Abstract
Study Objective:
Insomnia is a frequent complaint in breast cancer patients during and after treatment. Breast cancer survivors, 1–10 years posttreatment, underwent in-lab polysomnography (PSG) to objectively define the insomnia in those patients with such a complaint.
Methods:
Twenty-six breast cancer survivors (aged 39–80, mean 54.0 months posttreatment) spent 2 nights in the sleep laboratory. Sleep on Night 2 was scored for sleep stages, sleep onset latency, REM sleep onset latency, wake time, apneas and hypopneas, periodic limb movements and arousals. Subjects were allocated into 2 groups by their scores on the Pittsburgh Sleep Quality Index (PSQI): no/ mild sleep disturbance (PSQI score ≤ 9, n = 15) or moderate/ severe sleep disturbance (PSQI ≥ 10, n = 11).
Results:
Standard PSG/EEG parameters failed to differentiate insomniacs from non-insomniacs. The single variable that distinguished the insomnia group was periodic limb movements in sleep (PLMS). PLMS were significantly correlated (r ≅ 0.7, p < 0.02) with subjective report of insomnia on PSQI and insomnia severity index. Log[Number of PLMS] was higher in the moderate/severe insomnia group (p = 0.008). Five of 11 patients in the moderate/severe insomnia group had a PLMS index ≥ 15, compared to only one of 15 patients in the none/mild insomnia group (p = 0.02). Menopausal symptoms and use of caffeine, hypnotics, and antidepressants were unrelated to insomnia severity or PLMS.
Conclusions:
PLMS was the sole PSG variable that separated breast cancer survivors with moderate/severe insomnia from those with no/mild sleep disturbance. Further study of the incidence and significance of PLMS in breast cancer survivors with the complaint of insomnia is merited.
Citation:
Reinsel RA, Starr TD, O'Sullivan B, Passik SD, Kavey NB. Polysomnographic study of sleep in survivors of breast cancer. J Clin Sleep Med 2015;11(12):1361–1370.
Keywords: sleep, insomnia, breast cancer, cancer survivors, periodic limb movements in sleep
Insomnia and fatigue are frequent complaints in breast cancer patients, as in patients with other chronic illnesses.1,2 Several authors have noted that this problem has been underdiagnosed and undertreated in cancer patients.3,4 Insomnia appears to be particularly prevalent in women with breast cancer, where a symptom cluster of sleep problems, fatigue, and depressive symptoms has been identified.5
The multiple reasons why cancer and acute cancer treatments may disrupt patients' sleep include cancer itself, and the physiological and psychological effects of treatments by surgery, radiation and chemotherapy, opioid analgesics, and antiemetic medications.6,7 These treatment modalities may disrupt circa-dian rhythms, thereby affecting the sleep/wake cycle, as well as endocrine and immunologic processes.8–10 Spiegel underscores the fact that circadian rhythm disruption is associated with poor sleep and decreased quality of life in cancer patients.11
Many studies which have employed self-report measures have been able to garner large sample sizes with the use of survey methodology.1,12,13 Most studies reporting objective measures of sleep have employed actigraphy, which is convenient for the participants and cost-effective. Polysomnography can be cumbersome and expensive, but it has the advantages of distinguishing resting wakefulness from sleep and providing detailed measures of sleep parameters. Despite the potential value of PSG data, we found only three published studies using PSG to evaluate sleep in breast cancer patients.14–16
BRIEF SUMMARY
Current Knowledge/Study Rationale: Insomnia is a frequent complaint in breast cancer patients during and after treatment. Very few studies have looked at sleep in breast cancer survivors after the completion of treatment.
Study Impact: Periodic leg movements during sleep (PLMS) was the sole PSG variable that separated breast cancer survivors with moderate/severe insomnia from those with no/mild sleep disturbance. Further study of the incidence and significance of PLMS in breast cancer survivors with the complaint of insomnia is merited.
Parker and coworkers, using ambulatory PSG to study subjects with advanced cancer in the intervals between chemotherapy treatments, found decreased total sleep time, low sleep efficiency, near absence of slow wave sleep, and frequent arousals and awakenings.16 That these effects may persist after the end of cancer therapy was shown by Savard and colleagues who studied breast cancer patients 2–3 years posttreatment and reported decreased sleep efficiency and elevated awake time.15 Silberfarb et al. found the reported poor sleep of a mixed group breast cancer patients and survivors to be similar to the sleep of normal volunteers.14 However, 9 of the 15 (60%) breast cancer patients had a PLMS index > 15, approximately double that of age- and sex-matched cancer-free subjects.
Those studies reporting objective sleep measures in cancer patients have tended to focus on the period prior to commencement of therapy17–19 or during active treatment with chemotherapy and/or radiation.8,16,20,21 Very few studies have looked at sleep in breast cancer survivors after the completion of treatment.14,15 Our study falls in this latter group. This report is of PSG studies that were done on a subset of 26 women involved in a larger survey of 200 breast cancer survivors, which was conducted at Memorial Sloan Kettering Cancer Center (MSKCC) and which will be the subject of a separate report. We focus here on the objective sleep characteristics measured by PSG in these 26 survivors of breast cancer who spent two nights in a sleep laboratory between one and ten years after the end of cancer treatment.
METHODS
Participants
Participants for this study were selected from the total population of 231 patients in a larger questionnaire study addressing the prevalence of sleep problems and resultant consequences in breast cancer survivors (Lowery-Allison et al., unpublished data). Two hundred of the 231 women enrolled returned their questionnaire packets. Candidates for the questionnaire study and the PSG study were women over the age of 18 with a diagnosis of Stage I, II, or III breast cancer, who had completed treatment for breast cancer at least one year, but not more than 10 years, previously. Patients were recruited either by letter with a follow-up phone call from the research staff to introduce the study, or in person at a follow-up visit to an MSKCC out-patient clinic. Patients were approached by a research study assistant with a verbal description of the study. Those who signed the consent form (or provided verbal consent if recruited by phone) were asked to fill out several questionnaires. Participants who consented for the questionnaire study were also invited to participate in the PSG portion of the study. Women who agreed to participate were scheduled for a 2-night sleep study at the Rockefeller University Hospital Sleep Laboratory. Women with a history of use of hypnotics or antidepressants were allowed in the study, as those medications are part of the clinical reality of insomnia in this patient group. Women taking hypnotics were asked to abstain from these medications for 3–5 days prior to the sleep study; compliance was checked by the nurse admitting them to the Rockefeller University Hospital Sleep Laboratory. Women who were unable or unwilling to avoid alcohol, caffeine, or cigarette consumption after 3 p.m. on the day of the sleep study were excluded from participation. Only English-speaking women were included in this study due to the many questionnaires utilized, which have not been validated in other languages.
