Abstract
We report a rare case of ectopic pregnancy occurring in the scar of a previous caesarean section, diagnosed by ultrasonography and confirmed by 3.0-T magnetic resonance imaging of pelvis. We present the clinical details and imaging findings, followed by discussion of the etiology, pathogenesis, and imaging of this condition.
Keywords: Ectopic pregnancy, Caesarean section scar, USG, MRI
Introduction
Ectopic pregnancy is one of the leading causes of mortality among women of child-bearing age group. Most of these ectopic gestations are located in the fallopian tube, ampulla being the most common location. However, ectopic pregnancies are also known to occur in the cervix, ovary, previous cesarean scar, and abdomen. Intramural pregnancy with implantation in a previous caesarean section scar is probably the rarest location for ectopic pregnancy [1]. This type of pregnancy is prone for complications like uterine rupture, life-threatening hemorrhage, and hypovolemic shock [2], [3], [4].
The true incidence of pregnancy occurring in a uterine scar has not been determined because so few cases have been reported in the literature. However, the incidence of such cases seems to be on the rise [1], [5]. This may reflect both the increasing number of caesarean sections being performed and the more widespread use of the transvaginal scan that allows earlier detection of such pregnancies [4].
The diagnosis is usually made on ultrasonography and can be confirmed by magnetic resonance imaging (MRI) or during laparoscopy and/or laparotomy.
We present a case of ectopic pregnancy in caesarean section scar detected in an asymptomatic woman who had come for routine antenatal check up.
Case report
A 30-year-old woman had come for routine antenatal check up after 2 months of amenorrhea and positive urine pregnancy test. She was otherwise asymptomatic. She had history of 2 previous caesarean sections; first one performed 5 years back for intrapartum fetal distress and the second one preformed 2 years back due to complete placenta previa.
She was advised routine first trimester sonography.
Transabdominal sonography supplemented by transvaginal sonography revealed empty uterine cavity and empty cervical canal with a gestational sac in anterior myometrium of lower uterine segment (Fig. 1, Fig. 2, Fig. 3). The gestational sac had a fetal pole and yolk sac within, showing fetal cardiac activity (Fig. 4) and having average gestational age of 8 weeks 1 day. Anterior myometrium anterior to the gestational sac was thinned out. On Doppler examination, hyperechoic rim of choriodecidual reaction and umbilical cord shows vascularity.
Fig. 1.

Transabdominal sonography showing empty uterine cavity and empty cervical canal with a gestational sac in anterior myometrium of lower uterine segment. The gestational sac shows a fetal pole within. Anterior myometrium anterior to the gestational sac is thinned out.
Fig. 2.

Transabdominal sonography showing gestational sac in anterior myometrium of lower uterine segment, which shows a fetal pole (thick white arrow) within.
Fig. 3.
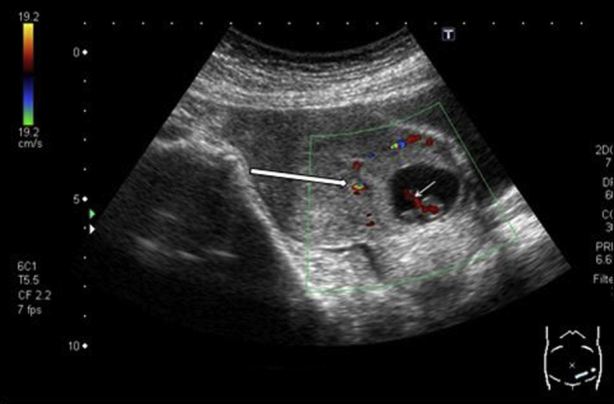
Color Doppler examination showing that hyperechoic rim of choriodecidual reaction (thick white arrow) and umbilical cord (thin white arrow) show vascularity.
Fig. 4.
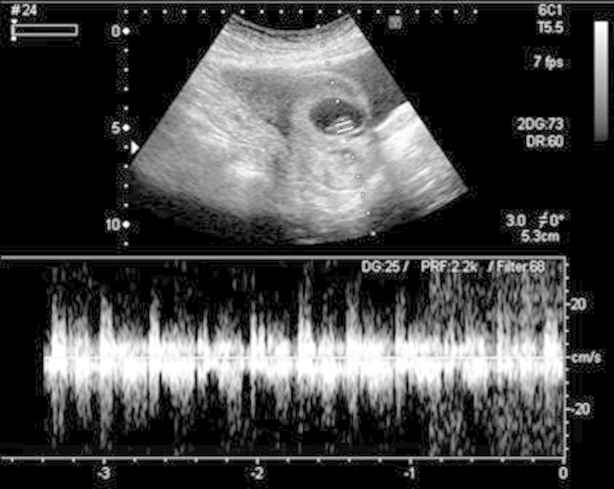
Spectral Doppler examination of the fetal pole demonstrating the presence of fetal cardiac activity.
