In the laboratory, environmental enrichment (EE) is used as a protocol to understand the functional, behavioral and molecular mechanisms that underlie neural plasticity (van Praag et al., 2000; Sale et al., 2014). In addition, it is utilized to provide supplementary resources to animals in order to maintain their well-being and to preserve the scientific validity of the study at hand (see http://www.nap.edu/catalog/12910/guide-for-the-care-and-use-of-laboratory-animals-eighth). Generally, EE is designed using a multifactorial approach incorporating novelty (e.g., alternating toys and locations of objects within the cage) alongside opportunities for physical activity (e.g., increased cage space, running wheels) and social engagement facilitated through group housing; see Figure 1. Such refinement of animal housing conditions can reduce stress and stereotyped behaviors (e.g., bar-biting, trichotillomania), that may interfere with research endpoints, by decreasing boredom and promoting species typical behaviors such as foraging, burrowing and exploration (Simpson and Kelly, 2011).
Figure 1.
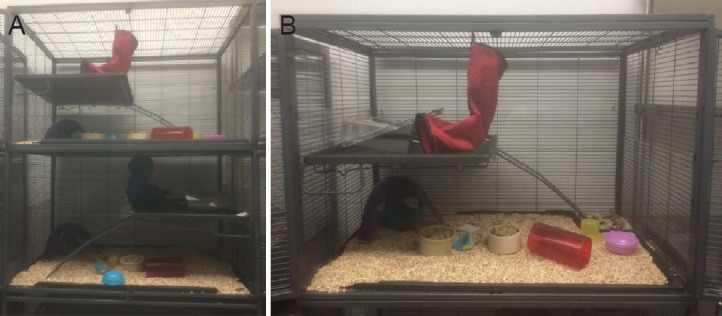
Modest environmental enrichment.
(A) Full two-level cage view, (B) one-level of a two-level cage; Critter Nation, Muncie IN. Housing design may be manipulated in multiple ways. For example, adding/removing dividers between levels to control space allotment, changing objects/toys and their location, providing access to running wheels, in addition to varying the number of cage mates. Set-up will be dependent on the overall purpose of enrichment and the controlled factors of interest (i.e., novelty, physical activity, social interaction).
Enriched laboratory housing has also been utilized to evaluate its neuroprotective and rehabilitative potential as a translational intervention for complications associated with stroke, Huntington's disease, Alzheimer's disease, age-related decline, traumatic brain injury (TBI), and even psychological stressors (Sozda et al., 2010; Ke et al., 2011; Branchi et al., 2013; Alwis and Rajan, 2014; Sale et al., 2014). In order to evaluate the ‘preventative’ effects of EE an animal is reared in this condition prior to the beginning of disease progression, or before encountering a challenge. The purpose is to determine if there is either a delay or inhibition of pathology. The ‘rehabilitative’ potential of EE is assessed by placing an animal into this housing after the initiation of the pathology, or challenge, to determine if there is a reversal of the associated adverse consequences. The benefits afforded to animals reared in EE suggest that this housing condition is akin to the clinical rehabilitation process. Despite there being a paucity of clinical trials to validate EE in either neuroprotection or recovery following human disease or trauma, it is believed that the cognitive, physical and/or social stimulation that accompany the rehabilitative processes is enriching and advantageous to patients.
Given that the specific components (i.e., novelty, physical exercise, social interaction) that make up ‘typical’ EE housing are not fully understood, animal studies have begun to isolate the contribution of each in the prevention and remediation of stress and disease. For example, communal nesting (a form of social enrichment) increases the resilience of adult male mice against a social stressor. Specifically, animals bred and reared in communal nests were protected from social instability-induced anhedonia and displayed lower plasma corticosterone levels compared to mice reared in standard laboratory housing (Branchi et al., 2013). However, during early-life these mice and their mothers were housed in enrichment together with two additional litters. Therefore, resiliency associated with the environment could be due to changes in maternal behavior, and/or the enhanced care provided by the extra dams. Indeed, EE housing has been shown to alter maternal care (Connors et al., 2015). In another study, controlling for both novelty and social variables, rats that voluntarily ran in wheels had better motor function recovery and increased hippocampal brain-derived neurotrophic factor (BDNF) levels following ischemia compared to forced exercise, involuntary muscle movement, and no-intervention groups (Ke et al., 2011). The associated motor improvements were monitored using the De Ryck's behavioral test which evaluates both forepaw and hindlimb proprioceptive and tactile placing, among other forepaw functions. Since many enriched environments include access to running wheels as part of the typical EE protocol, from a mechanistic perspective, it is important to further parse out the individual role of activity versus the other components of enrichment housing in neuroprotection and rehabilitation.
