Abstract
A nonenzymatic reaction between reducing sugars and amino groups of proteins, lipids and nucleic acids contributes to the aging of macromolecules and subsequently alters their structural integrity and function. This process has been known to progress at an accelerated rate under hyperglycemic and/or oxidative stress conditions. Over a course of days to weeks, early glycation products undergo further reactions such as rearrangements and dehydration to become irreversibly cross-linked, fluorescent and senescent macroprotein derivatives termed advanced glycation end products (AGEs). There is a growing body of evidence indicating that interaction of AGEs with their receptor (RAGE) elicits oxidative stress generation and as a result evokes proliferative, inflammatory, thrombotic and fibrotic reactions in a variety of cells. This evidence supports AGEs’ involvement in diabetes- and aging-associated disorders such as diabetic vascular complications, cancer, Alzheimer’s disease and osteoporosis. Therefore, inhibition of AGE formation could be a novel molecular target for organ protection in diabetes. This report summarizes the pathophysiological role of AGEs in vascular complications in diabetes and discusses the potential clinical utility of measurement of serum levels of AGEs for evaluating organ damage in diabetes.
INTRODUCTION
Diabetes is a global health challenge. In the recent report in the IDF Diabetes Atlas, the prevalence and number of diabetes cases in the world are estimated to be 8.3% and 387 million, and one person dies from diabetes every 7 s (1). Although diabetic vascular complications, including coronary heart disease and apoplexy, could mainly account for disabilities and high mortality rate in patients with diabetes (1,2), the risk of other aging-associated disorders such as cancer, Alzheimer’s disease and osteoporosis is also increased in diabetic subjects (3–6). As a result, average life span is reduced by more than 20 years in middle-aged people with type 1 diabetes and by up to 10 years in middle-aged, type 2 diabetic patients compared with nondiabetic subjects (7–9). The recent report of Emerging Risk Factors Collaboration showed that 40-year-old diabetic subjects without known cardiovascular disease (CVD) at the time of enrollment died about 6.3 years earlier than nondiabetic subjects (3). Furthermore, cumulative hyperglycemic exposure and subsequently enhanced accumulation of advanced glycation end products (AGEs) have been shown to contribute to the development and progression of these diabetes- and aging-related disorders (2,4–6). Therefore, inhibition of AGE formation could be a novel molecular target for various devastating and life-threatening disorders. In this report, we review the progress of research on AGEs from 1994 to the present, especially focusing on vascular complications in diabetes, and we discuss how our studies in the field of AGEs have been influenced by and contributed to the article published in Molecular Medicine in 2001 (10). Moreover, we would like to refer to how the information in the article may alter the diagnosis and treatment of diabetic vascular complications now or in the future.
METABOLIC MEMORY
The Diabetes Control and Complications Trial–Epidemiology of Diabetes Interventions and Complications (DCCT-EDIC) research has revealed that beneficial effects of intensive therapy on microvascular complications in type 1 diabetic patients persist for 14–18 years after the DCCT, despite deterioration of blood glucose control (11–13). Furthermore, intensive glycemic control during the DCCT resulted in decreased progression of intima-media thickness and subsequently reduced the risk of nonfatal myocardial infarction, stroke or death from CVD by 57% 11 years after the end of the trial (14–16). Recently, original intensive therapy for 6.5 years has been shown to yield benefits on all-cause mortality rate after a mean 27 years of follow-up in patients with type 1 diabetes (17). In addition, a follow-up study of the U.K. Prospective Diabetes Study (UKPDS), called UKPDS80, has also shown that benefits of an intensive therapy in patients with type 2 diabetes are sustained after the cessation of the trial (18). In this study, despite an early loss of glycemic differences between the original intensive therapy group and the conventional one, a continued reduction in microvascular risk and emergent risk reductions for myocardial infarction and death from any cause were observed during 10 years of post-trial follow-up (18). These findings demonstrate that so-called “metabolic memory” may cause chronic abnormalities in diabetic vessels that are not easily reversed, even by subsequent, relatively good blood glucose control, thus suggesting a long-term beneficial influence of early metabolic control (that is, the legacy effect) on the risk of diabetic vascular complications and death in both type 1 and type 2 diabetic patients.
AGEs AND RECEPTOR TO AGEs (RAGE)
AGEs are formed by the Maillard process, a nonenzymatic reaction between reducing sugars and the amino groups of proteins, lipids and nucleic acids that contribute to the aging of macromolecules (2,10,19). Under hyperglycemic and/or oxidative stress conditions, this process begins with the conversion of reversible Schiff base adducts to more stable, covalently bound Amadori rearrangement products (2,10,19). Over the course of days to weeks, these Amadori products undergo further rearrangement reactions to form the irreversibly cross-linked, fluorescent macroprotein derivatives, termed AGEs. About 10% of Amadori products could move to the irreversible process (20). AGEs are slowly degraded and remain for a long time in diabetic vessels, even after glycemic control has been improved (21,22).
Several types of AGE binding proteins have been reported (23). Among them, the receptor to AGEs (RAGE) is a cell surface receptor that belongs to the immunoglobulin superfamily and is a signal-transducing receptor for AGEs (23–27). There is a growing body of evidence that engagement of RAGE with AGEs elicits oxidative stress generation and results in evoking inflammatory and thrombogenic reactions in a variety of cells, thereby being involved in vascular complications in diabetes. Furthermore, AGEs are known to upregulate RAGE expression and induce sustained activation of nuclear factor-κB (NF-κB) (23–27). Therefore, it is conceivable that the AGE–RAGE–induced oxidative stress generation further potentiates the formation and accumulation of AGEs and subsequent RAGE overexpression. These positive feedback loops between AGEs and RAGE-downstream pathways could make a vicious cycle, thus providing a mechanistic basis for understanding why the phenomenon of metabolic memory exists in vascular complications in diabetes. Therefore, the biochemical nature and mode of action of AGEs are most compatible with the concept of metabolic memory (28,29).
PATHOPHYSIOLOGICAL ROLE OF AGEs IN VASCULAR COMPLICATIONS IN DIABETES
CVD
Vascular stiffness and inflammation
Cross-linking of proteins by AGE modification not only leads to an increase in vascular and myocardial stiffness, but also deteriorates structural integrity and physiological function of multiple organ systems, thus being involved in isolated systolic hypertension and diastolic heart failure (30).
There is a growing body of evidence, ranging from in vitro experiments to pathologic analysis and epidemiologic studies suggesting that atherosclerosis is intrinsically an inflammatory disease (31,32). Activation of the AGE–RAGE axis results in generation of intracellular oxidative stress generation and subsequent activation of NF-κB in vascular wall cells, which could promote a variety of atherosclerosis/inflammation-related gene expression, thereby contributing to the development and progression of CVD in diabetes (2,23–27).
Nitric oxide (NO) is the most potent endogenous vasodilator and, by the role of its antiinflammatory, antiproliferation and antithrombotic effects, it is widely recognized as an endogenous antiatherogenic factor (33–38). We, along with others, have shown that AGEs not only inhibit endothelial NO synthase expression in endothelial cells, but they also stimulate generation of peroxynitrite, a reactive intermediate and toxic product of NO with superoxide anion (33–35). Furthermore, the AGE–RAGE interaction enhances the production of asymmetric dimethylarginine (ADMA), an endogenous inhibitor of NO synthase in endothelial cells, mesangial cells and renal proximal tubular cells (35–38). Because ADMA is now considered one of the strongest biomarkers of CVD and chronic kidney disease progression (35), decreased production and/or impaired bioavailability of NO by the AGE–RAGE axis could also be involved in cardiorenal syndrome in diabetes.
Foam cell formation within the atherosclerosis
AGE modification impairs plasma clearance of low-density lipoprotein and transforms the lipoprotein into a more atherogenic and redox-sensitive mitogen-activated kinase stimulant in diabetic patients (39,40). Furthermore, we demonstrated that AGEs reduce adenosine triphosphate–binding membrane cassette transporter A1 (ABCA1) and ABCG1 levels in THP-1 cells and inhibit cholesterol efflux from THP-1 macrophages to apolipoprotein (apo) AI and HDL cholesterol, respectively (41). These findings suggest the involvement of the AGE–RAGE axis in impaired reverse cholesterol transport in diabetes and accelerated foam cell formation within the atherosclerotic lesions (41,42).