MRI pelvis was performed in a 3.0-T MRI scanner (Philips Achieva). The study confirmed a gestational sac implanted within the anterior myometrium of the lower uterine segment in the region of the scar of previous cesarean section (Fig. 5). The gestational sac showed a well-formed T1 isointense and T2 hypointense fetal pole within and was surrounded by a well-appreciated decidual reaction (Fig. 6). Anterior myometrium anterior to the gestational sac was thinned out. Posteriorly, the gestational sac was seen extending into the endometrial cavity in the lower uterine segment. The posterior myometrium showed good wall thickness.
Fig. 5.
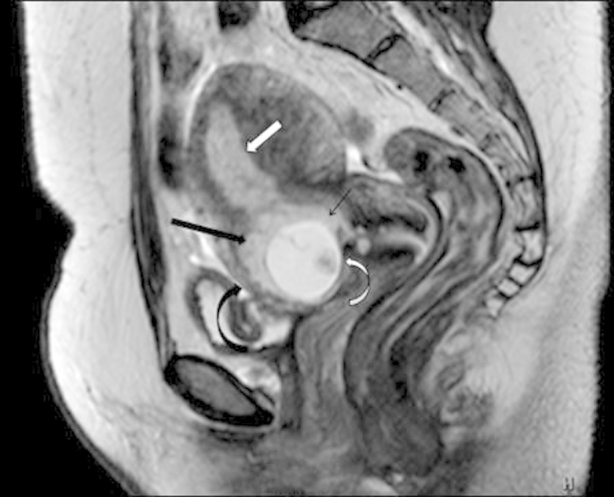
Sagittal T2-weighted imaging showing a gestational sac (curved white arrow) implanted within the anterior myometrium of the lower uterine segment in the region of the scar of previous cesarean section. The gestational sac shows a well-formed fetal pole within and is surrounded by a well-appreciated decidual reaction (thick black arrow). Anterior myometrium anterior to the gestational sac (curved black arrow) is thinned out. Posteriorly, the gestational sac is seen extending into the endometrial cavity in the lower uterine segment (thin black arrow). The posterior myometrium shows good wall thickness.
Fig. 6.
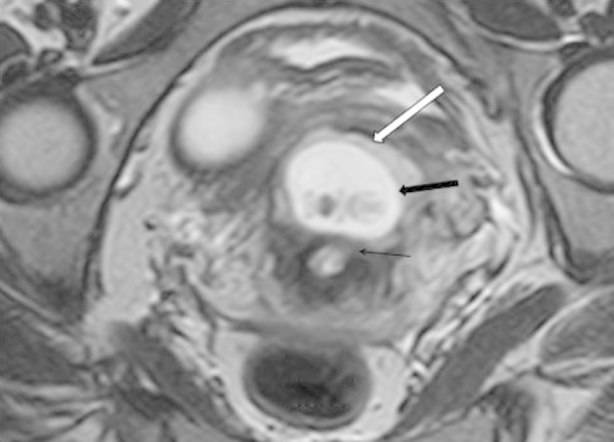
Axial T2-weighted imaging showing a gestational sac (thick black arrow) implanted within the anterior myometrium of the lower uterine segment. The gestational sac shows a well-formed fetal pole within and is surrounded by a well-appreciated decidual reaction (thick white arrow). A thin rim of myometrium (thin black arrow) between the gestational sac and endometrial cavity is noted. The posterior myometrium shows good wall thickness.
Because the patient already had 2 living issues, she went on to have a laparotomy and hysterectomy. She tolerated the procedure well and postprocedure follow-up serial ultrasound examinations of the pelvis showed no complications.
Discussion
There are many theories which explain the occurrence of intramural ectopic pregnancy. The most accepted theory seems to be that the blastocyst invades into the myometrium through a microscopic dehiscent tract, which may be the result of trauma of a previous caesarean section or any other uterine surgery [6] or even after manual removal of the placenta [3]. Another mechanism for intramural implantation may be in vitro fertilization and embryo transfer, even in the absence of any previous uterine surgery [7].
