Abstract
Multiple myeloma is a malignant tumour characterized by proliferation of a single clone of plasma cells, this cell line will produce large amount of ineffective immunoglobulins that are ineffective at fighting infection resulting in immunosuppression.
These are medullary tumours most of the time; however, in rare cases they may arise extra medullary.
The incidence of extramedullary plasmocytoma is about 5% and they arise in the chest most of the time; but they can also arise in other body systems like gastrointestinal system, which is involved in 10% of the time. We present a very rare case of primary plasmocytoma involving the pancreas. According to our research, there are only 25 cases of primary pancreatic plasmocytoma reported in english literature.
Keywords: Plasmocytoma, Primary, Multiple myeloma, Rare, Obstructing jaundice
Extramedullary plasmocytoma is a rare entity. It is usually diagnosed in patients with widespread multiple myeloma. Its primary form is extremely rare, and the upper respiratory tract is the most commonly involved site, with only 10% involving the gastrointestinal tract. Pancreatic involvement with plasmocytoma is extremely rare; there are only 25 cases reported in English literature until 2012 [1].
1. Case report
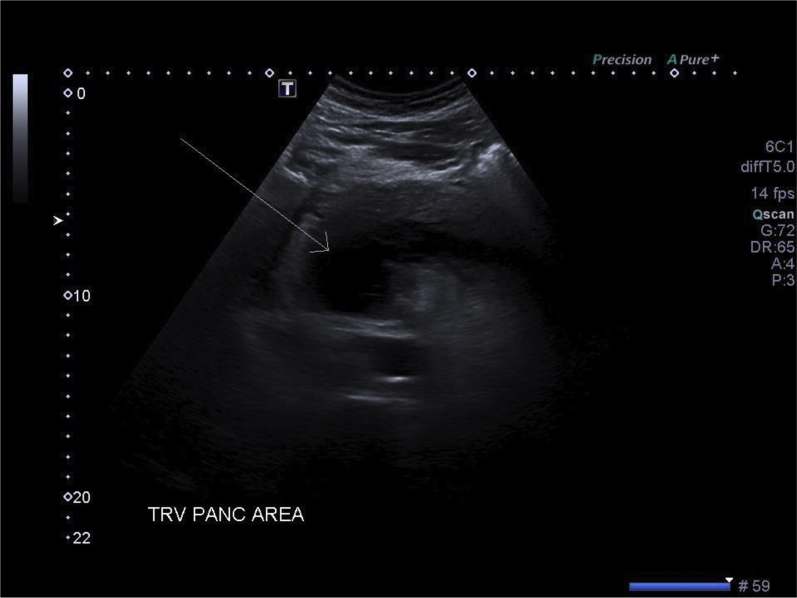