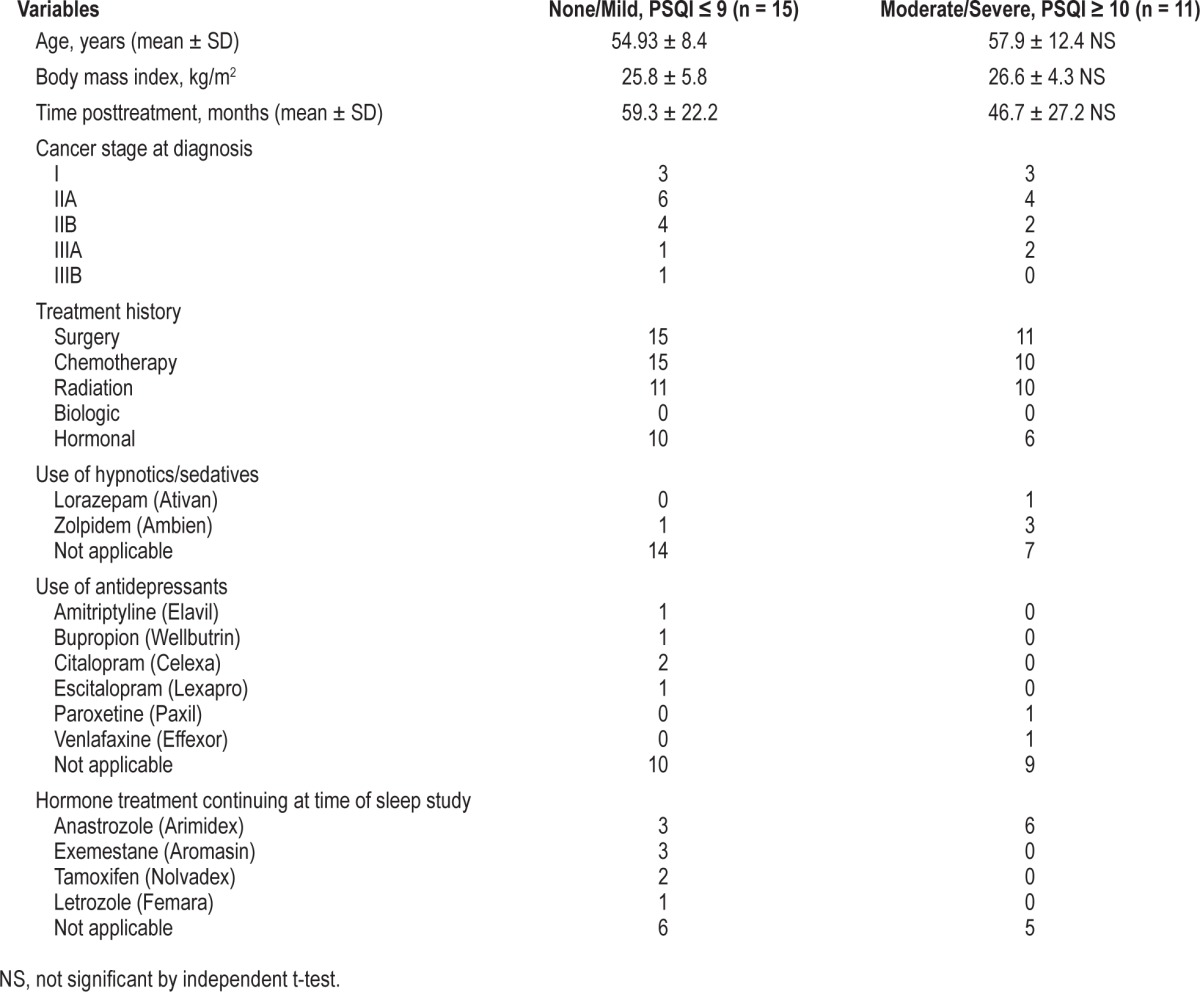
Twenty-seven patients were recruited for the study; one woman did not participate in the sleep lab portion due to scheduling difficulties. Ultimately, 26 women completed the sleep laboratory studies between September 2007 and October 2009. Demographics (age, socioeconomic status) and medical history were obtained from patient self-report supplemented by chart review for medical data (site and stage of disease, Eastern Cooperative Oncology Group (ECOG) score, medications, and prior oncologic treatments), as shown in Table 1. Patients ranged in age from 39 to 80 years, with a median age of 54 and a mean (± SD) of 56.2 ± 10.1 years. Average body mass index was 26.15 ± 5.04 (range 20.0 to 36.0).
Table 1.
Participant information and medical history including cancer treatment and time since end of treatment.
Cancer History
At the time of recruitment, study participants were a mean of 54.0 ± 4.9 months posttreatment, with the longest survivor being 119 months posttreatment. All women in the none/mild insomnia group were disease free at the time of the study, and so were 10/11 (90.9%) of the patients in the moderate/severe insomnia group. In the latter group, one woman was classified with stable disease (Stage IIA). The number of women who had early stage (Stage I) versus locally advanced disease (Stages II and III) at the time of diagnosis was similar in the 2 groups (Table 1). All patients were treated with surgery followed, in all but one case, by chemotherapy. In the moderate/severe insomnia group, 10/11 (90.9%) of the patients received radiation while slightly fewer (11/15, 73.3%) of the patients in the none/mild insomnia group were given radiation treatment; this difference is not significant. Biologic therapy was not administered to any patient in our sample, but hormonal therapy was given to the majority of patients in each group (Table 1). At the time of this study, 9/15 (60.0%) patients in the none/mild insomnia group and 6/11 (54.5%) patients in the moderate/severe group were still continuing with hormonal treatment, most commonly anastrozole (Arimidex), which was taken by 9 patients.
Measures
Pittsburgh Sleep Quality Index (PSQI)
The PSQI is a widely used and highly respected 24-item questionnaire about the patient's sleep habits and characteristics.22 Sleep disturbance is described by 7 components including onset latency, sleep duration, sleep disturbance, sleep efficiency and overall sleep quality, daytime dysfunction, and use of sleep medications. A global score which ranges from 0 to 21 is also calculated. As every point results from a subjective sleep complaint, higher scores indicate worse sleep quality. The PSQI has good reliability and validity and has been widely used in general medical and psychiatric studies. Its use in oncology has been mainly for studies of the effect of active chemotherapy or radiation treatment on sleep.21,23 A global score < 5 is consistent with good sleep, while a global score ≥ 5 indicates some degree of insomnia. A cutoff score > 6 has been suggested for increased specificity in identifying primary insomnia.24 For cancer patients, a cutoff score of 8 has been suggested.25 A higher cutoff score of 10 has been recommended for identification of clinically significant insomnia26 and for evaluation of sleep problems in women with ovarian cancer.27
Insomnia Severity Index (ISI)
The ISI is a 7-item questionnaire which assesses the perceived severity of insomnia over the last 2 weeks.28 Questions address difficulty falling asleep, maintaining sleep and the frequency of early morning awakenings, as well as the degree of dissatisfaction with current sleep. A clinical cutoff score of 8 gives maximal sensitivity and specificity for the detection of sleep difficulties. The ISI has been successfully used to screen for insomnia in breast cancer patients.15,29
Epworth Sleepiness Scale (ESS)
The ESS is a simple self-report scale used to assess daytime sleepiness.30 The scale asks the respondent to rate the probability of falling asleep in a variety of situations such as while reading, watching TV, sitting inactive in a public place, or while riding in a car. A 4-point rating scale is used ranging from 0 (no chance of dozing) to 3 (high chance of dozing). The ESS has been widely used in a variety of studies with normal sleepers and sleep disorders patients,31 and shift-workers with disrupted sleep schedules.32
The Postmenopausal Estrogen/Progestin Intervention (PEPI) Symptom Checklist
The PEPI Symptom Checklist33 is a self-report measure of menopausal symptoms consisting of 47 items measuring physical and psychological complaints. It has been used in several large-scale clinical trials, notably the Postmenopausal Estrogen/Progestin Interventions Trial and the national Women's Health Initiative.
Procedures
Sleep Laboratory
The sleep laboratory study comprised 2 consecutive nights per patient, and occurred within 30 days of completion of the questionnaire packet. On both nights, participants arrived at the sleep laboratory by 21:00 and had medical information taken (e.g. height, weight, current medications, allergies). Electrodes were placed (see below), and patients were generally in bed by 23:00. They were allowed to read or watch TV in bed until they fell asleep. Patients were awakened by 07:00. To control for first-night laboratory effects, Night 1 was used as an adaptation night; data were recorded but not scored. The data reported here are from Night 2.
