Abstract
Background
Turner syndrome (TS) is the most common chromosomal abnormality in females and is associated with several co-morbidities. It commonly results from X monosomy which is diagnosed on a 30 cell karyotype. Congenital heart disease is a clinical feature in 30% of cases. It is becoming evident that TS patients have an increased risk of cardiovascular and cerebrovascular diseases.
Scope of review
This review provides a detailed overview of the literature surrounding cardiometabolic health in childhood and adolescent TS. In addition, the review also summarises the current data on the impact of growth hormone (GH) therapy on cardiometabolic risk in paediatric TS patients.
Major conclusions
Current epidemiological evidence suggests that young women and girls with TS have unfavourable cardiometabolic risk factors which predispose them to adverse cardiac and cerebrovascular outcomes in young adulthood. It remains unclear whether this risk is the result of unidentified factors which are intrinsic to TS, or whether modifiable risk factors (obesity, hypertension, hyperglycaemia) are contributing to this risk.
General significance
From a clinical perspective, this review highlights the importance of regular screening and pro-active management of cardiometabolic risk from childhood in TS cohorts and that future research should aim to address whether modification of these variables at a young age can alter the disease process and atherosclerotic outcomes in adulthood.
Abbreviations: ABPM, ambulatory blood pressure monitor; BMI, body-mass index; BP, blood pressure; BSA, body surface area; cIMT, carotid intima media thickness; DBP, diastolic blood pressure; DXA, dual energy X-ray scan; FM, fat mass; GH, growth hormone; HDLc, high density lipoprotein cholesterol; HOMA-IR, homeostatic model assessment-insulin resistance; ISSI-2, insulin secretion-sensitivity index-2; IVGTT, intravenous glucose tolerance test; LBM, lean body mass; LDLc, low density lipoprotein cholesterol; MetS, metabolic syndrome; MRI, magnetic resonance scanning; OGTT, oral glucose tolerance test; PAT, peripheral arterial tonometry; TS, Turner syndrome; T2DM, type 2 diabetes
Keywords: Turner syndrome, Paediatrics, Cardiometabolic risk, Glucose intolerance, Hypertension, Hyperlipidemia
Highlights
-
•
Increase in cardiovascular and cerebrovascular diseases in adult Turner syndrome
-
•
Cardiometabolic risk factors impact adult metabolic health and outcome.
-
•
Cardiometabolic risk factors in childhood Turner syndrome need careful assessment.
-
•
Future research should focus on early modification of these risk factors and outcome.
1. Introduction
Turner syndrome (TS) is the most common chromosomal abnormality in females, affecting 3% of all female foetuses [1] and occurring in 1:2500 live female births. It results from complete or partial X chromosome monosomy and is associated with a characteristic phenotype and comorbidities. Diagnosis requires the study of a minimum 30 cell karyotype [2]. Congenital cardiovascular disease affects 30% of patients with TS [3] however, it is becoming increasingly recognised that TS patients are at an increased risk of early acquired cardiovascular and cerebrovascular diseases and have a 2-fold risk of developing coronary artery disease [2], [4].
An established precursor to cardiovascular disease is atherosclerosis, which results from a multifactorial process through a combination of several modifiable (hypertension, hyperglycaemia, hyperlipidaemia and obesity) and non-modifiable (including age, gender and family history) risk factors. The process of atherosclerosis begins in early childhood and metabolic risk factors at age 9 years in healthy children can be predictive of subclinical atherosclerosis in adulthood [5]. The early stages of atherosclerosis are reversible and thus, early detection offers a theoretical window of opportunity to modify disease progression. Similarly, in TS, the atherosclerotic process starts early [6] and the epidemiological data suggests that there is an associated 3-fold risk of mortality from cardiovascular and cerebrovascular diseases [7], [8]. This review will discuss current data on cardiometabolic risk factors and acquired cardiovascular diseases in young girls with TS.