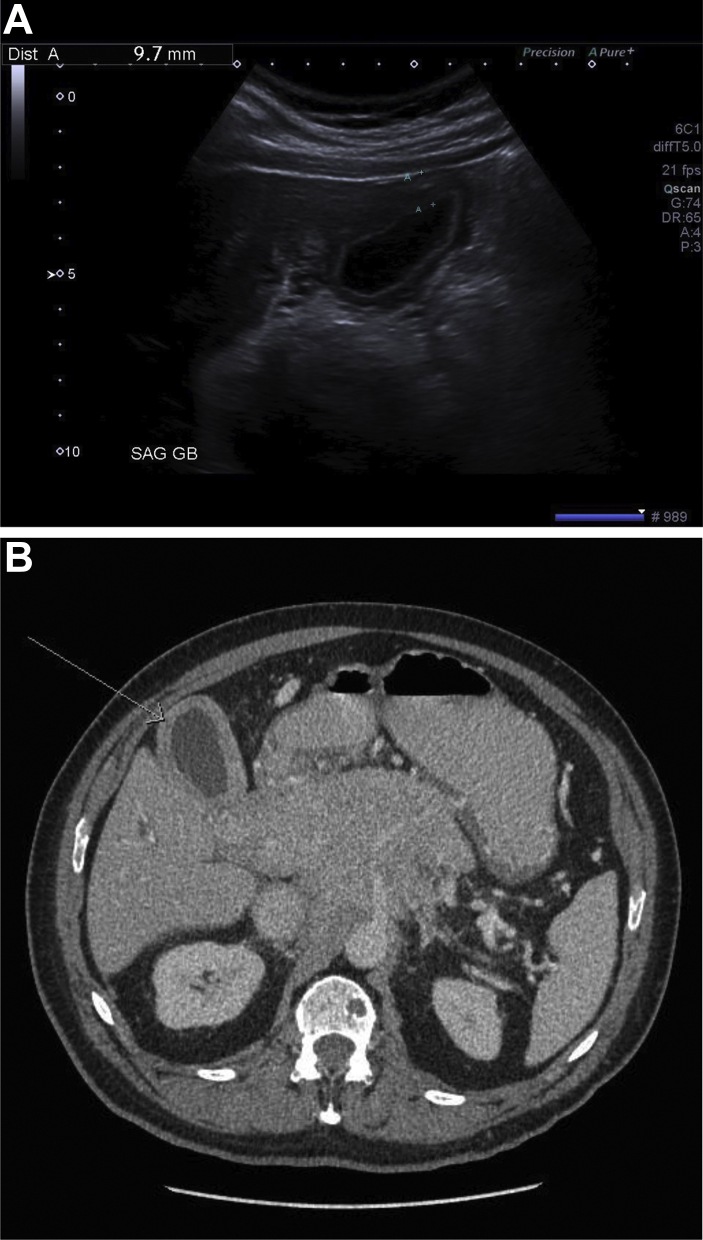
A 66-year-old male patient presented with epigastric pain, vomiting, and weight loss over a period of several months. Initial ultrasonographic examination of the upper abdomen revealed diffuse intrahepatic and extrahepatic bile duct dilatation with no intraductal stone (see Fig. 1). The pancreas was enlarged, with heterogeneous texture and no pancreatic duct dilatation. A large hypoechoic mass was identified in the region of pancreatic head (see Fig. 2) with the vessel piercing the lesion. The gall bladder wall was thick and edematous (see Fig. 3).
Fig. 1.
Transverse ultrasound image shows dilated common bile duct with thickened walls (arrow). CBD = common bile duct.
Fig. 2.
Transverse ultrasound image through the head and uncinate process of the pancreas shows large hypoechoic mass (arrow). TRV PANC AREA = transverse pancreatic area.
Fig. 3.
Transverse ultrasound (A) and enhanced axial CT (B) images through the gall bladder show thickened walls (arrow). SAG GB = sagittal gallbladder.
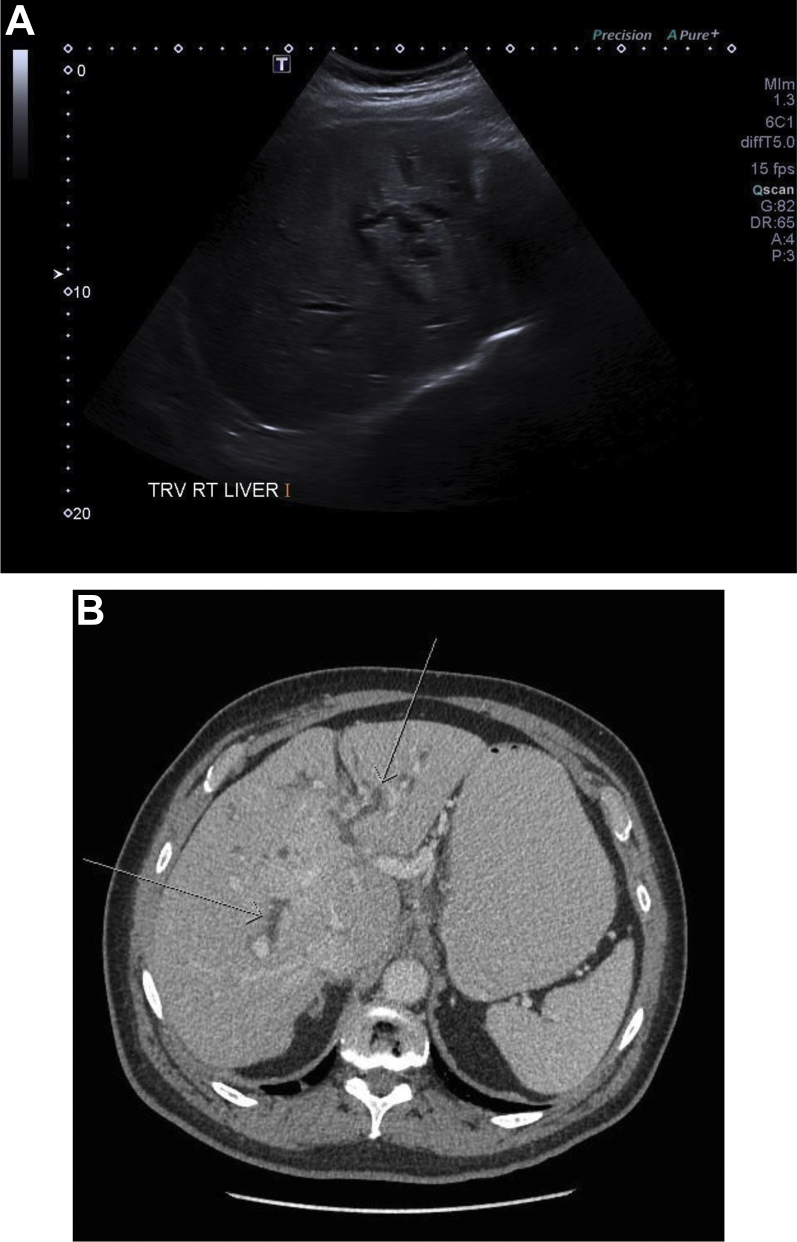
Subsequent computed tomography (CT) confirmed the pancreatic head mass had extended into porta hepatis causing dilatation of biliary ducts with gall bladder neck invasion (see Figs. 4 and 5).