EEG Recording and Polysomnography
Data were gathered using Grass amplifiers and Stellate Harmonie software (Natus Medical Inc., San Carlos CA, USA) (www.natus.com). All electrophysiological parameters were recorded using silver chloride disk electrodes filled with conductive gel. The international 10–20 system was utilized for electrode placement. As this study was designed before the new American Academy of Sleep Medicine (AASM) electrode placements were adopted, the older standard recording montage was followed: 2 central and occipital electroencephalogram (EEG) channels (C3/C4 and O1/O2), 2 horizontal electrooculogram (EOG) channels—left and right outer canthus (LOC/ROC), one bipolar submental electromyogram (EMG) channel, and an anterior tibialis bilateral EMG placement. EEG and EOG electrodes were referenced to linked mastoid placements. In addition to this standard electrode montage, sensors were placed to measure respiratory effort (thoraco-abdominal strain gauges), respiratory airflow (nasal/oral thermistors), and oxygen saturation of the blood via a finger pulse oximeter. The acquired sleep data was used to obtain several sleep variables in order to characterize sleep and sleep pathology. Scoring was performed according to AASM standards34 by a registered PSG technologist using Stellate Harmonie software.
Group Classification by Severity of Insomnia
Patients were divided into 2 groups of approximately equal size based on PSQI scores. Using the conventional cutoff score of PSQI > 5, we found 6 subjects in the “good sleepers” group and 20 subjects with PSQI scores ≥ 6, indicative of sleep problems. These unequal group sizes are not appropriate for t-test analysis. We elected to divide the sample at the mean (9.46), thus in effect using a cutoff score of 10 to separate good sleepers or those with mild insomnia from those with more severe insomnia or numerous insomnia complaints. Using that cutoff left us with 2 approximately equal size groups. Patients with PSQI scores ≤ 9 (n = 15) were considered to have no insomnia or mild insomnia, whereas PSQI scores ≥ 10 (n = 11) were taken to indicate moderate to severe insomnia. This cutoff score is consistent with recommendations for identification of clinically significant insomnia26 and for evaluation of sleep problems in women with ovarian cancer.27
Data Analysis
Categorical variables are reported as frequencies or percentages, and were analyzed with χ2 tests. Continuous variables are reported as mean ± standard deviation, unless otherwise noted, and compared by t-test for independent groups or non-parametric Mann-Whitney U test. All statistical analyses were conducted using IBM SPSS Statistics v. 21.0. Data that were extremely skewed (e.g., count of PLMS) were log-transformed using log base e. For statistical tests, p < 0.05 is taken as significant. For t-tests between independent groups, Levene's test for equality of variances was performed; in the case of unequal variances the corrected p value is reported.
RESULTS
Patient Groups
A PSQI cutoff score of 10, as suggested by other investigators,26,27 gave us 2 patient groups of near equal size: 15 patients with none/mild insomnia and 11 patients with moderate/severe insomnia. Table 1 gives the patient characteristics in the none/ mild and moderate/severe insomnia groups. The 2 groups did not differ in age, BMI, or time posttreatment. Cancer stage at diagnosis and treatment history were similar between the 2 groups.
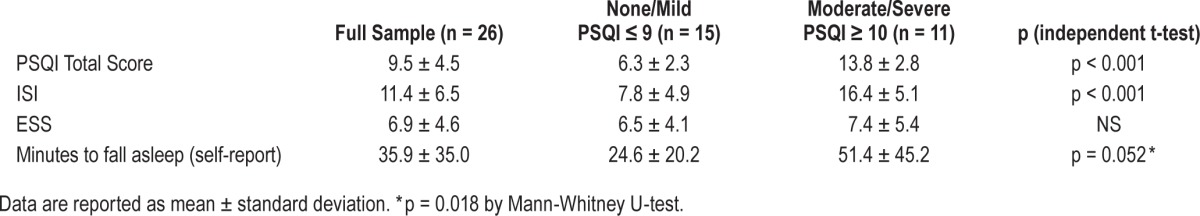
Self-Report of Insomnia
By self-report, the moderate/severe insomnia group took twice as long to fall asleep (51.4 ± 45.2 min) as the none/mild insomnia patients (24.6 ± 20.2 min, p = 0.018 by Mann-Whitney U Test). The distribution of scores on the PSQI for our patient sample is shown in Figure 1. As expected, the PSQI scores differed between groups, since this variable was used to define group membership as none/mild versus moderate/severe insomnia (Table 2). The significant difference in scores on the ISI (p < 0.001) between these 2 groups lends convergent validity to this group classification. The correlation between PSQI and ISI scores was positive (Pearson r = 0.620, p = 0.001). However reports of daytime sleepiness on the ESS did not differ between groups. Both PSQI and ISI scores had low and nonsignificant correlations with age (Pearson r < 0.18).
Figure 1. Histogram of PSQI scores.
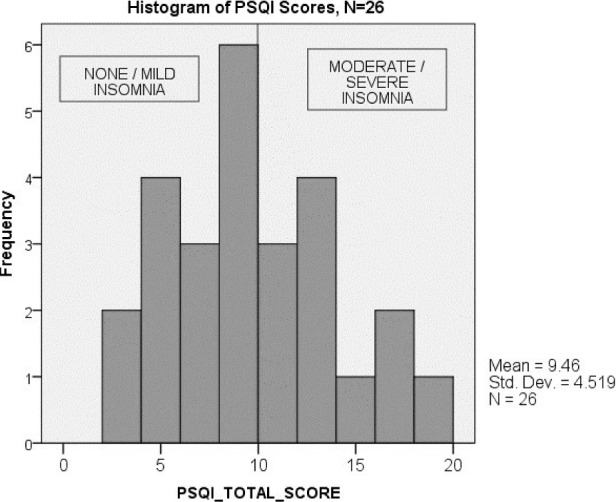
Histogram of PSQI scores for the full sample of 26 patients, showing the division of patients into two groups by severity of insomnia using a cutoff score of 10 on the PSQI.
Table 2.
Total sample: patients' self-report of insomnia.
Behaviors and Medications Affecting Sleep
Use of tobacco, caffeine, and alcohol was similar in the 2 patient groups. Only one patient currently smoked, though 10 of our 26 patients were former smokers. Caffeine use was frequent, as was moderate intake of wine or beer. Patients were required to abstain from caffeine-containing beverages after 3 pm on study nights. Compliance was verified by the sleep technician based on pre-sleep questionnaire reports.
Five patients reported current use of prescription medications for sleep at the time of the PSG study, notably zolpidem (n = 4) and lorazepam (n = 1). Only 2 patients reported taking over-the-counter sleep aids. Current hypnotic use was more prevalent in the moderate/severe group (4/11, 36.4%) than the none/mild group (1/15, 6.7%) (p = 0.058). Patients were required to abstain from hypnotic medication for 3–5 days prior to the sleep study.
Antidepressants were currently being taken by 6 women. The majority of antidepressants used were selective serotonin reuptake inhibitors (n = 4: citalopram, escitalopram, and paroxetine), with one serotonin/norepinephrine reuptake inhibitor (venlafaxine), one tricyclic antidepressant (amitriptyline, n = 1) and one patient using bupropion as an add-on to escitalopram. Patients were not required to abstain from their antidepressant medication for purposes of the PSG study.
Hormone Therapy for Breast Cancer
More than half of the women in each group were still taking hormonal treatment, as detailed in Table 1. Aromatase inhibitors are well-known causes of insomnia.35 Of the 13 subjects in this study who were taking aromatase inhibitors, 7 were in the no insomnia/mild insomnia group and 6 were in the moderate or severe insomnia group, so in this patient sample the aromatase inhibitors were not a significant cause of the reported insomnia. Two additional patients in the no insomnia/mild insomnia group were taking tamoxifen.
