Abstract
Background
Impacted third molar removal is a routine procedure in oral and maxillofacial surgery. Platelet-rich fibrin (PRF) is a second generation platelet concentration which is produced by simplified protocol. The aim of this study was to assess the effectiveness of PRF in the healing process by evaluating the changes in pain and swelling after third molar surgery.
Methods
Fifty-six patients (23 male, 33 female) who provide the inclusion criteria were selected to participate in this study. The evaluation of the facial swelling was performed by using a horizontal and vertical guide. The pain was evaluated in the postoperative period using a visual analog scale (VAS) of 100 mm.
Results
Horizontal and vertical measurements showed more swelling at the control side (without PRF) in 3th day postoperatively (p < 0.05). There were no statistically significant differences regarding pain among the groups.
Conclusion
As a conclusion, PRF seems to be effectiveness on postoperative horizontal swelling after third molar surgery. PRF could be used on a routine basis after third molar extraction surgery.
Keywords: PRF, Third molar surgery, Pain, Swelling
Background
The removal of impacted third molars is common oral surgical procedure. Surgical extraction of third molars is often accompanied by pain, swelling, trismus, and general oral dysfunction during the healing period [1–5]. Careful surgical technique and scrupulous perioperative care can minimize the frequency of complications and limit their severity [2].
Various pharmacological and/or extraction methods have been used for maintaining patients social activities. These include non-steroid anti-inflammatory drugs (NSAIDs), laser treatment, steroids and ultrasound [6–9]. However, the amount and intensity of edema, pain and trismus occurring after surgical extraction cannot be eliminated completely.
Platelet-rich fibrin (PRF) is a second generation platelet concentration which is produced by simplified protocol. PRF consists of a fibrin matrix polymerized in a tetramolecular structure, the incorporation of platelets, leukocyte, and cytokines, and the presence of circulating stem cells [10–12]. There are many studies showing accelerating wound healing of PRF in periodontal defects, cyst cavities and sinus floor augmentation in the literature [13–15]. There are limited studies on the effects of PRF on postoperative pain and swelling [16, 17].
The aim of this study is to evaluate the incidence and severity of postoperative swelling and pain following mandibular third molar surgery using PRF as a healing material in the extraction sockets. The null hypothesis tested was that PRF would effect the postoperative swelling and pain positively.
Method
This study was carried in two different Oral and Maxillofacial Surgery Departments. Institutional ethics committee’s approval was obtained for the protocol of the study. [Kırıkkale University, Faculty of dentistry local ethic committee 09/03 (15.04.2013)]. Based on previously treated trial cases we conducted a power analysis (Power and Precision software, Biostat, Englewood, NJ, USA). The findings indicated a minimum sample size of n = 50, based on an α of 5 % and a power of 80 %. Considering a possible loss of about 10 % of patients, we used 56 participants.
After preoperative evaluation and obtaining written informed consent, total of 56 patients (23 male, 33 female) ranging from 18-28 years who could follow postoperative instructions were selected for the study.
Clinical inclusion criteria were as follows:
Bilateral fully impacted third molars which have the same degree of surgical difficulty comparing one side with the other (Fig. 1).
No preexisting medical conditions or no use of medication that would influence or alter wound healing
No active pathology associated with the third molars
No temporomandibular joint disorder history that would affect the pain sensation after surgery.
Fig. 1.

PRF was prepared to place into extraction socket
Fifty-six patients (23 male-, 33 female) who met the inclusion criteria were selected to participate in this study. Pell and Gregory [18] classification was used to determine the difficulties of the patients included in the study. Of these 56 patients distribution of the classification was as: 20 horizontal, 15 mezioangular, 21 vertical. PRF and the technique were explained to patient and informed consent was taken from all patients.
Patients underwent surgical treatment in accordance with the rules of antisepsis and asepsis. All bilateral third molars surgeries were performed by a single experienced operator in each centers. Prior to the extractions, 10 ml of venous blood was collected from each patient by a surgical nurse and was placed in glass-coated plastic tubes. Tubes were transferred to a centrifuge device and centrifuged for 10 min at 3000 rpm according to Choukroun et al [14].