Fig. 4.
Transverse ultrasound (A) and enhanced axial CT (B) images show dilated intrahepatic biliary tree (arrow). TRV RT LIVER = transverse right liver.
Fig. 5.
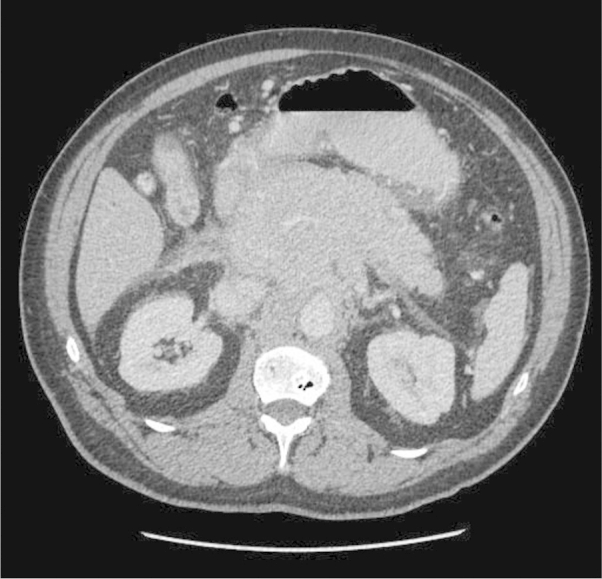
Enhanced axial CT image through the pancreatic mass at the portal venous phase demonstrated diffuse homogeneous enhancement.
CT images also demonstrated encasement of the celiac axis and superior mesenteric arteries without occlusion. Diffuse lytic bony lesions were also present (see Fig. 6).
Fig. 6.
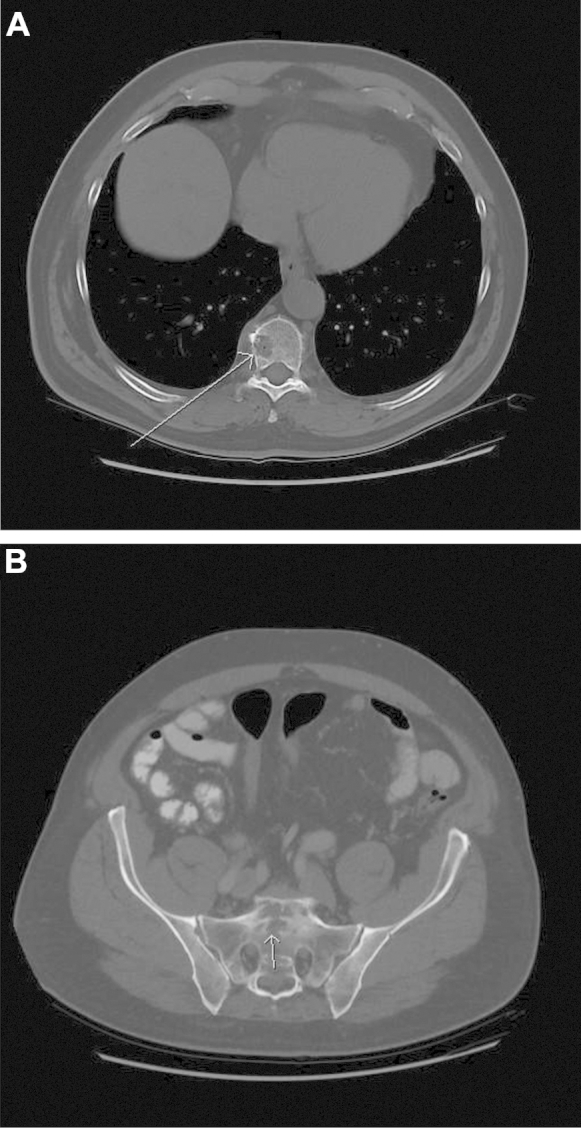
Axial CT images in bone window shows widespread lytic bony lesions (arrows). A, at the level of middle thoracic spine. B, at the level of sacrum.