Menopause Status
The PEPI Symptom Checklist elicits self-report of menopausal symptoms.33 Nineteen patients said they had already gone through menopause. Seven patients (26.9%) had reached menopause naturally, 2 (7.7%) after hysterectomy, and 10 (38.5%) as a result of cancer treatment. One patient did not complete the questionnaire. Three women had not yet started menopause, while another 3 said they were “going through it now.” These latter 3 patients were aged 45, 48, and 56, with PEPI scores ≤ 31, and had sleep efficiency scores of 90%, 90%, and 85%, respectively. The youngest patient of the 3 was in the moderate/severe insomnia group, while the other two were in the none/mild group. Symptoms of hot flashes and night sweats did not differ between the insomnia groups. Menopausal symptoms did not significantly affect sleep efficiency (correlation of PEPI score with SE%: Pearson r = 0.082, NS). Neither did PEPI scores differ between the 2 insomnia groups, although there was a trend for the moderate/severe group to have higher PEPI scores (p < 0.10). About 90% of the patients scored below 40 on the PEPI scale. Of the 3 patients with the highest PEPI scores (score > 60), 2 were in the moderate/severe insomnia group; but none of these 3 patients were currently going through menopause.
PSG Measures
PSG measures derived from sleep recorded on Night 2 in the laboratory are given in Table 3. There were no differences between subjects reporting none/mild or moderate/severe insomnia on PSG-derived measures of total sleep time, sleep efficiency, sleep onset and REM sleep onset latency, wake after sleep onset or sleep stage (calculated as percent of total sleep time). Age was not a strong predictor of sleep efficiency (SE%). For this sample of 26 patients, the correlation of SE% with Age was r = −0.338, p = 0.091, two-tailed. Similarly, the correla -tion of SE% with months posttreatment was r = −0.306, NS for these 26 survivors.
Table 3.
Polysomnography results on Night 2 by Pittsburgh Sleep Quality Index group.
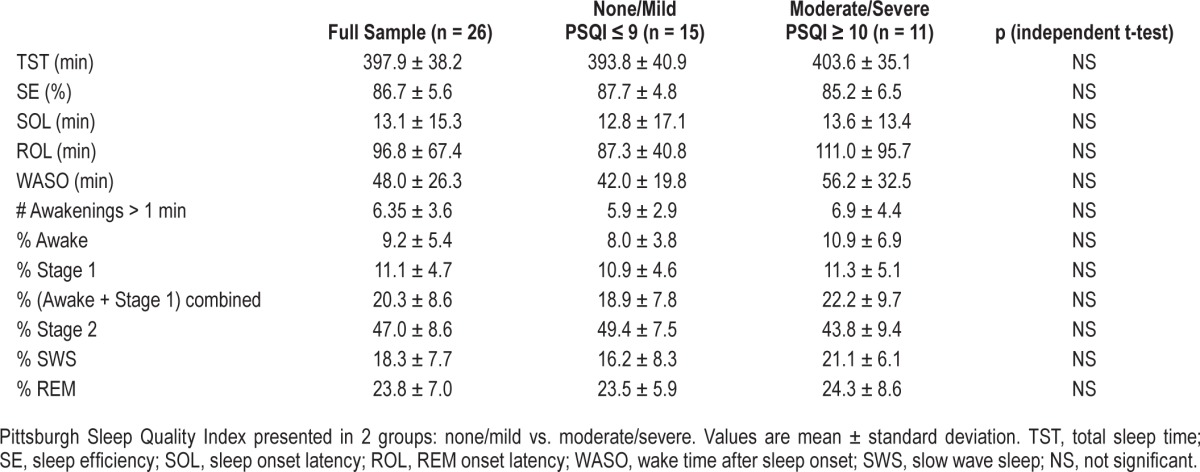
Periodic Leg Movements during Sleep (PLMS)
In this cohort (n = 26) of breast cancer survivors, PLMS were significantly associated with subjective report of insomnia. Correlations between total score on the PSQI and ISI with log[number of PLMS] were significant (PSQI: r = 0.7, p = 0.012; ISI: r = 0.68, p = 0.014). Similarly, correlations of PSQI total score with PLMS index and PLMS arousal index were significant (PLMS index r = 0.43, p = 0.027; PLMS arousal index r = 0.46, p = 0.019).
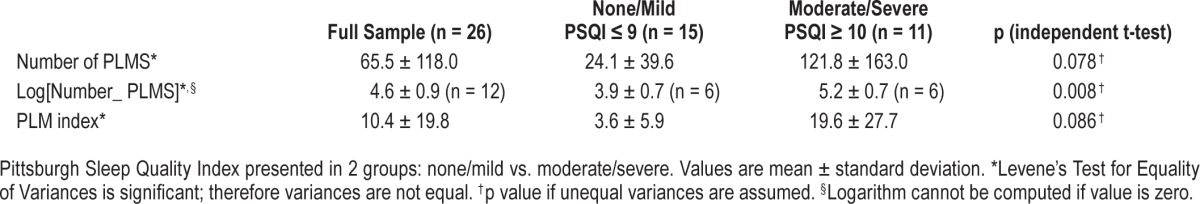
On PSG study, PLMS were dramatically higher in the group with moderate/severe insomnia (121.8 ± 163.0) than patients with less severe sleep disturbance (24.1 ± 39.6, p = 0.034 if equal variances are assumed). However the PLM count data were extremely skewed, leading to a rejection of the assumption of equal variances between groups. Log transformation of the PLM counts resulted in a highly significant difference between groups (t-test: p = 0.008 2-tailed), as shown in Table 4. Correspondingly, the PLMS index was also much increased in the more severe insomnia group (19.6 ± 27.7 compared to 3.6 ± 5.9 in the milder cases). Five of 11 patients in the moderate/severe insomnia group had a PLMS index ≥ 15, compared to only one patient in the none/mild insomnia group (p = 0.02 by χ2 test). PLMS arousal index was suggestively higher in the moderate/severe insomnia group (4.4 + 6.0) than in the patients with milder sleep disturbance (0.8 + 1.3, p = 0.031 uncorrected, p = 0.075 assuming unequal variances).
Table 4.
Periodic leg movements (PLMS) by Pittsburgh Sleep Quality Index group.
Presence of PLMS index ≥ 15 was not associated with use of caffeine. In fact, nearly all patients used caffeine. Therefore we divided the patients again based on use of more than one caffeine-containing beverage per day (i.e., number of caffeine drinks > 30/month). Four of the patients in the group with PLMS index ≥ 15 drank more than one caffeine beverage per day, compared to 2 in the low PLMS index group. This difference was not significant by χ2 analysis. Neither did the 2 PLMS groups differ with regard to current use of hypnotic medication. However, 5 of the 6 women taking antidepressants were in the group with PLMS index < 15. For all 26 subjects, the correlation of PLMS index with age was positive but only of borderline significance (Spearman rho = 0.33, p < 0.10). After removing the one patient who was age 80 and had the highest PLMS index, the correlation in the rest of the sample was non-significant (Spearman rho = 0.24, NS)
Respiratory Events
As this was a study to assess insomnia, all subjects had been screened for loud snoring during the questionnaire phase. Patients reporting a diagnosis of sleep apnea were excluded. As a result, obstructive apneas, central apneas, and hypopneas were low in number in our patient sample, with an apnea-hypopnea index < 5 in both groups. Patients who showed apneic events on PSG did not have a higher BMI than patients without apnea. Typical apnea duration was similar in the 2 groups (10–25 sec); the nadir of oxygen saturation did not differ between groups.
