Abstract
A randomized controlled trial for an innovative alcohol-adapted anger management treatment (AM) for outpatient alcohol dependent individuals scoring moderate or above on anger is described. AM treatment outcomes were compared to those of an empirically-supported intervention, Alcoholics Anonymous Facilitation treatment (AAF). Clients in AM, relative to clients in AAF, were hypothesized to have greater improvement in anger and anger-related cognitions and lesser AA involvement during the six-month follow-up. Anger-related variables were hypothesized to be stronger predictors of improved alcohol outcomes in the AM treatment condition and AA involvement was hypothesized to be a stronger predictor of alcohol outcomes in the AAF treatment group. Seventy-six alcohol dependent men and women were randomly assigned to treatment condition and followed for six months after treatment end. Both AM and AAF treatments were followed by significant reductions in heavy drinking days, alcohol consequences, anger, and maladaptive anger-related thoughts and increases in abstinence and self-confidence regarding not drinking to anger-related triggers. Treatment with AAF was associated with greater AA involvement relative to treatment with AM. Changes in anger and AA involvement were predictive of posttreatment alcohol outcomes for both treatments. Change in trait anger was a stronger predictor of posttreatment alcohol consequences for AM than for AAF clients; during-treatment AA meeting attendance was a stronger predictor of posttreatment heavy drinking and alcohol consequences for AAF than for AM clients. Anger-related constructs and drinking triggers should be foci in treatment of alcohol dependence for anger-involved clients.
Keywords: Alcohol dependence, outpatient treatment, anger, anger management treatment, Alcoholics Anonymous Facilitation treatment, randomized controlled trial
1.0 Introduction
Return to problematic drinking often occurs after treatment for alcohol dependence, even when that treatment was initially successful. Depending on how relapse is defined (consuming a single posttreatment drink, resumption of pretreatment drinking levels, experience of negative alcohol consequences), data indicate that 58–66% of treated individuals relapse three months after treatment and 50–90% relapse by a year posttreatment (Armor, Polich, & Stambul, 1978; Lowman et al., 1996). Relapsed individuals often start another negative cycle of alcohol-related problems and suffering in themselves and others (Lowman et al., 1996; Marlatt & Gordon, 1980). Notwithstanding the progress that has been made in the alcohol use disorders treatment field, innovative treatment strategies are still needed.
1.1 Anger and Alcohol: A Potentially Bad Mix
Anger and alcohol use and dependence have been linked in both theory and empirical studies for several decades. Anger and related emotions (irritability, frustration, annoyance) are positively associated with alcohol consumption and adverse alcohol consequences in the general population (Karyadi & King, 2011; Leibsohn, Oetting & Deffenbacher, 1994; Rabinovitz, 2014; Thomas, 1997). In addition, individuals with alcohol use disorders (AUD) score higher than those without AUDs on measures of anger and aggression (Bácskai, Czobor & Gerevich, 2011; Demirbas, Ilhan, & Dogan, 2011; Handelsman et al., 2000; Kelly, Stout, Tonigan, Magill & Pagano, 2010; Leite, Machado & Lara, 2014; O’Farrell, Fals-Stewart, Murphy, & Murphy, 2003; Small & Lewis, 2004). For example, in a large sample of individuals attending Alcoholics Anonymous (AA; see Kelly et al., 2010), anger was associated with heavier drinking, and this group began at the 98th percentile on trait anger and remained at the 89th percentile 15 months later. Such findings suggest that individuals with AUDs tend to be both alcohol- and anger-involved.
Although the relationship between alcohol and behavioral aggression is complex (Cavell & Malcolm, 2007), meta-analyses consistently suggest that alcohol increases aggression (Bushman & Cooper, 1990; Hull & Bond, 1986; Ito, Miller, & Pollock, 1996). Further, anger may exacerbate the alcohol – aggression relationship. For example, among males in their 20’s with high marital satisfaction and high alcohol dependence, those that scored low on hostility reported a .10 probability of marital aggression; for their counterparts who scored high on hostility, this probability rose to .72 (Leonard & Blane, 1992). In stark comparison, probability of marital aggression among those low on alcohol dependence was not influenced by hostility (.01 probability). Others have documented the relationship between alcohol consumption and violence toward intimate partners (e.g., Lisco, Parrott, & Tharp, 2012) and sexual minorities (e.g., Parrott, Peterson, & Bakeman, 2011). Anger, alcohol, and aggression relationships have been demonstrated in various laboratory paradigms where those high on trait anger and aggressiveness tend to engage in greater aggression when provoked and under the influence of alcohol (Miller, Parrott, & Giancola, 2009). Anger, either additively or in interaction with alcohol, was related to increases in negative anger- and alcohol-consequences (Leibsohn et al., 1994). That is, high-anger, alcohol-involved individuals were at greatest risk for a range of negative anger and alcohol consequences. Providing anger management skills to such individuals might help lower anger and conflict that would alter these negative consequence trajectories.
Anger is also implicated in relapse following treatment. At a simple level, anger, irritability and low frustration tolerance are common as a person copes with alcohol withdrawal and making significant life changes. Alcohol consumption reduces negative emotional states, including anger, and is negatively reinforcing via tension reduction (Sher & Levenson, 1982). Anger also contributes to relapse via psychological and interpersonal influences. For example, individuals with AUDs reported that negative emotional states, in which anger plays a significant part, contributed to 37–38% of intrapersonal triggers for relapse; interpersonal conflict, generally involving anger, accounted for 12–18% of interpersonal situations which put the person at risk for relapse (Marlatt & Gordon, 1980; Lowman et al., 1996). Stout, Longabaugh and Rubin (1996) reported that 22–28% of patients attributed relapse to situations involving “hostility/aggression,” and McKay, Maisto, and O’Farrell (1996) found that feelings of anger and being uptight were the two most common emotional precipitants of relapse in male problem drinkers who received behavioral couples’ therapy for alcohol problems. Although evidence indicates that relapse is typically not precipitated by a single emotion or stressor (e.g., Wallace, 1989; Zywiak, Connors, Maisto, & Westerberg, 1996), research shows that elevated anger plays a significant role in relapse, either as the primary precipitant or as a significant part of a complex set of personal and interpersonal factors influencing relapse. Enhancing anger management skills may improve coping with anger as well as enhance accessing other cognitive and behavioral coping skills disrupted by anger arousal. Either or both pathways may decrease the likelihood of relapse.
1.2 Addressing Anger in the Treatment of Alcohol Problems
According to AA philosophy, anger and resentment are important issues for recovery from alcohol problems (c.f., AA, 2001; Kelly, Stout, Tonigan, Magill, & Pagano, 2010), e.g., AA members must address their anger and resentments or they are at risk for relapse. In fact, anger is the only such issue to have its own specific AA worksheet on which individuals address angry thoughts and feelings. Although anger is a central construct in AA, one study (Kelly et al., 2010) revealed that the frequency of AA attendance was unrelated to changes in anger and anger reduction did not mediate the relationship between AA attendance and positive drinking outcomes. Another AA-based study (O’Farrell et al., 2003) is somewhat more positive. Prior to intervention, clients tended to be very high on measures of anger and aggression. Although mediational analyses were not conducted, the 60% who relapsed continued to remain high on anger and aggression compared to community controls, whereas the 40% who did not relapse were similar to community controls on anger and aggression, suggesting that those who did not relapse may have reduced anger and aggressiveness, and this reduction in anger and aggression may be associated with alcohol outcomes.
The emphasis on addressing anger in AA notwithstanding, there is little empirical evaluation regarding anger management in alcohol and substance abuse treatment. Indirect evidence comes from Project MATCH. Specifically, clients marked by higher anger did better at one- and three-year follow-up in the motivational enhancement condition than in cognitive-behavioral therapy (CBT) or the AAF condition (Karno & Longabaugh, 2004). That is, angry clients seemed to fare better in the less directive and structured condition than in the more structured CBT and AAF conditions. These findings, however, do not directly address anger management as part of intervention, but only how client characteristics interacted with other treatments. The CBT condition in Project MATCH which focused on enhancing cognitive-behavioral coping skills included two optional sessions focused on anger. The first session addressed increasing awareness of anger triggers and angry feelings, whereas the second focused on calming self-talk and problem-solving for angering situations. The effectiveness of the anger management component, however, is not clear. Because the anger intervention was optional, relatively brief and embedded within a larger CBT treatment, it is not possible to tease out its therapeutic effects.
In spite of the theoretical and empirical associations between anger, drinking and AUDs, our review revealed only four studies evaluating anger-specific treatment in alcohol and substance treatment. In the first, six alcohol- or other drug-involved patients with a history of anger and violence received 12 stress inoculation-like sessions of cognitive, relaxation, and behavioral coping skills training focusing upon anger management (Awalt, Reilly, & Shopshire, 1997). Individual case data suggested positive anger and abstinence outcomes. A larger study of 91 cocaine abusers with problems controlling their anger (Reilly & Shopshire, 2000) suggested positive anger outcomes for the 55% who completed eight or more of twelve sessions (operational definition of treatment completion) with 50% abstinent from cocaine and 40% abstinent from all substances. The third study, Lin, Mack, Krahn and Baskin (2004) compared seven substance dependence clients who completed 12 sessions of Forgiveness Therapy (targeting anger, anxiety and depression) with seven clients who completed 12 sessions of standard alcohol and drug counseling. At posttreatment, those clients completing the Forgiveness Therapy sessions reported greater improvements in composite anger and anxiety relative to those clients completing the alcohol and drug counselling sessions. The fourth study recruited 78 alcohol-dependent men with co-occurring interpersonal violence and compared alcohol outcomes among clients who received a cognitive-behavioral Substance Abuse Domestic Violence group program with those who received a Twelve-Step Facilitation group program (Easton et al., 2007). Clients receiving the anger and aggression focused cognitive-behavioral group therapy reported significantly less alcohol use during the 12 weeks of treatment relative to the comparison group. Although these initial studies each have methodological limitations, they provide early support for anger-based interventions in substance abusing populations.
1.3 Predicting Treatment Outcomes
Predicting outcomes of individuals with alcohol dependence following a treatment experience has long been of interest in the field (e.g., Edwards et al., 1988). Edwards et al. indicate that several pretreatment characteristics (e.g., personality, employment characteristics) predicted posttreatment outcomes. Since this research was conducted, the study of predictors of outcome has progressed substantially (c.f., Adamson, Sellman & Frampton, 2009 for a review). Recently reported characteristics and constructs that predict outcomes include pretreatment and/or postreatment alcohol involvement (Bottlender & Soyka, 2005; Witkiewitz, 2011), alcohol expectancies (Haskin & Oei, 2007; Young, Connor & Feeney, 2011), coping strategies (Hasking & Oei, 2007) negative affect and psychopathology (Bottlender & Soyka, 2005; Witkiewitz & Villarroel, 2009), and temptation to drink (Witkiewitz, 2013).
