Abstract
Primary testicular lymphoma (PTL) is an uncommon neoplasm (<5% of all testicular tumors). Testicular lymphoma presents with homogeneous mass, hyperintense on T1-weighted images, and iso-to-hypointense on T2-weighted images with strong diffusion restriction and homogeneous contrast enhancement. Seminoma testis, a close differential due to T2 hypointensity and homogeneousity, can be differentiated by its lower diffusion restriction and younger age group. Involvement of spermatic cord and epididymis is rare with seminoma. Intra-abdominal extension along the gonadal vein is not reported. PTL disseminates to extranodal sites. However, extension of PTL along the spermatic cord and gonadal vein up to the inferior vena cava is a rare phenomenon. We report 2 cases of PTL with involvement of epididymis and spermatic cord and further continuous extension along the gonadal vein up to the inferior vena cava. These findings are very rare and when present may help to differentiate testicular lymphoma from other testicular tumors.
Keywords: Primary testicular lymphoma, Intra-abdominal extension
Introduction
Primary testicular lymphoma (PTL) is a very uncommon neoplasm constituting <5% of all testicular tumors and 1%-2% of non-Hodgkin lymphomas [1], [2]. PTL has a tendency to disseminate to other extranodal sites such as contralateral testis, central nervous system, lung, pleura, Waldeyer ring, skin, and soft tissues [3], [4]. However, continuous extension of the PTL along the spermatic cord and gonadal veins in the absence of other deposits or manifestations is a very rare phenomenon. We report 2 such cases of PTL with extension along epididymis and spermatic cord into the inguinal canal with further continuous extension along the gonadal vessels up to inferior vena cava. These imaging findings, when present, may help to differentiate testicular lymphoma from other testicular tumors on imaging.
Case report
Case 1
An 85-year-old man presented with a history of gradually increasing painless swelling in the right hemiscrotum since 4 months. He also complained of vague abdominal discomfort and intermittent pain. On examination, the scrotum was visibly enlarged with normal overlying skin. On palpation, there was a firm to hard mass in the right side of the scrotal sac measuring approximately 12 × 10 cm. It was extending superiorly into the right inguinal canal along the spermatic cord. The right testis was not palpable separately from the mass. The left testis appeared normal in size. Magnetic resonance imaging examination of abdomen and pelvis was done.
On magnetic resonance imaging examination, a large heterogeneous signal intensity mass lesion was seen in scrotum arising from the right testis and completely replacing it (Figure 1 A to I). The lesion measured approximately 7 × 7.5 × 5 cm in size. It was T1 hypointense, T2 iso-to-hypointense, short tau inversion recovery (STIR) hyperintense, and showing strong diffusion restriction. Mild homogeneous postcontrast enhancement was seen within the mass. The mass was extending along the right epididymis and right spermatic cord into the right inguinal canal and further extending into the abdomen along the right gonadal vein up to its (venous) drainage into the inferior vena cava. No significant iliac, para-aortic, or mesenteric lymph nodes were detected. Abdominal visceral organs were normal. Overall picture was suggestive of malignant neoplasm of right testis with extension along spermatic cord and right gonadal vein; diagnostic possibilities of seminoma testis and PTL were considered.
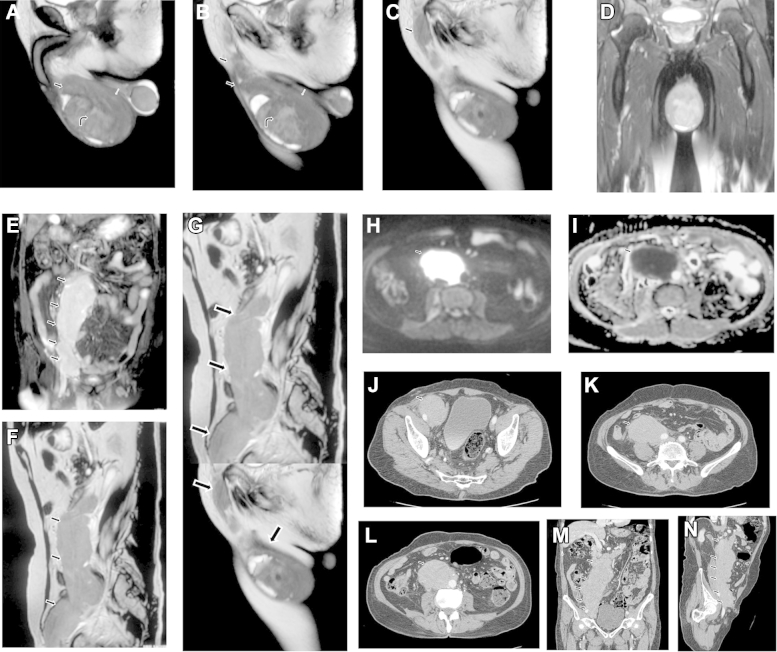
Fig. 1.