Notably, some elements of EE are reliant on the potentiated interactions between them. Following TBI motor functioning on the beam balance improved more rapidly in rats housed with a combination of social and novel enrichment, compared to rats reared with only the social or novel elements of the housing (Sozda et al., 2010). This combined complex environment also afforded protection against the associated TBI spatial learning deficits, as evaluated behaviorally in the Morris Water Maze. These mature EE animals also had smaller lesion volume three weeks following injury (Sozda et al., 2010). Again, typical complex environments are commonly made up of a conjunction of social, physical and novel enrichment. When evaluating the translational potential of EE future work will need to clarify the contribution of each component, and characterize their interactive natures, to best inform clinical interventions in terms of efficacy and cost. This aside, the success of EE in rescuing the brain from injury is most likely precipitated by the various morphological and molecular changes that underlie neuroplasticity. For example, EE has led to 1) increases in synaptogenesis and synaptic strength, 2) increased cortical thickness and overall brain weight, and 3) cell proliferation and neuronal survival, all of which have been linked to functional enhancement/maintenance of cognitive abilities and behavior (reviewed in Simpson and Kelly, 2011; Alwis and Rajan, 2014; Sale et al., 2014). These effects are promoted and maintained in part by enhanced expression/synthesis of trophic factors such as BDNF, insulin-like growth factor (IGF)-1, nerve growth factor (NGF) and neurotrophin (NT)-3. The dynamic expression of these factors are known to interact with transmitters such as serotonin, GABA, and glutamate in addition to their corresponding receptors/transporters which act as modifiers involved in neuroplasticity (Simpson and Kelly, 2011; Sale et al., 2014). Research suggests that EE is not only able to proliferate and modify new circuits but is able to functionally incorporate these changes into brain areas such as the cortex (Fan et al., 2014). Notably, some EE protocols extend beyond the traditional design and introduce other types of sensorimotor stimulation (i.e., olfactory, tactile, auditory, motor; Singhal et al., 2014) which certainly influences numerous changes across the brain.
The protective and neurorehabilitative effects of EE are most often evaluated in response to challenges that occur in later life (i.e., adulthood, senescence). Indeed, research looking at cognitive decline in aging has demonstrated that EE limits neurodegeneration in both physiological conditions (Mainardi Di et al., 2014) and in transgenic models of neurodegeneration (Lazarov et al., 2005). However, another research stream has focused this environmental intervention on pediatric and long-term consequences following early-life adversity; a small selection directly relating to neural regeneration/protection and behavior is described below. Notably, psychogenic stressors in the early pre/postnatal period increases the risk for stress-related illness behaviors, such as indicators of depression and anxiety, and cognitive impairments in rats. Rearing under typical EE conditions from postnatal day (PND) 21–60 following maternal separation (180 minutes from PND 2–14) significantly attenuated decreased sucrose preference (an indicator of anhedonia) and reversed memory disruptions (i.e., increased latency to locate a platform) in the Morris Water Maze (Hui et al., 2011). N-acetylaspartate (NAA), a marker of neuronal density and synaptic functioning closely associated with tissue glutamate, is decreased following early-life stressors in both humans and animals. Maternally-separated rats that were housed in EE had elevated NAA/creatine levels in the hippocampus that were thought to underlie the restoration of behavioral functioning in adulthood (Hui et al., 2011). Enriched housing has also been shown to reverse reductions in exploratory behavior and associated alterations in gene expression following early-life seizures in Long Evans male rats. Specifically, kainic acid-induced seizures occurring between postnatal days 20–25 were associated with decreased activity in the open field test. This was mirrored by the reduced expression of hippocampal messenger RNAs for the effector immediate early genes Arc and Homer1a, and the transcription factor Egr1. Juvenile rats housed for 10 days in typical EE, rather than standard housing, had significant elevations of each of these genes. Known for their involvement in synaptic plasticity and cell proliferation, increased expression of these genes was associated with recovery of exploratory behavior following injury (Koh et al, 2005). Pediatric TBI is also a focus for EE interventions. Rats housed in an enriched environment had enhanced spatial learning in the Morris Water Maze and a reduced lesion size following a controlled cortical impact received on postnatal day 17. The combination of buspirone (a 5-hydroxytryptamine (serotonin) receptor 1A (5-HT1A) receptor partial agonist/D2 autoreceptor antagonist) and EE resulted in better behavioral performance (i.e., faster time to hidden platform and longer percentage of time in target quadrant) in addition to smaller lesion size (Monaco et al., 2014), underscoring the role of combined pharmaceutic and environmental stimulation in facilitating the neuroplasticity of recovery.