2. Cardiometabolic risk factors in Turner syndrome in childhood
2.1. Glucose metabolism
Approximately 35% of young girls with TS have abnormalities in carbohydrate metabolism and the frequency of impaired glucose metabolism varies with karyotype: mosaic TS patients have normal glucose tolerance compared to monosomy X patients [9]. Furthermore, type 2 diabetes mellitus (T2DM) is up to 4 times more common in TS patients [1] and the frequency of T2DM can vary according to karyotype: 43% in isochromosome Xq as compared with 9% in del Xq [9]. This suggests that haploinsufficiency of genes on Xp increases the impaired glucose metabolism and risk of T2DM and possibly impacts transcription factors involved in pancreatic islet and beta cell function [10].
The pathophysiology of impaired glucose tolerance in TS still remains unclear but there are several studies which attempt to elucidate the nature of the impairment. Adult women with TS have higher 2 h glucose levels and reduced measures of insulin secretion (HOMA-b and first phase insulin release) when compared to age matched controls, suggesting impaired insulin secretion [11]. However, studies demonstrating discrete reduction in insulin secretion following a glucose load in an IVGTT suggest a dysfunction in insulin secretion [12]. There is a study demonstrating higher fasting glucose and insulin levels (HOMA-S) using hyperinsulinemic–euglycemic clamps in 16 TS subjects, when compared to age- and body composition-matched controls, suggestive of decreased insulin sensitivity and lower whole body insulin sensitivity [13].
In paediatric TS cohorts, 34% of TS patients have impaired glucose tolerance on oral glucose tolerance testing (OGTT) as compared to 8% of controls but insulin sensitivity improves as the girls progress to 12–16 years of age [9]. Similar findings have been demonstrated in adolescents by using the IVGTT [14]. However, the reverse has also been demonstrated using the euglycaemic insulin clamp technique, where TS girls and adolescents have a significant reduction in insulin sensitivity and in non-oxidative glucose disposal compared to age-matched controls [15]. In a recent paediatric cross-sectional study evaluating cardiometabolic, 5/19 girls with TS and 0/17 controls had significantly impaired fasting glucose or impaired glucose tolerance on OGTT, and ISSI-2 (insulin secretion sensitivity index-2) was significantly lower in TS, suggesting a pancreatic beta cell dysfunction [16].
What is evident from these studies is that girls and women with TS are at increased risk of impaired glucose metabolism and T2DM and that the aetiology, though inconclusive, is multifactorial. Further, in TS, it appears that the processes of insulin secretion and sensitivity are dynamic at different ages of childhood, adolescence and adulthood. This maybe the result of small study numbers and varying age range as well as varied insulin methodologies used. Larger studies are clearly required and especially studies examining glucose metabolism in paediatric TS cohorts and its impact on cardiovascular risk in adulthood.
2.2. Body composition
Patients with TS have an altered body composition when compared to age-matched controls. This may be due to the fact that TS cohorts are on average 20 cm shorter but often have similar weights compared to controls resulting in an unfavourable body composition, with increased body mass index (BMI) and waist circumference [17], [18], [19], [20], [21]. However, it is evident from research methodologies, such as dual energy X-ray scan (DXA) and magnetic resonance scanning (MRI) that it is not just the shorter average height which places TS cohorts in an unfavourable body composition. DXA and MRI have demonstrated that adult TS cohorts have higher fat mass (FM) and lower lean body mass (LBM) with alterations in regional fat distribution (increased visceral FM, decreased truncal LBM and decreased skeletal muscle mass) [22], [23]. A concerning finding is that the paediatric data demonstrates similar trends. TS girls have higher waist circumference than age-matched and BMI-SDS-matched control [16] and given that visceral fat is metabolically active and contributes to the development of insulin resistance, T2DM and metabolic syndrome, this presents clinicians with an opportunity for early detection and intervention in TS girls.
2.3. Lipid abnormalities
There are data which suggest that lipid metabolism in TS cohorts is altered, with approximately 50% of TS patients over 21 years displaying hypercholesterolemia [24]. Total cholesterol and low density lipoprotein cholesterol (LDLc) are elevated in TS and a positive correlation exists between total cholesterol and LDLc levels and age [24], [25], [26]. Furthermore, low high density lipoprotein cholesterol (HDLc) levels occur in about 25% of adult TS women [1] and other studies show increased triglycerides in TS women [27]. These are all components of the metabolic syndrome.