One line of research has robustly demonstrated the predictive value of abstinence self-efficacy in predicting aspects of alcohol involvement posttreatment outcomes (Adamson et al., 2009; Demmel, Nicolai & Jenko, 2006; Ludwig, Tadayon-Manssuri, Strik & Moggi, 2013; Sugarman et al., 2014; Witkiewitz, Donovan & Hartzler, 2012). The Adamson, et al. (2009) review suggests that self-confidence in avoiding relapse – and during-treatment improvements in self-confidence – is a consistent predictor of treatment outcomes (Adamson et al., 2009). The literature does not, however, describe whether specific areas of self-confidence, such as confidence specifically related to coping with anger and related emotions, predict outcomes.
1.4 Hypotheses
The goal of the current research was to conduct a randomized clinical trial to evaluate the efficacy of AM for alcohol dependent individuals. In order to provide a stringent test of AM, we used Alcoholics Anonymous Facilitation treatment (AAF) as a comparison condition to assess AM’s efficaciousness. Specifically, we hypothesized that clients in AM, relative to clients in AAF, would report greater improvement in anger and related emotions and anger-related cognition outcomes and lesser AA involvement during the six-month follow-up. In addition, we hypothesized that improvements in anger and anger-related cognitions would be stronger predictors of improved alcohol outcomes in the AM treatment condition relative to the AAF treatment condition. In contrast, we hypothesized that greater AA involvement would be a stronger predictor of alcohol outcomes among clients in the AAF treatment group, relative to clients in the AM treatment group. We hypothesized that both AM and AAF treatments would be associated with post-treatment improvements in alcohol outcomes.
2.0 Method
2.1 Recruitment
Clients were recruited through advertisements in local newspapers for a 17-month period beginning March, 2011. Eligibility was established in an initial phone interview and during baseline assessment. Inclusion criteria included: (a) being between the ages of 18 and 65; (b) meeting Diagnostic and Statistical Manual for Mental Disorders IV (APA, 1994) criteria for alcohol dependence; (c) English fluency; (d) consent to participate in all facets of research; and (e) answering “moderately” (the midpoint) or above on the Brief Symptom Inventory (BSI; Derogatis, 1992) item regarding how much the person was “distressed by feeling easily annoyed or irritated” during the past week. Exclusion criteria included: (a) court mandate; (b) evidence of acute psychosis or severe cognitive impairment; (c) medications that may modify alcohol use (i.e., disulfiram, naltrexone); (d) substance abuse treatment within the last 6 months; and (e) IV drug use.
2.2 Assessments
Assessments focused on three overarching constructs: alcohol involvement, anger and anger-related cognitions and AA involvement. The α reliabilities reported below are from the pretreatment assessment. At pretreatment, treatment end, and three and six months after the end of treatment (3- and 6-month follow-ups), clients completed an in-person assessment at the University at Buffalo Research Institute on Addictions’ Clinical Research Center (CRC). All in-person assessments included a breath test to ensure the participant a .000 blood alcohol content (BAC); if not, the session was rescheduled. If a client was unable to attend an assessment, the interview was conducted via telephone and questionnaires were mailed. Interviewers were blind to intervention condition.
2.2.1 Alcohol involvement
We conducted Time Line Follow-Back interviews (Sobell & Sobell, 1992) and calculated percent days abstinent (PDA) and drinks per drinking day (DDD). The pretreatment interview spanned the six months prior to treatment. For subsequent assessments, the interview spanned the time starting with the end of the previous interview and ending with the day before the current interview. PDA (arc sine transformed) and DDD (logarithmic transformed) measures were calculated for the pretreatment (six month) period, the treatment period and the six posttreatment month periods.
On the 15-item Short Inventory of Problems (SIP; Miller, Tonigan, & Longabaugh, 1995), respondents reported, on a 4-point scale (0 = never, 3 = daily/almost daily), how often their alcohol use led to specific negative consequences (e.g., being unhappy, taking foolish risks, or damaged a friendship or close relationship). The SIP score consisted of the sum across the 15 items.
2.2.2 Anger and anger-related cognitions
Three measures assessed angry emotions. On the 10-item Trait Anger Scale (STAXI-Trait; α = .87), respondents rated on a 4-point scale (1 = almost never, 4 = almost always) how each item (e.g., I am quick tempered, I fly off the handle) made them generally feel or react (Spielberger, 1999); the Trait Anger Scale was calculated as the mean of these 10 items. On the 5-item hostility scale (BSI-hostility, α = .78) from the Brief Symptom Inventory (Derogatis, 1992), participants rated on a 5-point scale (0 = not all, 4 = extremely) how much during the last week that they had been distressed by the content described in the item (e.g., anger outbursts that you could not control). On the 6-item hostility scale (PANAS-hostility; α = .83) from the Positive and Negative Affect Schedule—Expanded Form (Watson & Clark, 1994), respondents rated on 5-point scale (1 = very slightly or not at all, 5 = extremely) how a mood adjective (e.g., hostility) described them.
The Angry Cognitions Scale (Martin & Dahlen, 2007) presented six frustrating/provocative scenarios (e.g., you get home from the restaurant drive-through and realize that you were given the wrong food) followed by six possible thought reactions items. One thought item addressed adaptive thinking (e.g., “oh well, getting angry won’t bring me what I ordered”) and five others assessed maladaptive themes of overgeneralizing, inflammatory labeling, catastrophizing, demandingness and misattributing causation (e.g., “they always screw up my order,” “that place is totally worthless”). Participants rated items on a 5-point scale (1 = very unlikely, 5 = very likely) according to how likely they were to think the thought described. The maladaptive angry cognition scale (Cog-Anger; α = .95) is the mean of 30 maladaptive item responses.
Following the format of the Drug-Taking Confidence Questionnaire (Sklar, Annis & Turner, 1997), we developed a 5-item measure of self-confidence for resisting the urge to drink heavily when faced with anger-related drinking triggers (SC-Anger; α = .94). Items began with the stem, “I would be able to resist the urge to drink heavily,” followed by the specific item content (e.g., if I was feeling frustrated, if I was feeling irritated, if I was angry and thinking about it a lot). Participants rated their confidence on an 11-point scale with ratings in 10-point increments (0 = not at all confident, 100 = very confident).
2.2.3 AA Involvement
Three measures reflected involvement with AA. The Time Line Follow-Back interview generated a measure of AA attendance (i.e., reported frequency of AA meetings attended per month [AA-Days]) for the pretreatment period, treatment period, and six follow-up months. Two other measures were derived from the Alcoholics Anonymous Involvement Questionnaire (Tonigan, Connors, & Miller, 1996). In response to a single item, participants reported the number of 12 AA steps “worked” (AA-Steps). We added eight additional AA behaviors to the five original items (including celebrating an AA sobriety birthday, helping with meeting activities, having or being an AA sponsor) for a 13-item AA-behavior scale (AA-Beh). Participants rated items on a 5-point scale (0 = never, 4 = always) according to how often the participant engaged in each AA behavior.
2.2.5 Additional measures
Total number of therapy sessions attended served as a measure of treatment involvement. At treatment end, clients completed the eight-item Client Satisfaction Questionnaire (Attkisson & Zwick, 1982). Clients rated items (e.g., “to what extent has our program met your needs”) on 4-point Likert scales with varying response anchors. Higher scores indicate greater treatment satisfaction (α = .96).
2.3 Procedure
2.3.1 Random assignment
Following completion of the pretreatment assessment, clients were assigned to one of the two treatment conditions and to therapist via urn random assignment (Stout, Wirtz, Carbonari & Del Boca, 1994) with the constraint of balancing gender and pretreatment BSI-hostility scores across treatment conditions. The urn random assignment was carried out by the project coordinator via a computerized program.
2.3.2 Treatment
Treatment consisted of twelve 60-minute sessions at the CRC. Both treatments were delivered by female, masters-level social workers in accordance with treatment manuals for each condition; both therapists delivered both treatment protocols. Therapists received treatment manuals; four days of training including role plays, demonstrations and simulations; and supervised experience in both modalities with several clients prior to beginning the study. In order to maintain adherence to the treatment protocols, therapists referred to a condition-specific and session-specific content outline during each session. These content outlines provided reminders as to the manualized session content relevant to each therapy session.
The first two authors, experienced in AM and AAF treatment protocols, supervised therapists one hour per week in each condition throughout interventions. During supervision, each active case was discussed individually with regard to adherence to the manualized treatment protocol and the specific content of the session.
All treatment sessions included a breath test to ensure that participants had .000 BAC; if not, the session was rescheduled. AM and AAF included common alcohol treatment content. Sessions began with reviews of cravings, high-risk situations, and any alcohol consumption between each session. There was a brief mention of AA attendance and coverage of drink refusal skills and relapse prevention. Based on the content of treatment protocols, anger regulation material comprised approximately 0.4% of the AAF condition and 64.2% of the AM condition. AA-related material comprised approximately 45.0% of the AAF condition and 5.4% of the AM condition. Alcohol-related treatment material comprised approximately 54.6% of the AAF condition and 30.4% of the AM condition.
2.3.2.1 Alcohol-Adapted Anger Management Treatment (AM)
AM focused on the development of relaxation and cognitive coping skills for anger regulation (see Table 1 for outline of AM). Cognition-relaxation coping skills (CRCS; Deffenbacher & McKay, 2000) was chosen as the anger management protocol for four reasons. First, its coping skills approach fits conceptually into coping skills relapse prevention conceptualizations (Marlatt & Gordon, 1980; Witkiewitz & Marlatt, 2004). Second, studies support anger reduction effects for the cognitive (Dahlen & Deffenbacher, 2001; Deffenbacher, Dahlen, Lynch, Morris, & Gowensmith, 2000; Deffenbacher, Story, Brandon, Hogg, & Hazaleus, 1988; Hazaleus & Deffenbacher, 1986; Novaco, 1976) and relaxation (Deffenbacher, Demm & Brandon, 1986; Deffenbacher, Filetti, Lynch, Dahlen, & Oetting, 2002; Deffenbacher & Stark, 1992) components as well as their combination (Deffenbacher et al., 2002; Deffenbacher, Oetting, Huff, Cornell, & Dallager,1996; Deffenbacher, & Stark, 1992; McCloskey, Noblett, Deffenbacher, Gollan, & Coccaro, 2008; Novaco,1976). Moreover, meta-analyses (Beck & Fernandez, 1998; Del Vecchio & O’Leary, 2004; DiGuiseppe & Tafrate, 2003; Edmondson & Conger, 1996) show CRCS to be an effective intervention that had roughly equivalent effects to other interventions. Third, including both cognitive and relaxation coping skills provides a range of coping skills to assist most individuals with anger problems, i.e., this intervention addresses anger issues for most people. Fourth, CRCS is manualized (Deffenbacher & McKay, 2000), such that there was a publicly available manual to adapt to a 12-session format focusing heavily on anger management for alcohol dependent individuals scoring moderate or above on an index of anger.