Following centrifugation, PRF was dissected approximately 2 mm below its connection to the red corpuscle beneath to include remaining platelets, which have been proposed to localize below the junction between PRF and the red corpuscle. Then PRF was squeezed between gauzes to transform into a membrane (Fig. 2).
Fig. 2.

Bilateral impacted third molars which have the same degree of surgical difficulty comparing one side with the other
All patients underwent bilateral removal of 3rd molar in single appointment that were the same degree of surgical difficulty. Mandibular and buccal blocks were administered using articaine containing 1:200,000 epinephrine (Ultracain DS; Aventis, Istanbul, Turkey). Horizontal and vertical incisions were performed and a full-thickness mucoperiosteal flap was raised and the tooth was removed with elevators. Following the extraction, the socket was thoroughly irrigated so that pathologic tissue (eg, granulation tissue), follicular remnants, and bony spicules were removed from the cavity (Fig. 3). Following that PRF was placed in the socket on one side which was chosen randomly by coin toss and other side was taken as control group (Fig. 4). Both extraction cavities were primarily closed with 3-4 interrupted sutures using 3.0 silk sutures. Postoperatively, amoxicillin 1000 mg (Alfoxil 1gr; Fako, Istanbul, Turkey) twice daily, paracetamol 500 mg (Vermidon 500 mg; Sandoz, Istanbul, Turkey) thrice daily and chlorhexidine mouthwash thrice daily were administered to all patients for a week.
Fig. 3.
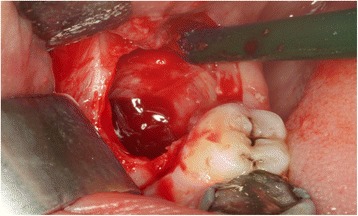
Extraction socket
Fig. 4.
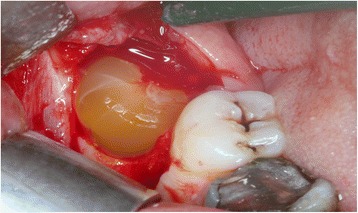
PRF placed into extraction socket on one side
Patients were blind to the knowledge of PRF placed side in order not to affect visual analog scale (VAS) scores. The pain was evaluated in the postoperative period using a VAS of 100 mm. After the surgery, the patients were instructed to note their postoperative discomfort and/or pain on the scale, which was designed as 0 indicating no pain whereas 100 indicating the worst ever experienced . The evaluation of the postoperative pain was carried out at 24 h, 72 h and seven days after the procedure.
The evaluation of the facial swelling was done by using a horizontal and vertical guide with a flexible ruler. For horizontal guide two points marked at the ear tragus and buccal comissura, and the distance between them was measured and recorded. The same procedure was performed for vertical guide at lateral chantus of the eye and gonion. The evaluation of the postoperative facial swelling was carried out at 24 th hours, 72th hours and seventh day after the procedure. The postoperative evaluations were performed by surgeons that were blinded to the operative procedures, in order to eliminate unwanted bias. The evolution of swelling was evaluated by subtracting the value obtained at each postoperative period by the obtained at baseline [19].
Statistical analysis was performed using the software program SPSS 20.0 (SPSS 20.0 for Windows; SPSS Inc., Chicago, IL, USA), at a significance level of α = 0.05. For analysis of swelling the Shapiro–Wilk test was used to evaluate the distribution of the data (normal or non-normal), the Wilcoxon test for paired samples was used since the data were not normally distributed. Regarding the pain statistical analysis were performed by using one–way analysis of variance (ANOVA). If there were difference between the measurements, the data were analyzed by the Paired Sample test.
Results
Statistically significant differences were observed in first and third days horizontal measurements between PRF and control side (p < 0.05). And more swelling was seen at the control side. The pain scores were measured by using VAS. There were no statistically significant differences observed between groups (Tables 1, 2 and 3).
Table 1.