Thrombogenesis
AGEs not only cause platelet activation and aggregation, but also stimulate procoagulant activity by increasing expression of tissue factor, the main initiator of the coagulation cascade, which is responsible for thrombus formation (43). Furthermore, we recently found that AGEs could potentiate thrombin or factor Xa–evoked endothelial and renal cell damages via upregulation of protease-activated receptor-1 and -2 (44–46). These observations suggest that blockade of the crosstalk between AGE–RAGE axis and coagulation system by factor Xa inhibitors might be a novel therapeutic target for thromboembolic disorders in diabetes. In addition, AGEs inhibit prostacyclin production and induce plasminogen activator inhibitor-1 generation in endothelial cells through an interaction with RAGE (47). Therefore, AGEs may have the ability to cause platelet aggregation and fibrin stabilization, resulting in a predisposition to thrombogenesis, thereby contributing to the promotion of vascular injury in diabetes.
Pathological angiogenesis within the atherosclerosis
Plaque neovascularization is comprised of a network of capillaries that arise from adventitial vasa vasorum and extend into the intimal layer of atherosclerotic lesions (48–50). They are often found in areas rich in inflammatory cells, such as macrophages and T cells, and have been considered to function as conduits for the entry of leukocytes and nutrients into the artery wall. Moreover, plaque vessels are associated with plaque rupture, intraplaque hemorrhage and unstable angina (48,50). Therefore, ischemia and hypoxia due to microthrombus formation within the atherosclerotic plaques may further stimulate vascular endothelial growth factor (VEGF) expression and trigger pathological angiogenesis in these vulnerable lesions (51,52). Therefore, the AGE-induced pathological angiogenesis may contribute to plaque growth and instability within the atherosclerotic plaques in diabetes.
Impaired endothelial cell repair
Diabetes is associated with endothelial dysfunction and decreased endothelial progenitor cell (EPC) function and mobilization, which could contribute to accelerated atherosclerosis and increased risk for CVD in diabetic patients (53). AGEs enhance apoptosis and suppress migration and tube formation of late EPCs through the interaction with RAGE via downregulation of Akt and cycloxygenase-2 (54). AGEs have also been shown to cause a reduction of length growth and EPC incorporation into the sprouts in association with RAGE overexpression and p38 mitogen-activated protein kinase activation (55). Moreover, AGE modification of vascular substrates impair vascular repair by inhibiting EPC adhesion, spreading and migration via glycation of the Arg-Gly-Asp motif of fibronectin (56).
Vascular calcification
AGEs have the ability to induce the osteoblatic differentiation of pericytes, thus contributing to the development of vascular calcification in atherosclerosis (57). Pericytes have the plasticity to differentiate into other mesenchymal cell types under various circumstances and may function as resting stem cells to be converted into smooth muscle cells, macrophage-like phagocytes or osteoblasts (48). Furthermore, activation of RAGE not only inhibits myocardin-dependent smooth muscle cell (SMC) gene expression, but also induces osteogenic differentiation of vascular SMCs through Notch/Msx2 induction, thus being involved in vascular calcification as well (58).
SMC proliferation
AGEs elicit reactive oxygen species generation and subsequently induce SMC proliferation through the interaction with RAGE via NADPH oxidase activation (59,60). AGE–RAGE–induced extracellular signal-related kinase activation is reported to increase Na+/H+ exchanger-1 activity, which leads to a decrease in intracellular H+ and subsequently promotes a cell-cycle progression and SMC proliferation (61).
Diabetic Retinopathy
Pericytes are elongated cells of the mesodermal origin, wrapping around and along endothelial cells of small vessels (48). Because pericytes have played an important role in the maintenance of microvascular homeostasis, AGE-caused pericyte apoptosis could predispose the vessels to angiogenesis, thrombogenesis and endothelial cell injury, thus leading to full-blown clinical expression of diabetic retinopathy (2). Moreover, AGEs directly stimulate growth and tube formation of microvascular endothelial cells, the key steps of angiogenesis, through the interaction with RAGE by inducing VEGF expression (49).
AGEs have been shown to increase leukocyte adhesion to cultured retinal microvascular endothelial cells by inducing intracellular cell adhesion molecule-1 expression as well (62). This phenomenon is also apparent in nondiabetic mice infused with preformed AGEs, which results in significant leukostasis and blood-retinal barrier dysfunction in these mice (62). Because retinal VEGF induces intra-cellular cell adhesion molecule-1 expression, which could lead to leukostasis and breakdown of the blood-retinal barrier in vivo (63–65), the AGE-elicited proinflammatory reactions could be modulated by the blockage of VEGF.
Diabetic Nephropathy
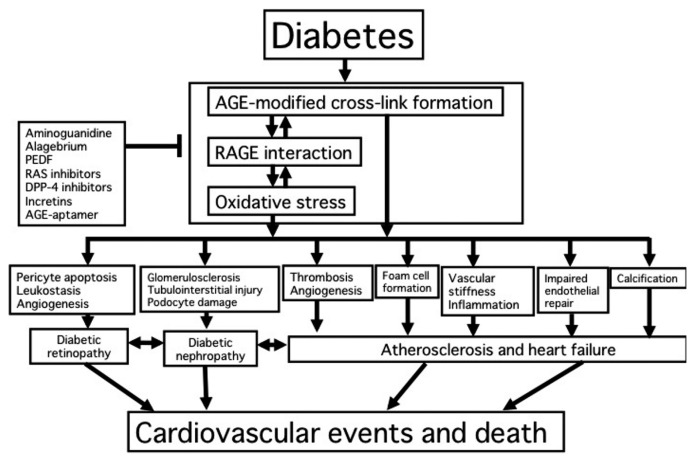
Accumulation of AGEs in the kidney may contribute to the progressive alteration in renal architecture and loss of renal function in patients and rodents via various mechanisms, including their cross-linking properties of matrix proteins and activation of the downstream signaling (2,66,67). AGE formation on extracellular matrix proteins alters both matrix–matrix and cell–matrix interactions, and is involved in diabetic glomerulosclerosis. AGEs induce apo ptotic cell death and VEGF expression in human cultured mesangial cells, as is the case in pericytes, a counterpart of mesangial cells in retinas (68). Because mesangial cells occupy a central anatomical position in the glomerulus and play a crucial role in maintaining structure and function of glomerular capillary tufts, the AGE-induced mesangial apoptosis and dysfunction may contribute in part to glomerular hyperfiltration, an early renal dysfunction in diabetes. Podocyte loss is a common and early feature in human and experimental diabetic nephropathy (69). AGEs have also been shown to induce podocyte damage and detachment (70). Furthermore, AGEs induce transforming growth factor-β expression in renal constituents such as podocytes, mesangial cells and proximal tubular cells, thereby contributing to glomerulosclerosis and tubulointerstitial fibrosis in diabetic nephropathy as well (71,72). We posit a scheme to summarize the pathophysiological role of AGEs in vascular complications in diabetes (73) (Figure 1).
Figure 1.
Pathophysiological role of AGEs in diabetic vascular complications.
RAGE TRANSGENIC AND KNOCKOUT MICE
Diabetic RAGE−/−/apoE−/− mice had significantly reduced atherosclerotic plaque area, which is associated with attenuation of leukocyte recruitment, decreased expression of proinflammatory mediators, reduced oxidative stress and AGE accumulation (74).
RAGE-overexpressing diabetic mice have exhibited progressive glomerulosclerosis with renal dysfunction, compared with diabetic littermates lacking the RAGE transgene (75). Furthermore, Wendt et al. (76) reported that diabetic homozygous RAGE null mice failed to develop mesangial matrix expansion or thickening of the glomerular basement membrane. They also claimed in their report that activation of RAGE in podocytes could contribute to expression of VEGF and enhanced attraction/activation of inflammatory cells in the diabetic glomeruli, causing albuminuria and glomerulosclerosis in diabetes (76). In addition, db/db or streptozotocin-induced diabetic mice have developed renal changes seen in human diabetic nephropathy such as glomerular hypertrophy, glomerular basement membrane thickening, mesangial matrix expansion, connective tissue growth factor overexpression and NF-κB activation, all of which are blocked by the administration of neutralizing antibody raised against RAGE (77,78).
