Abstract
Objective:
Duration of insomnia symptoms and nightmares are related to suicidal risk in young adults independent of current symptoms of insomnia, nightmares, anxiety, depression, and PTSD. However, this relation has yet to be examined among older adults, despite older adults being at higher risk of suicidal behavior. Further, the current study aims to replicate previous research among younger adults showing that insomnia symptoms and nightmares are associated with suicide risk independent of the interpersonal psychological theory of suicide (IPTS).
Methods:
The present study utilized 167 participants age 55 and older obtained by combining two independent mTurk data collections of adults in the United States.
Results:
In the current sample, duration of nightmares was associated with suicide risk in older adults independent of symptoms of current insomnia and nightmares, duration of insomnia, and symptoms of PTSD, anhedonia, and the IPTS.
Conclusions:
Our findings suggest that the duration of nightmares (i.e., how long someone has been experiencing nightmares) predict substantial variance in suicide risk among older adults in addition to the risk factors typically examined. Thus, assessment of sleep dysfunction is important when assessing suicide risk among older adults.
Citation:
Golding S, Nadorff MR, Winer ES, Ward KC. Unpacking sleep and suicide in older adults in a combined online sample. J Clin Sleep Med 2015;11(12):1385–1392.
Keywords: nightmares, insomnia symptoms, suicide risk, sleep disturbances, older adults
Suicide is a leading cause of death, yet it remains a challenge to predict and prevent. In 2012, suicide was the tenth leading cause of death in the United States, accounting for 40,600 deaths.1 Further, 2012 marks the first time in history that U.S. deaths by suicide have exceeded 40,000 in a year.2 Suicide is a particularly large problem for older adults: although older adults only made up about 13.7% of the population in 2012, older adults represented 16.4% of suicides.1 Suicidal intent, which refers to the degree to which one desires to end his/her life by suicidal behavior,3 is more common in older adults than in the rest of the population, and attempts made by older adults are more likely to be fatal.4 To illustrate this, there are 100–200 attempts for every one youth suicide and 4 attempts for every one older adult suicide.5 Thus, older adult suicide attempts are much more likely to be fatal than younger adult suicide attempts. Research has identified many risk factors for older adult suicide including the loss of independence, social isolation, mental illness, and decline in physical health.4,6–8 However, despite having identified these risk factors, clinicians are still very poor at predicting suicide.9 Thus, more research needs to be conducted to identify risk factors that explain variance above and beyond the established risk factors in order to improve the ability to predict and prevent suicide. Two factors that have emerged as strong candidates as suicide risk factors in recent years are insomnia symptoms and nightmares.
BRIEF SUMMARY
Current Knowledge/Study Rationale: Research has shown relations between duration of insomnia symptoms/duration of nightmares and suicide risk in younger adults. However, this relation has not been examined in older adults.
Study Impact: The present study found that, in older adults, nightmare duration was related to suicide risk independent of current nightmares, current symptoms of and duration of insomnia, and symptoms of anhedonia and PTSD. Nightmare duration was also related to suicide risk independent of the IPTS. Thus, nightmare duration is an important factor to be assessed when evaluating the level of suicide risk with patients.
Insomnia Symptoms and Suicide
Many studies have found an association between insomnia symptoms and suicidal behavior in both community and clinical samples.10–17 For instance, in a sample of individuals who suffer from depression and insomnia being treated by hypnotic and selective serotonin reuptake inhibitor (SSRI) medication, insomnia is correlated with suicidal thinking, suggesting a link between insomnia and suicidal ideation in a clinical population.11 Although research has clearly demonstrated that insomnia symptoms are associated with suicidal behavior, findings regarding whether this association is independent of other psychopathology are mixed. Pigeon and colleagues found that among Veteran suicide decedents, Veterans with sleep disturbance died in closer proximity to their last visit to the Veterans Affairs (VA) than those who did not have sleep disturbance, even after statistically accounting for mental health disorders.18 Thus, sleep disturbances may relate to the level of imminence of suicidal behaviors. Similarly, insomnia symptoms were associated with suicidal ideation cross-sectionally after controlling for symptoms of depression, hopelessness, anxiety, Posttraumatic Stress Disorder (PTSD) diagnosis, and substance abuse.19 Additionally, a recent study among older adults found that poor sleep quality predicted future death by suicide after controlling for baseline depressive symptoms.15 However, other studies have found that the association between insomnia and suicide risk is mediated by other psychopathology. A recent research study found the relation between insomnia and suicidal ideation to be mediated by nightmares and dysfunctional attitudes about sleep.16 Additionally, our research team has also found relations between insomnia symptoms and suicide to be mediated by symptoms of psychopathology among young adults20 and older adults.13 However, an emerging factor that may help explain this discrepancy in the literature is insomnia duration. Our recent research has found that insomnia duration is associated with suicide risk independent of nightmare duration and current symptoms of depression, anxiety, PTSD, insomnia, and nightmares. However, research has yet to examine these relations among older adults.
Nightmares and Suicide
Nightmares are associated with suicide,10,11,13,15,21–23 and several studies among younger adults have found that nightmares are associated with suicidal ideation or suicide risk independent of symptoms of psychopathology.10,12,20,23 However, the only study we are aware of looking at nightmares and suicidal ideation among older adults found that the relation between nightmares and suicidal ideation was mediated by both insomnia symptoms and depressive symptoms.13
Nightmares have also been shown to be associated with an increased risk of suicide attempts. In a sample of 165 suicide attempters, individuals who reported frequent nightmares were over four times more likely to have at least one repeated suicide attempt at a 2-year follow-up after adjusting for the effects of depression, anxiety, PTSD, and substance use disorders.21 Similar to insomnia symptoms, recent research suggests that the sleep disorder duration, or how long one has had insomnia or nightmares, may be more important than current symptomology. As was the case with insomnia, nightmare duration was also associated with suicidal ideation independent of insomnia duration and current symptoms of insomnia, nightmares, anxiety, depression, and PTSD.14 Because sleep disturbances and nightmares are associated with depression and PTSD, it is important to examine relations between sleep disturbances and suicide while accounting for symptoms of depression (e.g., symptoms of anhedonia) and PTSD.