Stemming from the evidence that EE can rescue the brain and behavior from early-life adversity we are interested in how the various components of enrichment may prevent and correct the behavioral and neural disruptions that accompany gestational and neonatal inflammatory challenges. A large area of research has focused on early-life infection and its link to schizophrenia and autism following influenza and other viral and bacterial infections (reviewed in Patterson, 2009). In brief, clinical evidence suggests that exposure to inflammation, primarily during the gestational period (i.e., maternal immune activation; MIA), increases susceptibility for these neurodevelopmental disorders. Both schizophrenia and autism are characterized by social and cognitive disruptions that are mirrored by early-life exposure to bacterial and viral mimetics during either the fetal or early postnatal period in animals. Moreover, accompanying brain abnormalities include region specific changes in glial fibrillary acidic protein (GFAP), synaptophysin, dopamine and GABA receptor expression, in addition to reductions in Purkinje cell density, reelin, and disrupted neural migration, all of which parallel the pathogenesis of autism and schizophrenia (see Patterson, 2009). Given the recent attention to these inflammation-induced disruptions in brain and behavior, and since research rarely evaluates non-invasive methods to rescue these neurodevelopmental effects, we have adopted early-inflammatory stress models using lipopolysaccharide (LPS) to evaluate the protective and rehabilitative potential of EE in rats. We have demonstrated that MIA on gestational day 11 results in disrupted social interaction in juvenile male, but not female, rats. In addition MIA was associated with elevated corticosterone and reduced glucocorticoid receptor expression in the hippocampus of males. These behavioral and neurophysiological consequences were fully prevented when rats were permanently reared (throughout their fetal period to the end of study) in a complex environment of combined social and novel enrichment. However, our EE conditions did not protect against MIA-induced reductions in hippocampal glutamate, which may account for sustained spatial discrimination impairments observed in these animals (Connors et al., 2014). The sex-specificity of the consequences that followed the MIA are notable given that autism is more commonly diagnosed in males compared to females; although, this could be related to the timing of early-life infection which should be considered. For example, in another study we sought to map out the trajectory of some behavioral and neurophysiological impairments between the juvenile and adult phases of development. In this case, both male and female rats treated as neonates on PND 3 and 5 with LPS had disrupted social interactions at adolescence, but not in adulthood (MacRae et al., 2015). However only male animals had intact spatial memory as juveniles which was impaired at maturity, following neonatal challenge. This is suggestive that the effects of inflammation in the neonatal period may impart a sex-specific risk of developing neurodegenerative processes affecting memory in later life. Again, life-long EE did not prevent spatial impairments but offered some protection against the consequences of inflammation on juvenile social behavior and reductions in glutathione (a marker of oxidative stress) in juvenile prefrontal cortex (MacRae et al., 2015). Preliminary data from our laboratory also suggests that six weeks of EE rearing beginning on PND 50 is unable to reverse the spatial deficits that accompany MIA in male rats, at least in the object-in-place task. However, combined social and novel enrichment, but not social enrichment alone, rescued the inflammatory mediated down regulation of BDNF and Ntrk2 gene expression in the hoppicampus and prefrontal cortex, respectively (Khoury and Kentner, unpublished data). It is likely that inclusion of a running wheel in our EE protocol would better address the persistent spatial deficits that follow early-life inflammation while combined opportunities for social interaction and novelty are sufficient for preventing and rescuing the other behavioral and neurophysiological complications described herein (MacRae et al., 2015; Khoury and Kentner, unpublished data). Indeed, EE conditions that include running wheels have been shown to reverse spatial impairments and reductions in NAA triggered by early-life adversity such as maternal separation (Hui et al., 2011). Moreover, running is sufficient to promote neurogenesis while EE maintains cell survival in dentate gyrus (van Praag, 1999), a structure important for learning and memory. To date, our research has shown that EE offers protection against some consequences of both fetal and neonatal exposure to LPS and a current line of inquiry continues to evaluate the components and mechanisms of EE involved in rehabilitation from MIA.