In paediatric TS cohorts, higher total cholesterol, triglycerides and HDL cholesterol have been described [6], [28], [29]. Furthermore, there is a significant positive correlation between LDLc and carotid intima media (cIMT) thickness and a negative correlation between HDLc (r = 0.518, p < 0.01) and cIMT [6] suggesting that dyslipidaemia may be associated with atherosclerosis in children with TS. Ross et al. (1995) [52] has previously shown a positive correlation between serum cholesterol levels and age in TS girls (older than 11 years) and have suggested that this may be related to primary ovarian failure.
The exact cause for dyslipidaemia is unclear but theories exist such as foetal programming; where a negative correlation between birth weight and total cholesterol and triglycerides in TS has been demonstrated [30]. Gene dosage may also be important; where 45,XO monosomy displays significantly higher levels of triglycerides and LDLc as well as aberrations in LDLc and HDLc particle size, density and concentration [8]. Lipid particle size may also play a role, with smaller particle size in TS patients compared with karyotypically-matched controls [25].
In summary, the data suggest that dyslipidemia is prevalent in TS patients from childhood and that it may be dynamic with age and puberty. However, though the theories attempting to explain dyslipidaemia in TS are inconclusive, what is an emerging concern is that dyslipidaemia is evident in childhood and given that it is an established risk factor for acquired cardiovascular morbidity and mortality in adulthood. This is an area which requires constant clinical monitoring, as recommended by the current TS guidelines [1] as well as further research.
2.4. Hypertension
Girls with TS have an increased risk of hypertension in childhood and in adulthood, even after excluding TS patients with cardiac or renal defects. Approximately 50% of adults with TS have clinical hypertension [31]. Approximately, 1 in 4 young girls and 1 in 2 adult women with TS require anti-hypertensive treatment [4], [32]. Thirty percent of girls with TS are mildly hypertensive on 24 h ambulatory blood pressure monitor (ABPM) and 50% have abnormal diurnal blood pressure (BP) regulation [33], [34] with elevations in diastolic and systolic night/day ratios. This finding has been replicated in TS adult subjects [33]. These findings suggest that clinically detectable hypertension is preceded by a phase of dysregulation of normal BP which is detectable on ambulatory blood pressure monitoring.
Paediatric studies quote a wide range of prevalence of hypertension, from 7% [2] up to 40% [35], [2]. TS girls demonstrate higher systolic, diastolic and mean BP and resting heart rate [18] with a loss of the normal circadian rhythm of diastolic BP [36]. In one recent study of TS subjects aged 7–23 years, ambulatory blood pressure monitoring identified hypertension in 5/23 subjects, and 12/23 lacked the normal nocturnal dip in blood pressure. In the same study, conventional BP monitoring identified hypertension in only 1/5 patients [35]. These data suggest that 24 h ambulatory blood pressure monitoring might identify early hypertension, i.e. loss of the nocturnal dip in BP. Currently, however, ABPM is not considered a routine first line investigation for hypertension in individuals with TS who do not have underlying cardiovascular disease but there may be an argument to change this and begin to use ambulatory BP monitoring earlier in TS.
Hypertension is a well-established risk factor for atherosclerosis and hypertension confers a risk of end-organ damage in non-TS subjects. This applies to TS subjects also [33]. In TS, there is a negative correlation between dipping of the nocturnal diastolic blood pressure (DBP) and carotid intima media thickness (cIMT) (r = − 0.641, p = 0.000) [36], [33]. Thus, loss of the normal nocturnal dip in DBP is associated with increased arterial stiffness in children. Increased cIMT is a precursor of atherosclerotic plaque advancement and cardiovascular risk. Furthermore, endothelial dysfunction, an indicator of early atherosclerosis, has been demonstrated in BMI-matched TS paediatric cohorts (up to 8 years of age) using peripheral arterial tonometry (PAT) [29].
These data are confounded in TS subjects. For example, hypertension in TS correlates with increasing BMI [37] and BP measurements in TS are complicated by shorter height; so corrections for BMI, height and/or body surface area (BSA) have been suggested and should be considered [38].
