Abstract
Persistent Müllerian duct syndrome is a rare genetic disorder characterized by a male with retained Müllerian structures. Remnant excision must be considered due to the possibility of malignant degeneration. We review a case of delayed diagnosis in a 25-year-old man presenting with hematuria. Preoperative counseling must emphasize the risk of malignancy versus the risks to fertility. The da Vinci robot offers a novel, safe approach for excision of the relevant Müllerian structures. Dissection should be limited to structures superior to the cavernosal neurovascular bundles to preserve the continence and erectile function. A semen analysis is recommended preoperatively to determine effects on fertility.
Keywords: Laparoscopic surgery, Persistent Mullerian duct syndrome, robotic surgery
INTRODUCTION
Persistent Müllerian duct syndrome (PMDS) is a rare disorder in which a normally virilized 46 XY male retains Müllerian duct structures. Beginning at 7 weeks of gestation, Sertoli cells release anti-Müllerian hormone (AMH) which leads to the regression of the Müllerian ducts.[1] In PMDS, there is a defect in either AMH or the AMH receptor, which leads to the presence of Müllerian structures in a male with an otherwise normal phenotype.[1]
Over the past 50 years, roughly 200 cases of PMDS have been reported. Usually, the diagnosis is made in the workup of cryptorchidism in infancy.[2] In some cases, diagnosis is delayed. The management usually involves the surgical removal of the retained Müllerian duct structures. In this article, we describe a case of delayed diagnosis of PMDS, outline management, and counseling and present a minimally invasive method of surgical management.
CASE REPORT
A 27-year-old male with a history of bilateral cryptorchidism status post orchiopexy at 18 months presented with intermittent, painless, gross hematuria, and hematospermia. Over the previous 9 months, these episodes occurred 1–2 times/month and lasted several days. Physical exam revealed small volume, descended testes bilaterally with difficult to palpate vasa and a normal penis.
Due to patient desire to limit the invasive procedures, the magnetic resonance (MR) was performed. MR urogram discovered a right unicornuate uterus with an endocervical canal that terminated within the right seminal vesicle [Figure 1]. Subsequent laboratory evaluation confirmed a 46 XY karyotype and a hormone panel including AMH, estradiol, follicle stimulating hormone, luteinizing hormone, and testosterone was all within the normal limits. Cystoscopy revealed a pinpoint orifice at the level of the verumontanum which communicated with the remnant uterus on fluoroscopy [Figure 2].
Figure 1.
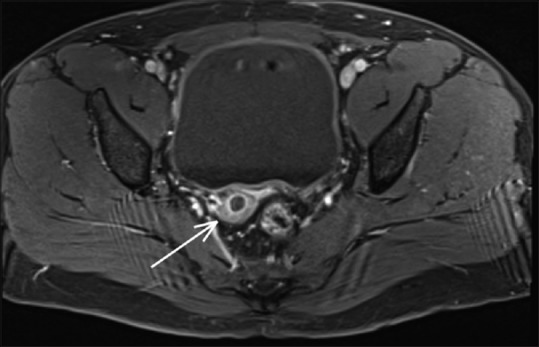
Magnetic resonance urogram revealed a right unicornuate uterus. A tubular structure (white arrow) originating from the endocervical canal travels medially along the superior aspect of the right seminal vesicle to the midline where it inserts into the prostatic urethra
Figure 2.
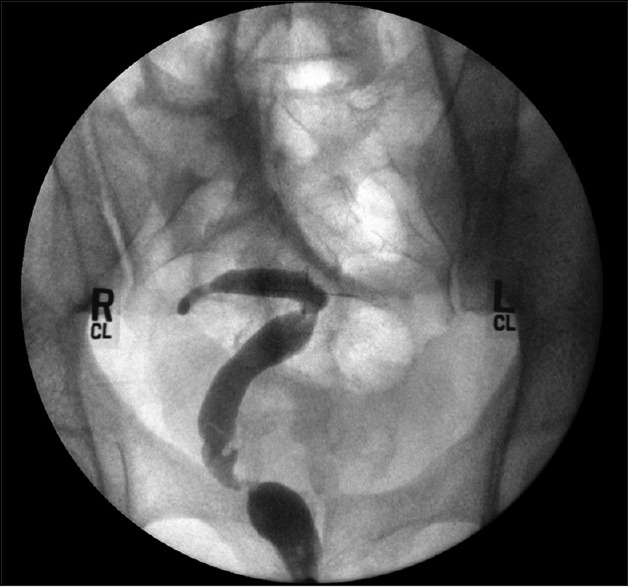
Fluoroscopy confirming communication between the Müllerian remnant and the verumontanum orifice
Upon the discussion of the findings, the patient strongly desired the removal of the remnant Müllerian structures. Open and laparoscopic surgical approaches were discussed and the patient elected robotic surgery. The patient was counseled regarding the risks of the procedure including infertility; however, he elected not to pursue a semen analysis or attempt sperm cryopreservation.