Table 1.
Overview of Treatment Content for Alcohol-adapted Anger Management and AA Facilitation Therapies
| Alcohol-adapted Anger Management | Alcoholics Anonymous Facilitation | |
|---|---|---|
| 1 | Assessment; Introduction to Alcohol Treatment | Assessment; Introduction to Alcohol Treatment |
| 2 | Problem solving; rationale for AM; introduction to self- monitoring | Problem solving; AA discussion; decisional balance |
| 3 | Relaxation strategies; trigger thoughts for anger | AA Discussion, AA readings, AA attendance contract |
| 4 | Relaxation strategies | Problem solving; AA readings |
| 5 | Cognitions contribute to anger; distorted thinking; coping thoughts | AA Readings; drink refusal |
| 6 | Rehearse Mild scene; coping skills rehearsal | AA Step 1; powerlessness, acceptance, denial; AA readings |
| 7 | Mid-way evaluation of progress; review treatment plan; drink refusal | Mid-way evaluation of progress; review treatment plan |
| 8 | Rehearse Moderate scene; distorted thinking; coping thoughts | Getting Active in AA; sponsors; AA readings |
| 9 | Rehearse Mod-High scene; less therapist guidance | AA Step 2; AA Step 3; surrender, Higher Power |
| 10 | Rehearse High scene; best coping thoughts; maintenance | High-risk situations, problem solving |
| 11 | Rehearse Worst scene; less therapist guidance | Relapse prevention, high-risk situations |
| 12 | Alcohol and Anger relapse prevention; termination | Review of progress, problem solving, termination |
Early AM sessions also focused upon having clients identify external situations that elicited anger and on the internal cognitive, emotional, and physiological aspects of arousal. The first four sessions trained clients in progressive relaxation and in the relaxation coping skills of: (a) relaxation without tension (i.e., focusing on area of tension and releasing tension); (b) breathing-cued relaxation (i.e., relaxing more with each of 3–5 deep breaths); (c) cue-controlled relaxation (i.e., relaxing more to the self-presentation of a word or phrase that had been paired with relaxation); (d) relaxation imagery (i.e., visualizing a personal relaxation image); and (e) relaxing by unobtrusive tension-release of specific problem muscle groups (e.g., tensing the shoulders by shrugging firmly). The cognitive component of anger arousal was also introduced in the first four sessions. Therapists helped clients identify anger-engendering cognitions and develop anger-reducing alternatives. Between sessions, clients received homework handouts, practiced relaxation skills and identified and developed alternative cognitive responses for anger situations. In subsequent sessions, therapists and clients reviewed homework and linked it to positive changes being made or problems identified. In later sessions, clients induced anger by visualizing anger scenes and employed relaxation and cognitive coping skills to lower anger arousal. Over sessions, the level of anger arousal was increased, and therapist assistance in coping skill retrieval was decreased. Between sessions, clients applied coping skills in naturally occurring, real life anger events. They also applied skills to coping with anger situations with a high risk for alcohol consumption or relapse. These efforts were self-monitored and reviewed in the sessions.
2.3.2.2 Alcoholics Anonymous Facilitation Treatment (AAF)
Content for this treatment condition was drawn from the Project MATCH Twelve Step Facilitation Therapy (Nowinski, Baker & Carroll, 1999) and an Alcoholics Anonymous Facilitation treatment (Walitzer, Dermen & Barrick, 2009). This treatment condition focused primarily on facilitation of mutual-help groups (principally AA), structured problem solving for alcohol-related problems and monitoring the client’s status and progress. AAF emphasized AA and other mutual-group involvement and associated reading materials; discussion of common barriers to attendance, rationales for attendance and involvement and AA Steps 1, 2, and 3; and discussion and review of meetings attended. If anger-related material was brought up by the client, therapists encouraged the client to use problem-solving strategies. Later sessions also emphasized attendance at AA or other groups to aid maintenance and relapse prevention (see Table 1 for outline of AAF).
2.4 Analytic Strategy
Two sets of analyses were conducted. First, hierarchical random effects models (SAS 9.3) examined posttreatment functioning (i.e., alcohol involvement, anger and anger-related cognitions and AA involvement during the six months of follow up) as a function of treatment condition. Clients served as random factors and repeated measures (baseline, during-treatment, 3-month and 6-month follow up) were nested within clients to accommodate for the fact that repeated within client measures were likely correlated; mixed effect models were used (SAS 9.3). Time was modeled piece-wise so that potential changes from pretreatment to during-treatment (Pre-post effect) and over the course of follow up (Follow-up effect) could be assessed separately. The main effects of Pre-post and Follow-up and their interactions with treatment condition were modeled. With regard to anger and anger-related cognitions variables, the clinical significance of pre- to posttreatment change was evaluated with the Reliable Change index (RC: Jacobson & Truax, 1991). RC index provides a determination of whether the magnitude of change for each client is both clinically significant and statistically reliable.
The second set of analyses assessed whether during-treatment changes in anger and anger-related cognitions and during-treatment AA involvement predicted posttreatment alcohol involvement (PDA, DDD and SIP score), controlling for the relevant pretreatment alcohol involvement measure. Further, we tested whether this predictive ability varied as a function of treatment condition. During-treatment changes in anger measures were calculated as the difference between each anger measure as assessed at pretreatment and at treatment end. For AA-Days, AA-Beh and AA-Step, the end-of-treatment score (i.e., the report of behavior during the treatment period) was used. To understand how changes in process variables affected outcomes, treatment condition, a process variable score and the interaction between treatment condition and the process variable score were included in each model. Time after treatment (months 1 through 6) was modeled as a continuous variable.
For both sets of analyses, mixed effects models (SAS 9.3) were used. This allowed us to model clients as random factors and to nest repeated measures within each client. Mixed models accommodated for the fact that repeated measures from each client were correlated and accommodated for missing data with maximum likelihood estimation.
3.0 Results
3.1 Participants
Table 2 displays demographic characteristics for the sample as a whole and separately by treatment condition. There were no significant differences between treatment conditions.
Table 2.
Participant Characteristics at Baseline as a Function of Treatment Condition
| Variable | Total | AAF n = 40 |
AM n = 36 |
|---|---|---|---|
| Age | 46.3 (8.8) | 46.7 (8.6) | 45.9 (9.0) |
| Gender | |||
| Male | 55.3% | 57.5% | 52.8% |
| Female | 44.7% | 42.5% | 47.2% |
| Marital Status | |||
| Single | 2.7% | 2.6% | 2.8% |
| Married or cohabitating | 66.7% | 71.8% | 61.1% |
| Divorced, separated, widowed | 33.7% | 25.6% | 36.1% |
| Ethnicity | |||
| White | 77.3% | 74.4% | 80.6% |
| Black | 12.0% | 15.4% | 8.3% |
| Other | 10.7% | 10.3% | 11.1% |
| Employed | 61.8% | 55.0% | 69.4% |
| Years of Education | 14.4 (2.4) | 13.9 (2.5) | 14.8 (3.4) |
Although no objective indicators of other substance use were obtained (e.g., urine screens), participants were asked whether they had used illicit substances. Infrequent other drug use was reported in the sample. For the six-month baseline period, 64.5% of the sample reported no illicit drug use, and another 10.5% of the sample reported average use at less than one time per month; there was no significant between-condition difference. The most frequent drug used was marijuana; 30% of the sample reported use of this drug at least once during the six-month baseline period. With regard to baseline levels of anger, males scored at the 75th percentile and females at the 55th percentile on the STAXI-trait anger scale.
3.2 Attendance and Treatment Satisfaction
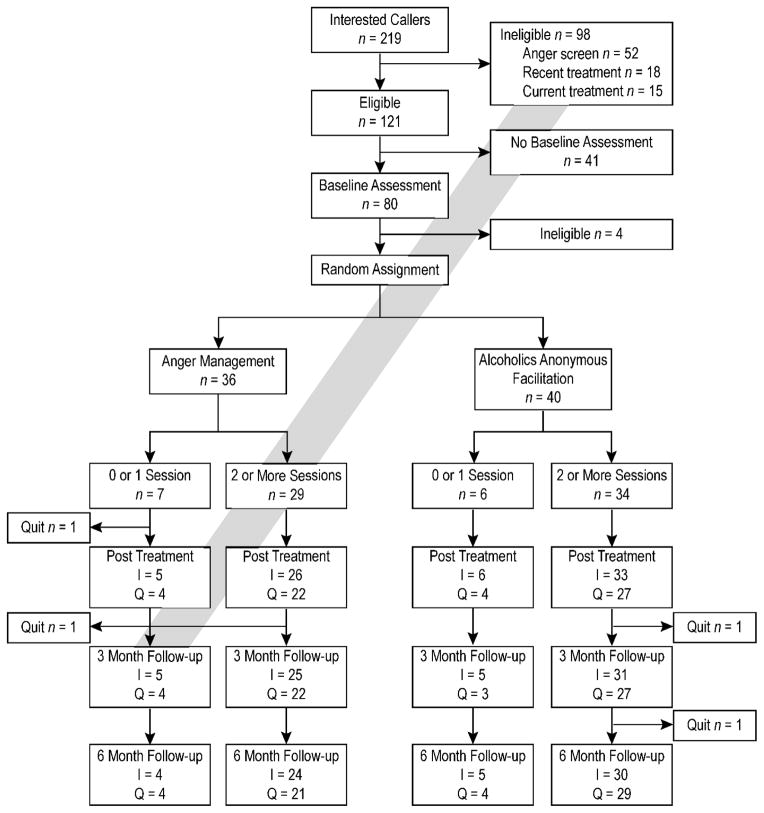
Figure 1 displays participant flow through the study. Participants in the intent-to-treat sample averaged 6.4 sessions out of a possible 12 (SD = 4.4) with 13 attending 0 or 1 sessions and 18 attending all sessions. The AM and AAF treatment conditions were not significantly different for attendance and treatment satisfaction. Specifically, attendance at AAF (M = 7.3, SD = 4.4) and AM (M = 5.4, SD = 4.4) were statistically similar, t(74) = 1.93. Overall, clients were satisfied with treatment (M = 3.4, SD = 0.6), and AAF (M = 3.5, SD = 0.6) and AM (M = 3.2, SD = 0.7) did not differ statistically in satisfaction, t(54) = 1.82.