Arousal Indices
Arousal indices were calculated as described in the manual of the American Academy of Sleep Medicine34 and are shown in Table 5. The arousal index (AI) is a measure of total arousals per hour from all causes. The respiratory arousal index (RAI) numbers arousals related to apneas and hypopneas per hour; these were more frequent in the none/mild group (Table 5) but the difference between groups was not significant. The spontaneous arousal index (SAI) is a measure of arousals that are temporally unrelated to apneas, hypopneas and PLMs. The SAI was not different in the 2 insomnia categories. PLMS arousal index records the number of arousals that are in temporal proximity to PLMS per hour of sleep. As previously mentioned, PLMS arousal index was suggestively higher in the moderate/ severe insomnia group than in the patients with milder sleep disturbance (p = 0.075). Total arousals due to all causes did not differ between groups (see Table 5 and Figure 2).
Table 5.
Arousal indices by Pittsburgh Sleep Quality Index group.
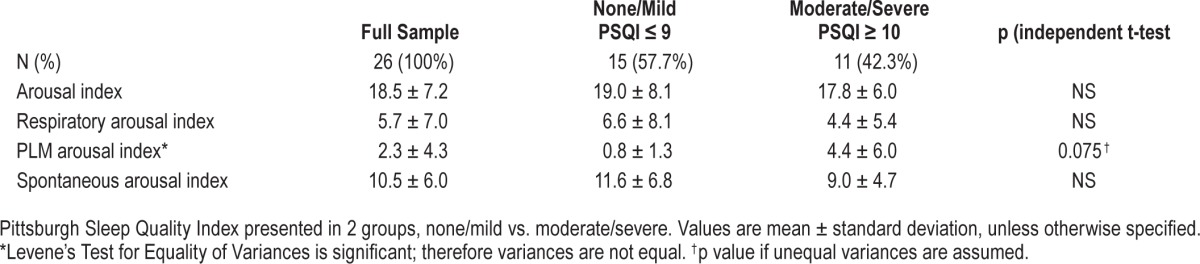
Figure 2. PLMS arousal index.
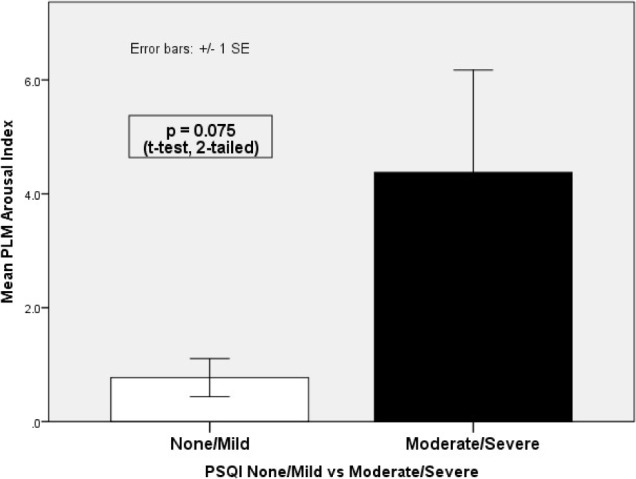
PLMS arousal index compared between patients with none/mild or moderate/severe insomnia as measured by the PSQI (using cutoff score of 10). A significant difference between groups is seen (p = 0.075 by t-test; p = 0.008 after log transformation).
DISCUSSION
The complaint of insomnia is well recognized in the clinical setting by physicians treating women who have survived breast cancer.36,37 Fiorentino and Ancoli-Israel report that between 20% and 70% of women with breast cancer have complaints of insomnia, with the problem being common both during treatment and after treatment has been completed.38 Savard and coworkers interviewed 300 women with non-metastatic breast cancer who had been treated with radiotherapy, and found that 51% of the sample met ICSD and DSM-IV criteria for insomnia.12 Fatigue and insomnia continue to be serious issues affecting quality of life of breast cancer survivors many years after the end of active treatment.39 It should not surprise us that the incidence of insomnia is high in breast cancer survivors. Insomnia increases with age, and cancer patients tend to be older than those free of cancer; insomnia increases in the post-menopausal state, and breast cancer patients are often post-menopausal at the onset or are thrown into the menopause by the treatments for the cancer. Thirdly, problems with sleep can be caused by the stress and anxiety of going through the diagnosis of breast cancer and the variety of invasive and uncomfortable treatments.
This polysomnographic study was part of a larger questionnaire study that explored the issue of insomnia and its impact on the lives of survivors of breast cancer at MSKCC. The PSG component was performed to see if we could find, in this specific group of patients, PSG changes that would help us better understand the nature of their insomnia complaint. It was understood from the start of the study that subjective complaints of insomnia are frequently not confirmed by objective PSG studies. The possible reasons for that have been discussed by others.40–43 Insomniacs may sleep better in the safe setting of a sleep laboratory. Good sleepers might find the sleep lab highly intrusive and disruptive. One or two nights in such a foreign setting may not reveal differences that occur in the regular home setting. Poor sleep habits and negative conditioning that impact an insomniac's night at home may not be in effect in the sleep lab. Finally, the physiologic differences may not reveal themselves in PSG recordings. Despite that general finding, we were hopeful that the specific population of breast cancer survivors might show objective PSG findings consistent with the severity of insomnia complaints.
In our search for visible physiological differences in our subjects, none of the standard PSG measures of sleep separated survivors with no or minor complaints about sleep from those with more severe complaints. As mentioned above, that is often the case with PSG studies; and our results are consistent with other reports of those measures failing to help us understand the basis of the complaint of insomnia.43,44 The only variable that differentiated the two groups was the presence of PLMS.
Six of our patients were currently taking antidepressants (SSRIs, an SNRI, a tricyclic antidepressant and bupropion), which can cause leg movements during sleep. Yet four of these patients were in the group with PLMS index < 15. Use of antidepressants therefore does not account for the increased incidence of PLMS in the insomnia group. The higher number of PLMS in the insomnia group was, as one might expect, associated with a higher number of arousals due to the PLMS. The difference in arousals associated with PLMS just missed reaching significance. Since the insomnia group had a higher incidence of use of hypnotics, medications which could affect arousal threshold, we considered the possibility that medication use in the insomnia group could have affected the number of PLMS associated arousals, thereby playing a role in the failure of the difference in arousals to reach significance. However, patients were required to abstain from use of hypnotics for 3 to 5 nights prior to the sleep study, so it is unlikely that hypnotic use decreased the number of PLMS associated arousals in either group. There is also no suggestion that drug withdrawal insomnia was a factor in this study. Of six subjects who had previously used and then discontinued sleeping medication at some point in the past, five were in the none/mild insomnia group.
Menopausal status could affect the sleep of women in the age range we studied. Savard and her group reported the disruptive effects of hot flashes on sleep in breast cancer survivors.45 However in our subjects, the vast majority had completed menopause, leaving little opportunity to discern a menopausal effect. Menopausal status was not a significant factor in determining whether subjects fell into the no/mild insomnia group or moderate/severe group. Furthermore, symptoms of hot flashes and night sweats and the overall PEPI score did not differ significantly in the two groups. Menopausal status was also unrelated to incidence of PLMS.
