Abstract
A 44-year-old female presented to the urology clinic with flank pain and tenderness. After full assessment, the patient was booked for surgery for partial nephrectomy and the patient was diagnosed with renal cell carcinoma (RCC) chromophob type. Six months later, the patient came back for follow-up; a mass was detected on the same kidney. Radical nephrectomy was performed to excise what is thought to be a recurrence of RCC and the tissues were sent to pathology. The postoperative pathology report confirmed the presence of xanthogranulomatous pyelonephritis rather than RCC recurrence.
Keywords: Chronic kidney infection, renal cell carcinoma, xanthogranulomatous pyelonephritis
INTRODUCTION
Xanthpgranulomatous pyelonephritis (XGP) is an uncommon, destructive and serious subtype of chronic pyelonephritis. It is characterized by the destructive inflammatory yellow mass that is formed of mixed inflammatory infiltrates clefts of cholesterol in the background and fibrosis. These infiltrates are composed of xanthomatouse histiocytes, multinucleated giant cells, lymphocytes, plasma cells and lipid-laden macrophages with adipocytes.[1] The inflammatory process can lead to parynchimal destruction and tubular atrophy. XGP can be associated with Proteus mirabilis, Escherichia coli, Klebseiella, Pseudomonas infections or even mixed organisms.[2] The condition can also be caused by calculus obstruction of the urinary tract. Middle-aged woman are more commonly affected by XGPN than others.[3] Unilateral involvement of the kidney is the usual scenario but, bilateral kidney involvement can occur, rarely.[4]
CASE REPORT
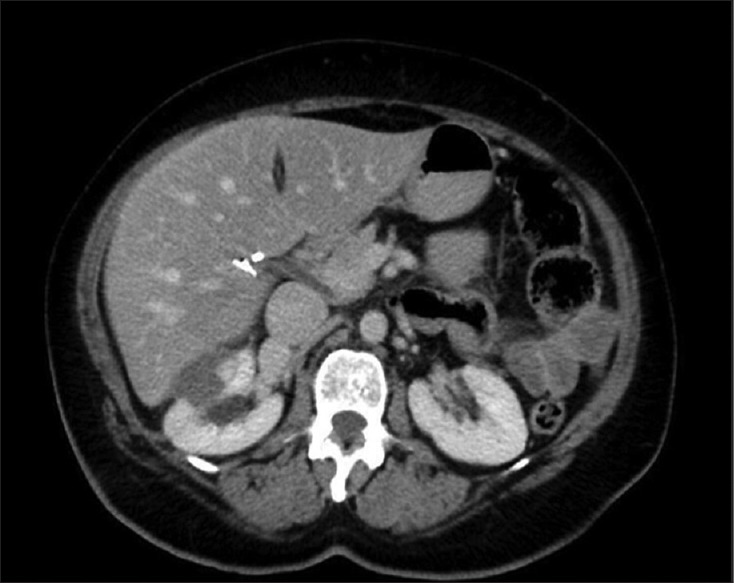
A 44-year-old female presented, to the urology clinic, with mild flank pain and tenderness. Her history was negative for hematuria, lower urinary tract symptoms, stones, fever, and weight loss. The past surgical medical and familial history was unremarkable. On inspection, the patient appeared well with normal vital signs. Normal general and abdominal exams were noted except for tenderness in the flank area. The laboratory results showed normal complete blood counts and normal renal profile. Her urine analysis and culture were also unremarkable. The radiological assessment included a kidney ultrasound and a computed tomography (CT) scan. Both of which displayed a mass. On the CT scan, a hyperdense mass that measuring 4.4 cm × 3.7 cm that is projecting from the mid/upper pole was appreciated [Figure 1]. The patient then underwent partial nephrectomy and was diagnosed with renal cell carcinoma (RCC) chromophobe type with positive margins. On 6 months follow-up, postsurgery, a mass was again detected on CT scan, which appeared at the site of the partial nephrectomy. The mass was hyper dense and measures 3.3 cm × 2.3 cm × 3.4 cm [Figure 2]. The decision was then taken to book the patient for surgery to undergo radical nephrectomy. The pathology report afterward confirmed the diagnoses of XGP with no residual chromophobe type RCC Identified.
Figure 1.
Hyper dense mass that measures 4.4 cm × 3.7 cm
Figure 2.