Figure 1.
Participant flow through the randomized controlled trial. I = interview assessment completed.
Q = questionnaire assessment completed.
3.3 Treatment Outcome Effects
3.3.1 Alcohol outcomes
Alcohol measures reflected a consistent pattern. Clients improved significantly from pre- to posttreatment on all three alcohol measures, PDA and DDD, Fs(1, 68) = 119.28 and 32.19, ps < .001, and SIP, F(1, 61) = 39.50, p < .001, and maintained these gains at 3- and 6-month follow-ups. Analyses revealed no evidence of differential treatment effects as Condition X Pre-post and Condition X Follow-up interactions were not significant. During the first posttreatment month, 28.2% of the AAF condition clients reported continuous abstinence; this figure was 29.0% for the AM condition clients.
3.3.2 Anger outcomes
Anger measures also revealed a common pattern. From pre- to posttreatment, clients reduced anger on all measures, STAXI-trait, BSI-hostility, and PANAS-hostility, Fs(1, 62) = 22.45, 24.45, and 61.45, ps < .001. No other main effects or interactions were significant, suggesting maintenance of anger reduction during follow-up and no between-treatment differences. Although not statistically significant, 28% of AM clients evidenced a positive RC on PANAS-hostility relative to only 14% of AAF clients (X2[1] = 1.73). For the sample as a whole, 27% of clients of AM clients evidenced a positive RC on BSI-hostility (relative to 20% of AAF clients) and 38% of AM clients evidenced a positive RC on STAXI-trait (relative to 37% of AAF clients).
3.3.3 Anger-related cognitions outcomes
Clients reported significant pre- to posttreatment reductions in maladaptive angry thoughts (Cog-Anger) and increases in self-confidence regarding not drinking heavily in angry situations (SC-Anger), Fs(1, 62) = 18.25 and 51.57, ps < .001, respectively. Analyses yielded no other significant main effects or interactions, suggesting maintenance of reductions of maladaptive angry thinking and improved self-confidence in controlling alcohol consumption when angry and no differential treatment effects for either condition. With regard to RC, 38% of clients in AM evidenced a positive RC on Con-Anger (relative to 40% of AAF clients); 31% of clients in AM evidenced a positive RC for SC-Anger (relative to 31% of AAF clients).
3.3.4 AA involvement outcomes
Although AA-Days was statistically stable from pretreatment through 6-month assessment, a near-significant Pre-post main effect was noted, F(1, 68) = 3.73, p = .058. Table 3 indicates that AA-Days may have increased from before to after treatment. No additional main or interaction effects were noted. During the treatment period, 46% of clients assigned to the AAF condition attended at least one AA meeting relative to only 16% of those assigned to the AM condition; this difference is statistically significant (X2[1] = 7.06, p = .008).
Table 3.
Primary Study Measures as a Function of Treatment Condition and Wave of Assessment
| Pretreatment | Post treatment | 3-Months | 6-Months | |||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| AM
|
AAF
|
AM
|
AAF
|
AM
|
AAF
|
AM
|
AAF
|
|
| Percent Days Abstinent | 31.03% (27.81) | 35.82% (30.29) | 63.86% (35.36) | 75.00% (30.51) | 65.81% (36.30) | 71.82% (34.43) | 68.73% (33.38) | 73.49% (32.82) |
| Drinks per Drinking Day | 8.91 (6.00) | 8.06 (4.78) | 5.34 (8.37) | 6.97 (12.77) | 5.02 (8.66) | 4.37 (4.19) | 4.63 (5.69) | 3.67 (4.13) |
| Short Inventory of Problems | 20.44 (9.78) | 21.98 (8.09) | 13.04 (10.44) | 13.37 (11.85) | 9.31 (11.52) | 11.00 (11.69) | 11.60 (10.77) | 12.31 (12.44) |
| STAXI – Trait Anger | 1.88 (0.58) | 1.91 (0.58) | 1.67 (0.47) | 1.71 (0.44) | 1.52 (0.45) | 1.56 (0.45) | 1.64 (0.54) | 1.58 (0.45) |
| BSI – Hostility | 0.84 (0.74) | 0.84 (0.63) | 0.55 (0.68) | 0.42 (0.45) | 0.38 (0.61) | 0.45 (0.53) | 0.43 (0.48) | 0.36 (0.30) |
| PANAS – Hostility | 2.48 (0.90) | 2.39 (0.81) | 1.75 (0.70) | 1.56 (0.62) | 1.68 (0.86) | 1.74 (0.82) | 2.07 (0.81) | 1.73 (0.70) |
| Anger Maladaptive Cognitions | 11.65 (2.88) | 11.54 (3.06) | 10.42 (2.96) | 10.74 (2.84) | 9.61 (3.69) | 10.47 (2.77) | 10.59 (3.36) | 10.13 (2.65) |
| Anger-Situations Self-Confidence | 45.00 (27.39) | 42.60 (29.08) | 65.23 (32.06) | 70.06 (28.92) | 74.31 (30.47) | 64.00 (33.58) | 70.08 (27.01) | 67.52 (31.63) |
| AA Meetings/Month | 0.06 (0.28) | 0.13 (0.54) | 0.86 (3.02) | 1.25 (2.29) | 1.31 (4.80) | 1.97 (4.26) | 1.17 (3.32) | 2.08 (4.04) |
| AA Behaviors | 0.67 (2.04) | 0.65 (1.41) | 1.48 (2.22) | 2.68 (3.13) | 0.73 (1.80) | 2.13 (3.51) | 1.24 (2.86) | 2.36 (3.80) |
| AA Steps Worked | 0.30 (1.06) | 0.28 (1.04) | 0.88 (1.74) | 2.97 (4.09) | 0.65 (2.23) | 2.67 (3.78) | 1.20 (2.81) | 2.36 (3.63) |
Notes. AM = alcohol-adapted anger management treatment. AAF = Alcoholics Anonymous facilitation treatment. STAXI = Spielberger State Trait Anxiety Inventory. BSI = Brief Symptom Inventory. PANAS = Positive and Negative Affect Scale.
AA-Beh and AA-Steps revealed significant Pre-post main effects, Fs(1, 62) =15.23 and 21.12, ps < .001 and significant Condition x Pre-post interactions qualified these effects, Fs(1, 62) = 4.89 and 9.69, ps = .031 and .003. Post hoc simple effects tests indicated that AAF clients significantly increased both AA-Beh and AA-Steps during treatment, ts(62) = 4.53 and 5.71, ps < .001, whereas AM participants did not change on these measures, (ts[62] = 1.15 and 1.00). Analyses yielded no further significant main effects or interactions.
3.4 Prediction of Alcohol Involvement Outcomes
3.4.1 Anger predictors
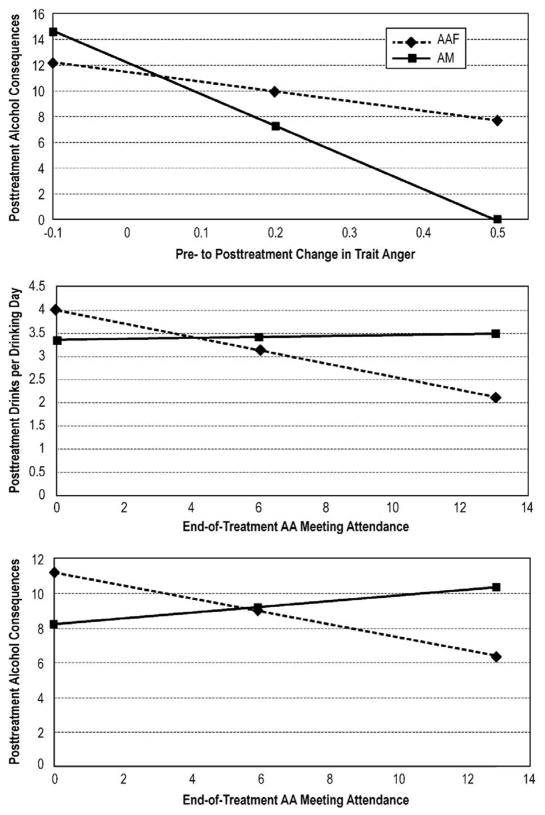
Pre- to end-of-treatment change in STAXI-trait significantly predicted posttreatment negative drinking consequences (F(1, 51) = 8.22, p < .006). Analyses also revealed a significant STAXI-trait X Condition interaction on the SIP, F(1, 51) = 5.76, p = .020, which indicated change in trait anger was a stronger predictor of adverse alcohol consequences for AM clients (F[1,23] = 21.81, p < .001) than for AAF clients (F[1,27] = 3.49, p = .072). Figure 2 (panel A) indicates that greater during-treatment improvement in trait anger was associated with lesser alcohol consequences within the AM condition than for AAF, whereas lesser trait anger improvements were associated with more posttreatment alcohol problems for both AM and AAF treatment conditions.
Figure 2.
Panel A: Interaction between Treatment Condition with during-treatment change in trait anger on posttreatment drinking problems. Panel B: Interaction between Treatment Condition with end-of-treatment AA attendance on posttreatment drinks per drinking day. Panel C: Interaction between Treatment Condition with end-of-treatment AA attendance on posttreatment adverse alcohol consequences.
Each graph plotted the model-generated means at the 25% and the 75% percentiles from the x-axis distributions.
There was a significant main effect for the STAXI-trait change score on PDA (F [1, 51] = 16.37, p < .001) and a near significant interaction between STAXI-trait X Condition (F[1, 51] = 3.18, p = .080). Post hoc analyses indicated that, as hypothesized, the predictive strength of the STAXI-change score may have been stronger in the AM condition (F[1, 23] = 9.20, p = .006) than in the AAF condition (F[1, 27] = 6.28, p = .019). Similarly, there was a significant main effect for the STAXI-trait change score on DDD (F[1, 51] = 7.21, p = .010) and a near significant interaction between the STAXI-trait X Condition (F[1, 51] = 3.43, p = .070). As hypothesized, post hoc analyses indicated that the STAXI-change score predicted the SIP in the AM condition (F[1, 23] = 7.88, p = .010) and not in the AAF condition (F[1, 27] = 1.00, p = .325).