Examining the Theoretical Basis of the Association of Sleep and Suicide
As outlined above, a substantial amount of research in recent years has focused on trying to understand the mechanism through which sleep disorders confer suicide risk by statistically controlling for the effects of other forms of psychopathology. However, until recently, the association between sleep problems and suicide risk had never been tested within a theoretical framework. In a recent paper,12 we examined whether the interpersonal-psychological theory of suicide (IPTS), a well-known and empirically supported model of suicidal behavior,24–26 may explain the association between sleep disturbance and suicide risk. The theory consists of 3 constructs: perceived burdensomeness, thwarted belongingness, and acquired capability to enact lethal self-harm.26 The interaction of these three constructs indicated the greatest risk for suicide attempts versus suicidal ideation in a clinical sample of young adults with suicidality.27 In our study, we found that nightmares were independently associated with suicide risk and past suicide attempts in 2 independent data sets; however, our data were mixed regarding insomnia symptoms and suicide, with the IPTS mediating the relation in one sample but not the other.12 Thus, it appears that the IPTS cannot fully explain the mechanism by which nightmares confer suicide risk, but that the theory may be useful in explaining the association between insomnia symptoms and suicidal behavior.
Statement of the Problem
There are several significant gaps in the empirical literature that warrant discussion and further examination. First, there is a paucity of studies examining the theoretical basis of the association between sleep disturbance and suicidality. This is important, as understanding how sleep disturbances lead to suicidality will likely aid clinicians in detecting and treating suicide risk. A second substantial limitation is that very few studies have examined sleep and suicide in older adults despite older adults having higher rates of sleep disturbances and suicide.1,28 Older adults experience an earlier circadian sleep-wake cycle,28 decreased total sleep time, increased wakefulness after onset of sleep, decreased sleep efficiency, and less slow wave sleep.29 Because of these differences in sleep and suicidal behavior, it cannot be assumed that the relations among sleep and suicide that occur in young people will be the same in older adults. Thus, there is a need for more research examining sleep and suicide among older adults.
Present Study
Although the duration of sleep dysfunction has been examined in relation to suicidal ideation in a young adult sample,14 and some research has been conducted examining the relations between sleep and suicide in older adults,13,15,30 substantial gaps in the literature remain. Specifically, research has yet to examine the impact of sleep disturbance duration on suicide risk among older adults. Further, the association between sleep disturbances and suicide risk among older adults has yet to be examined in relation to a leading suicide theory. To address these limitations in the empirical literature, the current study will examine the specific relations among duration of insomnia and nightmares and suicide risk, including examining these relations within the IPTS framework.
In line with previous findings related to younger adults,14 we hypothesize that insomnia duration and nightmare duration will be positively associated with suicide risk independent of current levels of insomnia symptoms and nightmare severity. Our second hypothesis is that insomnia duration and nightmare duration will be positively associated with suicide risk independent of current symptoms of insomnia, nightmares, PTSD, and anhedonia. Our third hypothesis is that insomnia duration and nightmare duration will be associated with suicide risk independent of current symptoms of insomnia, nightmares, and the IPTS (i.e., thwarted belongingness, burdensomeness, acquired capability, and relevant interactions).12
METHODS
Participants
The current study consists of a sub-sample of 167 individuals aged 55 or older who were obtained through combining data from 2 larger data collections (age 18+) utilizing Amazon.com's Mechanical Turk (mTurk), an online venue on which people can participate in online opportunities for nominal payments. Sample demographics from mTurk are of equal or greater representativeness and diversity than conventional samples.31 Further, and of importance to this study, samples collected through mTurk match or exceed incidence of clinical symptoms such as depression and anxiety and exposure to trauma when compared to the levels in the general population.32 Of the 167 respondents, 124 (74.3%) were female. The sample ranged in age from 55 to 75 years (mean = 60.64, SD = 4.94). The majority (91.6%) of participants were Caucasian. Participants received nominal payment (i.e., $0.25) for completion of the study; however, some analyses regarding motivation to complete mTurk studies suggest internal motivations, such as for entertainment, for participating in online studies.31 Further, the potential to reach Mechanical Turk master status may influence mTurk participants' completion of studies. In order to work toward this status, workers are encouraged to submit Human Intelligence Tasks, or HITs, with accuracy on a breadth of subjects and from a variety of requesters; further, this status is not something a worker can request; workers' performance can distinguish them for master status.33 Thus, participants may have completed our study for low pay in hopes of reaching master status.
All participants were from the United States, with 43 states represented. Most commonly, participants were from Florida (10.2%), California (7.2%), and Tennessee (6.6%). Further, participants from all regions of the US were represented: 13.2% from the Northeast, 25.1% from the Midwest, 19.2% from the West, and 41.3% from the South; these proportions are similar to those of the United States population in 2014 (17.6% in the Northeast, 21.2% in the Midwest, 23.6% in the West, and 37.6% in the South).34 Though previous analyses have found a representative split of sex on mTurk (55% female sample),31 our study had an unrepresentative majority of females who completed the study. Our study may have self-selected a majority women because of the subject matters of suicide, insomnia, and depression.
Measures
The insomnia severity index (ISI)35 assesses severity of insomnia symptoms over the past 2 weeks. This questionnaire has 7 items with answer options that range from 0 to 4 points, for a possible maximum of 28 points.36 Scores > 15 indicate a moderate to severe level of insomnia.36 Over 3 months, the ISI has demonstrated sufficient test-retest reliability; further, the ISI has shown concurrent validity with polysomnography and patients' sleep diaries.35,36 In the current study the ISI demonstrated acceptable internal consistency (α = 0.90). Means and standard deviations for all measures, including the ISI, can be found in Table 1.
Table 1.
Descriptive statistics for primary study variables.