Prior studies have shown that PSG differences may not be evident when one uses the PSQI index to separate good and bad sleepers.46 The ISI might also fail to coordinate with PSG findings.15 While the PSQI is very successful in separating out those subjects who report no problem with sleep from those with complaints of insomnia, the index is not predictive of PSG abnormalities or findings one would think of as associated with insomnia or poor sleep.47 The PSQI is, however, a very useful tool for collecting reports of sleep habits and problems and, with a sum score, allows for comparing groups of patients. A score of 5 is the standard cutoff that separates good from poor sleepers, although it has been suggested that a higher cutoff score is more suitable in cancer patients.25 A cutoff score of 10 on the PSQI has been recommended for identification of clinically significant sleep problems.26 This cutoff score of 10 has been used to evaluate sleep problems in populations with ovarian cancer27 and temporomandibular joint pain.48 We selected a cutoff score of 10 for two additional reasons. First, we wished to divide our subjects into groups which combined good sleepers and those with mild insomnia, for comparison to poor sleepers and those with at least a moderate insomnia. Second, the cutoff score of 10 reflects the use of the mean to divide our subjects into two almost equal-sized groups, which was important for the validity of the statistical tests.
In designing this study, we chose to use the PSQI to group patients for comparison rather than the ISI. While the ISI is arguably a more specific measure for insomnia severity, the PSQI has the additional advantage of including an assessment of other causes of disordered sleep, such as pain, nocturia, bad dreams, confusional awakenings, and PLMS. Therefore we felt that the PSQI would be potentially the more informative measure. The ISI confirmed that our population of subjective insomniacs gave consistent reports on these two different measures (see Table 2). In our patient sample, 11 of 26 patients (42.3%) scored above 10 on the PSQI, consistent with moderate/ severe insomnia. Sleeping medication use was more prevalent in this group, consistent with their having difficulties with sleep. Often, a history of poor sleep is not associated with an increase in daytime sleepiness as measured by the Epworth Sleepiness Scale,49 and that was the case with our patient sample.
Several studies have shown that cancer and/or chemotherapy may disrupt circadian rhythms, including the sleep/wake cycle.8,11,16,17 The duration of this effect is presently unknown. However our patients were a considerable time (one to ten years) after the end of treatment. It is not known if cancer treatment has effects on sleep so long after the end of treatment. One might expect sleep to improve with increasing time after the end of treatment, but this was not the case. The correlation of sleep efficiency with time posttreatment was weak but negative, indicating worse sleep as time increased. This correlation was largely driven by the effect of increasing age, especially by one outlier with age 80. Removing this one patient reduced the correlation of time posttreatment with both age and sleep efficiency to near zero.
Subjective complaints of insomnia may correlate with defined physiological causes, such as apnea and periodic leg movements during sleep. Liu and Ancoli-Israel cite a study from their laboratory showing that 48% of breast cancer patients had AHI ≥ 5 per hour of sleep, which is higher than in same-age women without cancer.50 Apneas were not a common occurrence in our patient sample, since we screened out subjects with loud, irregular snoring. With an apnea-hypopnea index of 5 or below considered in the normal range, neither of our groups demonstrated significant apnea. Consistent with the rarity of apneas, desaturations were minimal with nadirs of 88.4% and 91.9% in the no insomnia/insomnia groups, respectively. If a breast cancer survivor is a snorer or has a history of irregular breathing, then an assessment for apnea would be necessary, but this data suggests that in a random sample of non-snoring breast cancer survivors with a complaint of poor sleep, apnea is not a common cause of the insomnia.
The significance of PLMS in the absence of restless legs syndrome or other sleep or medical disorders remains unclear despite years of study. In two studies of older individuals, Claman and colleagues found PLMS to be very common in the elderly and to be associated with what are commonly considered markers of disturbed sleep, especially when the PLMS are accompanied by an EEG arousal.51,52 Yet the elevated number of PLMS in Claman's subjects was not associated with daytime sleepiness, and there was no discussion of an association with the complaint of insomnia.
In our study with patients free of restless legs syndrome, periodic leg movements in sleep and PLMS with arousal were both statistically correlated with subjective insomnia scores on the PSQI and ISI. Also, five of the 11 subjects (45%) in the insomnia group had a PLMS index ≥ 15, compared to only one patient in the non-insomnia group. This is consistent with previous reports in this patient population. The Ancoli-Israel laboratory reported a 36% incidence of PLMS in breast cancer patients studied immediately after chemotherapy.53 Silberfarb and coworkers found PLMS in 60% of breast cancer patients, compared to 25% of insomniac controls and 22% of normal sleepers.14 One must consider the possibility that in some insomnia subjects in this patient population, PLMS are a marker of some subtle disturbance of sleep that is not discernable by the usual PSG parameters. Combined with prior studies which have reported the same finding, the statistical association in our patient cohort is strong enough to encourage further exploration into the association of PLMS and the complaint of insomnia in breast cancer survivors.
In this study, we were unable to include a control group of normal sleepers with no history of cancer for comparison to the breast cancer survivors. We did compare results from our patients to available PSG sleep values in the literature. Norms for women's sleep are sparse, especially in this older age range (39–80 years). Using the available literature, we found that our patients were quite comparable in their sleep efficiency and sleep onset latency to other groups of cancer patients14,18,54 and to samples of healthy women in a similar age range,55–57 whether recorded by laboratory PSG or by home actigraphy. Despite the fact that all of our subjects were survivors of breast cancer, and despite the fact that one might expect such patients to have worse sleep overall than women of equal age who are free of cancer, our subjects slept surprisingly similarly to healthy subjects by PSG criteria.
There are several limitations of the present study. First is the small sample size (and consequent low statistical power), which can be attributed to a low recruitment rate for the sleep lab portion of the study. However, this is perhaps not unusual. We enrolled 26 of 109 patients (24.8%) who were invited to participate in the PSG study. Parker et al. screened 1,500 cancer patients, but only 114 (7.6%) agreed to be studied in the sleep laboratory.16 The extent to which our PSG findings are representative of the larger patient population is thus difficult to assess. The findings we report here require replication in a larger patient sample. Secondly, like so many of the other studies in this area, we lack a control group of non-cancer patients. Our intent was to use the group with no perceived insomnia symptoms as an internal control, but we recruited only 6 such patients—too few for a meaningful analysis. We attempt to rectify this problem by comparing our subjects to normative reports in the literature.
CONCLUSION
The purpose of this study was to see if, with PSG studies, we could begin to define anything specific about the subjective complaint of insomnia in survivors of breast cancer. We are making no attempt to define the causes of the insomnia. PSG studies by themselves may be limited in how much they can help us better understand the insomnia of a breast cancer survivor in the clinical situation. Larger research studies may help define differences in the sleep of breast cancer survivors with and without insomnia, and an exploration of the relevance of PLMS in this population is an avenue meriting further investigation. Spectral analysis may be a helpful research addition to standard PSG studies. We will report on the spectral analysis component of this study in a separate paper.
DISCLOSURE STATEMENT
This study was supported in part by Grant # 8 UL1 TR000043 from the National Center for Research Resources and the National Center for Advancing Translational Sciences (NCATS), National Institutes of Health (NIH). Additional funding was received from The Evelyn H. Lauder Breast Center of MSKCC Medical Director's Fund and a grant from the National Sleep Research Institute, New York, NY. The authors have indicated no financial conflicts of interest. There was no off-label or investigational use involved in this research. This work was performed at The Rockefeller University Hospital, New York, NY.
ACKNOWLEDGMENTS
The authors are extremely grateful to Larry Norton, MD of MSKCC for his initiation of this project and for financial support. We thank Rebecca Q. Scott, PhD for her assistance in developing and implementing this research protocol. We express our appreciation to Pia Wigren, PhD for assistance in PSG recording in the sleep laboratory, and Allison Shockley, RPSGT for scoring the PSG sleep records. We also thank Lauren Rogak, MA and Maria Farberov, MPA from MSKCC, for administrative assistance, help with recruiting patients, and entering the questionnaire data.