Vial et al. [8] proposed that there were 2 different types of such ectopic pregnancies. In the first type, after implantation of the gestational sac on the uterine scar, there is progression away from the serosal lining, either toward the cervicoisthmic space or toward the uterine cavity. Such a pregnancy may proceed to full term and a viable birth, but with an increased risk of life-threatening massive bleeding from the site of implantation [2]. The second type is a deep implantation into a uterine scar with progression towards the serosal surface. This culminates in rupture and bleeding during the first trimester of pregnancy. Some authors (Ghezzi et al.) [5] believe that the difference between those 2 types of pregnancy is of paramount importance. When there is a continuous connection to the uterine cavity, expectant management is justified because pregnancy may continue until a viable birth. In the latter type, if immediate treatment is not undertaken, the risk of late first-trimester uterine rupture and life-threatening bleeding is very high. According to Jurkovic et al. [4] in view of the lack of significant data, each woman should be given all the available information and the opportunity to decide on the management of her pregnancy. However, in a study done on 8 women diagnosed with caesarean scar ectopic pregnancy, of which 1 underwent expectant management, Maymon et al. [9] believed that the prognosis for an uneventful term pregnancy is still very poor.
Typically, the diagnosis is made based on ultrasound evaluation of the uterus and confirmed by MRI or during laparoscopy and/or laparotomy. Sonography combined with Doppler flow imaging has been advocated as a very reliable tool for detecting these cases, without the need for a pelvic MRI for confirmation [4], [9], [10].
Proposed ultrasound diagnostic criteria for diagnosis of an intramural ectopic gestation, with a differential diagnosis with cervical ectopic pregnancy are (1) a gestational sac located between the bladder wall and the anterior isthmic portion of the uterus; (2) no trophoblastic tissue visible in the uterine cavity and cervical canal; and (3) clearly visible circular blood flow surrounding the sac [8], [11], [12].
Two principal management options are available, the medical or the surgical. The medical or conservative treatment mainly consists of methotrexate, administered either systemically [13], [14], locally [4], or combined [10]. A caesarean scar ectopic pregnancy is surrounded by fibrous scar rather than by a normal vascularized decidual reaction. This also may potentially delay complete resorption of the pregnancy. Concomitant fine needle aspiration of the remaining fluid in the sac is often adopted [13]. Nevertheless, on rare occasions, rupture of the scar and heavy bleeding may occur after medical treatment [4]. The medical approach is sometimes combined with bilateral uterine artery embolization, minimizing risk of life-threatening hemorrhage [5].
A number of reports have supported the surgical alternative, even in the absence of active bleeding [1], [3], [15]. This consists of elective laparotomy and excision of the gestational mass. These authors have advocated that resection of the old scar with a new uterine closure can reduce the risk of recurrence. In addition, in the absence of complications, the follow-up period seems to be shorter compared with patients managed conservatively.
However, currently, no modality appears to be entirely reliable and none can guarantee uterine integrity [4], [16].
It is a recognized fact that a caesarean section is associated with a future risk for placental pathologies (eg, placenta previa, placental abruption, and placenta acccreta) and ectopic pregnancies. However, a caesarean scar pregnancy is considered to be even more aggressive than placenta previa or accreta because it invades the myometrium in the first trimester [17]. Patients who have undergone multiple caesarean sections appear to be at increased risk for in-scar implantation of the subsequent pregnancy because of increased scar surface area [4], [9].
With the advent of transvaginal sonography and with the use of saline infusion, it is possible to assess postcaesarean section uterine wall integrity even in the nonpregnant state [4], [12], [18]. Caesarean section scar defect is identified by the presence of fluid within the incision site [12] or any filling defect (“niche”), which is defined as a triangular anechoic structure at the presumed site of the scar [18].
Conclusion