The differential diagnosis at this point would possibly include
-
1.
lymphoma, given the homogeneous nature of the mass and encasement of the mesenteric blood vessels;
-
2.
pancreatic adenocarcinoma;
-
3.
or, less likely, cholangiocarcinoma.
The patient had a CT-guided biopsy of the pancreatic mass, which confirmed to be a plasmocytoma (see Fig. 7).
Fig. 7.

CT-guided biopsy of the pancreatic mass using 18-gauge quick core needle biopsy in the prone position.
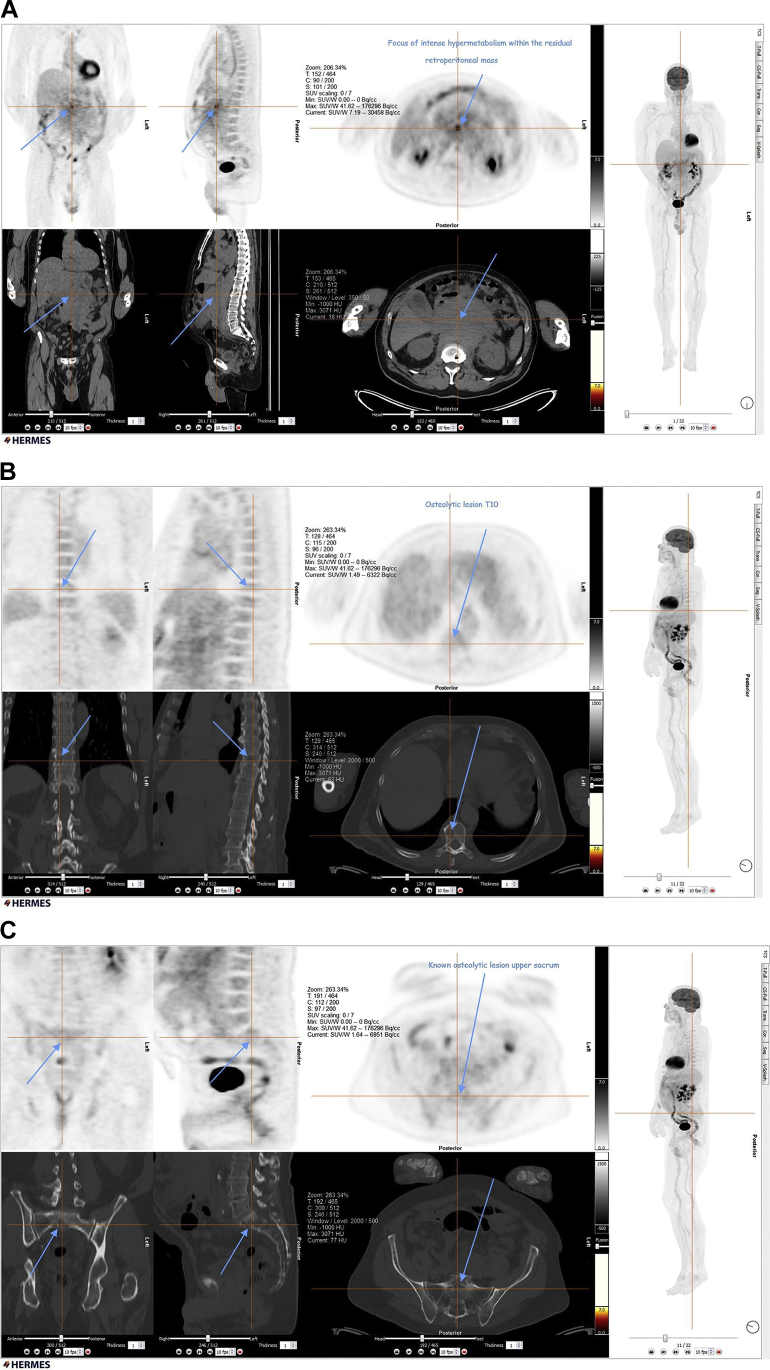
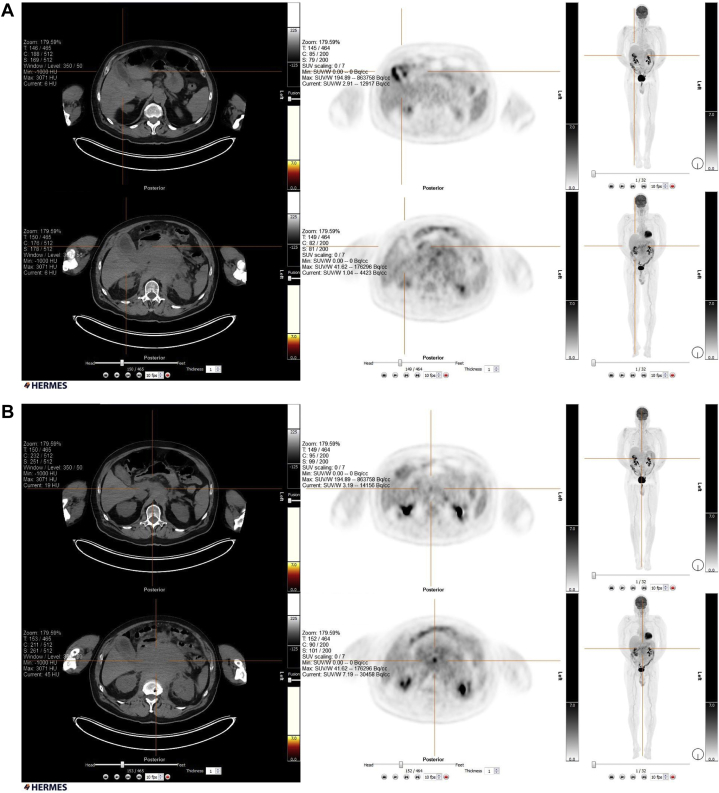
The patient received chemotherapy followed by autologous bone marrow transplant. Follow-up imaging confirmed initial good response