Blood-retinal barrier breakdown and retinal leukostasis were significantly augmented in RAGE-transgenic diabetic mice, which were blocked by the systemic administration of a soluble form of RAGE (79). Inflammatory reactions and the AGE–RAGE–NF-κB pathway were enhanced in peripheral nerves of diabetic mice, all of which were prevented by RAGE gene deficiency or the addition of a soluble form of RAGE, which was associated with dramatic improvement in the loss of pain perception (80).
THERAPEUTIC INTERVENTIONS OF THE AGE–RAGE AXIS
Inhibitors of AGE Formation and Breaker
Various types of inhibitors of AGE formation or AGE breaker alagebrium have been shown to prevent vascular damage in diabetic animals (81,82). Indeed, aminoguanidine was reported to increase vascular elasticity, improve left ventricular arterial coupling and decrease vascular permeability in diabetic rats (82,83). Aminoguanidine prevented the decreased myocardial compliance and cardiac hypertrophy in diabetic animals (83). Furthermore, aminoguanidine treatment decreased accumulation levels of AGEs and reduced atherosclerotic plaque area in the thoracic and abdominal aortas in streptozotocin-induced diabetic apoE-deficient mice (84). Alagebrium treatment significantly attenuated plaque area or complexity within the thoracic and abdominal aortas and inhibited accumulation of AGE-modified collagens in the aortas with reduced expression of RAGE and profibrotic cytokines, TGF-β and connective tissue growth factor in streptozotocin-induced diabetic apoE- deficient mice as well (84). In addition, alagebrium reduced transdifferentiation of proximal tubules in the diabetic kidneys in association with reduced tubular AGE and TGF-β levels. Alagebrium treatment also decreased AGE and collagen accumulation in the diabetic kidneys, inhibited glomerulosclerosis and tubulointerstitial injury and retarded albumin excretion rate in streptozotocin-induced diabetic rats. These rats were associated with reduced renal expression of RAGE, TGF-β and connective tissue growth factor (85).
Pigment Epithelium-Derived Factor
Pigment epithelium-derived factor (PEDF), a glycoprotein that belongs to the superfamily of serine protease inhibitors with potent neuronal differentiating activity, inhibits vascular hyperpermeability, inflammatory, thrombotic and fibrotic reactions in diabetic nephropathy and retinopathy partly by suppressing the AGE–RAGE axis, which could potentially be exploited as a therapeutic option for the treatment of vascular complications in diabetes (86–89).
Renin-Angiotensin System Inhibitors
The interaction of the renin- angiotensin system (RAS) and AGE–RAGE axis has been proposed (90). We have found that angiotensin II (Ang II) potentiates the deleterious effects of AGEs on pericytes by inducing RAGE protein expression (91). In vivo, AGE injection stimulated RAGE expression in the eye of spontaneously hypertensive rats, which was blocked by telmisartan, an Ang II type 1 (AT1) receptor blocker. In vitro, Ang II-AT1 receptor–mediated oxidative stress generation elicited RAGE gene upregulation in retinal pericytes through NF-κB activation. Furthermore, Ang II augmented AGE-induced pericyte apoptosis, the earliest hallmark of diabetic retinopathy (2). In addition, the AGE–RAGE axis stimulates Ang II production or AT1 receptor overexpression in renal constituents, further deteriorating diabetic nephropathy (92–94).
Dipeptidyl Peptidase-4 Inhibitors and Incretins
There is a pathological crosstalk between the AGE–RAGE system and dipeptidyl peptidase-4 (DPP-4)-incretin axis in the pathogenesis of vascular complications in diabetes (95,96). Glucagon-like peptide-1 directly acts on endothelial cells, mesangila cells and proximal tubular cells via the glucagon-like peptide-1 receptor, and glucagon-like peptide-1 could work as an antiinflammatory and antioxidative agent against AGEs by reducing RAGE expression via activation of cyclic AMP pathways (95,96). Moreover, we have recently found that AGE–RAGE–induced oxidative stress generation stimulates the release of DPP-4 from endothelial cells, which could act on endothelial cells in an autocrine manner via the interaction with mannose 6-phosphate insulin-like growth factor II receptor, further potentiating the deleterious effects of AGEs (97). DPP-4 deficiency or an inhibitor of DPP-4 protects against experimental diabetic nephropathy in a glucose-lowering–independent manner, where benefficial effects were partly mediated by suppression of the AGE–RAGE axis (98,99).
AGE-Aptamer
Aptamers are short, single-stranded DNA or RNA molecules that can bind with high affinity and specificity to a wide range of target proteins (100,101). We have recently found that a high- affinity DNA aptamer directed against AGEs (AGE-aptamer) inhibits glomerular hypertrophy and extracellular matrix protein accumulation, decreases urinary excretion levels of albumin and prevents renal dysfunction in type 2 diabetic animals (100). In this study, AGE-aptamer directly bound to AGEs and resultantly blocked the binding of AGEs to RAGE, and continuous infusion of AGE- aptamer dramatically decreased AGE levels in the glomeruli of diabetic mice (100). Therefore, it is conceivable that AGE-aptamer might decrease the glomerular accumulation of AGEs via the blockade of RAGE-induced, oxidative stress–mediated AGE formation in the kidney. In addition, turnover rate of aptamer-bound AGEs by THP-1 macro -phages was increased. Therefore, AGE-aptamer could enhance the elimination of AGEs from the body through increased turnover by macrophages.
MEASURING SERUM LEVELS OF AGES AND ITS CLINICAL UTILITY
The facts that AGEs could reflect cumulative diabetic exposure and play a role in the pathogenesis of diabetic vascular complications led us to speculate that circulating levels of AGEs could be a biomarker of vascular injury and organ damage in patients with diabetes. To address the issue, we began to develop an enzyme-linked immunosorbent assay (ELISA) system for measuring serum levels of toxic AGEs in humans.
In the article in Molecular Medicine in 2001, we produced five specific antibodies for noncarboxymethyllysine AGEs that recognized the immunoreactive types of AGEs (glucose-, glyceraldehyde-, glycolaldehyde-, methylglyoxal- and glyoxal-derived AGEs) (10). We found that (a) five distinct classes of AGE structures circulate in the blood of individuals with diabetic nephropathy on hemodialysis (DM-HD), (b) neurotoxic effects of serum fraction from DM-HD containing various AGEs structures are completely neutralized by the addition of antibodies raised against glyceraldehyde-derived AGEs, and (c) this type of AGE mimics the deleterious effects of AGE-rich serum purified from DM-HD on endothelial cells (85,102). Furthermore, because of the stronger binding affinity to RAGE (103), glyceraldehyde-derived AGEs are considered to be more toxic than glucose-derived AGEs. Hence, we focused on glyceraldehyde-derived AGEs, developed a specific ELISA for this type of AGE and examined the clinical utility of measuring glyceraldehyde-derived AGEs for evaluating disease activity in patients with various diabetes- and aging-associated disorders.
So far, we have found that glyceraldehyde-derived AGE levels are (a) correlated with a soluble form of RAGE that could reflect tissue RAGE expression in both nondiabetic and diabetic subjects (104–107), thus suggesting a marker of the activation of AGE–RAGE axis; (b) associated with low-density lipoprotein cholesterol levels and thrombogenic markers such as plasminogen activator inhibitor-1 and fibrinogen in a general population (108–110); (c) elevated under oxidative stress, chronic kidney disease and/or diabetic conditions and correlated with inflammatory biomarkers such as monocyte chemoattractant protein-1, the soluble form of vascular cell adhesion molecule-1 and ADMA (106,107,111–113); (d) increased in nonalcoholic steatohepatitis (NASH) patients and associated with insulin resistance in both NASH subjects and an non-NASH general population (114–116); (e) correlated with serum PEDF and DPP-4 levels, markers of insulin resistance (117,118); (f) associated with visceral and subcutaneous adipose tissue inflammation and decreased adiponectin levels (114,119); (g) correlated with vascular inflammation and endothelial dysfunction in high-risk patients (120,121); (h) inversely associated with number and migratory activity of EPCs (122), thus suggesting the involvement of this type of AGEs in impaired endothelial cell repair; and (i) significantly associated with plaque progression in patients with acute coronary syndrome (123). Moreover, atrovastatin, pioglitazone and α-glucosidase inhibitor have been shown to significantly decrease serum levels of glyceraldehyde-derived AGEs, which are associated with reduced biomarker levels for organ damage in diabetic, chronic kidney disease or NASH subjects (120,124–128).