Results of Postoperative Swelling (horizontal measurements)
| Horizontal swelling | |||
|---|---|---|---|
| Postoperative evaluation times | Control side Mean(SD) | PRF side Mean (SD) | P- value |
| 1st day | 4.64 (4.27) | 3.28 (3.02) | 0.041* |
| 3rd day | 3.62(3.51) | 1.83(2.52) | 0.001* |
| 7th day | 0.73 (1.89) | 0.57 (1.87) | 0.634 |
*statistically significant differences amongs groups
Table 2.
Results of Postoperative Swelling (vertical measurements)
| Vertical swelling | |||
|---|---|---|---|
| Postoperative evaluation times | Control side Mean(SD) | PRF side Mean (SD) | P- value |
| 1st day | 5.92 (7.42) | 5.19 (8.12) | 0.306 |
| 3rd day | 4.00 (6.42) | 3.42 (6.55) | 0.589 |
| 7th day | 1.28 (3.95) | 0.82 (3.81) | 0.061 |
Table 3.
Results of Postoperative pain
| VAS scores | |||
|---|---|---|---|
| Postoperative evaluation times | Control side Mean(SD) | PRF side Mean (SD) | P- value |
| 1st day | 42.84 (29.77) | 47.16 (30.59) | 0.413 |
| 3rd day | 26.48 (30.36) | 25.50 (29.95) | 0.296 |
| 7th day | 9.41 (16.57) | 10.21 (19.75) | 0.503 |
Discussion
The surgical removal of impacted third molars cause trauma of the soft tissue and bony structures in the oral cavity. The postoperative signs and symptoms of pain, edema and limited mouth opening due to muscle spasm might occur [20, 21].
Fibrin glue [also known as fibrin sealant or fibrin adhesive (platelet rich plasma, PRF)] is a protein based product developed for tissue hemostasis and sealing. Platelet–based materials combine plasma proteins and platelets [22].
PRF described by Choukrouns is prepared naturally without addition of thrombin, and it is hypothesized that PRF has a natural fibrin framework and can protect growth factors from proteolysis [13]. PRF releases high quantities of three main growth factors transforming growth factor β-1 (TGF beta-1), platelet-derived growth factor AB (PDGF-AB), vascular endothelial growth factor (VEGF), and an important coagulation matricellular glycoprotein (thrombospondin-1, TSP-1) during 7 days. Apart from these PRF also secrete EGF, FGF, and three important proinflammatory cytokines- IL-1b, IL-6, and TNF-α which obtained with a simple centrifugation procedure, to stimulate several biological functions such as chemotaxis, angiogenesis, proliferation, differentiation, modulation, thereby representing a possible therapeutic device for a more rapid and effective regeneration of hard and soft tissues [14, 16, 17]. Platelets also play a role in host defense mechanisms at the wound site, by delivering signaling peptides which attract macrophage cells. Platelet concentrates may contain small amounts of leukocytes that synthesize interleukins involved in the non-specific immune reaction [22].
Recently the use of PRF has been proposed as an aid for enhancing regeneration of osseous and epithelial tissues in oral surgery. Several in vitro studies, animal experiments and clinical trials suggested that platelet concentrates may effectively trigger stimulation of osseous and soft tissue regeneration, and reduce inflammation, pain and side effects. The clinical efficacy of PRF in oral surgical procedures is debated as contrasting results have been reported in different clinical procedures [22–25].
Use of PRF in oral cavity has been implicated in different procedures such as extraction socket preservation, intrabony defects, sinus augmentation, and sinus lift procedures for implant placement, bone augmentation, root coverage procedures, and healing in donor site with successful results [22].
Recently some studies evaluated the effect of platelet rich plasma (PRP) to the extraction sockets healing and postoperative complications [26, 27]. Several studies showing animal experiments and clinical trials showed that PRF might affect the regeneration of soft and hard tissue, healing and reduce the side effects [22, 24].
Zhang et al [25] evaluate the influence of PRF on bone regeneration in sinus augmentation. After a healing period of 6 months no statistical differences found between PRF and the control groups.