Intramural pregnancy with implantation in a previous caesarean section scar is probably the rarest location for ectopic pregnancy. This type of pregnancy may become complicated with uterine rupture and life-threatening hemorrhage. Therefore, early diagnosis of caesarean scar ectopic gestation using sonography combined with Doppler flow imaging is of paramount importance, followed by confirmation of pelvic MRI if and when indicated. Although expectant management has been attempted in some cases, currently available data support termination of such a pregnancy once the correct diagnosis is made.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
References
- 1.Fylstra D.L., Pound-Chang T., Miller M.G., Cooper A., Miller K.M. Ectopic pregnancy within a Caesarian delivery scar: a case report. Am J Obstet Gyneco. 2002;187:302–304. doi: 10.1067/mob.2002.125998. [DOI] [PubMed] [Google Scholar]
- 2.Herman A., Weinraub Z., Avrech O., Maymon R., Ron-El R., Bukovsky Y. Follow up and outcome of isthmic pregnancy located in a previous caesarean section scar. Br J Obstet Gynecol. 1995;102:839–841. doi: 10.1111/j.1471-0528.1995.tb10855.x. [DOI] [PubMed] [Google Scholar]
- 3.Fylstra D.L. Ectopic pregnancy within a Caesarian scar: a review. Obstet Gynecol Surv. 2002;57:537–543. doi: 10.1097/00006254-200208000-00024. [DOI] [PubMed] [Google Scholar]
- 4.Jurkovic D., Hillaby K., Woelfer B., Lawrence A., Salim R., Elson C.J. First-trimester diagnosis and management of pregnancies implanted into the lower uterine segment Caesarian section scar. Ultrasound Obstet Gynecol. 2003;21:220–227. doi: 10.1002/uog.56. [DOI] [PubMed] [Google Scholar]
- 5.Ghezzi F., Lagana D., Franchi M., Fugazzola C., Bolis P. Conservative treatment by chemotherapy and uterine arteries embolization of a Caesarian scar pregnancy. Eur J Obstet Gynecol Reprod Biol. 2002;103:88–91. doi: 10.1016/s0301-2115(02)00003-9. [DOI] [PubMed] [Google Scholar]
- 6.Cheng P.J., Chueh H.Y., Soong Y.K. Sonographic diagnosis of a uterine defect in a pregnancy at 6 weeks gestation with a history of curettage. Ultrasound Obstet Gynecol. 2003;21:501–503. doi: 10.1002/uog.109. [DOI] [PubMed] [Google Scholar]
- 7.Hamilton C.J., Legarth J., Jaroudi K.A. Intramural pregnancy after in vitro fertilization and embryo transfer. Fertil Steril. 1992;57:215–217. doi: 10.1016/s0015-0282(16)54804-3. [DOI] [PubMed] [Google Scholar]
- 8.Vial Y., Petignat P., Hohlfeld P. Pregnancy in a Caesarian scar. Ultrasound Obstet Gynecol. 2000;16:592–593. doi: 10.1046/j.1469-0705.2000.00300-2.x. [DOI] [PubMed] [Google Scholar]
- 9.Maymon R., Halperin R., Mendlovic S., Schneider D., Vaknin Z., Herman A. Ectopic pregnancies in Caesarean section scars: the 8 year experience of one medical centre. Hum Reprod. 2004;19(2):278–284. doi: 10.1093/humrep/deh060. [DOI] [PubMed] [Google Scholar]
- 10.Nawroth F., Foth D., Wilhelm L., Schmidt T., Warm M., Romer T. Conservative treatment of ectopic pregnancy in a Caesarian section scar with methotrexate: a case report. Eur J Obstet Gynecol. 2001;99:135–137. doi: 10.1016/s0301-2115(01)00365-7. [DOI] [PubMed] [Google Scholar]
- 11.Sugawara J., Senoo M., Chisaka H., Yaegashi N., Okamura K. Successful conservative treatment of a cesarean scar pregnancy with uterine artery embolization. Tohoku J Exp Med. 2005;206:261–265. doi: 10.1620/tjem.206.261. [DOI] [PubMed] [Google Scholar]
- 12.Armstrong V., Hansen W.F., Van Voorhis B.J., Syrop C.H. Detection of Caesarian scars by transvaginal ultrasound. Obstet Gynecol. 2003;101:61–65. doi: 10.1016/s0029-7844(02)02450-x. [DOI] [PubMed] [Google Scholar]
- 13.Ravhon A., Ben-Chetrit A., Rabinowitz R., Neuman M., Beller U. Successful methotrexate treatment of a viable pregnancy within a thin uterine scar. Br J Obstet Gynecol. 1997;104:628–629. doi: 10.1111/j.1471-0528.1997.tb11547.x. [DOI] [PubMed] [Google Scholar]
- 14.Shufaro Y., Nadjari M. Implantation of a gestational sac in a Caesarian section scar. Fertil Steril. 2001;75:1217. doi: 10.1016/s0015-0282(01)01795-2. [DOI] [PubMed] [Google Scholar]
- 15.Rampen A. An ectopic pregnancy embedded in the myometrium of a previous Caesarian section scar. Acta Obstet Gynecol Scand. 1997;76:492. doi: 10.3109/00016349709047838. [DOI] [PubMed] [Google Scholar]
- 16.Lee C.L., Wang C.J., Chao A., Yen C.F., Soong Y.K. Laparoscopic management of an ectopic pregnancy in a previous caesarean section scar. Hum Reprod. 1999;14:1234–1236. doi: 10.1093/humrep/14.5.1234. [DOI] [PubMed] [Google Scholar]
- 17.Seow K.-M., Hwang J.-L., Tsai Y.-L. Ultrasound diagnosis of a pregnancy in a Caesarian section scar. Ultrasound Obstet Gynecol. 2001;18:547–551. doi: 10.1046/j.0960-7692.2001.00569.x. [DOI] [PubMed] [Google Scholar]
- 18.Monteagudo A., Carreno C., Timor-Tritsch I.E. Saline infusion sonohysterography in nonpregnant women with previous Caesarian delivery: the ‘niche’ in the scar. J Ultrasound Med. 2001;20:1105–1115. doi: 10.7863/jum.2001.20.10.1105. [DOI] [PubMed] [Google Scholar]