The PANAS-hostility change score significantly predicted PDA (F[1, 51] = 14.16, p < .001), DDD (F[1,51] = 7.84, p = .007) and SIP (F[1, 51] = 10.38, p = .002) with no further significant main effects or interactions noted. BSI-hostility change did not predict alcohol outcomes.
3.4.2 Anger-related cognition predictors
Reductions in maladaptive angry cognitions (Cog-Anger) predicted all drinking outcomes, PDA and DDD, Fs(1, 51) = 7.06 and 5.23, p = .010 and p = .026, and SIP, F(1, 51) = 7.12, p = .010. Increased self-confidence in managing alcohol consumption in the face of anger (SC-Anger) also predicted positive change in alcohol measures, PDA and DDD, Fs(1, 51) = 37.70 and 15.16, ps < .001; SIP F(1, 51) = 7.13, p = .010. No significant interactions were found on either measure suggesting that strength of prediction was similar within each treatment condition.
3.4.3 AA involvement predictors
Overall, AA involvement measures assessed at treatment end predicted drinking outcomes. Specifically, AA attendance predicted PDA and DDD, Fs(1, 61) = 8.48 and 8.18, ps = .005 and .006. A significant interaction between AA-Days and treatment condition was found for DDD, F(1, 61) = 7.39, p = .008. Figure 2 (panel B) indicates that AA meeting attendance was a stronger predictor of heavy drinking within the AAF condition (F[1, 32] = 14.02, p = .001) than within AM (F[1, 26] = 0.01). Also, an interaction between AA-Days with treatment condition on the SIP was found, F(1, 57) = 4.74, p = .034, suggesting that AA meeting attendance was a stronger predictor of adverse alcohol consequences within AAF (F[1, 30] = 4.29, p = .047) than within AM treatment (F[1, 26] = 1.06, p = .312; see Figure 2, panel C).
Finally, AA-Beh predicted both PDA and DDD, Fs(1, 50) = 8.11 and 6.24, ps = .006 and .016. AA-Steps predicted PDA and DDD, F(1, 50) = 6.45 and 8.28, p =.014 and .006. No further main effects or interactions were significant.
4.0 Discussion
4.1 Outcomes of Alcohol-adapted Anger Management Treatment
Alcohol-adapted anger management treatment is a new intervention focusing on clients’ acquiring an understanding of the connection of anger to alcohol consumption and relapse and developing cognitive and relaxation coping skills with which to reduce anger and related emotions and disconnect the anger-drinking linkage. In this initial evaluation, as a group, moderate-to-high anger clients receiving the alcohol-adapted anger management treatment reported increased abstinence and reduced drinks per drinking day and adverse alcohol consequences. This treatment protocol was also associated with reductions in anger, maladaptive anger-related cognition and increases in confidence regarding not drinking to anger-related triggers. With regard to trait anger, we report a reliable change index of 38% within our AM treatment condition, similar to the 41% reported in Deffenbacher et al. (1996). Changes in anger-related variables were stable during the six-month follow-up. Improvements in multiple anger-related variables were predictive of improved alcohol outcomes.
When considering the efficacy of a treatment protocol, it is critical to evaluate alcohol involvement outcomes in the context of a protocol which has known efficacy (i.e., either an inactive control protocol or an efficacious treatment). We examined the effects of alcohol-adapted anger management treatment in comparison to a known efficacious treatment: Alcoholics Anonymous Facilitation (see Kelly, Magill & Stout, 2009; Walitzer, Dermen & Barrick, 2009). In the present study, clients receiving the alcohol-adapted anger management treatment reported improved six-month alcohol involvement outcomes that were not significantly different from clients receiving the AA Facilitation treatment. Analyses indicated no significant outcome differences between the two treatment protocols, suggesting generally comparable pre- to posttreatment improvements in abstinence, heavy drinking frequency and negative consequences for alcohol-adapted anger management treatment and the AA Facilitation treatment. The current data provide early positive support for an anger-focused intervention in the treatment of alcohol dependence, suggesting that it is worthy of further refinement and evaluation and may be of use with anger- and alcohol-involved individuals.
As anticipated, clients receiving the alcohol-adapted anger management treatment reported positive reductions in anger and related emotions and maladaptive cognitive style and increased self-confidence regarding not drinking heavily in response to anger-related triggers; no differences in these constructs were found between treatment conditions. We had hypothesized that clients in the alcohol-adapted anger management treatment would report differentially greater improvements on these anger-related variables relative to clients in the AA Facilitation treatment; this was not supported.
4.2 Outcomes of AA Facilitation Treatment
As noted in section 4.1, in the present study AA Facilitation treatment was also associated with increased abstinence and decreased drinking and negative consequences during the six months posttreatment. These improvements mirror the findings of the three-year follow up of Project MATCH clients (Project MATCH Research Group, 1998) demonstrating improvements in alcohol involvement posttreatment among clients receiving AA-based treatment. Further, outcome analyses indicated that the Project MATCH clients treated with Twelve-Step Facilitation treatment reported greater posttreatment improvements in abstinence and lower drinks per drinking day relative to clients treated with Cognitive-Behavioral Therapy (Project MATCH Research Group; 1998). Thus, our findings are consistent with previous research documenting improved drinking outcomes for clients treated with AA approaches (c.f., Kelly et al., 2009).
As hypothesized, clients receiving this treatment were more likely to attend an AA meeting and evidenced increased AA behaviors and steps worked, and to a greater extent than that reported by clients receiving the alcohol-adapted anger management treatment. These findings are consistent with the work of Pagano, White, Kelly, Stout and Tonigan (2013) which documents that AA-based treatment is initially associated with increased AA meeting attendance, behaviors and step work. As a caveat, however, Pagano et al.’s 10-year follow up of a subset of Project MATCH outpatient clients suggests that this increased AA involvement may be relatively-short lived; their data suggest that these increases dissipated after the initial year after treatment. As the present follow-up period was only six months, these increases in AA involvement may not be stable over the long term. However, this over-time decline in initially increased AA behaviors noted by Pagano et al. (2013) may represent the process of clients working to maintain treatment gains during the especially-challenging early posttreatment period and then decreasing their involvement further into recovery.
As did clients in the alcohol-adapted anger management treatment, clients receiving AA facilitation also reported significant reductions of anger, maladaptive anger-related cognitive style and increases in confidence in resisting angry drinking triggers. These improvements were maintained over the six-month follow up, suggesting durability and maintenance of these changes. The present research documenting improvements in multiple dimensions of anger extends our understanding of the multiple beneficial outcomes associated with AA-based treatments.
4.3 Predicting Treatment Outcomes
To further our understanding of alcohol-adapted anger management treatment and AA facilitation treatment outcomes, the present data also evaluated several constructs targeted for change during treatment and their ability to predict posttreatment alcohol outcomes, both in the sample as a whole and differentially by condition. We considered anger measures and indices of AA involvement as potential candidates in this regard.
4.3.1 Anger and related emotions and cognitions
During-treatment improvements in two of the three anger variables – trait anger and hostile affect – were associated with posttreatment improvements in alcohol outcomes. Further, during-treatment improvements in trait anger were more strongly associated with reductions in drinking problems during follow up within the alcohol-adapted anger management treatment condition, relative to the strength of this relationship within the AA Facilitation treatment condition. Consistent with this finding, near-significant effects were noted indicating that during-treatment improvements in trait anger were also more strongly predictive of improved drinking outcomes in the alcohol-adapted anger management treatment, relative to the AA Facilitation treatment. Together, these findings support the therapeutic rationale that specifically targeting anger in the alcohol-adapted anger management treatment is directly connected with reductions in posttreatment alcohol involvement. Of note however, this differential predictive ability was not replicated with other anger measures.
During-treatment improvements in the remaining anger and anger-related cognition measures predicted clients’ positive posttreatment alcohol involvement; however, predictive strength was not significantly different between treatment conditions. For both treatment conditions, improvements in hostile affect (but not psychiatric hostility), anger-related cognitions and self-confidence regarding not drinking heavily in response to anger-related drinking triggers predicted multiple aspects of alcohol involvement outcomes.
There is scant existing literature on the relationship between treatment levels of anger and posttreatment alcohol outcomes in those seeking treatment for alcohol dependence. One report does describe this relationship; Kelly et al. (2010) reports nonsignificant trends between anger and several measures of alcohol outcomes in a secondary analysis of Project MATCH data. Specifically, time-lagged assessments of posttreatment anger predicted, but to a relatively weak extent, (ps < .10), posttreatment abstinence and drinks per drinking day. Our data indicate that clients receiving AA facilitation treatment reported decreased anger over the course of treatment and that positive changes in anger predicted positive posttreatment alcohol outcomes. Both our findings and those reported by Kelly et al. (2010) are consistent with the hypothesis that during-treatment anger changes may predict alcohol outcomes.
4.3.2 AA involvement
Consistent with our previous work (Walitzer et al., 2009), we hypothesized that AA Facilitation treatment would lead to greater AA involvement, and increased AA involvement would predict improved drinking outcomes among these clients. These hypotheses received some support. Clients receiving the AA facilitation treatment reported significantly more AA behaviors and steps worked than clients receiving alcohol-adapted anger management treatment. Further, condition-specific differences in the strength of relationships between these AA variables and alcohol outcomes were observed; greater during-treatment AA attendance was predictive of reduced heavy drinking to a stronger extent for the AA facilitation treatment, relative to these relationships within the alcohol-adapted anger management treatment. This differential effect was also marginally present for during-treatment AA meeting attendance and posttreatment drinking consequences. In sum, these findings underscore that AA meeting attendance, behaviors, and steps worked are important therapeutic factors in AA facilitation treatment.
Kelly et al. (2011) examined several potential mediators of the positive effect of AA-based treatment on alcohol outcomes. Their secondary analyses of the Project MATCH data implicate adaptive changes in clients’ social networks, increases in abstinence self-efficacy, increased spirituality and reductions in depression as potential mechanisms of AA’s beneficial effects. The Kelly et al. (2010) report suggests that anger, although associated with drinking outcomes, did not serve as a mechanism for AA’s effects on alcohol outcomes. Our data are not conclusive on this point; however, anger remains an important construct for AA processes.