Hyper dense mass that measures 3.3 cm × 2.3 cm × 3.4 cm
DISCUSSION
We report this case of XGP that appeared 6 months after a surgical resection of a renal cell carcinoma. XGP is a form of chronic destructive infection that affects the entire kidney. It is quite difficult to diagnose XGP based on radiological assessment, signs and symptoms alone. XGP has been staged by Malek and Elder into 3 different stages: Stage 1, nephric, when there is only kidney involvement. Stage 2, perinephric, is when the perirenal fat is involved. The 3rd stage, paranephric, is when there is widespread involvement of the retroperitoneal area. Even though the etiology is unclear, the literature displayed 2 factors that are linked with the development of XGP, urine tract obstruction and nephrolithiasis. Examples of obstruction include tumors of the urine tract like renal cell carcinoma, ureteral carcinoma or even bladder cancer[5] laboratory parameters may reveal changes in XGP patients. These changes may include anemia, elevated white blood counts and elevated acute phase reactants that are, erythrocyte sedimentation rate and positive urine cultures. A physical exam may reveal flank tenderness, weight loss, and a palpable mass.[6] Many differential diagnoses could give similar clinical pictures to XGP. RCC, certainly a main differential diagnosis, can present in near time intervals with XGP in rare situations. A study that reviewed 16 cases documented the coexistence of both RCC and XGP in one of the patients.[7] Fallatah et al., reported the coexistence of RCC and XGP in one case and transitional cell carcinoma of the kidney with XGP in another case.[8] Tuberculosis, another differential diagnosis, can also mimic XGP. Shah et al., reported a case that was thought to be XGP. After surgical resection, the pathological results surprisingly confirmed the diagnosis tuberculosis that spread to the liver and formed an abscess.[9] The radiological assessment of XGP is usually nonspecific but, the preferred diagnostic imaging modality is CT scan. CT scan can provide help in surgical planning, as it can reflect the amount of extra-renal extension if any. The most specific findings on CT scans are; an enlarged nonfunctional kidney, a central calculus along with a contracted renal pelvis, inflammation of the perinephric fat area and calyceal expansion.[10] Histopathological assessment is the mainstay of diagnosis. The inflammatory changes, as mentioned in the introduction section, along with immunohistochemistry studies in which, XGP is positive to CD68 confirms the diagnosis.[1] The treatment of XGP is mainly surgical. Generally, Radical nephrectomy along with resection of the involved tissues is the treatment modality of choice. Antimicrobials should be administered prior to surgery to control local infection. However, partial nephrectomy was performed in a bilateral kidney involvement case.[4]
CONCLUSION
XGP is a serious condition that can mimic different conditions including RCC. Careful evaluation of patients through thorough history taking and examination, laboratory investigations and radiological assessment must be performed in order to help reduce the chances if incorrect diagnosis of the condition.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Li L, Parwani AV. Xanthogranulomatous pyelonephritis. Arch Pathol Lab Med. 2011;135:671–4. doi: 10.5858/2009-0769-RSR.1. [DOI] [PubMed] [Google Scholar]
- 2.Goodman M, Curry T, Russell T. Xanthogranulomatous pyelonephritis (XGP): A local disease with systemic manifestations. Report of 23 patients and review of the literature. Medicine (Baltimore) 1979;58:171–81. [PubMed] [Google Scholar]
- 3.Chuang CK, Lai MK, Chang PL, Huang MH, Chu SH, Wu CJ, et al. Xanthogranulomatous pyelonephritis: Experience in 36 cases. J Urol. 1992;147:333–6. doi: 10.1016/s0022-5347(17)37229-4. [DOI] [PubMed] [Google Scholar]
- 4.Peréz LM, Thrasher JB, Anderson EE. Successful management of bilateral xanthogranulomatous pyelonephritis by bilateral partial nephrectomy. J Urol. 1993;149:100–2. doi: 10.1016/s0022-5347(17)36011-1. [DOI] [PubMed] [Google Scholar]
- 5.Dell'Aprovitola N, Guarino S, Del Vecchio W, Camera L, Chiancone F, Imbimbo C, et al. Xanthogranulomatous pyelonephritis mimicking a renal cell carcinoma: A unique and challenging case. Acta Radiol Short Rep. 2014;3:2047981613513763. doi: 10.1177/2047981613513763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Al-Ghazo MA, Ghalayini IF, Matalka II, Al-Kaisi NS, Khader YS. Xanthogranulomatous pyelonephritis: Analysis of 18 cases. Asian J Surg. 2006;29:257–61. doi: 10.1016/S1015-9584(09)60099-3. [DOI] [PubMed] [Google Scholar]
- 7.Siddappa S, Ramprasad K, Muddegowda MK. Xanthogranulomatous pyelonephritis: A retrospective review of 16 cases. Korean J Urol. 2011;52:421–4. doi: 10.4111/kju.2011.52.6.421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fallatah A, Tarakji M, Amuesi J. Xanthogranulomatous pyelonephritis: A retrospective study of 10 cases and review of the literature. Saudi J Kidney Dis Transpl. 2001;12:520–4. [PubMed] [Google Scholar]
- 9.Shah HN, Jain P, Chibber PJ. Renal tuberculosis simulating xanthogranulomatous pyelonephritis with contagious hepatic involvement. Int J Urol. 2006;13:67–8. doi: 10.1111/j.1442-2042.2006.01227.x. [DOI] [PubMed] [Google Scholar]
- 10.Craig WD, Wagner BJ, Travis MD. Pyelonephritis: Radiologic-pathologic review. Radiographics. 2008;28:255–77. doi: 10.1148/rg.281075171. [DOI] [PubMed] [Google Scholar]