According to a study by Choukroun et al. a cystic cavity filled with PRF would be totally healed in 2 months instead of the 6 to 12 months required for physiologic healing [22].
There are some controversies in the literature. A study evaluating the effectiveness of PRF in the treatment of intrabony defects of chronic periodontitis patients, thirty-two defects were treated with PRF or a conventional open flap debridement alone. They showed that PRF can be used in the treatment of intrabony defects of chronic periodontitis patients [28]. Lee et al [24] used the PRF for restoration of peri-implant defects in rabbit. Their results showed the possibility of PRF use in bone regeneration.
Contradictory, Aroca et al [15] evaluated that the claimed benefits for soft tissue wound healing induced by PRF membranes and they reported that their results failed to show any beneficial effect of PRF membrane in terms of root coverage or short term wound healing for the treatment of multiple gingival recessions.
Mozatti et al [26] evaluated that the effects of PRP on inflammation process, wound healing, pain and swelling after third molar extraction. They reported that PRP was more effective on wound healing in the extraction socket. Our results supported that PRF was more effective on the swelling in the third day after third molar surgery.
Alissa et al [27] evaluated the influence of PRP on healing of extraction sockets. They reported that PRP may have some benefits in reducing complications such as alveolar osteitis, swelling, pain and improving healing of soft tissue.
Kumar et al [17] investigated the effect of platelet-rich fibrin (PRF) on postoperative pain, swelling, trismus, periodontal healing they concluded that case group had less pain, swelling, and trismus on the first postoperative day compared with the control group. Their results also showed increased and faster periodontal healing in the case group.
In another study by Singh et al [16] they concluded that use of PRF after bilaterally third molar surgeries resulted in less pain compared to control side.
In the present study, PRF was used after third molar extraction, swelling and pain were evaluated. Statistically significant difference was found concerning first and third day horizontal measurements of PRF and control sides with more swelling at the control side (p < 0.05). These results are in accordance with Kumar et al [17].
The present study found no significant difference between PRF and control sides in terms of pain which is similar to Singh et al [16], but different from Kumar et al [17] study where the control and PRF groups consisted of different patients. As the results of the study the null hypothesis was partially rejected since there was no positive effect of PRF seen on the pain.
There are some limits to our study; the present study was conducted on bilaterally removed third molars at the same session the results of pain might have been influenced by the control side. Also the use of 3-D optical scanner for the measurements of facial swelling might have given more precise recordings however the funding of the study did not support such expenses. We recommend that further studies investigating this manner should consider the mentioned limitations of the present study.
Conclusion
As a conclusion, PRF seems to be efficient on postoperative horizontal swelling after third molar surgery. PRF could be used for control swelling after third molar extraction surgery. Studies with a larger sample that will need a bilateral third molar removal that will be extracted in different sessions with a longer follow-up is warranted to obtain a more statistically meaningful results with respect to bone regeneration.
Abbreviations
- NSAID
Non-steroid anti-inflammatory drugs
- PRF
Platelet-rich fibrin
- PRP
Platelet-rich plasma
- VAS
Visual analog scale
Footnotes
Competing interest
All authors declare that they have no competing interests.
Authors’ contributions
All authors contributed extensively to the work presented in this paper. OO searched the articles for the review, drafted the manuscript and wrote the manuscript. FS and NE have performed the surgeries. IDK and AA performed the postoperative measurements. IDK and FA designed the study and helped in wrote the manuscript. AA and HHT drafted the manuscript and reviewed it critically. UT revised the final version of the manuscript. All authors read and approved the final version of the manuscript.