4.4 Theoretical, Clinical and Future Research Implications
Section 1.1 outlined a number of direct and indirect mechanisms that describe how anger and related emotions may be related to alcohol consumption and relapse after alcohol dependence treatment. Alcohol-adapted anger management treatment directly addresses these links by helping clients identify anger triggers and internal cues of anger arousal and providing cognitive and relaxation coping skills with which to lower anger and break up anger-alcohol links, in addition to focusing on alcohol-specific skills such as drink refusal. Initial support for alcohol-adapted anger management treatment suggests that clinicians and researchers may have an additional intervention to address anger-alcohol associations. Clinically, not all alcohol-involved clients accept the philosophies and approaches of AA and other mutual-help groups. AM may be a particularly relevant tool for such anger- and alcohol-involved clients. Also, it may be important to consider alcohol-adapted anger management treatment primarily for combined anger- and alcohol-involved clients, as these were the clients eligible for the present study. To increase the efficacy of this new treatment protocol, future anger management interventions might focus more explicitly on anger-related cues that have triggered alcohol consumption in the past and on feelings of agitation and irritation that may be part of alcohol withdrawal. Improving tolerance of general emotional distress, and improving clients’ ability to experience emotional distress (e.g., Bornovalova, Gratz, Daughters, Hunt & Lejuez, 2012; Linehan, 1993) – therapeutic techniques not included in the present alcohol-adapted anger management therapy – may also enhance treatment outcomes. Our treatment protocol focused on relaxation skills and cognitive therapy to manage and reduce the experience of anger; tolerating the experience of remaining angry affect may be an important and additionally therapeutic component for improving both anger and alcohol involvement outcomes.
Alcohol dependence and significant alcohol involvement not reaching the level of dependence are often comorbid with a variety of anger-related consequences including interpersonal violence and conflict (Chermack et al., 2010). Research has strongly supported the inclusion of efficacious interventions to address this serious problem area as a part of alcohol dependence treatment (Chermack et al., 2008; Rothman et al., 2008). Research focusing on alcohol-adapted anger management treatment might include assessment and intervention of couples conflict and interpersonal violence (such as Easton et al., 2007) to determine whether AM provides additional strategies to address this important clinical issue.
AA Facilitation treatment can also address anger-alcohol links as several AA tenets and practices address linkages between anger, resentment, and relapse (see Kelly et al., 2010). Even without specific discussion of anger material, our AA Facilitation treatment was associated with decreased anger and maintained these reductions. These reductions were similar to those in the anger-focused intervention, suggesting that the present AA Facilitation Treatment at least partially attended to these important processes. In line with the findings of Kelly et al. (2010), our study is one of the few which focused on and documented anger reduction in an AA-based intervention. Assessing these critical AA constructs (anger and resentment) is important both clinically as well as in future AA-related research.
Finally, although beyond the scope of the present paper, consideration of multiple dimensions of affect and affective disorders may lead to a deeper understanding of the role of anger and other negative affect states in the treatment of alcohol dependence. Although little empirical work addresses the role of anger in the treatment of alcohol dependence, research has focused on other affect experiences. The Kelly et al. (2011) secondary analyses of the Project MATCH data indicate that attending AA meetings may reduce depressive symptoms, thereby improving drinking outcome. A review of randomized controlled trials suggests that addressing depression and anxiety disorders may improve drinking outcomes among individuals being treated for alcohol dependence (Hobbs, Kushner, Lee, Reardon & Maurer, 2011); this may be especially relevant to women with anxiety (Farris, Epstein, McCrady & Hunter-Reel, 2012). Finally, improvements in positive affect may also play an important role in treatment outcomes; enhancing positive affect may serve as a protective effect on the experience of stress for alcohol dependent individuals (see McHugh, Kaufman, Frost, Fitzmaurice & Weiss, 2013). Taken together, this body of research emphasizes the role of emotions in general as important therapeutic targets in alcohol dependence treatment.
4.5 Limitations
As with all research, this study has limitations which should be considered in interpreting our findings. First, the modest sample size did not allow for detection of meaningful but relatively small between-group differences and effect sizes. However, the sample size was appropriate to the state of knowledge in the field, this being the first randomized controlled trial with a new and untested intervention. Relatively small between-condition differences may have gone undetected, and future research should consider larger sample sizes to increase power to detect more modest effect sizes.
Second, although therapists completed intensive training and training cases, measures of therapist adherence or competence were not obtained. It is thus possible that therapists did not abide by treatment manuals and procedures or did so poorly, outside of awareness of the supervisors. Challenges to treatment fidelity such as a Rosenthal Effect and non-adherence to the treatment protocol cannot be ruled out. Future research should incorporate stringent treatment fidelity methodology in order to document adherence to protocol. Relatedly, our experimental design did not include a no-treatment control group and thus internal validity threats such as regression toward the mean and maturation cannot be ruled out as alternate explanations for significant pre- to posttreatment differences in the study variables. Previous work, however, has demonstrated the efficacy of the present-study’s comparison condition – the AAF treatment protocol; thus, although these threats to internal validity are possible explanations for the positive pre- to post-treatment findings, the previously-demonstrated efficacy of AAF is consistent with the interpretation that the pre- to posttreatment change is a function of treatment experience.
Third, although women comprised 48% of the sample, low statistical power prevented an assessment of gender as a possible moderator of treatment outcomes. Although the empirical literature is limited and somewhat mixed, men and women may differ in the experience, expression and management of anger (see Sloan, 2012, for a review); in the relationship between anger and drinking (Morrison, Noel & Ogle, 2012); and in relapse precipitants (Walitzer & Dearing, 2006). Future research should assess gender as a moderator of treatment outcome and use that information to inform the content of alcohol-adapted anger management for alcohol dependent men and women.
Finally, despite positive ratings of treatment satisfaction, attendance was less than ideal for both interventions. Analyses utilized the intent-to-treat sample, i.e., all participants without regard to attendance and treatment completion. Potential modest treatment responses among clients with little or no exposure to treatment may have obscured positive effects for those receiving all or nearly all of the intervention. Future research should continue to explore ways to maximize treatment participation, assess dose-response relationships between participation and outcomes and develop and evaluate interventions designed to increase readiness for and acceptance of novel anger management interventions (see Howells & Day, 2003).
4.6 Summary
In sum, outcomes for outpatient alcohol dependent clients receiving alcohol-adapted anger management treatment were generally similar to, and not significantly different from, those for clients who received an established efficacious therapy, i.e., AA Facilitation treatment. Two interventions, one new and provisional and one established and empirically supported, were both associated with improved alcohol outcomes and reduced anger and cognitions. Clinically, these findings suggest that anger-related treatment content is a worthy therapeutic focus and that anger-related drinking situations can be beneficially addressed in treatment for alcohol dependence. Moreover, some findings were consistent with theoretically relevant vectors of change; improvements in trait anger more strongly predicted alcohol changes within alcohol-adapted anger management treatment than within AA Facilitation treatment, whereas AA involvement more strongly predicted alcohol outcomes within AA Facilitation treatment. Future research may elucidate whether theory-consistent improvements in anger serve to mediate the beneficial outcomes within alcohol-adapted anger management treatment and whether pretreatment levels of anger (and/or anger-related drinking situations) serve to moderate response to this treatment.
Highlights.
Innovative treatments for alcohol dependence are needed to improve outcomes.
Anger management (AM) for alcohol dependent clients reduces anger, drinking and consequences.
AA Facilitation (AAF) for alcohol dependent clients reduces anger, drinking and consequences.
Improvements in trait anger are especially influential to AM treatment outcomes.
Frequency of AA meetings is especially influential to AAF treatment outcomes.
Acknowledgments
Portions of these data have been presented at the August 2014 American Psychological Association annual convention. We acknowledge gratefully the efforts of the project’s therapists and interviewers: Diane Augustino, Aileen Touhy Dlugosz, Mark Duerr, Sarah Pearson, Molly Rath and Laura Slawiak Weichmann. Graphics assistance was provided by Robert Marcyznski, RIA Graphics Editor and tables were prepared by Kimberly Larkin. Also, appreciation is due to Joseph Lucke, RIA Senior Statistician.