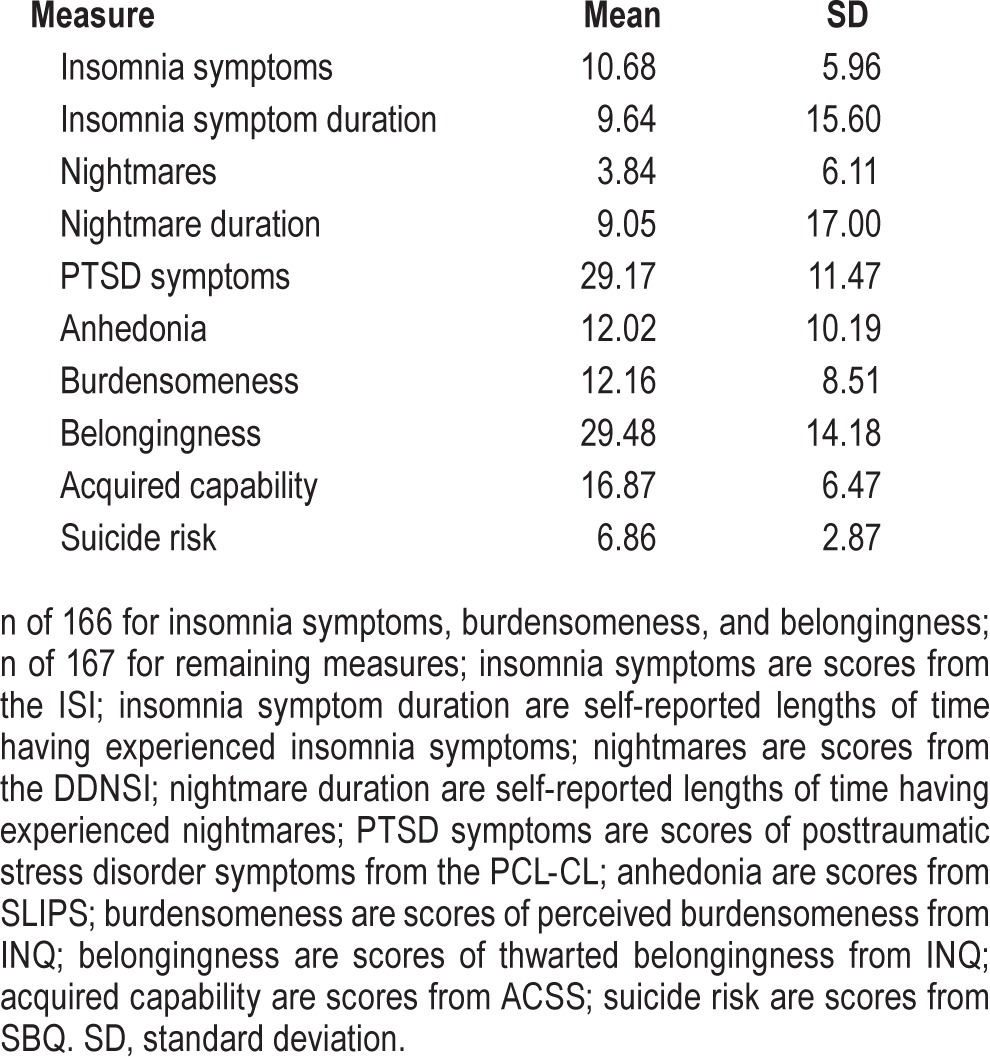
The Disturbing Dreams and Nightmares Severity Index (DDNSI) was used to assess frequency and severity of nightmares over the past year.35,36 The DDNSI assesses frequency based on the number of nights per week with nightmares and the number of nightmares participants endorse having each week (maximum of 14 nightmares).37 Likert-type scale questions further assessed nightmare severity by measuring how often individuals are awakened by nightmares and nightmare severity and intensity. Higher scores on the DDNSI reflect higher levels of current nightmare difficulties, with scores ≥ 10 indicating the possible presence of a nightmare disorder.38 In the current study the DDNSI demonstrated acceptable internal consistency (α = 0.90).
Insomnia duration was measured by asking the participants “If you have an insomnia problem, how long have you had it for (please specify months and years)?” After converting participant answers, a duration variable of total months of reported insomnia was created.14 Nightmare duration was determined by one item from the DDNSI that does not factor into the total DDNSI score. On this item, participants were asked to provide an estimation of the number of months and/or years they have been experiencing nightmares or disturbing dreams.39 Again, data were converted to reflect the total number of months of reported nightmares or disturbing dreams. These measures of duration of insomnia symptoms and nightmares have been used in a previous study evaluating sleep disturbance duration.14
The Posttraumatic Stress Disorder Checklist-Civilian Version (PCL-CL)40 was used to measure how much trouble associated with PTSD symptoms participants have experienced related to their most significant life stressor. For each of the 17 items, participants could choose from 1 (not at all) up to 5 (extremely); higher total scores on the measure are associated with greater levels of PTSD symptoms.41 The PCL-CL has shown convergent validity with a PTSD scale administered by a clinician and has demonstrated high internal consistency (α = 0.94).41 Two items from the PCL-CL (i.e., “Repeated, disturbing dreams of a stressful experience” and “Trouble falling or staying asleep”)40 were excluded from our analyses in an effort to reduce multicollinearity. In the current study the PCLCL demonstrated acceptable internal consistency (α = 0.92).
The Specific Loss of Interest and Pleasure Scale (SLIPS) assesses recent changes in symptoms of anhedonia. This measure includes 23 items with ordinal scales that allow individuals to indicate the level of change in interest in or pleasure from certain activities from 0 (no change), 1 (some decrease), 2 (marked decline), and 3 (interest/pleasure has never been present).42 Because items originally scored as 3 inflate scores and relate to trait anhedonia, those items were re-coded as a score of 0, such that the SLIPS score in the current study would capture recent changes in levels of anhedonia.42 The SLIPS has demonstrated high levels of internal consistency (α = 0.94) and strong incremental validity when compared with other measures of anhedonia.42 In the current study the SLIPS demonstrated acceptable internal consistency (α = 0.94).
The Interpersonal Needs Questionnaire (INQ) has 15 items used to assess participant's level of perceived burdensomeness with 6 items and perceived levels of thwarted belongingness with the remaining 9 items.43 Based on the IPTS, the INQ examines levels of suicidal desire where higher scores are associated with higher levels of perceived burdensomeness or thwarted belongingness.44 In the current study both burdensomeness (α = 0.95) and belongingness (α = 0.94) demonstrated acceptable internal consistency.
The Acquired Capability for Suicide Scale – Fearlessness about Death (ACSS-FAD) is a self-report measure adapted from the original ACSS to differentiate fearlessness about death from the concept of physiological pain tolerance – both of which make up acquired capability within the IPTS. The ACSS-FAD uses 7 items to assess the level of habituation to fear of death participants exhibit.45 The ACSS-FAD has demonstrated appropriate convergent and discriminant validity.45,46 In the current study the ACSS-FAD demonstrated acceptable internal consistency (α = 0.81).
The Suicidal Behaviors Questionnaire – Revised (SBQ-R) is a 4-item self-report, derived from the SBQ47, that is used to measure suicidal risk levels.48 A score ranging from 3 to 18 reflects past suicidal thoughts, ideation, threats, and attempts as well as future suicidal behaviors.48 The SBQ-R has demonstrated acceptable internal consistency (α = 0.87, clinical sample; α = 0.88, nonclinical sample).48 In the current study the SBQ-R demonstrated acceptable internal consistency (α = 0.74).
Analyses
Data were initially collected from 177 individuals aged 55 and older. Steps were taken in order to check and help ensure data quality, as the data were collected via an online survey. As a first step, any participant who did not make it to the demographics questions of the study was removed. Participants who endorsed the same answer for each item (i.e., all 1s, all 2s, all 3s) on the INQ or the ACSS-FAD, both of which have items that are reverse-scored, were removed. After removing participants for these reasons, the current sample included data from 167 individuals.