to treatment, but unfortunately, the most recent positron emission tomography scan demonstrated persistent metabolic activity in a lymph node anterior to the pancreas and in the wall of gall bladder (see Fig. 8, Fig. 9, Fig. 10).
Fig. 8.
A shows the extent of soft tissue involvement, B and C demonstrate the extent of bony involvement. Positron emission tomography scan before chemotherapy demonstrates the extent of the disease (arrows).
Fig. 9.
Positron emission tomography scan after chemotherapy demonstrates a response manifested by decrease in the pancreatic mass with persistent activity in the gall bladder (A and B).
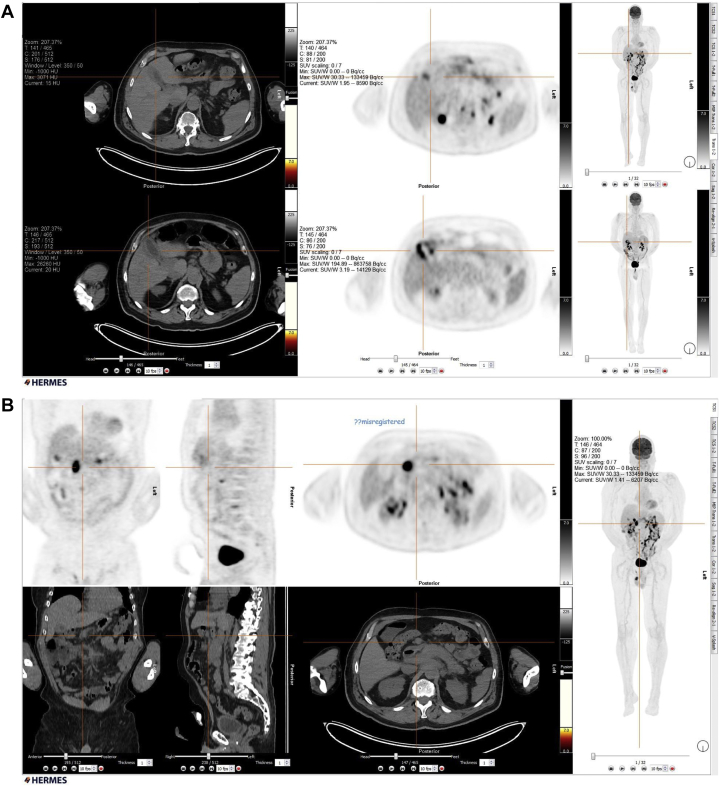
Fig. 10.