References
- 1.Koerner KR, Medlin KE. Clinical procedures for third molar surgery. 2. South Sheridan: PennWell; 1995. [Google Scholar]
- 2.Szmyd L. Impacted teeth. Dent Clin North Am. 1971;15:299–318. [PubMed] [Google Scholar]
- 3.Nageshwar Comma incision for impacted third molars. J Oral Maxillofac Surg. 2002;60(12):1506–1509. doi: 10.1053/joms.2002.36152. [DOI] [PubMed] [Google Scholar]
- 4.Fonseca RJ, Frost DE, Hersh EV, Levin LM. Oral and maxillofacial surgery: anaesthesia/dentoalveolar surgery/office management. 1. Philadelphia: Saunders; 2001. [Google Scholar]
- 5.Kirk DG, Liston PN, Tong DC, Love RM. Influence of two different flap designs on incidence of pain, swelling, trismus, and alveolar osteitis in the week following third molar surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104:e1–e6. doi: 10.1016/j.tripleo.2007.01.032. [DOI] [PubMed] [Google Scholar]
- 6.Bagan JV, Lopez JS, Valencia E. Clinical comparison of dexketoprofen trometamol and dipyrone in postoperative dental pain. J Clin pharmacol. 1998;38:55–64. [PubMed] [Google Scholar]
- 7.Björnsson GA, Haanaes HR, Skoglund LA. Naproxen 500 mg bid versus acetaminophen 1000 mg qid: effect on swelling and other acute postoperative events after bilateral third molar surgery. J Clin Pharmacol. 2003;43:849–858. doi: 10.1177/0091270003255361. [DOI] [PubMed] [Google Scholar]
- 8.Spilka CJ. The placebo of corticosteroids and antihistamines in oral surgery. Oral Surg Oral Med Oral Pathol. 1961;14:1034–1042. doi: 10.1016/0030-4220(61)90493-5. [DOI] [Google Scholar]
- 9.Skjelbred P, Løkken P. Post-operative pain and inflammatory reaction reduced by injection of a corticosteroid. A controlled trial in bilateral oral surgery. Eur J Clin Pharmacol. 1982;21(5):391–6. doi: 10.1007/BF00542325. [DOI] [PubMed] [Google Scholar]
- 10.Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J, et al. Platelet-rich fibrin (PRF): A second-generation platelet concentrate.Part III: Leucocyte activation: A new feature for platelet concentrates? Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:E51–5. doi: 10.1016/j.tripleo.2005.07.010. [DOI] [PubMed] [Google Scholar]
- 11.Gaultier F, Navarro G, Donsimoni JM, Dohan D. Platelet concentrates. Part 3: Clinical applications. Implantodontie. 2004;13:3–11. doi: 10.1016/j.implan.2003.11.002. [DOI] [Google Scholar]
- 12.Simonpieri A, Choukroun J, Girard MO, Ouaknine T, Dohan D. Immediate post-extraction implantation: interest of the PRF. Implantodontie. 2004;13:177–89. doi: 10.1016/j.implan.2004.06.004. [DOI] [Google Scholar]
- 13.Simonpieri A, Del Corso M, Sammartino G, Dohan Ehrenfest DM. The Relevance of Choukroun’s Platelet-Rich Fibrin and Metronidazole During Complex Maxillary Rehabilitations Using Bone Allograft. Part I: A New Grafting Protocol. Implant Dent. 2009;18:102–111. doi: 10.1097/ID.0b013e318198cf00. [DOI] [PubMed] [Google Scholar]
- 14.Choukroun J, Adda F, Schoeffler C, Vervelle A. Une opportunité en paro-implantologie: le PRF. Implantodontie. 2001;42:55–62. [Google Scholar]
- 15.Aroca S, Keglevich T, Barbieri B, Gera I, Etienne D. Clinical evaluation of a Modified Coronally Advanced Flap Alone or in Combination With a Platelet-Rich Fibrin Membrane for the Treatment of Adjacent Multiple Gingival Recessions: A 6-Month Study. J Periodontol. 2009;80:244–52. doi: 10.1902/jop.2009.080253. [DOI] [PubMed] [Google Scholar]