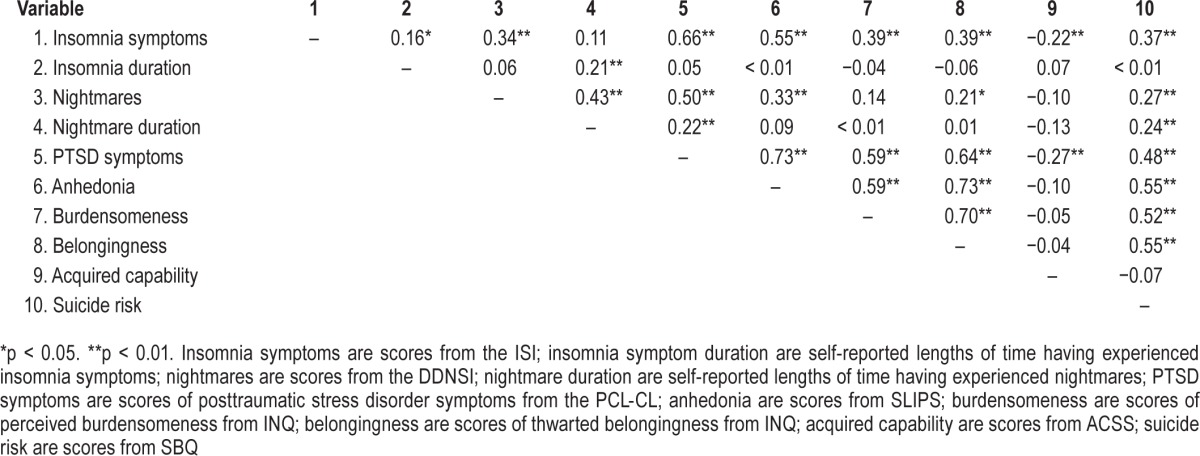
The SBQ was assessed for distribution normality. No deviation from normality was noted (skew = 0.89, kurtosis = 0.01), so no transformations were necessary. Descriptive statistics and correlations for the current sample can be found in Table 1 and Table 2, respectively. An analysis of variance (ANOVA) was utilized to test for effects of gender. Gender, F1,165 = 0.31, p = 0.58, was not significantly related to suicide risk. Thus, gender was not included as a covariate in our analyses.
Table 2.
Correlations of study variables.
RESULTS
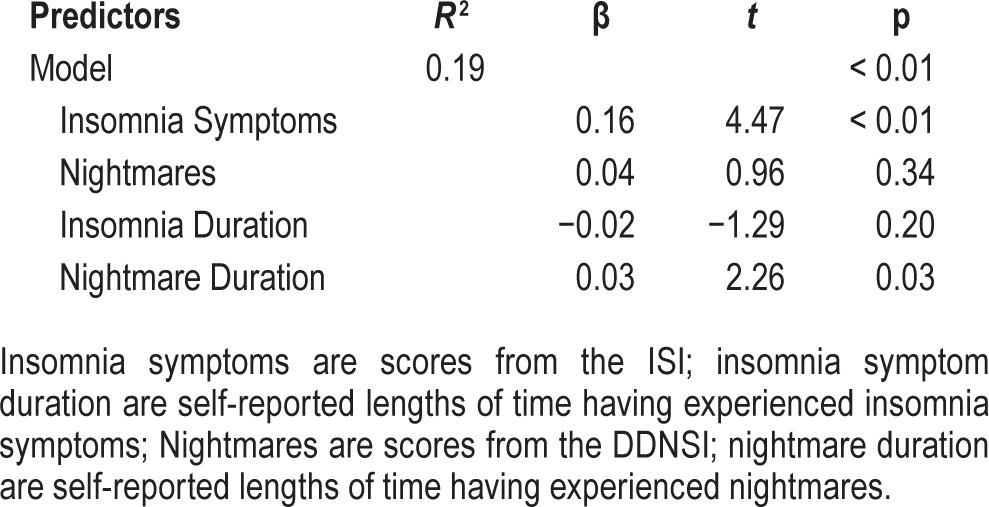
A multiple linear regression assessed the first hypothesis which stated that insomnia duration and nightmare duration are associated with suicide risk independent of current levels of insomnia symptoms and current nightmare severity (see Table 3). The overall regression was significant, n = 165, F4,161 = 9.56, p < 0.01, R2 = 0.19. Level of current insomnia symptoms, β = 0.16, p < 0.01, and nightmare duration, β = 0.03, p = 0.03, were significantly associated with suicide risk; however, duration of insomnia symptoms and current nightmares were not statistically significant in the model. Thus, our first hypothesis was only partially supported, as duration of insomnia symptoms was not associated with suicide risk.
Table 3.
Insomnia duration and nightmare duration predicting suicide risk, controlling for current insomnia and nightmare symptoms.
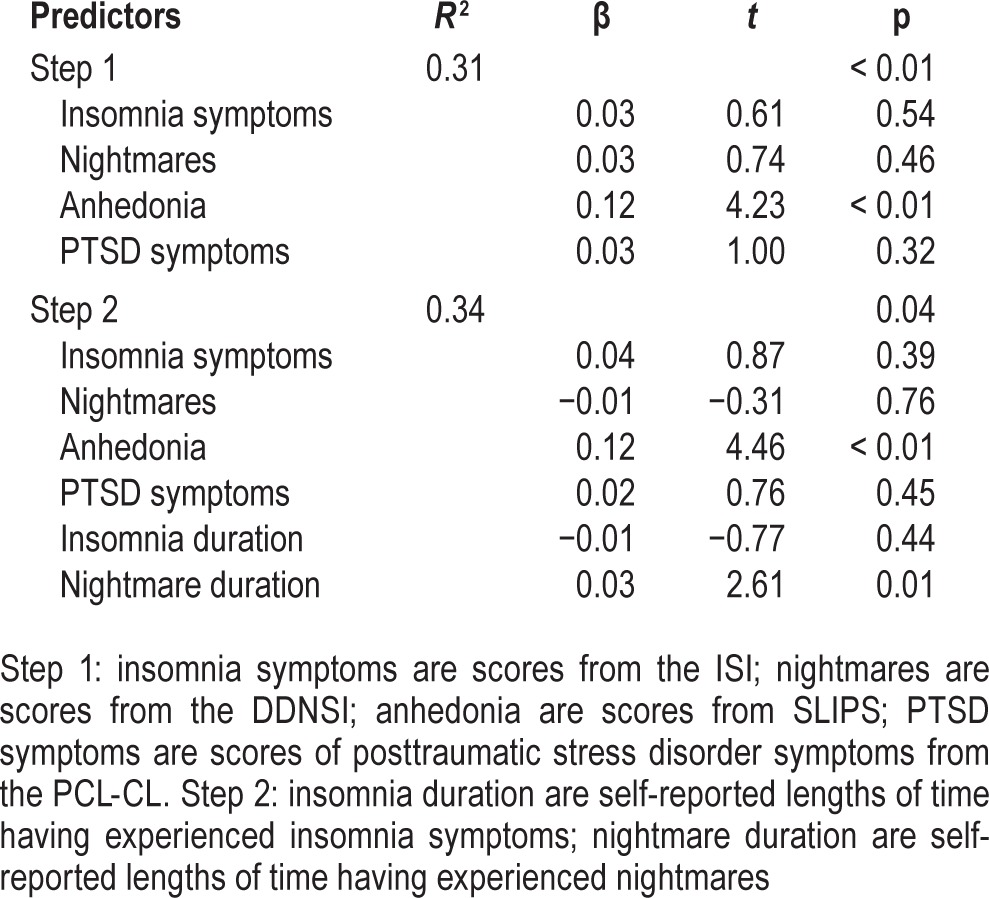
Using a multiple linear regression, the second hypothesis, which stated that insomnia duration and nightmare duration are associated with suicide risk independent of current insomnia symptoms, nightmares, PTSD symptoms, and symptoms of anhedonia, was tested (see Table 4). Current insomnia symptoms, nightmares, PTSD symptoms, and anhedonic symptoms were added in the first step. Insomnia duration and nightmare duration were added in step two. The overall regression was significant in step one, n = 165, F4,161 = 18.36, p < 0.01, R2 = 0.31. Initially, only symptoms of anhedonia, β = 0.12, p < 0.01, were associated with suicide risk, consistent with the previous finding that anhedonic symptoms of depression are related to suicidal ideation independent of cognitive and affective symptoms of depression.49 After adding insomnia duration and nightmare duration to the regression in step two (R2 change = 0.03, F = 3.44, p = 0.04), symptoms of anhedonia, β = 0.12, p < 0.01, and nightmare duration, β = 0.03, p = 0.01, were the only variables associated with suicide risk. Again, our hypothesis was partially supported. Although nightmare duration was associated with suicide risk independent of pathology and current nightmares, insomnia duration again did not have a significant relation with suicide risk within this model.
