1111/j.1365-2605.2006.00710.x. [DOI] [PubMed] [Google Scholar]
- 16.Marmar JL. The pathophysiology of varicoceles in the light of current molecular and genetic information. Hum Reprod Update. 2001;7:461–72. doi: 10.1093/humupd/7.5.461. [DOI] [PubMed] [Google Scholar]
- 17.Zini A, Azhar R, Baazeem A, Gabriel MS. Effect of microsurgical varicocelectomy on human sperm chromatin and DNA integrity: A prospective trial. Int J Androl. 2010;33:1–6. doi: 10.1111/j.1365-2605.2009.01048.x. [DOI] [PubMed] [Google Scholar]
- 18.Smit M, Romijn JC, Wildhagen MF, Veldhoven JL, Weber RF, Dohle GR. Decreased sperm DNA fragmentation after surgical varicocelectomy is associated with increased pregnancy rate. J Urol. 2010;183:270–4. doi: 10.1016/j.juro.2009.08.161. [DOI] [PubMed] [Google Scholar]
- 19.Baker K, McGill J, Sharma R, Agarwal A, Sabanegh E., Jr Pregnancy after varicocelectomy: Impact of postoperative motility and DFI. Urology. 2013;81:760–6. doi: 10.1016/j.urology.2012.12.005. [DOI] [PubMed] [Google Scholar]
- 20.Ding H, Tian J, Du W, Zhang L, Wang H, Wang Z. Open non-microsurgical, laparoscopic or open microsurgical varicocelectomy for male infertility: A meta-analysis of randomized controlled trials. BJU Int. 2012;110:1536–42. doi: 10.1111/j.1464-410X.2012.11093.x. [DOI] [PubMed] [Google Scholar]
- 21.Kadioglu TC, Aliyev E, Celtik M. Microscopic varicocelectomy significantly decreases the sperm DNA fragmentation index in patients with infertility. Biomed Res Int. 2014;2014:695713. doi: 10.1155/2014/695713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang YJ, Zhang RQ, Lin YJ, Zhang RG, Zhang WL. Relationship between varicocele and sperm DNA damage and the effect of varicocele repair: A meta-analysis. Reprod Biomed Online. 2012;25:307–14. doi: 10.1016/j.rbmo.2012.05.002. [DOI] [PubMed] [Google Scholar]