CONCLUSIONS
Glyceraldehyde, which could be derived from glucose metabolism, is not a major sugar in vivo and its incubation with proteins will generate a large number of AGEs; in addition, there is some criticism that measurement of AGEs using liquid chromatography–tandem mass spectrometry technique may produce different results to that using ELISA (129). However, our series of studies have suggested that serum levels of glyceraldehyde-derived AGEs might be a novel biomarker for insulin resistance and vascular injury and may predict future cardiovascular events in diabetes. Measuring this type of AGEs by specific ELISA could identify high-risk patients and may provide us variable information for treatment decision-making in the future.
In addition, we have recently found that AGE-aptamer raised against glyceraldehyde-derived AGEs, but not control-aptamer, binds to glyceraldehyde-derived pyridinium (GLAP) and the 3-hydroxy-5-hydroxymethyl-pyridinium adduct and subsequently blocks the interaction of GLAP with RAGE. Moreover, a GLAP-evoked increase in oxidative stress generation and upregulation in RAGE as well as inflammatory reactions were significantly inhibited by treatment with AGE-aptamer but not control-aptamer (130). These findings suggest that GLAP is a target compound for AGE-aptamer and might be a main glyceraldehyde-related AGE structure that interacted with RAGE and elicited oxidative, inflammatory and thrombogenic reactions in endothelial cells. GLAP was only formed in glyceraldehyde-modified bovine serum albumin, not in another sugar-modified one, thus supporting our speculation (131). So, development of a simple, specific, reliable assay system for GLAP would be desired, and it should be an important issue in the feature to examine whether serum levels of GLAP may be a novel biomarker for vascular damage and CVD in diabetes.
ACKNOWLEDGMENTS
This study was supported in part by Grants-in-Aid for Scientific Research (B) (grant number 25293127) from the Ministry of Education, Culture, Sports, Science and Technology, Japan (to S Yamagishi).
Footnotes
Online address: http://www.molmed.org
DISCLOSURE
The authors declare that they have no competing interests as defined by Molecular Medicine, or other interests that might be perceived to influence the results and discussion reported in this paper.
Cite this article as: Yamagishi S-i, Nakamura N, Suematsu M, Kaseda K, and Matsui T. (2015) Advanced glycation end products: a molecular target for vascular complications in diabetes. Mol. Med. 21 Suppl 1:S32–40.
REFERENCES
- 1.International Diabetes Federation. IDF Diabetes Atlas. 6th ed. Brussels, Belgium: International Diabetes Federation; 2013. [Google Scholar]
- 2.Yamagishi S, Imaizumi T. Diabetic vascular complications: pathophysiology, biochemical basis and potential therapeutic strategy. Curr Pharm Des. 2005;11:2279–99. doi: 10.2174/1381612054367300. [DOI] [PubMed] [Google Scholar]
- 3.Emerging Risk Factors Collaboration, et al. Diabetes mellitus, fasting glucose, and risk of cause-specific death. N Engl J Med. 2011;364:829–41. doi: 10.1056/NEJMoa1008862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yamagishi S, Matsui T, Fukami K. Role of receptor for advanced glycation end products (RAGE) and its ligands in cancer risk. Rejuvenation Res. 2015;18:48–56. doi: 10.1089/rej.2014.1625. [DOI] [PubMed] [Google Scholar]
- 5.Takeuchi M, Yamagishi S. Possible involvement of advanced glycation end-products (AGEs) in the pathogenesis of Alzheimer’s disease. Curr Pharm Des. 2008;14:973–8. doi: 10.2174/138161208784139693. [DOI] [PubMed] [Google Scholar]
- 6.Yamagishi S. Role of advanced glycation end products (AGEs) in osteoporosis in diabetes. Curr Drug Targets. 2011;12:2096–102. doi: 10.2174/138945011798829456. [DOI] [PubMed] [Google Scholar]
- 7.Loukine L, Waters C, Choi BC, Ellison J. Impact of diabetes mellitus on life expectancy and health-adjusted life expectancy in Canada. Popul Health Metr. 2012;10:7. doi: 10.1186/1478-7954-10-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Turin TC, et al. NIPPON DATA80 Research Group: Diabetes and life expectancy among Japanese-NIPPON DATA80. Diabetes Res Clin Pract. 2102;96:e18–22. doi: 10.1016/j.diabres.2012.01.003. [DOI] [PubMed] [Google Scholar]
- 9.Rhodes ET, et al. Estimated morbidity and mortality in adolescents and young adults diagnosed with type 2 diabetes mellitus. Diabet Med. 2012;29:453–63. doi: 10.1111/j.1464-5491.2011.03542.x. [DOI] [PubMed] [Google Scholar]
- 10.Takeuchi M, et al. Immunological detection of a novel advanced glycation end-product. Mol Med. 2001;7:783–91. [PMC free article] [PubMed] [Google Scholar]
- 11.Diabetes Control and Complications Trial (DCCT)/Epidemiology of Diabetes Interventions and Complications (EDIC) Research Group. Effect of intensive diabetes therapy on the progression of diabetic retinopathy in patients with type 1 diabetes: 18 years of follow-up in the DCCT/EDIC. Diabetes. 2015;64:631–42. doi: 10.2337/db14-0930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.DCCT/EDIC Research Group. Effect of intensive diabetes treatment on albuminuria in type 1 diabetes: long-term follow-up of the Diabetes Control and Complications Trial and Epidemiology of Diabetes Interventions and Complications study. Lancet Diabetes Endocrinol. 2014;2:793–800. doi: 10.1016/S2213-8587(14)70155-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Martin CL, Albers JW, Pop-Busui R. DCCT/EDIC Research Group: Neuropathy and related findings in the Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications study. Diabetes Care. 2014;37:31–8. doi: 10.2337/dc13-2114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nathan DM, et al. Epidemiology of Diabetes Interventions and Complications Research Group: Intensive diabetes therapy and carotid intima-media thickness in type 1 diabetes mellitus. N Engl J Med. 2003;348:2294–303. doi: 10.1056/NEJMoa022314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nathan DM, et al. Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications (DCCT/EDIC) Study Research Group: Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. N Engl J Med. 2005;353:2643–53. doi: 10.1056/NEJMoa052187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nathan DM DCCT/EDIC Research Group. The Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications study at 30 years: overview. Diabetes Care. 2014;37:9–16. doi: 10.2337/dc13-2112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Writing Group for the DCCT/EDIC Research Group, et al. Association between 7 years of intensive treatment of type 1 diabetes and long-term mortality. JAMA. 2015;313:45–53. doi: 10.1001/jama.2014.16107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med. 2008;359:1577–89. doi: 10.1056/NEJMoa0806470. [DOI] [PubMed] [Google Scholar]
- 19.Monnier VM, Kohn RR, Cerami A. Accelerated age-related browning of human collagen in diabetes mellitus. Proc Natl Acad Sci U S A. 1984;81:583–7. doi: 10.1073/pnas.81.2.583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Makita Z, et al. Hemoglobin-AGE: a circulating marker of advanced glycosylation. Science. 1992;258:651–3. doi: 10.1126/science.1411574. [DOI] [PubMed] [Google Scholar]
