Summary
Azathioprine, a purine analogue that competitively inhibits the biosynthesis of purine nucleotides, is used in a wide range of conditions. Although its side-effects are well known, cardiac side effects like paroxysmal atrial fibrillation (AF) are based on only a few case reports. We describe here the case of a 55-year-old woman with primary biliary cirrhosis who presented a first-detected, symptomatic AF 2 h after azathioprine therapy which resolved after discontinuation of the drug with no predisposing factors for supraventricular arrhythmias (systemic hypertension, diabetes or coronary artery disease). The temporal coincidence of atrial fibrillation and azathioprine intake and disappearance of the AF episode after discontinuation of therapy allows us to suggest an intrinsic pro-arrhythmic effect of azathioprine. Therefore, physicians should be aware of this problem when this drug is administered.
Keywords: Azathioprine, atrial fibrillation, cardiac side effects
1. Introduction
Azathioprine, a purine analogue that competitively inhibits the biosynthesis of purine nucleotides, is used in a wide range of conditions such as inflammatory bowel disease, rheumatoid arthritis, systemic lupus erythematosus, solid organ transplantation and vasculitis. Azathioprine is quickly and nearly completely absorbed from the digestive tract. Bioavailability varies greatly between individual patients, between 30 and 90%, because the drug is partly inactivated in the liver. The peak serum levels occur roughly 2 h after ingestion, and the average half-life is 26 to 80 min for azathioprine and 3 to 5 h for drug plus metabolites. Azathioprine is extensively metabolized, and only about 2% is excreted, unchanged, in the urine, 20–30% is bound to plasma proteins while circulating in the bloodstream. The side effects of azathioprine are well-documented and include dose dependent myelosuppression and hepatotoxicity as well as a dose-independent hypersensitivity syndrome ranging from isolated fever, and rash to multi-organ failure, which is relatively less frequent (1). Cardiovascular side effects have included rare cases of hypotension, including cardiogenic shock (2). A few cases of atrial fibrillation (AF) induced by this drug have been reported (3,4) although causality is unknown. We report a case of a 55-year-old woman with primary biliary cirrhosis who developed a first-detected, symptomatic AF after azathioprine therapy.
2. Case repor
A 55-year-old woman presented to the emergency department complaining of palpitation lasting for 4 h, which began 2 h after 50 mg of azathioprine therapy. Her body weight was 75 kg and her height was 170 cm. Physical examination revealed a blood pressure of 130/80 mmHg, clear lungs and normal heart sounds. The temperature was 36.4°C. There was no history of fever, illicit drugs, alcohol or exposure to toxic chemicals. Electrocardiographic (ECG) examination showed atrial fibrilation of 130 beats/min without conduction abnormalities or ST-T changes (Figure 1) Trans-thoracic echocardiography showed normal left ventricular size and function with no valvular abnormalities and normal left atrial para-sternal diameter of 39 mm and left ventricular ejection fraction of 65%. Chest radiograph and routine laboratories including cardiac enzymes were normal. Hematological examination, urinary analysis and thyroid function were all normal. Her medical history included primary biliary cirrhosis for 2 years. The patient's medications included ursodeoxycholic acid, and prednisolone and had not changed for many months except for the recent addition of azathioprine 2 h before her arrival at the emergency department. She reported that her complaints started immediately after azathioprine therapy which was the first dose given for primary biliary cirrhosis. Metoprolol i.v. was administered immediately with resultant conversion to normal sinus rhythm within 1.5 h (Figure 2). Patient was discharged without antiarrhythmic medication. The therapy with azathioprine was discontinued in view of the suspicion of its pro-arrhythmic effect. After stopping azathioprine the patient's condition markedly improved. A 24 h ambulatory ECG monitoring revealed no cardiac arrhythmias as well as during the control examination one month after the attack of AF. No other episodes were reported and the patient was asymptomatic without medication after 3 months of follow-up. Other treatments were not changed.
Figure 1.
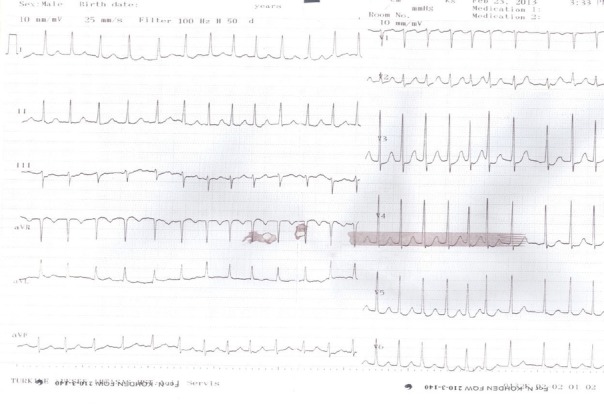
Examples of ECG showing that AF developed after azathioprine intake. ECG, electrocardiographic; AF, atrial fibrillation.
Figure 2.
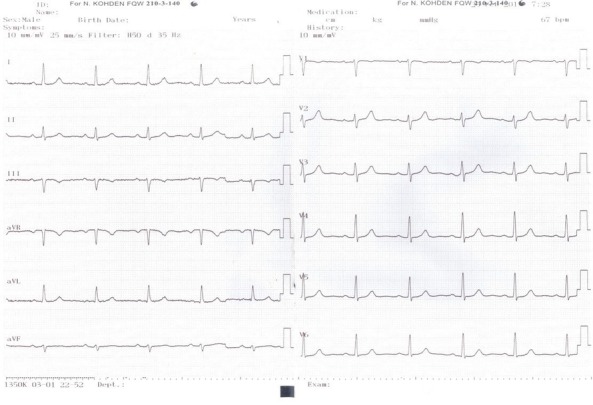
Complete restoration to sinus rhythm using IV metoprolol after discontinuation of Azothiophirin.