In summary, hypertension is prevalent in TS subjects from childhood. It is associated with several poor cardiovascular outcomes in adulthood and can be detected in its earliest form as loss of nocturnal diastolic BP dip on ambulatory blood pressure monitoring. Hypertension in TS subjects begins in childhood and may be complicated by co-existing congenital heart or renal disease. However, it is detectable in its early stages. Hypertension is an important modifiable risk factor for aortic dissection [40], ischaemic heart disease and cerebrovascular disease. These data provides compelling evidence for early detection, regular monitoring and aggressive treatment of hypertension in girls with TS and perhaps consideration should be given to the use of ambulatory blood pressure monitoring early in the monitoring phase.
2.5. Metabolic syndrome
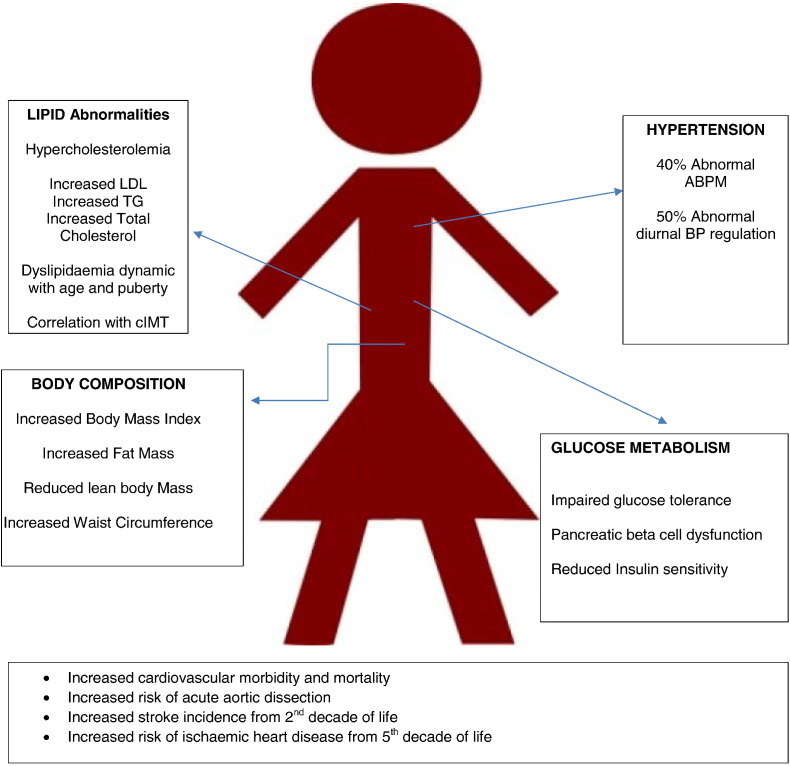
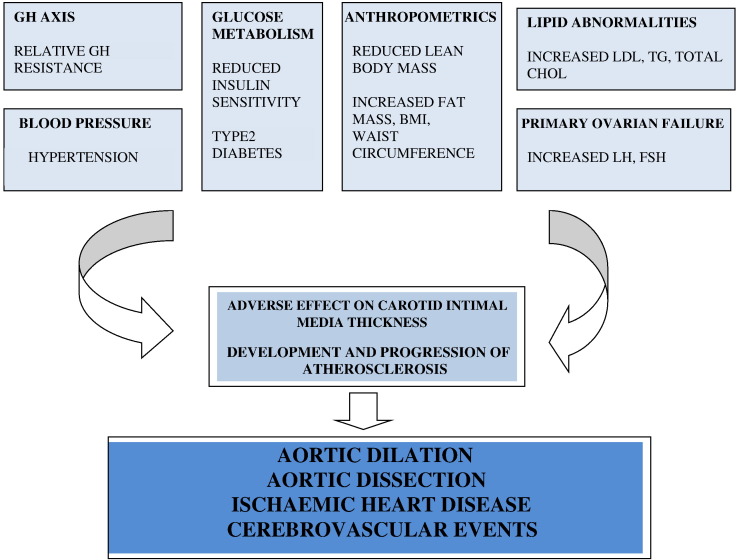
Metabolic syndrome (MetS) comprises a cluster of cardiovascular risk factors including hypertension, abdominal obesity, and impaired glucose metabolism, which confer an adverse cardiovascular outcome in adulthood. Though there is a lack of consistent diagnostic criteria for MetS there are a few proposed definitions [39]. Girls and adolescent women with TS also have adverse cardiometabolic profiles, placing them at increased risk of cardiovascular and cerebrovascular diseases. Interestingly, however, there are limited data on the prevalence of MetS in TS. A recent study [20] in an adult TS cohort of 85 patients reported a prevalence of 4.7% of MetS, using the International Diabetes Federation definition. Those with MetS included 12.5% obese and 4.3% non-obese. Data in paediatric TS cohorts are limited, but a recent study showed that 7/19 paediatric TS subjects met one criterion for MetS, 8/19 met two criteria however, and 0/19 were diagnosed with MetS [16]. Given that the data in the paediatric TS cohort are limited and knowing that the risk factors for MetS are prevalent in young girls with TS, future research must address questions about the impact of cardiometabolic risk factors in paediatric TS on adult cardiovascular outcome Refer to Figs. 1 and 2 for a detailed schematic of the interaction of the various cardiometabolic risk factors in Turner Syndrome.