- 21.Wolffenbuttel BH, Giordano D, Founds HW, Bucala R. Long-term assessment of glucose control by haemoglobin-AGE measurement. Lancet. 1996;347:513–5. doi: 10.1016/s0140-6736(96)91141-1. [DOI] [PubMed] [Google Scholar]
- 22.Hricik DE, Wu YC, Schulak A, Friedlander MA. Disparate changes in plasma and tissue pentosidine levels after kidney and kidney-pancreas transplantation. Clin Transplant. 1996;10:568–73. [PubMed] [Google Scholar]
- 23.Sourris KC, Forbes JM. Interactions between advanced glycation end-products (AGE) and their receptors in the development and progression of diabetic nephropathy: are these receptors valid therapeutic targets. Curr Drug Targets. 2009;10:42–50. doi: 10.2174/138945009787122905. [DOI] [PubMed] [Google Scholar]
- 24.Yamagishi S, Nakamura K, Matsui T, Noda Y, Imaizumi T. Receptor for advanced glycation end products (RAGE): a novel therapeutic target for diabetic vascular complication. Curr Pharm Des. 2008;14:487–95. doi: 10.2174/138161208783597416. [DOI] [PubMed] [Google Scholar]
- 25.Yamagishi S, Matsui T. Soluble form of a receptor for advanced glycation end products (sRAGE) as a biomarker. Front Biosci. 2010;2:1184–95. doi: 10.2741/e178. [DOI] [PubMed] [Google Scholar]
- 26.Daffu G, et al. Radical roles for RAGE in the pathogenesis of oxidative stress in cardiovascular diseases and beyond. Int J Mol Sci. 2013;14:19891–910. doi: 10.3390/ijms141019891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fukami K, Yamagishi S, Okuda S. Role of AGEs-RAGE system in cardiovascular disease. Curr Pharm Des. 2014;20:2395–402. doi: 10.2174/13816128113199990475. [DOI] [PubMed] [Google Scholar]
- 28.Ceriello A, Ihnat MA, Thorpe JE. Clinical review 2: The “metabolic memory”: is more than just tight glucose control necessary to prevent diabetic complications? J Clin Endocrinol Metab. 2009;94:410–5. doi: 10.1210/jc.2008-1824. [DOI] [PubMed] [Google Scholar]
- 29.Chilelli NC, Burlina S, Lapolla A. AGEs, rather than hyperglycemia, are responsible for microvascular complications in diabetes: a “glycoxidation-centric” point of view. Nutr Metab Cardiovasc Dis. 2013;23:913–9. doi: 10.1016/j.numecd.2013.04.004. [DOI] [PubMed] [Google Scholar]
- 30.Yamagishi S. Potential clinical utility of advanced glycation end product cross-link breakers in age- and diabetes-associated disorders. Rejuvenation Res. 2012;15:564–72. doi: 10.1089/rej.2012.1335. [DOI] [PubMed] [Google Scholar]
- 31.Rizvi AA. Cytokine biomarkers, endothelial inflammation, and atherosclerosis in the metabolic syndrome: emerging concepts. Am J Med Sci. 2009;55:659–65. doi: 10.1097/MAJ.0b013e3181a4158c. [DOI] [PubMed] [Google Scholar]
- 32.Lamon BD, Hajjar DP. Inflammation at the molecular interface of atherogenesis: an anthropological journey. Am J Pathol. 2008;173:1253–64. doi: 10.2353/ajpath.2008.080442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yamagishi S, et al. Pigment epithelium-derived factor (PEDF) prevents advanced glycation end products (AGEs)-elicited endothelial nitric oxide synthase (eNOS) reduction through its anti-oxidative properties. Protein Pept Lett. 2007;14:832–5. doi: 10.2174/092986607781483705. [DOI] [PubMed] [Google Scholar]
- 34.Soro-Paavonen A, et al. Advanced glycation end-products induce vascular dysfunction via resistance to nitric oxide and suppression of endothelial nitric oxide synthase. J Hypertens. 2010;28:780–8. doi: 10.1097/HJH.0b013e328335043e. [DOI] [PubMed] [Google Scholar]
- 35.Ueda S, Yamagishi S, Yokoro M, Okuda S. Role of asymmetric dimethylarginine in cardiorenal syndrome. Curr Pharm Des. 2014;20:2448–55. doi: 10.2174/13816128113199990480. [DOI] [PubMed] [Google Scholar]
- 36.Ojima A, et al. Glucagon-like peptide-1 receptor agonist inhibits asymmetric dimethylarginine generation in the kidney of streptozotocin-induced diabetic rats by blocking advanced glycation end product-induced protein arginine methyltranferase-1 expression. Am J Pathol. 2013;182:132–41. doi: 10.1016/j.ajpath.2012.09.016. [DOI] [PubMed] [Google Scholar]
- 37.Ando R, et al. Involvement of advanced glycation end product-induced asymmetric dimethylarginine generation in endothelial dysfunction. Diab Vasc Dis Res. 2013;10:436–41. doi: 10.1177/1479164113486662. [DOI] [PubMed] [Google Scholar]
- 38.Ishibashi Y, et al. Irbesartan inhibits advanced glycation end product-induced increase in asymmetric dimethylarginine level in mesangial cells through its anti-oxidative properties. Int J Cardiol. 2014;176:1120–2. doi: 10.1016/j.ijcard.2014.07.299. [DOI] [PubMed] [Google Scholar]
- 39.Bucala R, et al. Modification of low density lipoprotein by advanced glycation end products contributes to the dyslipidemia of diabetes and renal insufficiency. Proc Natl Acad Sci U S A. 1994;191:9441–5. doi: 10.1073/pnas.91.20.9441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cai W, et al. High levels of dietary advanced glycation end products transform low-density lipoprotein into a potent redox-sensitive mitogen-activated protein kinase stimulant in diabetic patients. Circulation. 2004;110:285–91. doi: 10.1161/01.CIR.0000135587.92455.0D. [DOI] [PubMed] [Google Scholar]
- 41.Ishibashi Y, Matsui T, Takeuchi M, Yamagishi S. Rosuvastatin blocks advanced glycation end products-elicited reduction of macrophage cholesterol efflux by suppressing NADPH oxidase activity via inhibition of geranylgeranylation of Rac-1. Horm Metab Res. 2011;43:619–24. doi: 10.1055/s-0031-1283148. [DOI] [PubMed] [Google Scholar]
- 42.Khera AV, et al. Cholesterol efflux capacity, high-density lipoprotein function, and atherosclerosis. N Engl J Med. 2011;364:127–35. doi: 10.1056/NEJMoa1001689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Takenaka K, Yamagishi S, Matsui T, Nakamura K, Imaizumi T. Role of advanced glycation end products (AGEs) in thrombogenic abnormalities in diabetes. Curr Neurovasc Res. 2006;3:73–7. doi: 10.2174/156720206775541804. [DOI] [PubMed] [Google Scholar]
- 44.Ishibashi Y, Matsui T, Ueda S, Fukami K, Yamagishi S. Advanced glycation end products potentiate citrated plasma-evoked oxidative and inflammatory reactions in endothelial cells by up-regulating protease-activated receptor-1 expression. Cardiovasc Diabetol. 2014;13:60. doi: 10.1186/1475-2840-13-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ishibashi Y, Matsui T, Yamagishi S. Apixaban exerts anti-inflammatory effects in mesangial cells by blocking thrombin/protease-activated receptor-1 system. Thromb Res. 2014;134:1365–7. doi: 10.1016/j.thromres.2014.09.028. [DOI] [PubMed] [Google Scholar]
- 46.Ishibashi Y, et al. Rivaroxaban inhibits oxidative and inflammatory reactions in advanced glycation end product-exposed tubular cells by blocking thrombin/protease-activated receptor-2 system. Thromb Res. 2015;135:770–3. doi: 10.1016/j.thromres.2015.01.023. [DOI] [PubMed] [Google Scholar]
- 47.Yamagishi S, Fujimori H, Yonekura H, Yamamoto Y, Yamamoto H. Advanced glycation end-products inhibit prostacyclin production and induce plasminogen activator inhibitor-1 in human microvascular endothelial cells. Diabetologia. 1998;41:1435–41. doi: 10.1007/s001250051089. [DOI] [PubMed] [Google Scholar]
- 48.Yamagishi S, Imaizumi T. Pericyte biology and diseases. Int J Tissue React. 2005;27:125–35. [PubMed] [Google Scholar]