Funding
This research was supported by a National Institute on Alcohol Abuse and Alcoholism at the National Institutes of Health grant (R01 AA17603) to the first author. The NIAAA and NIH had no further role in study design, in the collection, analysis and interpretation of the data; in the writing of the report, or in the decision to submit the paper for publication. The views herein do not necessarily represent the official views of the NIAAA or the NIH.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Adamsom SJ, Sellman JD, Frampton C. Patient predictors of alcohol treatment outcome: A systematic review. Journal of Substance Abuse Treatment. 2009;36:75–86. doi: 10.1016/j.jsat.2008.05.007. [DOI] [PubMed] [Google Scholar]
- Alcoholics Anonymous: The Story of How Many Thousands of Men and Women Have Recovered from Alcoholism. 4. A.A. World Services; 2001. Alcoholics Anonymous. [Google Scholar]
- American Psychological Association. Diagnostic and Statistical Manual of Mental Disorders. 4. APA; Washington, DC: 1994. [Google Scholar]
- Armor D, Polich J, Stambul H. Alcoholism and treatment. New York: Wiley; 1978. [Google Scholar]
- Attkisson CC, Zwick R. The client satisfaction questionnaire: Psychometric properties and correlations with service utilization and psychotherapy outcome. Evaluation and Program Planning. 1982;5:233–237. doi: 10.1016/0149-7189(82)90074-x. [DOI] [PubMed] [Google Scholar]
- Awalt RM, Reilly PM, Shopshire MS. The angry patient: An intervention for managing anger in substance abuse treatment. Journal of Psychoactive Drugs. 1997;29:353–358. doi: 10.1080/02791072.1997.10400562. [DOI] [PubMed] [Google Scholar]
- Bácskai E, Czobor P, Gerevich J. Gender differences in trait aggression in young adults with drug and alcohol dependence compared to the general population. Progress in Neuro-Psychopharmacology & Biological Psychiatry. 2011;35:1333–1340. doi: 10.1016/j.pnpbp.2011.04.005. [DOI] [PubMed] [Google Scholar]
- Beck R, Fernandez E. Cognitive-behavioral therapy in the treatment of anger: A meta-analysis. Cognitive Therapy and Research. 1998;22:63–74. [Google Scholar]
- Bornovalova MA, Gratz KL, Daughters SB, Hunt ED, Lejuez CW. Initial RCT of a distress tolerance treatment for individuals with substance use disorders. Drug and Alcohol Dependence. 2012;122:70–76. doi: 10.1016/j.drugalcdep.2011.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bottlender M, Soyka M. Efficacy of an intensive outpatient rehabilitation program in alcoholism: Predictors of outcome 6 months after treatment. European Addiction Research. 2005;11:132–137. doi: 10.1159/000085548. [DOI] [PubMed] [Google Scholar]
- Bushman BJ, Cooper HM. Effects of alcohol on human aggression: An integrative research review. Psychological Bulletin. 1990;107:341–354. doi: 10.1037/0033-2909.107.3.341. [DOI] [PubMed] [Google Scholar]
- Cavell TA, Malcolm KT. Introduction: The anger-aggression relation. In: Cavell TA, Malcolm KT, editors. Anger, aggression, and interventions for interpersonal violence. Mahwah, NJ: Lawrence Erlbaum Associates; 2007. pp. xv–xxxi. [Google Scholar]
- Chermack ST, Grogan-Kaylor A, Perron BE, Murray RL, De Chavez P, Walton MA. Violence among men and women in substance use disorder treatment: A multi-level event-based analysis. Drug and Alcohol Dependence. 2010;112:194–200. doi: 10.1016/j.drugalcdep.2010.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chermack ST, Murray RL, Walton MA, Booth BA, Wryobeck J, Blow FC. Partner aggression among men and women in substance use disorder treatment: Correlates of psychological and physical aggression and injury. Drug and Alcohol Dependence. 2008;98:35–44. doi: 10.1016/j.drugalcdep.2008.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahlen ER, Deffenbacher JL. Anger management. In: Lyddon WJ, Jones JV Jr, editors. Empirically supported cognitive therapies: Current and future applications. New York: Springer Publishing; 2001. pp. 163–181. [Google Scholar]
- Deffenbacher JL, Dahlen ER, Lynch RS, Morris CD, Gowensmith WN. An application of Beck’s cognitive therapy to general anger reduction. Cognitive Therapy and Research. 2000;24:689–697. [Google Scholar]
- Deffenbacher JL, Demm PM, Brandon AD. High general anger: Correlates and treatment. Behaviour Research and Therapy. 1986;24:481–489. doi: 10.1016/0005-7967(86)90014-8. [DOI] [PubMed] [Google Scholar]
- Deffenbacher JL, Filetti LB, Lynch RS, Dahlen ER, Oetting ER. Cognitive-behavioral treatment of high anger drivers. Behaviour Research and Therapy. 2002;40:895–910. doi: 10.1016/s0005-7967(01)00067-5. [DOI] [PubMed] [Google Scholar]
- Deffenbacher JL, McKay M. Overcoming situational anger and general anger: Therapist protocol. Oakland, California: New Harbinger Publications; 2000. [Google Scholar]
- Deffenbacher JL, Oetting ER, Huff ME, Cornell GR, Dallager CJ. Evaluation of two cognitive-behavioral approaches to general anger reduction. Cognitive Therapy and Research. 1996;20:551–573. [Google Scholar]
- Deffenbacher JL, Stark RS. Relaxation and cognitive-relaxation treatments of general anger. Journal of Counseling Psychology. 1992;39:158–167. [Google Scholar]
- Deffenbacher JL, Story DA, Brandon AD, Hogg JA, Hazaleus SL. Cognitive and cognitive-relaxation treatments of anger. Cognitive Therapy and Research. 1988;12:167–184. [Google Scholar]
- Del Vecchio TD, O’Leary KD. Effectiveness of anger treatments for specific anger problems: A meta-analytic review. Clinical Psychology Review. 2004;24:15–34. doi: 10.1016/j.cpr.2003.09.006. [DOI] [PubMed] [Google Scholar]
- Demirbas H, Ilhan IO, Dogan YB. Assessment of the mode of anger expression in alcohol dependent male inpatients. Alcohol and Alcoholism. 2011;46:542–546. doi: 10.1093/alcalc/agr056. [DOI] [PubMed] [Google Scholar]
- Demmel R, Nicolai J, Jenko DM. Self-efficacy and alcohol relapse: Concurrent validity of confidence measures, self-other discrepancies, and prediction of treatment outcome. Journal of Studies on Alcohol. 2006;67:637–641. doi: 10.15288/jsa.2006.67.637. [DOI] [PubMed] [Google Scholar]
- Derogatis LR. The Brief Symptom Inventory: Administration, Scoring & Procedures Manual II. Baltimore, MD: Clinical Psychometric Research, Inc; 1992. [Google Scholar]
- DiGiuseppe R, Tafrate RC. Anger treatment for adults: A meta-analytic review. Clinical Psychology: Science and Practice. 2003;10:70–84. [Google Scholar]
- Easton CJ, Mandel DL, Hunkele KA, Nich C, Rounsaville BJ, Carroll KM. A cognitive behavioral therapy for alcohol-dependent domestic violence offenders: An integrated substance abuse-domestic violence treatment approach (SADV) The American Journal on Addictions. 2007;16:24–31. doi: 10.1080/10550490601077809. [DOI] [PubMed] [Google Scholar]
- Edmondson CB, Conger JC. A review of treatment efficacy for individuals with anger problems: Conceptual, assessment, and methodological issues. Clinical Psychology Review. 1996;16:251–275. [Google Scholar]
- Edwards G, Brown D, Oppenheimer E, Sheehan M, Taylor C, Duckitt A. Long term outcome for patients with drinking problems: The search for predictors. British Journal of Addictions. 1988;83:917–927. doi: 10.1111/j.1360-0443.1988.tb01584.x. [DOI] [PubMed] [Google Scholar]
- Farris SG, Epstein EE, McCrady BS, Hunter-Reel D. Do co-morbid anxiety disorders predict drinking outcomes in women with alcohol use disorders? Alcohol and Alcoholism. 2012;47:143–148. doi: 10.1093/alcalc/agr155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Handelsman L, Stein JA, Bernstein DP, Oppenheim SE, Rosenblum A, Magura S. A laten variable analysis of coexisting emotional deficits in substance abusers: Alexithymia, hostility and PTSD. Addictive Behaviors. 2000;25:423–428. doi: 10.1016/s0306-4603(99)00010-6. [DOI] [PubMed] [Google Scholar]
- Haskin PA, Oei TPS. Alcohol expectancies, self-efficacy and coping in an alcohol-dependent sample. Addictive Behaviors. 2007;32:99–113. doi: 10.1016/j.addbeh.2006.03.024. [DOI] [PubMed] [Google Scholar]
- Hazaleus SL, Deffenbacher JL. Relaxation and cognitive treatments of anger. Journal of Consulting and Clinical Psychology. 1986;54:222–226. doi: 10.1037//0022-006x.54.2.222. [DOI] [PubMed] [Google Scholar]
- Hobbs JDJ, Kushner MG, Lee SSL, Reardon SM, Maurer EW. Meta-analysis of supplemental treatment for depressive and anxiety disorders in patients being treated for alcohol dependence. The American Journal on Addictions. 2011;20:319–329. doi: 10.1111/j.1521-0391.2011.00140.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howells K, Day A. Readiness for anger management: Clinical and theoretical issues. Clinical Psychology Review. 2003;23:319–337. doi: 10.1016/s0272-7358(02)00228-3. [DOI] [PubMed] [Google Scholar]
- Hull JG, Bond CF., Jr Social and behavioral consequences of alcohol consumption and expectancy: A meta-analysis. Psychological Bulletin. 1986;99:347–360. [PubMed] [Google Scholar]
- Ito TA, Miller N, Pollock VE. Alcohol and aggression: A meta-analysis on the moderating effects of inhibitory cues, triggering events, and self-focused attention. Psychological Bulletin. 1996;120:60–82. doi: 10.1037/0033-2909.120.1.60. [DOI] [PubMed] [Google Scholar]
- Karno MP, Longabaugh R. What do we know? Process analysis and the search for a better understanding of Project MATCH’s anger-by-treatment matching effect. Journal of Studies on Alcohol. 2004;65:501–512. doi: 10.15288/jsa.2004.65.501. [DOI] [PubMed] [Google Scholar]
- Karyadi KA, King KM. Urgency and negative emotions: Evidence for moderation on negative alcohol consequences. Personality and Individual Differences. 2011;51:635–640. [Google Scholar]
- Kelly JF, Hoeppner B, Stout RL, Pagano M. Determining the relative importance of the mechanisms of behavior change within Alcoholics Anonymous: A multiple mediator analysis. Addiction. 2011;107:289–299. doi: 10.1111/j.1360-0443.2011.03593.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Magill M, Stout RL. How do people recover from alcohol dependence? A systematic review of the research on mechanism of behavior change in Alcoholics Anonymous. Addiction Research and Theory. 2009;17:236–259. [Google Scholar]
- Kelly JF, Stout RL, Tonigan JS, Magill M, Pagano ME. Negative affect, relapse, and Alcoholics Anonymous (AA): Does AA work by reducing anger? Journal of Studies on Alcohol. 2010;71:434–444. doi: 10.15288/jsad.2010.71.434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leibsohn MT, Oetting ER, Deffenbacher JL. Effects of trait anger on alcohol consumption and consequences. Journal of Child and Adolescent Substance Abuse. 1994;3:17–32. [Google Scholar]
- Leite L, Machado LN, Lara DR. Emotional traits and affective temperaments in alcohol users, abusers and dependents in a national sample. Journal of Affective Disorders. 2014;163:65–69. doi: 10.1016/j.jad.2014.03.021. [DOI] [PubMed] [Google Scholar]