An 85-year-old man: (A) Sagittal T2-weighted images of the scrotum - a large heterogeneous T2 isointense-to-hypointense mass lesion seen in the scrotum arising from the right testis and completely replacing it (curved black arrow); (B) the mass was extending along the right epididymis (white arrow) and right spermatic cord (black arrow); and (C) continuous extension of the mass along up to inguinal ring (black arrow). (D) Coronal STIR image of the scrotum of an 85-year-old man: a large heterogeneous STIR hyperintense mass lesion seen in the scrotum arising from the right testis and completely replacing it (black arrow). Magnetic resonance images of the scrotum of the 85-year-old man: (E) coronal STIR image of abdomen: large STIR hyperintense mass lesion is seen extending obliquely from the right inguinal region to the right para-aortic region (black arrow); (F) sagittal T2-weighted image of the abdomen: large T2 isointense-to-hypointense mass lesion is seen extending obliquely from the right inguinal region to the right para-aortic region (black arrow); (G) sagittal T2-weighted pasted image shows continuous extension of the mass lesion from the right testis and epididymis, along the right spermatic cord to the abdomen (black arrow); (H) axial diffusion-weighted image shows increased signals from the mass suggestive of strong diffusion restriction (black arrow); (I) corresponding axial ADC map shows hypointensity within the mass suggestive of strong diffusion restriction (black arrow). Contrast-enhanced CT of the abdomen of the 85-year-old man: (J) axial postcontrast CT image, at the level of external iliac vessels, shows large well-defined homogeneous mass lesion along the right external iliac vessels (black arrow); (K) axial postcontrast CT image, at the level of internal iliac vessels, shows large well-defined homogeneous mass lesion encasing the right gonadal vessels and partly encasing the right external iliac artery (black arrow); (L) axial postcontrast CT image, at the lower para-aortic level, shows large well-defined homogeneous mass lesion along the right gonadal vessels (black arrow); (M) coronal postcontrast CT image shows continuous extension of the homogeneous mass lesion from the right external iliac vessels to the para-aortic region (black arrow); and (N) oblique sagittal postcontrast CT image shows continuous extension of the homogeneous mass lesion from the right inguinal region to the para-aortic region (black arrow).
The patient underwent right inguinal orchiectomy. The histopathology examination revealed diffuse large B cell lymphoma of testis. Further staging workup revealed no other deposits or lymphadenopathy. Contrast computed tomography (CT) abdomen study (part of staging workup) also confirmed homogeneous mildly enhancing soft tissue attenuation mass extending along right gonadal vein with no significant retroperitoneal or mesenteric lymphadenopathy (Figure 1 J to N). Final diagnosis was diffuse large B cell non-Hodgkin lymphoma stage IIAE. The patient was offered chemotherapy and radiotherapy.
Case 2
A 68-year-old man presented with a history of pain and redness over the right hemiscrotum since 2 months which was gradually increasing in size. Ultrasonographic examination in a local hospital revealed left inguinal hydrocele and right testicular hypoechoic lesion extending into the right spermatic cord. Possibilities of chronic orchitis and testicular neoplasm were considered. The patient was operated, and right orchiectomy with eversion of left tunica vaginalis sac was done. The histopathology examination revealed diffuse large B cell lymphoma of testis. The patient was referred to our hospital for further workup and management.
Ultrasonographic scan of neck and contrast CT scan of thorax, abdomen, and pelvis were done as a part of staging workup, which revealed homogeneous well-defined cordlike mass lesion along right gonadal vein extending from the right inguinal canal below to the junction of right gonadal vein and inferior vena cava superiorly. No solid visceral organ or bowel involvement was detected. No retroperitoneal or mesenteric lymph nodes or ascites were detected. No obvious lymphoma deposits were detected above diaphragm (Figure 2).
Fig. 2.
Contrast-enhanced CT of the abdomen of a 68-year-old man. (A) Axial postcontrast CT image, at the level of deep inguinal ring, shows well-defined homogeneous mass lesion at the right deep inguinal ring (black arrow). (B-D) axial postcontrast CT image, at the level of external iliac vessels, shows well-defined homogeneous mass lesion encasing right gonadal vessels, just anterior to the right external iliac artery (black arrow). (E) Axial postcontrast CT image, at the level of internal iliac vessels, shows well-defined homogeneous mass lesion encasing the right gonadal vessels (black arrow). (F) Axial postcontrast CT image, at the lower para-aortic level, shows well-defined homogeneous mass lesion along the right gonadal vessels (black arrow). (G) Coronal postcontrast CT image shows continuous cordlike extension of the homogeneous mass lesion from the right external iliac vessels to the para-aortic region (black arrow). (H) Oblique sagittal postcontrast CT image shows continuous cordlike extension of the homogeneous mass lesion from the right deep inguinal region to the para-aortic region (black arrow).