- 49.Yamagishi Si, et al. Advanced glycation end products-driven angiogenesis in vitro: induction of the growth and tube formation of human microvascular endothelial cells through autocrine vascular endothelial growth factor. J Biol Chem. 1997;272:8723–30. doi: 10.1074/jbc.272.13.8723. [DOI] [PubMed] [Google Scholar]
- 50.Moulton KS. Plaque angiogenesis and atherosclerosis. Curr Atheroscler Rep. 2001;3:225–33. doi: 10.1007/s11883-001-0065-0. [DOI] [PubMed] [Google Scholar]
- 51.Nomura M, et al. Possible participation of autocrine and paracrine vascular endothelial growth factors in hypoxia-induced proliferation of endothelial cells and pericytes. J Biol Chem. 1995;270:28316–24. doi: 10.1074/jbc.270.47.28316. [DOI] [PubMed] [Google Scholar]
- 52.Yamagishi S, et al. Vascular endothelial growth factor acts as a pericyte mitogen under hypoxic conditions. Lab Invest. 1999;79:501–9. [PubMed] [Google Scholar]
- 53.Hoenig MR, Bianchi C, Rosenzweig A, Sellke FW. Decreased vascular repair and neo-vascularization with ageing: mechanisms and clinical relevance with an emphasis on hypoxia-inducible factor-1. Curr Mol Med. 2008;8:754–67. doi: 10.2174/156652408786733685. [DOI] [PubMed] [Google Scholar]
- 54.Chen Q, Dong L, Wang L, Kang L, Xu B. Advanced glycation end products impair function of late endothelial progenitor cells through effects on protein kinase Akt and cyclooxyge-nase-2. Biochem Biophys Res Commun. 2009;381:192–7. doi: 10.1016/j.bbrc.2009.02.040. [DOI] [PubMed] [Google Scholar]
- 55.Scheubel RJ, et al. Depression of progenitor cell function by advanced glycation endproducts (AGEs): potential relevance for impaired angiogenesis in advanced age and diabetes. Exp Gerontol. 2006;41:540–8. doi: 10.1016/j.exger.2006.01.002. [DOI] [PubMed] [Google Scholar]
- 56.Bhatwadekar AD, et al. Advanced glycation of fibronectin impairs vascular repair by endothelial progenitor cells: implications for vasodegeneration in diabetic retinopathy. Invest Ophthalmol Vis Sci. 2008;49:1232–41. doi: 10.1167/iovs.07-1015. [DOI] [PubMed] [Google Scholar]
- 57.Yamagishi S, Fujimori H, Yonekura H, Tanaka N, Yamamoto H. Advanced glycation endproducts accelerate calcification in microvascular pericytes. Biochem Biophys Res Commun. 1999;258:353–7. doi: 10.1006/bbrc.1999.0625. [DOI] [PubMed] [Google Scholar]
- 58.Suga T, et al. Activation of receptor for advanced glycation end products induces osteogenic differentiation of vascular smooth muscle cells. J Atheroscler Thromb. 2011;18:670–83. doi: 10.5551/jat.7120. [DOI] [PubMed] [Google Scholar]
- 59.Yamagishi S, Matsui T. Smooth muscle cell pathophysiology and advanced glycation end products (AGEs) Curr Drug Targets. 2010;11:875–81. doi: 10.2174/138945010791320827. [DOI] [PubMed] [Google Scholar]
- 60.Yoon YW, et al. Pathobiological role of advanced glycation endproducts via mitogen-activated protein kinase dependent pathway in the diabetic vasculopathy. Exp Mol Med. 2008;40:398–406. doi: 10.3858/emm.2008.40.4.398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wu S, et al. Involvement of Na+/H+ exchanger 1 in advanced glycation end products-induced proliferation of vascular smooth muscle cell. Biochem Biophys Res Commun. 2008;375:384–9. doi: 10.1016/j.bbrc.2008.08.008. [DOI] [PubMed] [Google Scholar]
- 62.Moore TC, et al. The role of advanced glycation end products in retinal microvascular leukostasis. Invest Ophthalmol Vis Sci. 2003;44:4457–64. doi: 10.1167/iovs.02-1063. [DOI] [PubMed] [Google Scholar]
- 63.Lu M, et al. VEGF increases retinal vascular ICAM-1 expression in vivo. Invest Ophthalmol Vis Sci. 1999;40:1808–12. [PubMed] [Google Scholar]
- 64.Yamagishi S, Matsui T, Nakamura K, Takeuchi M, Imaizumi T. Pigment epithelium-derived factor (PEDF) prevents diabetes- or advanced glycation end products (AGE)-elicited retinal leukostasis. Microvasc Res. 2006;72:86–90. doi: 10.1016/j.mvr.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 65.Yamagishi S, Matsui T. Advanced glycation end products (AGEs), oxidative stress and diabetic retinopathy. Curr Pharm Biotechnol. 2011;12:362–8. doi: 10.2174/138920111794480534. [DOI] [PubMed] [Google Scholar]
- 66.Yamagishi S, Matsui T. Advanced glycation end products, oxidative stress and diabetic nephropathy. Oxid Med Cell Longev. 2010;3:101–8. doi: 10.4161/oxim.3.2.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Fukami K, Taguchi K, Yamagishi S, Okuda S. Receptor for advanced glycation endproducts and progressive kidney disease. Curr Opin Nephrol Hypertens 2. 2015;4:54–60. doi: 10.1097/MNH.0000000000000091. [DOI] [PubMed] [Google Scholar]
- 68.Yamagishi S, et al. Advanced glycation end product-induced apoptosis and overexpression of vascular endothelial growth factor and monocyte chemoattractant protein-1 in human-cultured mesangial cells. J Biol Chem. 2002;277:20309–15. doi: 10.1074/jbc.M202634200. [DOI] [PubMed] [Google Scholar]
- 69.Stieger N, Worthmann K, Schiffer M. The role of metabolic and haemodynamic factors in podocyte injury in diabetes. Diabetes Metab Res Rev. 2011;27:207–15. doi: 10.1002/dmrr.1164. [DOI] [PubMed] [Google Scholar]
- 70.Fukami K, et al. Telmisartan inhibits AGE-induced podocyte damage and detachment. Microvasc Res. 2013;88:79–83. doi: 10.1016/j.mvr.2013.04.006. [DOI] [PubMed] [Google Scholar]
- 71.Yamagishi S, et al. Advanced glycation end products inhibit de novo protein synthesis and induce TGF-beta overexpression in proximal tubular cells. Kidney Int. 2003;63:464–73. doi: 10.1046/j.1523-1755.2003.00752.x. [DOI] [PubMed] [Google Scholar]
- 72.Ojima A, Matsui T, Nishino Y, Nakamura N, Yamagishi S. Empagliflozin, an inhibitor of sodium-glucose cotransporter 2 exerts anti-inflammatory and antifibrotic effects on experimental diabetic nephropathy partly by suppressing AGEs-receptor axis. Horm Metab Res. 2015 2015 Jan 22; doi: 10.1055/s-0034-1395609. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 73.Nishikawa T, et al. Normalizing mitochondrial superoxide production blocks three pathways of hyperglycaemic damage. Nature. 2000;404:787–90. doi: 10.1038/35008121. [DOI] [PubMed] [Google Scholar]
- 74.Soro-Paavonen A, et al. Receptor for advanced glycation end products (RAGE) deficiency attenuates the development of atherosclerosis in diabetes. Diabetes. 2008;57:2461–9. doi: 10.2337/db07-1808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Yamamoto Y, et al. Development and prevention of advanced diabetic nephropathy in RAGE-overexpressing mice. J Clin Invest. 2001;108:261–8. doi: 10.1172/JCI11771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Wendt TM, et al. RAGE drives the development of glomerulosclerosis and implicates podocyte activation in the pathogenesis of diabetic nephropathy. Am J Pathol. 2003;162:1123–37. doi: 10.1016/S0002-9440(10)63909-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Flyvbjerg A, et al. Long-term renal effects of a neutralizing RAGE antibody in obese type 2 diabetic mice. Diabetes. 2004;53:166–72. doi: 10.2337/diabetes.53.1.166. [DOI] [PubMed] [Google Scholar]
- 78.Jensen LJ, et al. Renal effects of a neutralising RAGE-antibody in long-term streptozotocin-diabetic mice. J Endocrinol. 2006;188:493–501. doi: 10.1677/joe.1.06524. [DOI] [PubMed] [Google Scholar]