3. Discussion
AF is the most common arrhythmia treated in clinical practice and the most common arrhythmia for which patients are hospitalized. AF is associated with risk of stroke, and all-cause mortality and development of heart failure. Acute temporary causes of AF include alcohol abuse, excessive coffee intake, surgery, pericarditis, myocarditis, and pulmonary embolism. Medications also have been associated with the induction of AF both in case reports and clinical trials (5). This is one report of a first-detected, symptomatic AF probably due to cardiac toxicity of azathioprine.
A pro-arrhythmic effect of azathioprine is strongly suggested by the temporal coincidence of atrial fibrilation and azathioprine intake in our patient with no cardiovascular diseases. The AF episode was closely related in time to treatment with azathioprine that occurred 2 h after drug intake. We couldn't determine any other precipitating factor beyond the azathioprine therapy as a cause for the arrhythmia. The complete symptoms resolution and the disappearance of AF episodes after azathioprine discontinuation while other drugs were continued is in line with its pharmacokinetic. Since average plasma half-life is 26 to 80 min for azathioprine the precipitating role of this drug is strongly suspected because arrhythmic episodes occurred 2 h after azathioprine and no other predisposing clinical factors, such as electrolyte imbalance, neuro-autonomic dysfunction, thyrotoxicosis or subclinical hyperthyroidism, pulmonary embolism, hypertensive crisis, alcohol abuse, or excessive coffee intake were involved. Although several case reports and case-control studies have associated this condition with the use of systemic corticosteroids, azathioprine seems more likely as a cause for the arrhythmia since no episodes occurred when this drug was discontinued and the other drugs such as prednisolone used in our patient were continued.
We have found three other similar reports of pro-arrhythmic cardiac toxicity like AF during azathioprine use. A case of fast AF induced by treatment of psoriasis with azathioprine had been reported (3). However alcohol consumption and fever could be the possible trigger of atrial fibrilation in that case. In another case in ulcerative colitis Cassinotti et al. reported very rapid appearance of AF after 2 h of drug administration as in our case (4). Other cardiac effects described in the literature are hypotension, tachycardia and some forms of shock in the context of hypersensitivity reactions occurring within 4 weeks of starting azathioprine (2).
Mechanism of arrhythmia seen during treatment with azathioprine is unknown. All drug induced AF is reported to have the following main mechanisms: adrenergic or vagal stimulation, direct cardiotoxicity, changing atrial conduction, refractoriness or automaticity, coronary vasoconstriction/ischemia, and electrolyte disturbances (5). In the literature there have been some reports focused on effects of azathioprine on ion channels which may be the cause of cardiac rhythm disturbance (6,7). But they failed to show its electrophysiological effects by modulating ionic transport across cellular membranes. The pathophysiology of rhythm dysfunction during treatment with azathioprine by the way mentioned above remains to be established.
This case highlights an unusual causal relationship between azathioprine and AF. We conclude that AF is an unusual, but potentially dangerous, side-effect of azathioprine therapy. The arrhythmia should be suspected whenever patients complain of dyspnea and palpitations beginning immediately after treatment. In these cases, the treatment for AF consists of anti-arrhythmic drugs in order to obtain a sinus rhythm or control the heart rate. It is important for physicians using azathioprine to keep in mind this serious but reversible adverse effect.
References
- 1. Patel AA, Swerlick RA, McCall CO. Azathioprine in dermatology: The past, the present, and the future. J Am Acad Dermatol. 2006; 55: 369-389. [DOI] [PubMed] [Google Scholar]
- 2. Brown G, Boldt C, Webb JG, Halperin L. Azathioprine-induced multisystem organ failure and cardiogenic shock. Pharmacotherapy. 1997; 17: 815-818. [PubMed] [Google Scholar]
- 3. Dodd HJ, Tatnall FM, Sarkany I. Fast atrial fibrillation induced by treatment of psoriasis with azathioprine. Br Med J (Clin Res Ed). 1985; 291: 706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Cassinotti A, Massari A, Ferrara E, Greco S, Bosani M, Ardizzone S, Bianchi Porro G. New onset of atrial fibrillation after introduction of azathioprine in ulcerative colitis: Case report and review of the literature. Eur J Clin Pharmacol. 2007; 63: 875-878. [DOI] [PubMed] [Google Scholar]
- 5. van der Hooft CS, Heeringa J, van Herpen G, Kors JA, Kingma JH, Stricker BH. Drug-induced atrial fibrillation. J Am Coll Cardiol. 2004; 44: 2117-2124. [DOI] [PubMed] [Google Scholar]
- 6. Frost L, Danielsen H, Dørup I, Kjaer T, Pedersen EB. Skeletal muscle magnesium content during cyclosporin and azathioprine treatment in renal transplant recipients. Nephrol Dial Transplant. 1993; 8: 79-83. [DOI] [PubMed] [Google Scholar]
- 7. Rabini RA, Testa I, Corvetta A, Lombardello M, Polenta M, Danieli G, Mazzanti L. Cyclosporine effect on sodium and potassium transport across erythrocytes in rheumatoid arthritis. Scand J Rheumatol. 1990; 19: 356-362. [DOI] [PubMed] [Google Scholar]