- 16.Singh A, Kohli M, Gupta N. Platelet rich fibrin: a novel approach for osseous regeneration. J Maxillofac Oral Surg. 2012;11(4):430–4. doi: 10.1007/s12663-012-0351-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kumar N, Prasad K, Ramanujam L, K R, Dexith J, Chauhan A. Evaluation of Treatment Outcome After Impacted Mandibular Third Molar Surgery With the Use of Autologous Platelet-Rich Fibrin: A Randomized Controlled Clinical Study. J Oral Maxillofac Surg. 2014 Dec 13. doi: 10.1016/j.joms.2014.11.013. [Epub ahead of print] [DOI] [PubMed]
- 18.Pell GJ, Gregory BT. Impacted mandibular third molars: classification and modified techniques for removal. Dent Digest. 1933;39:330–338. [Google Scholar]
- 19.Alcântara CE, Falci SG, Oliveira-Ferreira F, Santos CR, Pinheiro ML. Pre-emptive effect of dexamethasone and methylprednisolone on pain, swelling, and trismus after third molar surgery: a split-mouth randomized triple-blind clinical trial. Int J Oral Maxillofac Surg. 2014;43:93–8. doi: 10.1016/j.ijom.2013.05.016. [DOI] [PubMed] [Google Scholar]
- 20.Grossi GB, Maiorana C, Garramone RA, Borgonovo A, Creminelli L, Santoro F. Assesing postoperative discomfort after third molar surgery:A prospective study. J Oral Maxillofacial Surg. 2007;65:901–17. doi: 10.1016/j.joms.2005.12.046. [DOI] [PubMed] [Google Scholar]
- 21.Baqain Z, Karaky AA, Sawair F, Khraisat A, Duaibis R, Rajab LD. Frequency estimates and risk factors for post operative morbidity after third molar removal:A prospective cohort study. J Oral Maxillofac Surg. 2008;66(11):2276–83. doi: 10.1016/j.joms.2008.06.047. [DOI] [PubMed] [Google Scholar]
- 22.Choukroun J, Diss A, Simonpieri A, Girard MO, Schoeffler C, Dohan SL, et al. Platelet-rich fibrin (PRF): A second-generation platelet concentrate.Part IV: Clinical effects on tissue healing. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:E56–60. doi: 10.1016/j.tripleo.2005.07.011. [DOI] [PubMed] [Google Scholar]
- 23.Su CY, Kuo YP, Tseng YH, Su CH, Burnouf T. In vitro release of growth factors from platelet-rich fibrin (PRF): a proposal to optimize the clinical applications of PRF. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108(1):56–61. doi: 10.1016/j.tripleo.2009.02.004. [DOI] [PubMed] [Google Scholar]
- 24.Lee JW, Kim SG, Kim JY, Lee YC, Choi JY, Dragos R, et al. Restoration of a peri-implant defect by platelet- rich fibrin. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2012;113(4):459–63. doi: 10.1016/j.tripleo.2011.03.043. [DOI] [PubMed] [Google Scholar]
- 25.Zhang Y, Tangl S, Huber CD, Lin Y, Qiu L, Rausch-Fan X. Effects of Choukroun’s platelet-rich fibrin on bone regeneration in combination with deproteinized bovine bone mineral in maxillary sinus augmentation:A histological and histomorphometric study. J Cranio-Maxillofac Surg. 2012;40(4):321–8. doi: 10.1016/j.jcms.2011.04.020. [DOI] [PubMed] [Google Scholar]
- 26.Mozzatti M, Martinasso G, Pol R, Polastri C, Cristiano A, Muzio G, et al. The impact of plasma rich in growth factors on clinical and biological factors involved in healing processes after third molar extraction. J Biomed Mater Res. 2010;95(3):741–6. doi: 10.1002/jbm.a.32882. [DOI] [PubMed] [Google Scholar]
- 27.Alissa R, Esposito M, Horner K, Oliver R. The influence of platelet-rich plasma on the healing of extraction sockets: an explorative randomised clinical trial. Eur J Oral Implantol. 2010;3(2):121–34. [PubMed] [Google Scholar]
- 28.Thorat MK, Pradeep AR, Pallavi B. Clinical effect of autulogous platelet-rich fibrin in the treatment of intra-bony defects : a controlled clinical trial. J Clin Periodontol. 2011;38:925–932. doi: 10.1111/j.1600-051X.2011.01760.x. [DOI] [PubMed] [Google Scholar]