- 79.Kaji Y, et al. Inhibition of diabetic leukostasis and blood-retinal barrier breakdown with a soluble form of a receptor for advanced glycation end products. Invest Ophthalmol Vis Sci. 2007;48:858–65. doi: 10.1167/iovs.06-0495. [DOI] [PubMed] [Google Scholar]
- 80.Bierhaus A, et al. Loss of pain perception in diabetes is dependent on a receptor of the immunoglobulin superfamily. J Clin Invest. 2004;114:1741–51. doi: 10.1172/JCI18058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Yamagishi S, et al. Agents that block advanced glycation end product (AGE)-RAGE (receptor for AGEs)-oxidative stress system: a novel therapeutic strategy for diabetic vascular complications. Expert Opin Investig Drugs. 2008;17:983–96. doi: 10.1517/13543784.17.7.983. [DOI] [PubMed] [Google Scholar]
- 82.Norton GR, Candy G, Woodiwiss AJ. Aminoguanidine prevents the decreased myocardial compliance produced by streptozotocin-induced diabetes mellitus in rats. Circulation. 1996;93:1905–12. doi: 10.1161/01.cir.93.10.1905. [DOI] [PubMed] [Google Scholar]
- 83.Chang KC, et al. Aminoguanidine prevents arterial stiffening in a new rat model type 2 diabetes. Eur J Clin Invest. 2006;36:528–35. doi: 10.1111/j.1365-2362.2006.01672.x. [DOI] [PubMed] [Google Scholar]
- 84.Forbes JM, et al. Advanced glycation end product interventions reduce diabetes-accelerated atherosclerosis. Diabetes. 2004;53:1813–23. doi: 10.2337/diabetes.53.7.1813. [DOI] [PubMed] [Google Scholar]
- 85.Forbes JM, et al. The breakdown of preexisting advanced glycation end products is associated with reduced renal fibrosis in experimental diabetes. FASEB J. 2003;17:1762–4. doi: 10.1096/fj.02-1102fje. [DOI] [PubMed] [Google Scholar]
- 86.Yamagishi S, et al. Pigment epithelium-derived factor inhibits advanced glycation end product-induced retinal vascular hyperpermeability by blocking reactive oxygen species-mediated vascular endothelial growth factor expression. J Biol Chem. 2006;281:20213–20. doi: 10.1074/jbc.M602110200. [DOI] [PubMed] [Google Scholar]
- 87.Yamagishi S, et al. Pigment epithelium-derived factor (PEDF): its potential therapeutic implication in diabetic vascular complications. Curr Drug Targets. 2008;9:1025–9. doi: 10.2174/138945008786786154. [DOI] [PubMed] [Google Scholar]
- 88.Maeda S, et al. Pigment epithelium-derived factor (PEDF) inhibits proximal tubular cell injury in early diabetic nephropathy by suppressing advanced glycation end products (AGEs)-receptor (RAGE) axis. Pharmacol Res. 2011;63:241–8. doi: 10.1016/j.phrs.2010.11.008. [DOI] [PubMed] [Google Scholar]
- 89.Yamagishi S, Matsui T. Pigment epithelium-derived factor (PEDF) and cardiometabolic disorders. Curr Pharm Des. 2014;20:2377–86. doi: 10.2174/13816128113199990473. [DOI] [PubMed] [Google Scholar]
- 90.Yamagishi S, Nakamura K, Matsui T. Potential utility of telmisartan, an angiotensin II type 1 receptor blocker with peroxisome proliferator-activated receptor-gamma (PPAR-gamma)-modulating activity for the treatment of cardiometabolic disorders. Curr Mol Med. 2007;7:463–9. doi: 10.2174/156652407781387073. [DOI] [PubMed] [Google Scholar]
- 91.Yamagishi S, et al. Angiotensin II augments advanced glycation end product-induced pericyte apoptosis through RAGE overexpression. FEBS Lett. 2005;579:4265–70. doi: 10.1016/j.febslet.2005.06.058. [DOI] [PubMed] [Google Scholar]
- 92.Fukami K, et al. AGEs activate mesangial TGF-beta-Smad signaling via an angiotensin II type I receptor interaction. Kidney Int. 2004;66:2137–47. doi: 10.1111/j.1523-1755.2004.66004.x. [DOI] [PubMed] [Google Scholar]
- 93.Matsui T, Nishino Y, Maeda S, Takeuchi M, Yamagishi S. Irbesartan inhibits advanced glycation end product (AGE)-induced up-regulation of vascular cell adhesion molecule-1 (VCAM-1) mRNA levels in glomerular endothelial cells. Microvasc Res. 2011;81:269–73. doi: 10.1016/j.mvr.2011.01.001. [DOI] [PubMed] [Google Scholar]
- 94.Fukami K, et al. Telmisartan inhibits AGE-induced podocyte damage and detachment. Microvasc Res. 2013;88:79–83. doi: 10.1016/j.mvr.2013.04.006. [DOI] [PubMed] [Google Scholar]
- 95.Yamagishi S, Matsui T. Pleiotropic effects of glucagon-like peptide-1 (GLP-1)-based therapies on vascular complications in diabetes. Curr Pharm Des. 2011;17:4379–85. doi: 10.2174/138161211798999456. [DOI] [PubMed] [Google Scholar]
- 96.Yamagishi SI, Fukami K, Matsui T. Crosstalk between advanced glycation end products (AGEs)-receptor RAGE axis and dipeptidyl peptidase-4-incretin system in diabetic vascular complications. Cardiovasc Diabetol. 2015;14:2. doi: 10.1186/s12933-015-0176-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Ishibashi Y, Matsui T, Maeda S, Higashimoto Y, Yamagishi S. Advanced glycation end products evoke endothelial cell damage by stimulating soluble dipeptidyl peptidase-4 production and its interaction with mannose 6-phosphate/insulin-like growth factor II receptor. Cardiovasc Diabetol. 2013;12:125. doi: 10.1186/1475-2840-12-125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Nakashima S, Matsui T, Takeuchi M, Yamagishi SI. Linagliptin blocks renal damage in type 1 diabetic rats by suppressing advanced glycation end products-receptor axis. Horm Metab Res. 2014;46:717–21. doi: 10.1055/s-0034-1371892. [DOI] [PubMed] [Google Scholar]
- 99.Matsui T, et al. Dipeptidyl peptidase-4 deficiency protects against experimental diabetic nephropathy partly by blocking the advanced glycation end products-receptor axis. Lab Invest. 2015;95:525–33. doi: 10.1038/labinvest.2015.35. [DOI] [PubMed] [Google Scholar]
- 100.Kaida Y, et al. DNA aptamer raised against AGEs blocks the progression of experimental diabetic nephropathy. Diabetes. 2013;62:3241–50. doi: 10.2337/db12-1608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Ojima A, Oda E, Higashimoto Y, Matsui T, Yamagishi S. DNA aptamer raised against advanced glycation end products inhibits neointimal hyperplasia in balloon-injured rat carotid arteries. Int J Cardiol. 2014;171:443–6. doi: 10.1016/j.ijcard.2013.12.143. [DOI] [PubMed] [Google Scholar]
- 102.Takeuchi M, et al. Neurotoxicity of advanced glycation end-products for cultured cortical neurons. J Neuropathol Exp Neurol. 2000;59:1094–105. doi: 10.1093/jnen/59.12.1094. [DOI] [PubMed] [Google Scholar]
- 103.Yamamoto Y, et al. Short-chain aldehyde-derived ligands for RAGE and their actions on endothelial cells. Diabetes Res Clin Pract. 2007;77(3 Suppl):S30–40. doi: 10.1016/j.diabres.2007.01.030. [DOI] [PubMed] [Google Scholar]
- 104.Yamagishi S, et al. Positive association between serum levels of advanced glycation end products and the soluble form of receptor for advanced glycation end products in nondiabetic subjects. Metabolism. 2006;55:1227–31. doi: 10.1016/j.metabol.2006.05.007. [DOI] [PubMed] [Google Scholar]
- 105.Nakamura K, et al. Serum levels of soluble form of receptor for advanced glycation end products (sRAGE) are correlated with AGEs in both diabetic and non-diabetic subjects. Clin Exp Med. 2007;7:188–90. doi: 10.1007/s10238-007-0146-7. [DOI] [PubMed] [Google Scholar]
- 106.Nakamura K, et al. Serum levels of soluble form of receptor for advanced glycation end products (sRAGE) are positively associated with circulating AGEs and soluble form of VCAM-1 in patients with type 2 diabetes. Microvasc Res. 2008;76:52–6. doi: 10.1016/j.mvr.2007.09.004. [DOI] [PubMed] [Google Scholar]