- Leonard KE, Blane HT. Alcohol and marital aggression in a national sample of young men. Journal of Interpersonal Violence. 1992;7:19–30. [Google Scholar]
- Lin WF, Mack D, Enright RD, Krahn D, Baskin TW. Effects of Forgiveness Therapy on anger, mood, and vulnerability to substance use among inpatient substance-dependent clients. Journal of Consulting and Clinical Psychology. 2004;72:1114–1121. doi: 10.1037/0022-006X.72.6.1114. [DOI] [PubMed] [Google Scholar]
- Linehan MM. Cognitive Behavioral Treatment of Borderline Personality Disorder. Guilford Press; New York, NY: 1993. [Google Scholar]
- Lisco CG, Parrott DJ, Tharp AT. The role of heavy episodic drinking and hostile sexism in men’s sexual aggression toward female intimate partners. Addictive Behaviors. 2012;37:1264–1270. doi: 10.1016/j.addbeh.2012.06.010. [DOI] [PubMed] [Google Scholar]
- Lowman C, Allen J, Stout RL The Relapse Research Group. Replication and extension of Marlatt’s taxonomy of relapse precipitants: Overview of procedures and results. Addiction. 1996;91(Supplement):51–71. [PubMed] [Google Scholar]
- Ludwig F, Tadayon-Manssuri E, Strik W, Moggi F. Self-efficacy as a predictor of outcome after residential treatment programs for alcohol dependence: Simply ask the patient one question! Alcoholism: Clinical and Experimental Research. 2013;37:663–667. doi: 10.1111/acer.12007. [DOI] [PubMed] [Google Scholar]
- Marlatt GA, Gordon JA. Determinants of relapse: Implications for the maintenance of behavior change. In: Davidson PO, Davidson SM, editors. Behavioral medicine: Changing health lifestyles. New York: Brunner/Mazel; 1980. pp. 410–452. [Google Scholar]
- Martin RC, Dahlen ER. The angry cognitions scale: A new inventory for assessing cognitions in anger. Journal of Rational-Emotive & Cognitive-Behavior Therapy. 2007;25:155–173. [Google Scholar]
- McCloskey MS, Noblett KL, Deffenbacher JL, Gollan JK, Coccaro EF. Cognitive-behavioral therapy for intermittent explosive disorder: A pilot randomized clinical trial. Journal of Consulting and Clinical Psychology. 2008;76:876–886. doi: 10.1037/0022-006X.76.5.876. [DOI] [PubMed] [Google Scholar]
- McHugh RK, Kaufman JS, Frost KH, Fitzmaurice GM, Weiss RD. Positive affect and stress reactivity in alcohol-dependent outpatients. Journal of Studies on Alcohol and Drugs. 2013;74:152–157. doi: 10.15288/jsad.2013.74.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKay JR, Maisto SA, O’Farrell TJ. Alcoholics’ perceptions of factors in the onset and termination of relapses and the maintenance of abstinence: Results from a 30-month follow-up. Psychology of Addictive Behaviors. 1996;10:167–180. [Google Scholar]
- Miller CA, Parrott DJ, Giancola PR. Agreeableness and alcohol-related aggression: The mediating effect of trait aggressivity. Experimental and Clinical Psychopharmacology. 2009;17:445–455. doi: 10.1037/a0017727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, Tonigan S, Longabaugh R. The Drinker Inventory of Consequences (DrInC): An instrument for assessing adverse consequences of alcohol abuse. Vol. 4. Washington DC: Government Printing Office; 1995. NIAAA Project MATCH Monograph Series. [Google Scholar]
- Morrison PM, Noel NE, Ogle RL. Do angry women choose alcohol? Addictive Behaviors. 2012;37:908–913. doi: 10.1016/j.addbeh.2012.03.018. [DOI] [PubMed] [Google Scholar]
- Novaco RW. Treatment of chronic anger through cognitive and relaxation controls. Journal of Consulting and Clinical Psychology. 1976;44:681. doi: 10.1037//0022-006x.44.4.681. [DOI] [PubMed] [Google Scholar]
- Novaco RW. Stress Inoculation Therapy for Anger Control: A Manual for Therapists. University of California; Irvine: 1983. Unpublished manuscript. [Google Scholar]
- Nowinski J, Baker S, Carroll K. Twelve Step Facilitation Therapy Manual: A Clinical Research Guide for Therapists Treating Individuals with Alcohol Abuse and Dependence. National Institute on Alcohol Abuse and Alcoholism; Rockville, Maryland: 1999. http://pubs.niaaa.nih.gov/publications/ProjectMatch/match01.pdf. [Google Scholar]
- O’Farrell TJ, Fals-Stewart W, Murphy M, Murphy CM. Partner violence before and after individually based alcoholism treatment for male alcoholic patients. Journal of Consulting and Clinical Psychology. 2003;71:92–102. doi: 10.1037//0022-006x.71.1.92. [DOI] [PubMed] [Google Scholar]
- Pagano ME, White WL, Kelly JF, Stout RL, Tonigan JS. The 10-year course of Alcoholics Anonymous participation and long-term outcomes: A follow-up study of outpatient subjects in Project MATCH. Substance Abuse. 2013;34:51–59. doi: 10.1080/08897077.2012.691450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parrott DJ, Peterson JL, Bakeman R. Determinants of aggression toward sexual minorities in a community sample. Psychology of Violence. 2011;1:41–52. doi: 10.1037/a0021581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Project MATCH Research Group. Matching alcoholism treatments to client heterogeneity: Project MATCH three-year drinking outcomes. Alcoholism: Clinical and Experimental Research. 1998;22:1300–1311. doi: 10.1111/j.1530-0277.1998.tb03912.x. [DOI] [PubMed] [Google Scholar]
- Rabinovitz S. Drowning your sorrows? Social exclusion and anger effects on alcohol drinking. Addiction Research and Theory. 2014;22:363–370. [Google Scholar]
- Reilly PM, Shopshire MS. Anger management group treatment for cocaine dependence: Preliminary outcomes. American Journal of Drug and Alcohol Abuse. 2000;26:161–177. doi: 10.1081/ada-100100598. [DOI] [PubMed] [Google Scholar]
- Rothman EF, Cheng DM, Pedley A, Samet JH, Palfai T, Liebschutz JM, Saitz R. Interpersonal violence exposure and alcohol treatment utilization among medical inpatients with alcohol dependence. Journal of Substance Abuse Treatment. 2008;34:464–470. doi: 10.1016/j.jsat.2007.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sher KJ, Levenson RW. Risk for alcoholism and individual differences in the stress-response-dampening effect of alcohol. Journal of Abnormal Psychology. 1982;91:350–367. doi: 10.1037//0021-843x.91.5.350. [DOI] [PubMed] [Google Scholar]
- Sklar SM, Annis HM, Turner NE. Development and validation of the drug-taking confidence questionnaire: A measure of coping self-efficacy. Addictive Behaviors. 1997;22:655–670. doi: 10.1016/s0306-4603(97)00006-3. [DOI] [PubMed] [Google Scholar]
- Sloan MM. Controlling anger and happiness at work: An examination of gender differences. Gender, Work and Organization. 2012;19:370–398. [Google Scholar]
- Small M, Lewis S. Changes in hostility in residents undergoing treatment for drug and/or alcohol misuse in a residential rehabilitation centre. Therapeutic Communities. 2004;25:219–235. [Google Scholar]
- Sobell LC, Sobell MB. Timeline follow-back: A technique for assessing self-reported ethanol consumption. In: Allen J, Litten R, editors. Techniques to assess alcohol consumption. New Jersey: Humana Press; 1992. pp. 41–72. [Google Scholar]
- Spielberger CD. State-Trait Anger Expression Inventory-2: Professional Manual. Odessa: Psychological Assessment Resources, Inc; 1999. [Google Scholar]
- Stout RL, Longabaugh R, Rubin A. Predictive validity of Marlatt’s relapse taxonomy versus a more general relapse code. Addiction. 1996;91(Supplement):S99–S110. [PubMed] [Google Scholar]
- Stout RL, Wirtz P, Carbonari JP, Del Boca FK. Ensuring balanced distribution of prognostic factors in treatment outcome research. Journal of Studies on Alcohol. 1994;12:70–75. doi: 10.15288/jsas.1994.s12.70. [DOI] [PubMed] [Google Scholar]
- Thomas BS. Direct and indirect effects of selected risk factors in producing adverse consequences of drug use. Substance Use & Misuse. 1997;32:377–398. doi: 10.3109/10826089709039360. [DOI] [PubMed] [Google Scholar]
- Tonigan JS, Connors GJ, Miller WR. Alcoholics Anonymous Involvement (AAI) scale: Reliability and norms. Psychology of Addictive Behaviors. 1996;10:75–80. [Google Scholar]
- Walitzer KS, Dearing RL. Gender differences in alcohol and substance use relapse. Clinical Psychology Review. 2006;26:128–148. doi: 10.1016/j.cpr.2005.11.003. [DOI] [PubMed] [Google Scholar]
- Walitzer KS, Dermen KH, Barrick C. Facilitating involvement in Alcoholics Anonymous during out-patient treatment: A randomized clinical trial. Addiction. 2009;104:391–401. doi: 10.1111/j.1360-0443.2008.02467.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker JS, Bright JA. Cognitive therapy for violence: Reaching the parts that anger management doesn’t reach. The Journal of Forensic Psychiatry & Psychology. 2009;20:174–201. [Google Scholar]
- Wallace BC. Psychological and environmental determinants of relapse in crack cocaine smokers. Journal of Substance Abuse Treatment. 1989;6:95–106. doi: 10.1016/0740-5472(89)90036-6. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA. Manual for the Positive and Negative Affect Schedule (Expanded Form) University of Iowa; 1994. [Google Scholar]
- Witkiewitz K. Predictors of heavy drinking during and following treatment. Psychology of Addictive Behaviors. 2011;25:426–438. doi: 10.1037/a0022889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K. Temptation to drink as a predictor of drinking outcomes following psychosocial treatment for alcohol dependence. Alcoholism: Clinical and Experimental Research. 2013;37:529–537. doi: 10.1111/j.1530-0277.2012.01950.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Donovan DM, Hartzler B. Drink refusal training as part of a combined behavioral intervention: Effectiveness and mechanisms of change. Journal of Consulting and Clinical Psychology. 2012;80:440–449. doi: 10.1037/a0026996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Marlatt GA. Relapse prevention for alcohol and drug problems: That was Zen, this is Tao. American Psychologist. 2004;59:224–235. doi: 10.1037/0003-066X.59.4.224. [DOI] [PubMed] [Google Scholar]
- Witkiewitz K, Villarroel NA. Dynamic association between negative affect and alcohol lapses following alcohol treatment. Journal of Consulting and Clinical Psychology. 2009;77:633–644. doi: 10.1037/a0015647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young R, Mc D, Connor JP, Feeney GFX. Alcohol expectancy changes over a 12-week cognitive-behavioral therapy program are predictive of treatment success. Journal of Substance Abuse Treatment. 2011;40:18–25. doi: 10.1016/j.jsat.2010.08.003. [DOI] [PubMed] [Google Scholar]
- Zywiak WH, Connors GJ, Maisto SA, Westerberg VS. Relapse research and the reasons for drinking questionnaire: A factor analysis of Marlatt’s relapse taxonomy. Addiction. 1996;91(Supplement):S121–S130. [PubMed] [Google Scholar]