ABBREVIATIONS
- AASM
American Academy of Sleep Medicine
- AHI
apnea-hypopnea index
- AI
arousal index
- BMI
body mass index
- DSM
Diagnostic and Statistical Manual of Mental Disorders
- ECOG
Eastern Cooperative Oncology Group
- EEG
electroencephalogram
- ESS
Epworth Sleepiness Scale
- ICSD
International Classification of Sleep Disorders
- ISI
Insomnia Severity Index
- MSKCC
Memorial Sloan Kettering Cancer Center
- NS
not significant
- PEPI
Postmenopausal Estrogen/Progestin Intervention
- PLM
periodic leg movements
- PLMS
periodic leg movements in sleep
- PSG
polysomnography
- PSQI
Pittsburgh Sleep Quality Index
- RAI
respiratory arousal index
- REM
rapid eye movement
- ROL
REM sleep onset latency
- SAI
spontaneous arousal index
- SD
standard deviation
- SE
sleep efficiency
- SNRI
serotonin/norepinephrine reuptake inhibitor
- SOL
sleep onset latency
- SPSS
Statistical Package for the Social Sciences
- SSRI
selective serotonin reuptake inhibitor
- SWS
slow wave sleep
- TST
total sleep time
- WASO
wake time after sleep onset
REFERENCES
- 1.Davidson JR, MacLean AW, Brundage MD, Schulze K. Sleep disturbance in cancer patients. Soc Sci Med. 2002;54:1309–21. doi: 10.1016/s0277-9536(01)00043-0. [DOI] [PubMed] [Google Scholar]
- 2.Ancoli-Israel S. The impact and prevalence of chronic insomnia and other sleep disturbances associated with chronic illness. Am J Manag Care. 2006;12:S221–9. [PubMed] [Google Scholar]
- 3.Savard J, Morin CM. Insomnia in the context of cancer: a review of a neglected problem. J Clin Oncol. 2001;19:895–908. doi: 10.1200/JCO.2001.19.3.895. [DOI] [PubMed] [Google Scholar]
- 4.Ancoli-Israel S. Recognition and treatment of sleep disturbances in cancer. J Clin Oncol. 2009;27:5864–6. doi: 10.1200/JCO.2009.24.5993. [DOI] [PubMed] [Google Scholar]
- 5.Fiorentino L, Rissling M, Liu L, Ancoli-Israel S. The symptom cluster of sleep, fatigue and depressive symptoms in breast cancer patients: severity of the problem and treatment options. Drug Discov Today Dis Models. 2011;8:167–73. doi: 10.1016/j.ddmod.2011.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Theobald DE. Cancer pain, fatigue, distress, and insomnia in cancer patients. Clin Cornerstone. 2004;6:S15–21. doi: 10.1016/s1098-3597(05)80003-1. [DOI] [PubMed] [Google Scholar]
- 7.Graci G. Pathogenesis and management of cancer-related insomnia. J Support Oncol. 2005;3:349–59. [PubMed] [Google Scholar]
- 8.Savard J, Liu L, Natarajan L, et al. Breast cancer patients have progressively impaired sleep-wake activity rhythms during chemotherapy. Sleep. 2009;32:1155–60. doi: 10.1093/sleep/32.9.1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Savard J, Simard S, Ivers H, Morin CM. Randomized study on the efficacy of cognitive-behavioral therapy for insomnia secondary to breast cancer, part II: immunologic effects. J Clin Oncol. 2005;23:6097–106. doi: 10.1200/JCO.2005.12.513. [DOI] [PubMed] [Google Scholar]
- 10.Miller AH, Ancoli-Israel S, Bower JE, Capuron L, Irwin MR. Neuroendocrine-immune mechanisms of behavioral comorbidities in patients with cancer. J Clin Oncol. 2008;26:971–82. doi: 10.1200/JCO.2007.10.7805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Spiegel D. Losing sleep over cancer. J Clin Oncol. 2008;26:2431–2. doi: 10.1200/JCO.2008.16.2008. [DOI] [PubMed] [Google Scholar]
- 12.Savard J, Simard S, Blanchet J, Ivers H, Morin CM. Prevalence, clinical characteristics, and risk factors for insomnia in the context of breast cancer. Sleep. 2001;24:583–90. doi: 10.1093/sleep/24.5.583. [DOI] [PubMed] [Google Scholar]
- 13.Palesh OG, Roscoe JA, Mustian KM, et al. Prevalence, demographics, and psychological associations of sleep disruption in patients with cancer: University of Rochester Cancer Center-Community Clinical Oncology Program. J Clin Oncol. 2010;28:292–8. doi: 10.1200/JCO.2009.22.5011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Silberfarb PM, Hauri PJ, Oxman TE, Schnurr P. Assessment of sleep in patients with lung cancer and breast cancer. J Clin Oncol. 1993;11:997–1004. doi: 10.1200/JCO.1993.11.5.997. [DOI] [PubMed] [Google Scholar]
- 15.Savard J, Simard S, Ivers H, Morin CM. Randomized study on the efficacy of cognitive-behavioral therapy for insomnia secondary to breast cancer, part I: sleep and psychological effects. J Clin Oncol. 2005;23:6083–96. doi: 10.1200/JCO.2005.09.548. [DOI] [PubMed] [Google Scholar]
- 16.Parker KP, Bliwise DL, Ribeiro M, et al. Sleep/wake patterns of individuals with advanced cancer measured by ambulatory polysomnography. J Clin Oncol. 2008;26:2464–72. doi: 10.1200/JCO.2007.12.2135. [DOI] [PubMed] [Google Scholar]
- 17.Ancoli-Israel S, Liu L, Marler MR, et al. Fatigue, sleep, and circadian rhythms prior to chemotherapy for breast cancer. Support Care Cancer. 2006;14:201–9. doi: 10.1007/s00520-005-0861-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Berger AM, Farr LA, Kuhn BR, Fischer P, Agrawal S. Values of sleep/wake, activity/rest, circadian rhythms, and fatigue prior to adjuvant breast cancer chemotherapy. J Pain Symptom Manage. 2007;33:398–409. doi: 10.1016/j.jpainsymman.2006.09.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wright CE, Schnur JB, Montgomery GH, Bovbjerg DH. Psychological factors associated with poor sleep prior to breast surgery: an exploratory study. Behav Med. 2010;36:85–91. doi: 10.1080/08964280903521305. [DOI] [PubMed] [Google Scholar]
- 20.Berger AM, VonEssen S, Khun BR, et al. Feasibilty of a sleep intervention during adjuvant breast cancer chemotherapy. Oncol Nurs Forum. 2002;29:1431–41. doi: 10.1188/02.ONF.1431-1441. [DOI] [PubMed] [Google Scholar]
- 21.Liu L, Rissling M, Natarajan L, et al. The longitudinal relationship between fatigue and sleep in breast cancer patients undergoing chemotherapy. Sleep. 2012;35:237–45. doi: 10.5665/sleep.1630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 23.Berger AM, Kuhn BR, Farr LA, et al. One-year outcomes of a behavioral therapy intervention trial on sleep quality and cancer-related fatigue. J Clin Oncol. 2009;27:6033–40. doi: 10.1200/JCO.2008.20.8306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Backhaus J, Junghanns K, Broocks A, Riemann D, Hohagen F. Test-retest reliability and validity of the Pittsburgh Sleep Quality Index in primary insomnia. J Psychosom Res. 2002;53:737–40. doi: 10.1016/s0022-3999(02)00330-6. [DOI] [PubMed] [Google Scholar]
- 25.Carpenter JS, Andrykowski MA. Psychometric evaluation of the Pittsburgh Sleep Quality Index. J Psychosom Res. 1998;45:5–13. doi: 10.1016/s0022-3999(97)00298-5. [DOI] [PubMed] [Google Scholar]
- 26.Okun ML, Kravitz HM, Sowers MF, Moul DE, Buysse DJ, Hall M. Psychometric evaluation of the Insomnia Symptom Questionnaire: a self-report measure to identify chronic insomnia. J Clin Sleep Med. 2009;5:41–51. [PMC free article] [PubMed] [Google Scholar]