- 107.Yanagisawa K, et al. Switching to multiple daily injection therapy with glulisine improves glycaemic control, vascular damage and treatment satisfaction in basal insulin glargine-injected diabetic patients. Diabetes Metab Res Rev. 2014;30:693–700. doi: 10.1002/dmrr.2537. [DOI] [PubMed] [Google Scholar]
- 108.Enomoto M, et al. Positive association of serum levels of advanced glycation end products with thrombogenic markers in humans. Metabolism. 2006;55:912–7. doi: 10.1016/j.metabol.2006.02.019. [DOI] [PubMed] [Google Scholar]
- 109.Yamagishi S, et al. Serum level of advanced glycation end-products (AGEs) is an independent determinant of plasminogen activator inhibitor-1 (PAI-1) in nondiabetic general population. Horm Metab Res. 2007;39:845–8. doi: 10.1055/s-2007-991176. [DOI] [PubMed] [Google Scholar]
- 110.Yamagishi S, et al. Low-density lipoprotein levels are one of the independent determinants of circulating levels of advanced glycation end products in nondiabetic subjects. Clin Cardiol. 2009;32:E12–5. doi: 10.1002/clc.20532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Nakamura K, et al. Circulating advanced glycation end products (AGEs) and soluble form of receptor for AGEs (sRAGE) are independent determinants of serum monocyte chemoattractant protein-1 (MCP-1) levels in patients with type 2 diabetes. Diabetes Metab Res Rev. 2008;24:109–14. doi: 10.1002/dmrr.766. [DOI] [PubMed] [Google Scholar]
- 112.Nakamura T, et al. Circulating levels of advanced glycation end products (AGE) and in-terleukin-6 (IL-6) are independent determinants of serum asymmetric dimethylarginine (ADMA) levels in patients with septic shock. Pharmacol Res. 2009;60:515–8. doi: 10.1016/j.phrs.2009.05.002. [DOI] [PubMed] [Google Scholar]
- 113.Nakamura T, et al. Positive association of serum levels of advanced glycation end products and high mobility group box-1 with asymmetric dimethylarginine in nondiabetic chronic kidney disease patients. Metabolism. 2009;58:1624–8. doi: 10.1016/j.metabol.2009.05.018. [DOI] [PubMed] [Google Scholar]
- 114.Hyogo H, et al. Elevated levels of serum advanced glycation end products in patients with non-alcoholic steatohepatitis. J Gastroenterol Hepatol. 2007;22:1112–9. doi: 10.1111/j.1440-1746.2007.04943.x. [DOI] [PubMed] [Google Scholar]
- 115.Tahara N, Imaizumi T, Takeuchi M, Yamagishi SI. Insulin resistance is an independent correlate of high serum levels of advanced glycation end products (AGEs) and low testosterone in non-diabetic men. Oxid Med Cell Longev. 2010;3:262–265. doi: 10.4161/oxim.3.4.12734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Tahara N, et al. Serum levels of advanced glycation end products (AGEs) are independent correlates of insulin resistance in nondiabetic subjects. Cardiovasc Ther. 2012;30:42–8. doi: 10.1111/j.1755-5922.2010.00177.x. [DOI] [PubMed] [Google Scholar]
- 117.Yamagishi S, Matsui T, Adachi H, Takeuchi M. Positive association of circulating levels of advanced glycation end products (AGEs) with pigment epithelium-derived factor (PEDF) in a general population. Pharmacol Res. 2010;61:103–7. doi: 10.1016/j.phrs.2009.07.003. [DOI] [PubMed] [Google Scholar]
- 118.Tahara N, et al. Serum levels of advanced glycation end products (AGEs) are independently correlated with circulating levels of dipeptidyl peptidase-4 (DPP-4) in humans. Clin Biochem. 2013;46:300–3. doi: 10.1016/j.clinbiochem.2012.11.023. [DOI] [PubMed] [Google Scholar]
- 119.Tahara N, et al. Clinical and biochemical factors associated with area and metabolic activity in the visceral and subcutaneous adipose tissues by FDG-PET/CT. J Clin Endocrinol Metab. 2015;100:E739–47. doi: 10.1210/jc.2014-3896. [DOI] [PubMed] [Google Scholar]
- 120.Tahara N, et al. Positive association between serum level of glyceraldehyde-derived advanced glycation end products and vascular inflammation evaluated by [(18)F]fluorodeoxyglucose positron emission tomography. Diabetes Care. 2012;35:2618–25. doi: 10.2337/dc12-0087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Kajikawa M, et al. Ratio of serum levels of AGEs to soluble form of RAGE is a predictor of endothelial function. Diabetes Care. 2015;38:119–25. doi: 10.2337/dc14-1435. [DOI] [PubMed] [Google Scholar]
- 122.Ueda S, et al. Serum levels of advanced glycation end products (AGEs) are inversely associated with the number and migratory activity of circulating endothelial progenitor cells in apparently healthy subjects. Cardiovasc Ther. 2012;30:249–54. doi: 10.1111/j.1755-5922.2011.00264.x. [DOI] [PubMed] [Google Scholar]
- 123.Fukushima Y, et al. Relationship between advanced glycation end products and plaque progression in patients with acute coronary syndrome: the JAPAN-ACS sub-study. Cardiovasc Diabetol. 2013;12:5. doi: 10.1186/1475-2840-12-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Jinnouchi Y, et al. Atorvastatin decreases serum levels of advanced glycation end products (AGEs) in patients with type 2 diabetes. Clin Exp Med. 2006;6:191–3. doi: 10.1007/s10238-006-0115-6. [DOI] [PubMed] [Google Scholar]
- 125.Kimura Y, et al. Atorvastatin decreases serum levels of advanced glycation endproducts (AGEs) in nonalcoholic steatohepatitis (NASH) patients with dyslipidemia: clinical usefulness of AGEs as a biomarker for the attenuation of NASH. J Gastroenterol. 2010;45:750–7. doi: 10.1007/s00535-010-0203-y. [DOI] [PubMed] [Google Scholar]
- 126.Nakamura T, et al. Atorvastatin reduces proteinuria in non-diabetic chronic kidney disease patients partly via lowering serum levels of advanced glycation end products (AGEs) Oxid Med Cell Longev. 2010;3:304–7. doi: 10.4161/oxim.3.5.13069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Sakata K, et al. Efficacy of alogliptin, a dipeptidyl peptidase-4 inhibitor, on glucose parameters, the activity of the advanced glycation end product (AGE)-receptor for AGE (RAGE) axis and albuminuria in Japanese type 2 diabetes. Diabetes Metab Res Rev. 2013;229:624–30. doi: 10.1002/dmrr.2437. [DOI] [PubMed] [Google Scholar]
- 128.Tsunosue M, et al. An alpha-glucosidase inhibitor, acarbose treatment decreases serum levels of glyceraldehyde-derived advanced glycation end products (AGEs) in patients with type 2 diabetes. Clin Exp Med. 2010;10:139–41. doi: 10.1007/s10238-009-0074-9. [DOI] [PubMed] [Google Scholar]
- 129.Ahmed N, et al. Assay of advanced glycation endproducts in selected beverages and food by liquid chromatography with tandem mass spectrometric detection. Mol Nutr Food Res. 2005;49:691–9. doi: 10.1002/mnfr.200500008. [DOI] [PubMed] [Google Scholar]
- 130.Matsui T, Oda E, Higashimoto Y, Yamagishi SI. Glyceraldehyde-derived pyridinium (GLAP) evokes oxidative stress and inflammatory and thrombogenic reactions in endothelial cells via the interaction with RAGE. Cardiovasc Diabetol. 2015;14:1. doi: 10.1186/s12933-014-0162-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Usui T, Shimohira K, Watanabe H, Hayase F. Detection and determination of glyceraldehyde-derived pyridinium-type advanced glycation end products in streptozotocin-induced diabetic rats. Biosci Biotechnol Biochem. 2007;71:442–8. doi: 10.1271/bbb.60497. [DOI] [PubMed] [Google Scholar]