With respect to its translational potential, EE has been evaluated in autistic children with some success (Woo et al., 2015). Following a randomized sixth-month standard care + sensorimotor enrichment protocol, scores for sensory reactivity, receptive language, and the Autism Diagnostic Observation Schedule (ADOS) showed clinically significant improvements compared to standard care alone. Moreover, EE led to increased Leiter-R scores suggestive of progress in cognitive functions such as visualization and reasoning (Woo et al., 2015). The potential utility of EE in pediatric settings is also evidenced by a randomized clinical trial evaluating motor enrichment/parental engagement interventions in children at risk for cerebral palsy (Morgan et al., 2015). In this small trial, the EE intervention conferred a statistically significant advantage in the Peabody Developmental Motor Scale-2 (PDMS-2), which evaluates fine motor skills, compared to standard care. Larger trials are needed to better assess the clinical impact of this intervention. However, the results of such studies utilizing sensorimotor enrichment components (e.g., olfactory, tactile, auditory, cognitive, motor, parental interaction etc; Morgan et al., 2015; Woo et al., 2015) are beginning to provide information that will identify the specific elements of EE that may lead to clinical benefits, and for which populations. Given recent concerns of behavioral and cognitive changes following exposure to bacteria and viruses during pregnancy and the neonatal period, this ongoing research offers some assurance that the environment may be protective and could offer rehabilitative options following early-life exposure to inflammation and other developmental adversities.
The laboratory gratefully acknowledges the institutional support provided by MCPHS University.
References
- 1.Alwis DS, Rajan R. Environmental enrichment and the sensory brain: the role of enrichment in remediating brain injury. Front Syst Neurosci. 2014;8:156. doi: 10.3389/fnsys.2014.00156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Branchi I, Santarelli S, D’Andrea I, Alleva E. Not all stressors are equal: early social enrichment favors resilience to social but not physical stress in male mice. Horm Behav. 2013;63:503–509. doi: 10.1016/j.yhbeh.2013.01.003. [DOI] [PubMed] [Google Scholar]
- 3.Connors EJ, Shaik AN, Migliore MM, Kentner AC. 2014 Environmental enrichment mitigates the sex-specific effects of gestational inflammation on social engagement and the hypothalamic pituitary adrenal axis-feedback. Brain Behav Immun. 42:178–190. doi: 10.1016/j.bbi.2014.06.020. [DOI] [PubMed] [Google Scholar]
- 4.Connors EJ, Migliore MM, Pillsbury S, Shaik AN, Kentner AC. Environmental enrichment models a naturalistic form of maternal separation and shapes the anxiety response patterns of offspring. Psychoneuroendocrinology. 2015;52:153–167. doi: 10.1016/j.psyneuen.2014.10.021. [DOI] [PubMed] [Google Scholar]
- 5.Fan C, Zhang M, Shang L, Cynthia NG, Li Z, Yang Z, Chen D, Huang J, Xiong K. Short-term environmental enrichment exposure induces proliferation and maturation of doublcortin-positive cells in the prefrontal cortex. Neural Regen Res. 2014;9:318–328. doi: 10.4103/1673-5374.128231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hui JJ, Zhang ZJ, Lui SS, Xi GJ, Zhang XR, Teng GJ, Chan KC, Wu EX, Nie BB, Shan BC, Li LJ, Reynold GP. Hippocampal neurochemistry is involved in the behavioural effects of neonatal maternal separation and their reversal by post-weaning environmental enrichment: a magnetic resonance study. Behav Brain Res. 2011;217:122–127. doi: 10.1016/j.bbr.2010.10.014. [DOI] [PubMed] [Google Scholar]