Fig. 1.
Cardiometabolic and vascular risks in girls and adolescents with Turner syndrome.
Fig. 2.
Interaction of cardiovascular and metabolic risk factors in Turner syndrome.
3. Growth hormone treatment and cardiometabolic risk in Turner syndrome
Growth hormone (GH) is the primary growth-promoting treatment for short stature in TS. GH also has an impact on metabolic processes. Thus it is relevant to ascertain potential beneficial or adverse effects of GH therapy on metabolic risk factors in girls with TS.
3.1. The impact of GH treatment on glucose metabolism in TS
The effect of GH on glucose metabolism in TS has been extensively studied but the results are conflicting. Earlier randomised, placebo-controlled cross-over studies demonstrated that 2 months of GH treatment is associated with worsening insulin sensitivity, measured by HOMA-IR and composite insulin sensitivity index [40]. Conversely, studies of long-term treatment (4 years) with GH doses up to 8 IU/m2/day suggest that GH does not affect fasting glucose levels, but that it does increase fasting and post-prandial insulin levels however, these findings normalise within 6 months of discontinuing GH, suggesting a picture of transient insulin resistance [41], [42], [43]. In another study, GH treatment was associated with reduced insulin sensitivity by the QUICK-I method, but without an impaired response to an oral glycaemic load. Reassuringly, the reduced insulin sensitivity normalised within 12 months of cessation of GH treatment, again supporting the hypothesis of transient insulin resistance [43]. The decreased insulin sensitivity associated with GH therapy may vary with age, with less effects in TS subjects older than 12 years [44]. Additionally, increased BMI, which commonly exists in TS, may have a negative impact on insulin sensitivity [44]. Finally, it may be that the impact of GH on glucose metabolism may improve following cessation of the treatment [44]. Although the pathophysiology of impaired glucose sensitivity effects of GH in TS is unclear, the dysregulation appears to be reassuringly transient.
3.2. The impact of GH treatment on obesity and lipid metabolism in TS
The beneficial effect of GH on body composition has been demonstrated in cohorts other than TS [45]. GH has a positive impact on body composition in GH-treated TS cohorts: it leads to reduced total body fat, subcutaneous body fat and intra-abdominal fat, as quantified on DXA scan after 2 months of GH therapy [46], [40], increased lean body mass and reduced fat mass [47].
GH therapy also positively influences the metabolic profile by decreasing total cholesterol and reducing LDLc, while increasing HDLc and triglycerides [27]. However, these changes are evident in the first 4 years of GH therapy and might not be sustained on discontinuing treatment [27]. A similar observation has been demonstrated in paediatric TS cohorts [48]. Again, it would seem that GH has the potential for positive impact on body composition and lipid metabolism, but it is difficult to establish this with certainty in the absence of large longitudinal studies.
3.3. The impact of GH treatment on blood pressure
The studies examining the impact of GH on blood pressure control show conflicting data. In one study, diastolic BP was reduced significantly in a cohort of 39 GH-treated TS patients, and this BP reduction was sustained up to 5 years after discontinuing treatment [49]. However, when TS girls are treated with GH for up to 7 years with doses of 8 IU/m2/day, there does not appear to be a beneficial effect on blood pressure [50]. Further research is required to address these disparate results.