Table 4.
Insomnia duration and nightmare duration predicting suicide risk, controlling for symptoms of psychopathology including insomnia and nightmare symptoms.
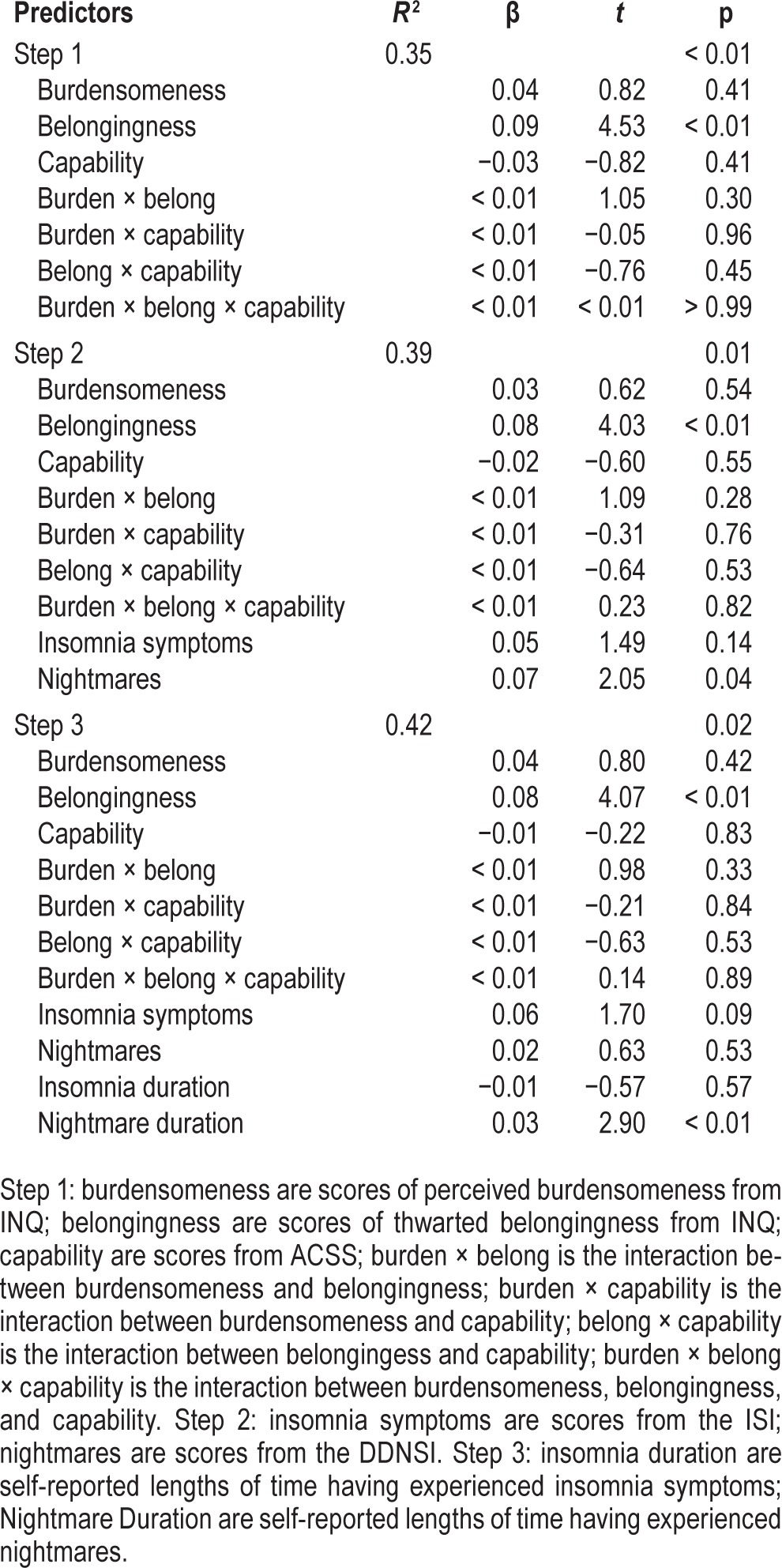
To test the third hypothesis, which predicted that duration of insomnia and nightmares would be associated with risk of suicide independent from current insomnia symptoms, current nightmares, and the IPTS, a multiple linear regression was utilized (see Table 5). In the first step, the constructs and interactions of the IPTS were added; in the second step, current insomnia symptoms and current nightmares were added in. In the third and final step, nightmare duration and insomnia duration were added to the model. The overall regression was significant in step one, n = 164, F7,157 = 12.31, p < 0.01, R2 = 0.35. Thwarted belongingness, β = 0.09, p < 0.01, was positively associated with suicide risk; however, no other part of the IPTS was significantly associated with suicide risk. After adding insomnia severity and current nightmares to the model in step two, thwarted belongingness, β = 0.08, p < 0.01, and current nightmares, β = 0.07, p = 0.04, were positively associated with suicide risk, but no other aspect of the IPTS or current insomnia symptoms were associated with suicide risk. In the final step of the regression (R2 change = 0.03, F = 4.21, p = 0.02), thwarted belongingness, β = 0.08, p < 0.01, and duration of nightmares, β = 0.03, p < 0.01, were positively associated with suicide risk. Thus, our hypothesis was partially supported in that nightmare duration is related to suicide risk independent of the IPTS, current insomnia symptoms, and current nightmares. However, the duration of insomnia symptoms was not significantly associated with suicide risk independent of IPTS, current insomnia, and nightmares and nightmare duration.