Final diagnosis was diffuse large B cell non-Hodgkin lymphoma stage II. Chemotherapy with CHOP regimen (Cyclophosphamide, doxorubicin, vincristine, Prednisolone) was planned for the patient.
Discussion
PTL is a very uncommon neoplasm constituting <5% of all testicular tumors. For lymphoma per se also, it is an uncommon site of involvement, representing 1%-2% of all non-Hodgkin lymphomas. PTL occurs mainly in patients older than 50 years, and almost 85% of all PTL patients are older than 60 years [1], [2]. Most patients present with early localized disease (stage I or II).
Radiologically, the closest differential diagnosis of PTL is seminoma, as it also presents as homogeneous testicular mass usually replacing the testis. Typical features of testicular lymphoma are homogeneous mass lesion replacing the testis, hyperintense on T1-weighted images, and isointense to hypointense on T2-weighted images. It shows moderate-to-strong diffusion restriction and homogeneous contrast enhancement. Calcifications and hemorrhages are rare. Intra-abdominal lymphadenopathy is rare with PTL. However, in occult or manifest generalized lymphoma, testicular involvement is usually associated with intra-abdominal solid organ or lymph node involvement in disease course.
Although seminoma testis is a close differential, owing to T2 hypointensity and homogeneous texture, it can be differentiated by its lower diffusion restriction and presentation in a younger patient subset. Involvement of the spermatic cord and epididymis are also rare with seminoma, whereas intra-abdominal extension along the gonadal vein has not been reported so far.
CT scan of abdomen and pelvis is usually indicated in testicular tumors for staging workup as it is more sensitive in detecting retroperitoneal, para-aortic, and mesenteric lymph nodes and also solid organ metastasis. In known lymphoma cases, it can detect other visceral organ infiltration or lymphoma deposits in abdomen.
PTL has a tendency to disseminate to other extra-nodal sites such as contralateral testes, central nervous system, lung, pleura, Waldeyer ring, skin, and soft tissues over the course of disease [3], [4]. However, continuous extension of the PTL along the spermatic cord and gonadal vein right up to the inferior vena cava in the absence of other deposits or manifestations is a very rare phenomenon. We have described 2 such cases in this article.
A similar single case has been reported in the literature by Scalcione et al. [5]. They have described similar positron emission tomography CT abdomen findings in a case of carcinoma prostate, which on orchiectomy was proven to be a second primary B cell lymphoma.
Chemotherapy and radiotherapy have well-established widely accepted role in the treatment of lymphoma and are associated with a good prognosis. However, orchiectomy is usually preferred in the initial management of suspected testicular lymphoma as it provides definite histopathology tissue diagnosis. In addition, testicular lymphomas are considered less responsive to chemotherapy because of blood testicular barrier preventing peak concentration of chemotherapeutic agent within testis.
Conclusion
We report 2 cases of PTL with extension along epididymis and spermatic cord into inguinal canal with further continuous extension along the gonadal vein up to inferior vena cava. These specific imaging findings are very rare and when present may help to differentiate testicular lymphoma from other testicular tumors on imaging.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
References
- 1.Freeman C., Berg J.W., Cutler S.J. Occurrence and prognosis of extranodal lymphomas. Cancer. 1972;29:252–260. doi: 10.1002/1097-0142(197201)29:1<252::aid-cncr2820290138>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 2.Shahab N., Doll D.C. Testicular lymphoma. Semin Oncol. 1999;26:259–269. [PubMed] [Google Scholar]
- 3.Zucca E., Conconi A., Mughal T.I., Sarris A.H., Seymour J.F., Vitolo U. Patterns of outcome and prognostic factors in primary large-cell lymphoma of the testis in a survey by the International Extranodal Lymphoma Study Group. J Clin Oncol. 2003;21:20–27. doi: 10.1200/JCO.2003.11.141. [DOI] [PubMed] [Google Scholar]
- 4.Fonseca R., Habermann T.M., Colgan J.P., O'Neill B.P., White W.L., Witzig T.E. Testicular lymphoma is associated with a high incidence of extranodal recurrence. Cancer. 2000;88:154–161. doi: 10.1002/(sici)1097-0142(20000101)88:1<154::aid-cncr21>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 5.Scalcione L.R., Katz D.S., Santoro M.S., Mahboob S., Badler R.L., Yung E.Y. Primary testicular lymphoma involving the spermatic cord and gonadal vein. Clin Nucl Med. 2009;34:222–223. doi: 10.1097/RLU.0b013e31819a20b5. [DOI] [PubMed] [Google Scholar]