Positron emission tomography scan after bone marrow transplant demonstrates a significant decrease in the pancreatic mass size with some persistent activity in a small node anterior to the pancreas and the wall of gall bladder (A and B).
2. Discussion
Multiple myeloma is malignant proliferation of single clone of plasma cell–producing monoclonal antibodies. Plasmocytoma is a discrete mass of plasma cells, most often in the bones or occasionally in an extramedullary location [2]. The latter is rare [3], with median age of presentation at 55 years and a slight male predominance. Plasmocytoma can be primary or secondary, with the secondary form more common [2]. Only 5% of plasmocytomas involve extraosseous tissue, and they are typically diagnosed after the diagnosis of multiple myeloma had been established. Most of these involve the upper respiratory tract; only 10% involves gastrointestinal tract, mainly the stomach, the liver, and the spleen. There are only 25 cases of pancreatic involvement in the English literature [1]. A pancreatic mass in a patient with an established diagnosis of multiple myeloma should raise the suspicion of pancreatic involvement by the disease [4].
It can involve any part of the pancreas. Pancreatic head involvement is by far the most common [2], resulting in upper abdominal pain and obstructive jaundice.
The radiologic findings of pancreatic plasmocytoma are not very specific. Ultrasonography demonstrates a heterogeneous mass that is hypoechoic to the surrounding tissue. CT shows homogeneous enhancement of a multilobulated mass. Diffuse pancreatic enlargement is often described. Dual-phase CT with pancreatic protocol is considered the modality of choice allowing assessment of vascularity. Magnetic resonance imaging is felt less favored currently [5]. Although CT scan is the investigation of choice, imaging features are not specific and may mimic other entities such as pancreatic carcinoma, lymphoma, islets cell tumor, and metastasis [6].
The treatment of multiple myeloma includes steroid and chemotherapy in addition to radiation therapy for symptomatic lesions. Other methods of treatment are under investigation such as thalidomide, angiogenic agents, and stem cell transplant. To our knowledge, there is no standardized treatment targeting extramedullary plasmocytoma [5].
3. Conclusion
Pancreatic plasmocytoma is a rare entity; it should be considered in the differential diagnosis in patients presenting with a hypoechoic pancreatic head mass and diffuse lytic bony lesions.
Footnotes
Competing Interests: The authors hereby certify that, to the best of their knowledge, (1) the work which is reported on in said manuscript has not received financial support from any pharmaceutical company or other commercial source and (2) neither the author nor any first-degree relative has any special financial interest in the subject matter discussed in said manuscript. The authors declare that they have no competing interests.
References
- 1.Smith A., Hal H., Frauenhoffer E. Extramedullary plasmacytoma of the pancreas: a rare entity. Case Rep Radiol. 2012;2012:798264. doi: 10.1155/2012/798264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pallavi R., Ravella P.M., Popescu-Martinez A. An unusual pancreatic mass: a case report and literature review. Transl Gastrointest Cancer. 2014;3(2):106–110. [Google Scholar]
- 3.Deguchi Y., Nonaka A., Takeuchi E., Funaki N., Kono Y., Mizuta K. Primary pancreatic plasmacytoma. Am J Clin Oncol. 2004;27(3):247–249. doi: 10.1097/01.coc.0000092613.05046.28. [DOI] [PubMed] [Google Scholar]
- 4.Wilson T.E., Korobkin M., Francis I.R. Pancreatic plasmacytoma: CT findings. AJR Am J Roentgenol. 1989;152:1227–1228. doi: 10.2214/ajr.152.6.1227. [DOI] [PubMed] [Google Scholar]
- 5.Leake P.A., Coard K.C., Plummer J.M. Extramedullary plasmacytoma of the pancreas as an uncommon cause of obstructive jaundice: a case report. J Med Case Rep. 2009;3:8785. doi: 10.4076/1752-1947-3-8785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hiller N., Goitein O., Ashkenazi Y.J. Plasmacytoma of the pancreas. Isr Med Assoc J. 2004;6:704–705. [PubMed] [Google Scholar]