- 7.Ke Z, Yip SP, Li, Zheng XX, Tong KY. The effects of voluntary involuntary and forced exercises on brain-dervied neurotrophic factor and motor function recovery: a rat brain ischemia model. PLos One. 2011;6:e16643. doi: 10.1371/journal.pone.0016643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Koh S, Chung H, Xia H, Mahadevia A, Song Y. Environmental enrichment reverses the impaired exploratory behavior and altered gene expression induced by early-life seizures. J Child Neurol. 2005;20:796–802. doi: 10.1177/08830738050200100301. [DOI] [PubMed] [Google Scholar]
- 9.Lazarov O, Robinson J, Tang YP, Hairston IS, Korade-Mirnics Z, Lee VM, Hersh LB, Sapolsky RM, Mirnics K, Sisodia SS. Environmental enrichment reduced Aβ levels and amyloid deposition in transgenic mice. Cell. 2005;120:701–713. doi: 10.1016/j.cell.2005.01.015. [DOI] [PubMed] [Google Scholar]
- 10.MacRae M, Macrina T, Khoury A, Migliore MM, Kentner AC. Tracing the trajectory of behavioral impairments and oxidative stress in an animal model of neonatal inflammation. Neuroscience. 2015;298:455–466. doi: 10.1016/j.neuroscience.2015.04.048. [DOI] [PubMed] [Google Scholar]
- 11.Mainardi M, Di Garbo A, Caleo M, Berardi N, Sale A, Maffei L. Environmental enrichment strengthens corticocortical interactions and reduces amyloid-β oligomers in aged mice. Front Aging Neurosci. 2014;6:1. doi: 10.3389/fnagi.2014.00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Monaco CM, Gebhardt KM, Chlebowski SM, Shaw KE, Cheng JF, Henchir JJ, Zupa MF, Kline AE. A combined therapeutic regimen of buspirone and environmental enrichment is more efficacious than either alone in enhancing spatial learning in brain-injured pediatric rats. J Neurotrauma. 2014;31:1934–1941. doi: 10.1089/neu.2014.3541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Morgan C, Novak I, Dale RC, Badawi N. Optimising motor learning in infants at high risk of cerebral palsy: a pilot study. BMC Pediatrics. 2015;15:30. doi: 10.1186/s12887-015-0347-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Patterson PH. Immune involvement in schizophrenia and autism: etiology pathology and animal models. Behav Brain Res. 2009;204:313–321. doi: 10.1016/j.bbr.2008.12.016. [DOI] [PubMed] [Google Scholar]
- 15.Sale A, Berardi N, Maffei L. Environmental and brain plasticity: towards an endogenous pharmacotherapy. Physiol Rev. 2014;94:189–234. doi: 10.1152/physrev.00036.2012. [DOI] [PubMed] [Google Scholar]
- 16.Simpson J, Kelly JP. The impact of environmental enrichment in laboratory rats – behavioral and neurochemical aspects. Behav Brain Resh. 2011;222:246–264. doi: 10.1016/j.bbr.2011.04.002. [DOI] [PubMed] [Google Scholar]
- 17.Singhal G, Jaehne EJ, Corrigan F, Baune BT. Cellular and molecular mechanism of immunomodulation in the brain through environmental enrichment. Front Cell Neurosci. 2014;8:97. doi: 10.3389/fncel.2014.00097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sozda CN, Hoffman AN, Olsen AS, Cheng JP, Zafonte RD, Kline AE. Empirical comparison of typical and atypical environmental enrichment paradigms on functional and histological outcome after experimental traumatic brain injury. J Neurotrauma. 2010;27:1047–1057. doi: 10.1089/neu.2010.1313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.van Praag H, Kemperman G, Gage FH. Neural consequences of environmental enrichment. Nat Rev Neurosci. 2000;1:191–198. doi: 10.1038/35044558. [DOI] [PubMed] [Google Scholar]
- 20.van Praag H, Kempermann G, Gage FH. Running increases cell proliferation and neurogenesis in the adult mouse dentate gyrus. Nat Neurosci. 1999;2:266–270. doi: 10.1038/6368. [DOI] [PubMed] [Google Scholar]
- 21.Woo CC, Donnelly JH, Steinberg-Epstein R, Leon M. Environmental enrichment as a therapy for autism: a clinical trial replication and extension. Behav Neurosci. 2015;129:412–422. doi: 10.1037/bne0000068. [DOI] [PMC free article] [PubMed] [Google Scholar]