Table 5.
Insomnia duration and nightmare duration predicting suicide risk, controlling for symptoms of IPTS and insomnia and nightmare symptoms.
DISCUSSION
The current study is significant as it is the first study to examine whether insomnia and nightmare duration are related to suicide risk among older adults, as well as the first study to examine sleep disturbance duration, suicide risk, and the IPTS in any age group. Although prior findings suggest that duration of sleep disturbance is important in level of suicide risk in young people,14 it was important to examine the role of insomnia and nightmare duration in older adults because sleep disturbances and suicide risk in older adults has presented differently than that for younger or mixed-age samples.13
We found that insomnia symptoms (but not duration of insomnia symptoms) and nightmare duration (but not the current severity of nightmares) were significantly associated with suicide risk. This finding is partially in line with previous research that found insomnia symptoms, but not current nightmares, to be related to suicide risk in older adults.13 However, once symptoms of anhedonia and PTSD (in one regression) and the IPTS (in a second regression) were accounted for, current insomnia symptoms no longer showed a significant relation with suicide risk. Though previous research suggested that current nightmares in older adults may not be relevant in suicide risk assessment,13 which was replicated in the present study, our findings suggest that the duration of nightmares explains a significant proportion of variance in suicide risk level in older adults. In each of our analyses, nightmare duration showed a relation with suicide risk independent of other features of our models; however, insomnia symptom duration did not hold a significant relation with suicide risk for any of our models. Though duration of insomnia symptoms was associated with suicide risk in a college-aged sample,14 that relation was not seen in the current sample of older adults.
The current paper is the first to suggest that duration of nightmares is important in understanding suicide risk among older adults. This finding has clinical relevance in the detection of suicide risk, and we believe that the assessment of suicide risk among older adults who report a long history of nightmares is warranted.
Though the current study did not ultimately find relations among current insomnia symptoms, duration of insomnia, the presence of nightmares, and suicide risk independent of the IPTS, the current study builds off the previous finding that insomnia and nightmares are associated with suicide risk independent of the IPTS in younger adults.12 In older adults, current nightmares and not current insomnia symptoms relate to suicide risk independent of the IPTS; however, nightmare duration mediates the relation between nightmares and suicide risk, suggesting that how long an individual has been experiencing nightmares is more predictive of suicide risk than the current presence of nightmares. These findings suggest that the IPTS cannot fully explain why nightmare duration increases suicide risk among older adults and that further research in this area is warranted.
Lastly, our current findings along with our previous findings among younger adults14 suggest that failing to treat nightmares may increase one's risk for suicide. In assessing patients with suicide risk, it is pertinent to investigate not only current presence of nightmares, but also their history of nightmares. Further, suicide risk should be assessed in patients who report a history of nightmares, as the duration of nightmares is predictive of suicide over and above the typically assessed factors. Given that duration of nightmares is related to suicide risk, treating nightmares early on may prevent suicide risk from increasing. However, to date, no research has found that treating nightmares reduces suicide risk. Based upon our findings, we believe that this research would greatly benefit the literature and is clearly warranted.
Limitations
The current study has a few limitations that must be considered. The first limitation is that the data comprising our sample was combined from two separate studies conducted on mTurk, so it was not a continuous data collection. However, our analyses failed to find any participants who took the study more than once, so we believe the responses meet the statistical assumption of independence. Second, our sample included individuals ages 55 and older, whereas many older adult studies include only those over age 60 or 65. However, we do not believe this to detract from the current findings, as other studies examining insomnia and older adults have used individuals as young as age 50.50 Additionally, a limitation of our current sample is that there was an uneven gender split; however, given that there were no differences in our outcome variable based on gender, the current findings are generalizable and valid. The current sample is not a clinical sample; thus, the findings may not generalize to those at severe risk of suicide. Previous findings, however, have indicated that respondents to mTurk studies exhibit similar or higher levels of anxiety, depression, and exposure to trauma as compared to individuals in the general population.32 Fourth, the current sample relies on retrospective reporting as a measure of duration of insomnia symptoms and nightmares; thus, the data may be less reliable than sleep diaries, actigraphy, or polysomnography for insomnia or nightmare diaries for nightmares. However, the ISI has demonstrated concurrent validity with polysomnography and sleep diaries, suggesting that participants' reports are representative of their current sleep.35,36 A further limitation is that other sleep disorders, such as obstructive sleep apnea, are prevalent among older adults and could not be controlled for in the current study. Although obstructive sleep apnea cannot be ruled out as a cause of sleep disturbance in the current sample, our results indicate that the resulting subjective distress associated with sleep problems can be associated with risk for suicide, though this relation is no longer significant when symptoms of anhedonia and PTSD are statistically removed. Despite this mediation, the literature would benefit from future studies that include sleep studies to examine insomnia and obstructive sleep apnea separately. Additionally, although the DDNSI is a widely used, validated measure of nightmares, it does not include a definition of nightmares and thus relies on respondents' interpretation of whether what they are experiencing is a nightmare. Therefore, it is possible that some respond affirmatively based on night terrors instead of nightmares. However, given that the prevalence rate of night terrors in adults 45 and older ranges from 1% to 2.3%,51 the current findings are unlikely to be impacted by individuals who may have answered the questions based on night terrors.
Future Directions
The current findings indicate that insomnia symptoms and nightmare duration are clinically relevant and should be evaluated in older adults. Further, if endorsed, further screening of mental disorders and suicide risk is warranted. Future longitudinal studies may help further elucidate the timing and mechanism of insomnia and nightmares in relation to suicide risk. Finally, assessing whether nightmare treatment for older adults with nightmares reduces the risk for suicide in those individuals is pertinent. With increased knowledge of risk factors for suicide in older adults, it is important to determine what may eliminate or decrease those risk factors effectively.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
ABBREVIATIONS
- ACSS-FAD
Acquired Capability for Suicide Scale – Fearlessness about Death
- ANOVA
analysis of variance
- DDNSI
Disturbing Dreams and Nightmares Severity Index
- HIT
Human Intelligence Tasks
- INQ
Interpersonal Needs Questionnaire
- IPTS
Interpersonal-Psychological Theory of Suicide
- ISI
insomnia severity index
- mTurk
Amazon.com's Mechanical Turk
- PCL-CL
Posttraumatic Stress Disorder Checklist – Civilian Version
- PTSD
posttraumatic stress disorder
- SBQ-R
Suicidal Behaviors Questionnaire – Revised
- SLIPS
Specific Loss of Interest and Pleasure Scale
- SSRI
Selective Serotonin Reuptake Inhibitor
- VA
Veterans Affairs
REFERENCES
- 1.Centers for Disease Control and Prevention. Web-based Injury Statistics Query and Reporting System. [cited 2014 December 29] Available from: http://www.cdc.gov/injury/wisqars/index.html.