In the operating room, bilateral #6 French ureteral catheters were placed to the level of the proximal ureter, and a #4 French catheter was placed into the os of the Müllerian remnant via the verumontanum orifice. A robotic approach with a standard port placement, as robotic prostatectomy, was utilized. The Müllerian remnant was immediately visible and dissected free using sharp instruments and cautery [Figure 3].
Figure 3.
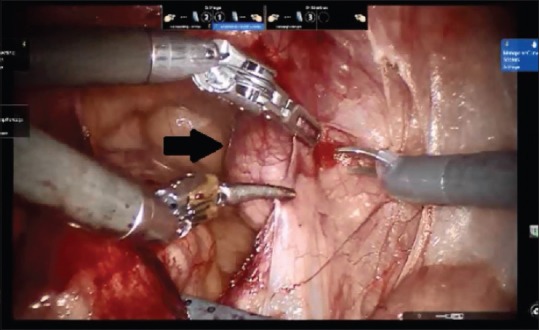
Intra-operative photograph showing the Mullerian remnant (arrow) as adhesions are taken down. Three working arms and helper suction are appreciated as well
The round ligaments were ligated bilaterally with electrocautery and the uterine arteries were controlled with a combination of Weck® clips and electrocautery. The seminal vesicles were densely adherent but dissected away from the Müllerian remnant. Dissection was limited to the vaginal cuff superior to the level of the seminal vesicles to avoid injury to the cavernosal neurovasculature [Figure 4].
Figure 4.
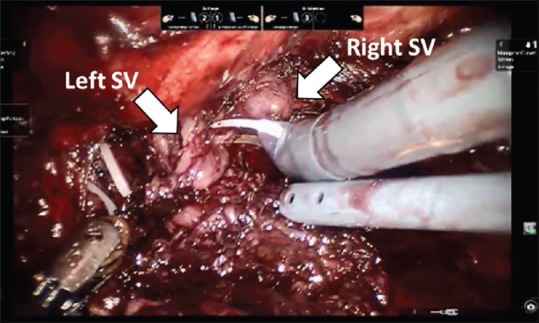
Continued dissection of the remnant structure with bilateral seminal vesicles demonstrated
The cuff was oversewn, and a Jackson-Pratt drain was left in place. The case and recovery were uncomplicated. Surgical pathology demonstrated mostly uterine-like smooth muscle with a central cavity lined by underdeveloped endocervical-type tissue.
DISCUSSION
In the management of PMDS, treatment options must address the Müllerian remnant as well as the cryptorchidism. Although it is agreed that orchiopexy is necessary for cryptorchidism, the decision for excision of the Müllerian remnant is controversial. Early reports argued that there was no absolute indication for the removal of Müllerian remnants since the risk of malignant degeneration had never been established.[3] Furthermore, the excision carries high risks such as the damage to the vasa and to the deferential arteries which provide a critical collateral blood supply to the testes in the case of a Stephens-Fowler approach to the undescended testicle.[3,4] Therefore, an excision was determined to be necessary only when the remnants limited the orchiopexy.
A more recent report, however, has demonstrated the association of malignant degeneration in Müllerian duct remnants.[2] In a review of the literature, Farikullah et al. found 11 reports of Müllerian duct malignancies out of approximately 200 cases over the past 50 years. Three of the 11 cases demonstrated metastatic spread with 2 deaths as a result. They concluded with 90% of confidence that PMDS patients have a 3.1–8.4% risk of developing Müllerian malignancies. However, they acknowledged that the accuracy of this value is limited since not all cases of PMDS are diagnosed and not all Müllerian duct malignancies are reported.