- 27.Clevenger L, Schrepf A, Degeest K, et al. Sleep disturbance, distress, and quality of life in ovarian cancer patients during the first year after diagnosis. Cancer. 2013;119:3234–41. doi: 10.1002/cncr.28188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bastien CH, Vallieres A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2:297–307. doi: 10.1016/s1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- 29.Savard MH, Savard J, Simard S, Ivers H. Empirical validation of the Insomnia Severity Index in cancer patients. Psychooncology. 2005;14:429–41. doi: 10.1002/pon.860. [DOI] [PubMed] [Google Scholar]
- 30.Johns MW. A new method for measuring daytime sleepiness: the Epworth Sleepiness Scale. Sleep. 1991;14:540–5. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 31.Dauvilliers Y. Differential diagnosis in hypersomnia. Curr Neurol Neurosci Rep. 2006;6:156–62. doi: 10.1007/s11910-996-0039-2. [DOI] [PubMed] [Google Scholar]
- 32.Thorpy M. Understanding and diagnosing shift work disorder. Postgrad Med. 2011;123:96–105. doi: 10.3810/pgm.2011.09.2464. [DOI] [PubMed] [Google Scholar]
- 33.Greendale GA, Reboussin BA, Hogan P, et al. Symptom relief and side effects of postmenopausal hormones: results from the Postmenopausal Estrogen/ Progestin Interventions Trial. Obstet Gynecol. 1998;92:982–8. doi: 10.1016/s0029-7844(98)00305-6. [DOI] [PubMed] [Google Scholar]
- 34.Iber C, et al. Westchester, IL: American Academy of Sleep Medicine; 2007. for the American Academy of Sleep Medicine. The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications. [Google Scholar]
- 35.Desai K, Mao JJ, Su I, et al. Prevalence and risk factors for insomnia among breast cancer patients on aromatase inhibitors. Support Care Cancer. 2013;21:43–51. doi: 10.1007/s00520-012-1490-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Norton L. Personal Communication to Neil B. Kavey, 2007 [Google Scholar]
- 37.Bower JE. Behavioral symptoms in patients with breast cancer and survivors. J Clin Oncol. 2008;26:768–77. doi: 10.1200/JCO.2007.14.3248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fiorentino L, Ancoli-Israel S. Insomnia and its treatment in women with breast cancer. Sleep Med Rev. 2006;10:419–29. doi: 10.1016/j.smrv.2006.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kornblith AB, Herndon JE, 2nd, Weiss RB, et al. Long-term adjustment of survivors of early-stage breast carcinoma, 20 years after adjuvant chemotherapy. Cancer. 2003;98:679–89. doi: 10.1002/cncr.11531. [DOI] [PubMed] [Google Scholar]
- 40.Dorsey CM, Bootzin RR. Subjective and psychophysiologic insomnia: an examination of sleep tendency and personality. Biol Psychiatry. 1997;41:209–16. doi: 10.1016/0006-3223(95)00659-1. [DOI] [PubMed] [Google Scholar]
- 41.Rosa RR, Bonnet MH. Reported chronic insomnia is independent of poor sleep as measured by electroencephalography. Psychosom Med. 2000;62:474–82. doi: 10.1097/00006842-200007000-00004. [DOI] [PubMed] [Google Scholar]
- 42.Silva GE, Goodwin JL, Sherrill DL, et al. Relationship between reported and measured sleep times: the sleep heart health study (SHHS) J Clin Sleep Med. 2007;3:622–30. [PMC free article] [PubMed] [Google Scholar]
- 43.Littner M, Hirshkowitz M, Kramer M, et al. Practice parameters for using polysomnography to evaluate insomnia: an update. Sleep. 2003;26:754–60. doi: 10.1093/sleep/26.6.754. [DOI] [PubMed] [Google Scholar]
- 44.Edinger JD, Ulmer CS, Means MK. Sensitivity and specificity of polysomnographic criteria for defining insomnia. J Clin Sleep Med. 2013;9:481–91. doi: 10.5664/jcsm.2672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Savard J, Davidson JR, Ivers H, et al. The association between nocturnal hot flashes and sleep in breast cancer survivors. J Pain Symptom Manage. 2004;27:513–22. doi: 10.1016/j.jpainsymman.2003.10.013. [DOI] [PubMed] [Google Scholar]
- 46.Grandner MA, Kripke DF, Yoon IY, Youngstedt SD. Criterion validity of the Pittsburgh Sleep Quality Index: investigation in a non-clinical sample. Sleep Biol Rhythms. 2006;4:129–39. doi: 10.1111/j.1479-8425.2006.00207.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Buysse DJ, Hall ML, Strollo PJ, et al. Relationships between the Pittsburgh Sleep Quality Index (PSQI), Epworth Sleepiness Scale (ESS), and clinical/ polysomnographic measures in a community sample. J Clin Sleep Med. 2008;4:563–71. [PMC free article] [PubMed] [Google Scholar]
- 48.Yatani H, Studts J, Cordova M, Carlson CR, Okeson JP. Comparison of sleep quality and clinical and psychologic characteristics in patients with temporomandibular disorders. J Orofac Pain. 2002;16:221–8. [PubMed] [Google Scholar]
- 49.Lichstein KL, Wilson NM, Noe SL, Aguillard RN, et al. Daytime sleepiness in insomnia: behavioral, biological and subjective indices. Sleep. 1994;17:693–702. doi: 10.1093/sleep/17.8.693. [DOI] [PubMed] [Google Scholar]
- 50.Liu L, Ancoli-Israel S. Sleep disturbances in cancer. Psychiatr Ann. 2008;38:627–34. doi: 10.3928/00485713-20080901-01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Claman DM, Redline S, Blackwell T, et al. Prevalence and correlates of periodic limb movements in older women. J Clin Sleep Med. 2006;2:438–45. [PubMed] [Google Scholar]
- 52.Claman DM, Ewing SK, Redline S, et al. Periodic leg movements are associated with reduced sleep quality in older men: the MrOS Sleep Study. J Clin Sleep Med. 2013;9:1109–17. doi: 10.5664/jcsm.3146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Fiorentino L, Mason W, Parker B, et al. Sleep disruption in breast cancer patients post-chemotherapy. Sleep. 2005;28:A294. (Abstract Suppl) [Google Scholar]
- 54.Enderlin CA, Coleman EA, Cole C, et al. Subjective sleep quality, objective sleep characteristics, insomnia symptom severity, and daytime sleepiness in women aged 50 and older with nonmetastatic breast cancer. Oncol Nurs Forum. 2011;38:E314–25. doi: 10.1188/11.ONF.E314-E325. [DOI] [PubMed] [Google Scholar]
- 55.Webb WB. Sleep in older persons: sleep structures of 50- to 60-year-old men and women. J Gerontol. 1982;37:581–6. doi: 10.1093/geronj/37.5.581. [DOI] [PubMed] [Google Scholar]
- 56.Williams RL, Karacan I, Hursch CJ. New York: John Wiley & Sons; 1974. Electroencephalograpy (EEG) of Human Sleep: Clinical Applications. [Google Scholar]
- 57.Vitiello MV, Larsen LH, Moe KE, Borson S, Schwartz RS, Prinz PN. Objective sleep quality of healthy older men and women is differentially disrupted by nighttime periodic blood sampling via indwelling catheter. Sleep. 1996;19:304–11. doi: 10.1093/sleep/19.4.304. [DOI] [PubMed] [Google Scholar]