- 2.McIntosh JL. Personal communication. 2014. Dec 23,
- 3.Silverman MM, Berman AL, Sanddal ND, O'Carroll PW, Joiner TE., Jr Rebuilding the tower of babel: a revised nomenclature for the study of suicide and suicidal behaviors: part II: suicide-related ideations, communications and behaviors. Suicide Life Threat Behav. 2007;37:264–77. doi: 10.1521/suli.2007.37.3.264. [DOI] [PubMed] [Google Scholar]
- 4.Miret M, Nuevo R, Morant C, et al. Differences between younger and older adults in the structure of suicidal intent and its correlates. Am J Geriatr Psychiatry. 2010;18:839–47. doi: 10.1097/JGP.0b013e3181d145b0. [DOI] [PubMed] [Google Scholar]
- 5.Chan J, Draper B, Banerjee S. Deliberate self-harm in older adults: a review of the literature from 1995 to 2004. Int J Geriatr Psychiatry. 2007;22:720–32. doi: 10.1002/gps.1739. [DOI] [PubMed] [Google Scholar]
- 6.Beautrais AL. A case control study of suicide and attempted suicide in older adults. Suicide Life Threat Behav. 2002;32:1–9. doi: 10.1521/suli.32.1.1.22184. [DOI] [PubMed] [Google Scholar]
- 7.Conwell Y, Duberstein PR, Caine ED. Risk factors for suicide in later life. Biol Psychiatry. 2002;52:193–204. doi: 10.1016/s0006-3223(02)01347-1. [DOI] [PubMed] [Google Scholar]
- 8.Pompili M, Innamorati M, Masotti V, et al. Suicide in the elderly: a psychological autopsy study in a north Italy area (1994-2004) Am J Geriatric Psychiatry. 2008;16:727–35. doi: 10.1097/JGP.0b013e318170a6e5. [DOI] [PubMed] [Google Scholar]
- 9.Mays D. Structured assessment methods may improve suicide prevention: standard patient interview processes can mislead clinicians about acute risk factors. Psychiatr Ann. 2004;34:367–72. [Google Scholar]
- 10.Cukrowicz KC, Otamendi A, Pinto JV, Bernert RA, Krakow B, Joiner TE., Jr The impact of insomnia and sleep disturbances on depression and suicidality. Dreaming. 2006;16:1–10. [Google Scholar]
- 11.McCall WV, Blocker JN, D'Agostino R, Jr, et al. Insomnia severity is an indicator of suicidal ideation during a depression clinical trial. Sleep Med. 2010;11:822–27. doi: 10.1016/j.sleep.2010.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nadorff MR, Anestis MD, Nazem S, Claire Harris H, Samuel Winer E. Sleep disorders and the interpersonal-psychological theory of suicide: independent pathways to suicidality? J Affect Disord. 2014;152-4:505–12. doi: 10.1016/j.jad.2013.10.011. [DOI] [PubMed] [Google Scholar]
- 13.Nadorff MR, Fiske A, Sperry JA, Petts R, Gregg JJ. Insomnia symptoms, nightmares, and suicidal ideation in older adults. J Gerontol Psychol Sci. 2013;68B:145–52. doi: 10.1093/geronb/gbs061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nadorff MR, Nazem S, Fiske A. Insomnia symptoms, nightmares, and suicide risk: duration of sleep disturbance matters. Suicide Life Threat Behav. 2013;43:139–49. doi: 10.1111/sltb.12003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bernert RA, Turvey CL, Conwell Y, Joiner TE., Jr Association of poor subjective sleep quality with risk for death by suicide during a 10-year period: a longitudinal, population-based study of late life. JAMA Psychiatry. 2014;71:1129–37. doi: 10.1001/jamapsychiatry.2014.1126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McCall WV, Batson N, Webster M, et al. Nightmares and dysfunctional beliefs about sleep mediate the effect of insomnia symptoms on suicidal ideation. J Clin Sleep Med. 2013;9:135–40. doi: 10.5664/jcsm.2408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McCall WV, Black CG. The link between suicide and insomnia: theoretical mechanisms. Curr Psychiatry Rep. 2013;15:389–89. doi: 10.1007/s11920-013-0389-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pigeon WR, Britton PC, Ilgen MA, Chapman B, Conner KR. Sleep disturbance preceding suicide among veterans. Am J Public Health. 2012;102:S93–7. doi: 10.2105/AJPH.2011.300470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ribeiro JD, Pease JL, Gutierrez PM, et al. Sleep problems outperform depression and hopelessness as cross-sectional and longitudinal predictors of suicidal ideation and behavior in young adults in the military. J Affect Disord. 2012;136:743–50. doi: 10.1016/j.jad.2011.09.049. [DOI] [PubMed] [Google Scholar]
- 20.Nadorff MR, Nazem S, Fiske A. Insomnia symptoms, nightmares, and suicidal ideation in a college student sample. Sleep. 2011;34:93–8. doi: 10.1093/sleep/34.1.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sjöström N, Hetta J, Waern M. Persistent nightmares are associated with repeat suicide attempt: a prospective study. Psychiatry Res. 2009;170:208–11. doi: 10.1016/j.psychres.2008.09.006. [DOI] [PubMed] [Google Scholar]
- 22.Sjöström N, Wærn M, Hetta J. Nightmares and sleep disturbances in relation to suicidality in suicide attempters. Sleep. 2007;30:91–5. doi: 10.1093/sleep/30.1.91. [DOI] [PubMed] [Google Scholar]
- 23.Bernert RA, Joiner TE, Cukrowicz KC, Schmidt NB, Krakow B. Suicidality and sleep disturbances. Sleep. 2005;28:1135–41. doi: 10.1093/sleep/28.9.1135. [DOI] [PubMed] [Google Scholar]
- 24.Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite SR, Selby EA, Joiner TE., Jr The interpersonal theory of suicide. Psychol Rev. 2010;117:575–600. doi: 10.1037/a0018697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Van Orden KA, Witte TK, Gordon KH, Bender TW, Joiner TE., Jr Suicidal desire and the capability for suicide: tests of the interpersonal-psychological theory of suicidal behavior among adults. J Consult Clin Psychol. 2008;76:72–83. doi: 10.1037/0022-006X.76.1.72. [DOI] [PubMed] [Google Scholar]
- 26.Joiner T. Cambridge, MA: Harvard University Press; 2005. Why people die by suicide. [Google Scholar]
- 27.Joiner T, Van Orden KA, Witte TK, et al. Main predictions of the interpersonal- psychological theory of suicidal behavior: empirical tests in two samples of young adults. J Abnorm Psychol. 2009;118:634–46. doi: 10.1037/a0016500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vitiello MV. Sleep in normal aging. Sleep Med Clin. 2006;1:171–6. doi: 10.1016/j.jsmc.2017.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ohayon MM, Carskadon MA, Guilleminault C, Vitiello MV. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan. Sleep. 2004;27:1255–73. doi: 10.1093/sleep/27.7.1255. [DOI] [PubMed] [Google Scholar]
- 30.Van Orden KA, Talbot N, King D. Using the interpersonal theory of suicide to inform interpersonal psychotherapy with a suicidal older adult. Clin Case Stud. 2012;11:333–47. doi: 10.1177/1534650112457710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Buhrmester M, Kwang T, Gosling SD. Amazon's Mechanical Turk: a new source of inexpensive, yet high-quality, data? Perspectives Psychol Sci. 2011;6:3–5. doi: 10.1177/1745691610393980. [DOI] [PubMed] [Google Scholar]
- 32.Shapiro DN, Chandler J, Mueller PA. Using Mechanical Turk to study clinical populations. Clin Psychol Sci. 2013;1:213–20. [Google Scholar]
- 33.Amazon.com Mechanical Turk. Worker Web Site FAQs. [cited 2015 May 15] Available from https://www.mturk.com/mturk/help?helpPage=worker#what_is_master_worker.