The development of the da Vinci surgical system has provided an invaluable tool in the approach to PMDS. To date, two successful robotic-assisted remnant excisions and orchiopexies have been reported in pediatric patients.[4,5] This article represents the third overall and the first to occur in the setting of an adult with a delayed diagnosis. In our experience, the visualization and precision provided by the robotic approach was critical to the difficult, nerve-sparing dissection. A purely laparoscopic approach has been well-documented in the literature with good success,[6,7] but we believe a robotic approach provides even more advantage when excising remnant masses.
In delayed diagnoses of PMDS, it is imperative to counsel the patient on his options including observation. Preeminent among these discussions should be the risks of impaired fertility with consideration for a semen analysis in older patients. Although the robotic approach provides an excellent tool for excision, the inherent risks of surgery remains. In the case of our patient, it was critical to avoid damaging the neurovascular bundles.
In regards to fertility, it is unclear how and if PMDS directly affects reproduction. In cases of delayed diagnoses of PMDS, patients are often infertile.[8,9] Although our patient's cryptorchidism was treated in infancy, his fertility status remains unclear. Although our patient chose to defer fertility testing, in selected individuals, the testicular sperm extraction remains a viable option.
CONCLUSION
Although PMDS is rare, it deserves important consideration due to its potential for malignant degeneration and infertility. In the excision of Müllerian remnants, the risk of malignant degeneration must be weighed against the risk of damage to critical structures in the genitourinary tract. During the management discussions, it is imperative to counsel patients on the 3.1–8.4% estimated the rate of malignancy as well as the risks of infertility. For patients who elect for surgical removal, the robot represents a novel and safe approach. Intraoperatively, the dissection should be limited to superior to the neurovascular. A semen analysis is recommended before and after excision to determine any effects on fertility.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Josso N, Belville C, di Clemente N, Picard JY. AMH and AMH receptor defects in persistent Müllerian duct syndrome. Hum Reprod Update. 2005;11:351–6. doi: 10.1093/humupd/dmi014. [DOI] [PubMed] [Google Scholar]
- 2.Farikullah J, Ehtisham S, Nappo S, Patel L, Hennayake S. Persistent Müllerian duct syndrome: Lessons learned from managing a series of eight patients over a 10-year period and review of literature regarding malignant risk from the Müllerian remnants. BJU Int. 2012;110(11 Pt C):E1084–9. doi: 10.1111/j.1464-410X.2012.11184.x. [DOI] [PubMed] [Google Scholar]
- 3.Vandersteen DR, Chaumeton AK, Ireland K, Tank ES. Surgical management of persistent müllerian duct syndrome. Urology. 1997;49:941–5. doi: 10.1016/s0090-4295(97)00104-0. [DOI] [PubMed] [Google Scholar]
- 4.Najmaldin A, Antao B. Early experience of tele-robotic surgery in children. Int J Med Robot. 2007;3:199–202. doi: 10.1002/rcs.150. [DOI] [PubMed] [Google Scholar]
- 5.Wu JA, Hsieh MH. Robot-assisted laparoscopic hysterectomy, gonadal biopsy, and orchiopexies in an infant with persistent Mullerian duct syndrome. Urology. 2014;83:915–7. doi: 10.1016/j.urology.2013.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shalaby MM, Kurkar A, Zarzour MA, Faddan AA, Khalil M, Abdelhafez MF. The management of the persistent Müllerian duct syndrome. Arab J Urol. 2014;12:239–44. doi: 10.1016/j.aju.2014.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Demir O, Kizer O, Sen V, Esen AA. Persistent Mullerian duct syndrome in adult men diagnosed using laparoscopy. Urology. 2011;78:566. doi: 10.1016/j.urology.2010.11.015. [DOI] [PubMed] [Google Scholar]
- 8.Patil V, Muktinaini S, Patil R, Verma A. Persistent Müllerian duct syndrome: A case report. Indian J Surg. 2013;75(Suppl 1):460–2. doi: 10.1007/s12262-013-0831-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Beatty JS, Bhalla VK, Hatley RM, Pipkin WL, Howell CG. Neglected cryptorchidism: Delayed recognition of persistent Müllerian duct syndrome and subsequent malignant degeneration. Urology. 2013;82:511–4. doi: 10.1016/j.urology.2013.05.020. [DOI] [PubMed] [Google Scholar]