- 34.US Census Bureau. Population Growth Tables. [cited 2015 May 12] Available from: www.census.gov/popclock/data_tables.php?component=growth.
- 35.Bastien CH, Vallières A, Morin CM. Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Med. 2001;2:297–307. doi: 10.1016/s1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- 36.Savard M-H, Savard J, Simard S, Ivers H. Empirical validation of the insomnia severity index in cancer patients. Psychooncology. 2005;14:429–41. doi: 10.1002/pon.860. [DOI] [PubMed] [Google Scholar]
- 37.Krakow B, Hollifield M, Schrader R, et al. A controlled study of imagery rehearsal for chronic nightmares in sexual assault survivors with PTSD: a preliminary report. J Trauma Stress. 2000;13:589–609. doi: 10.1023/A:1007854015481. [DOI] [PubMed] [Google Scholar]
- 38.Krakow B, Schrader R, Tandberg D, et al. Nightmare frequency in sexual assault survivors with PTSD. J Anxiety Disord. 2002;16:175–90. doi: 10.1016/s0887-6185(02)00093-2. [DOI] [PubMed] [Google Scholar]
- 39.Krakow BJ, Melendrez DC, Johnston LG, et al. Sleep dynamic therapy for Cerro Grande fire evacuees with posttraumatic stress symptoms: a preliminary report. J Clin Psychiatry. 2002;63:673–84. doi: 10.4088/jcp.v63n0804. [DOI] [PubMed] [Google Scholar]
- 40.Weathers FW, Litz BT, Herman DS, Huska JA, Keane TM. The PTSD Checklist (PCL): reliability, validity, and diagnostic utility. International Society of Traumatic Stress Studies. 1993 [Google Scholar]
- 41.Peterlin BL, Tietjen G, Meng S, Lidicker J, Bigal M. Post-Traumatic Stress Disorder in Episodic and Chronic Migraine. Headache: J Head Face Pain. 2008;48:517–22. doi: 10.1111/j.1526-4610.2008.00917.x. [DOI] [PubMed] [Google Scholar]
- 42.Winer ES, Veilleux JC, Ginger EJ. Development and validation of the Specific Loss of Interest and Pleasure Scale (SLIPS) J Affect Disord. 2014;152-154:193–201. doi: 10.1016/j.jad.2013.09.010. [DOI] [PubMed] [Google Scholar]
- 43.Van Orden KA, Cukrowicz KC, Witte TK, Joiner TE., Jr Thwarted belongingness and perceived burdensomeness: construct validity and psychometric properties of the Interpersonal Needs Questionnaire. Psychol Assess. 2012;24:197–215. doi: 10.1037/a0025358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Van Orden KA, Witte TK, James LM, et al. Suicidal ideation in college students varies across semesters: The mediating role of belongingness. Suicide Life Threat Behav. 2008;38:427–35. doi: 10.1521/suli.2008.38.4.427. [DOI] [PubMed] [Google Scholar]
- 45.Ribeiro JD, Witte TK, Van Orden KA, et al. Fearlessness about death: the psychometric properties and construct validity of the revision to the Acquired Capability for Suicide Scale. Psychol Assess. 2014;26:115–26. doi: 10.1037/a0034858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Witte TK, Gordon KH, Smith PN, Van Orden KA. Stoicism and sensation seeking: male vulnerabilities for the acquired capability for suicide. J Res Pers. 2012;46:384–92. doi: 10.1016/j.jrp.2012.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Linehan MM. The Suicidal Behaviors Questionnaire (SBQ) University of Washington. 1981 [Google Scholar]
- 48.Osman A, Bagge CL, Gutierrez PM, Konick LC, Kopper BA, Barrios FX. The Suicidal Behaviors Questionnaire--Revised (SBQ-R): validation with clinical and nonclinical samples. Assess. 2001;8:443–54. doi: 10.1177/107319110100800409. [DOI] [PubMed] [Google Scholar]
- 49.Winer ES, Nadorff MR, Ellis TE, Allen JG, Herrera S, Salem T. Anhedonia predicts suicidal ideation in a large psychiatric inpatient sample. Psychiatry Res. 2014;218:124–28. doi: 10.1016/j.psychres.2014.04.016. [DOI] [PubMed] [Google Scholar]
- 50.Lichstein KL, Nau SD, Wilson NM, et al. Psychological treatment of hypnotic-dependent insomnia in a primarily older adult sample. Behav Res Ther. 2013;51:787–96. doi: 10.1016/j.brat.2013.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ohayon MM, Guilleminault C, Priest RG. Night terrors, sleepwalking, and confusional arousals in the general population: their frequency and relationship to other sleep and mental disorders. J Clin Psychiatry. 1999;60:268–76. doi: 10.4088/jcp.v60n0413. [DOI] [PubMed] [Google Scholar]