4. Conclusion
Current epidemiological evidence suggests that young women and girls with TS have unfavourable cardiometabolic risk factors which predispose them to adverse cardiac and cerebrovascular outcomes in young adulthood. The literature also describes adverse cardiovascular risk factors which place them at risk of developing the early stages of atherosclerosis, even in the paediatric age group. But what remains unclear is whether there are unidentified factors intrinsic to TS, which are also contributory to the cardiovascular risk or whether this is due to the adverse but modifiable risk factors (obesity, hyperglycaemia, hypertension and hyperlipidaemia) which are identified in childhood. The importance of regular screening and pro-active management of cardiometabolic risk from childhood in TS cohorts is clear. Future research should address whether modification of these variables at a young age can alter the disease process and atherosclerotic outcomes in adulthood, as well as to determine the potential risks and benefits of initiating specific therapies for factors such as obesity, hyperglycaemia, hypertension and hyperlipidaemia, at younger ages. Finally, from a clinical perspective, the foundation of delivering best practice care to girls and women with TS should include physician awareness of the cardiometabolic and vascular risks in TS.
Suggested screening of cardiometabolic risk factors in young girls and adult women with TS [51]
Adapted from Bondy (2007).
| •Annual blood pressure assessment –manual syphgmomanometer can be used –ABPM can be considered if clinically indicated |
| •Annual check of fasting blood glucose level |
| •Annual assessment of fasting lipids in older girls and adults |
Transparency documents
Transparency documents.
Footnotes
The Transparency documents associated with this article can be found, in the online version.
References
- 1.El Sheikh M., Conway G.S., Wass J.A.H.D.D.B. Turner's syndrome in adults. Endocr. Rev. 2002;23(1):120–140. doi: 10.1210/edrv.23.1.0457. [DOI] [PubMed] [Google Scholar]
- 2.Gravholt C.H. Epidemiological, endocrine and metabolic features in Turner syndrome. Eur. J. Endocrinol. 2004;151:657–687. doi: 10.1530/eje.0.1510657. [DOI] [PubMed] [Google Scholar]
- 3.Saenger P., COnway G.S., Davenport M. Recommendations for the diagnosis and management of Turner syndrome. J Clin Endocrinol Metab. 2001;86 doi: 10.1210/jcem.86.7.7683. [DOI] [PubMed] [Google Scholar]
- 4.Turtle E.J., Sule A.a., Bath L.E., Denvir M., Gebbie A., Mirsadraee S. Assessing and addressing cardiovascular risk in adults with Turner syndrome. Clin. Endocrinol. May, 2013;78(5):639–645. doi: 10.1111/cen.12104. ([Internet]. [cited 2014 Jun 8] Available from: http://www.ncbi.nlm.nih.gov/pubmed/23173989) [DOI] [PubMed] [Google Scholar]
- 5.Juonala M., Magnussen C.G., Venn A., Dwyer T., Burns T.L., Davis P.H. Influence of age on associations between childhood risk factors and carotid intima-media thickness in adulthood: the Cardiovascular Risk in Young Finns Study, The Childhood Determinants of Adult Health Study, The Bogalusa Heart Study, and The Muscatine St. Circulation. Dec 14 2010;122(24):2514–2520. doi: 10.1161/CIRCULATIONAHA.110.966465. ([Internet]. [cited 2014 Jun 9] Available from: http://www.ncbi.nlm.nih.gov/pubmed/21126976) [DOI] [PubMed] [Google Scholar]
- 6.Pirgon O., Atabek M.E., Oran B., Guclu R. Atherogenic lipid profile and systolic blood pressure are associated with carotid artery intima-media thickness in children with Turner syndrome. J Clin Res Pediatr Endocrinol. 2008;1(2):62–71. doi: 10.4008/jcrpe.v1i2.9. (2008/12/01 ed) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Czyzyk A.M.B. Cardiovascular and metabolic problems in Turner's syndrome patients. Arch Perinat Med. 2012;18(1):47–52. [Google Scholar]
- 8.Bondy C.A. Congenital cardiovascular disease in Turner syndrome. Congenit. Heart Dis. 2008;3:2–15. doi: 10.1111/j.1747-0803.2007.00163.x. [DOI] [PubMed] [Google Scholar]
- 9.Cicognani A., Mazzanti L., Tassinari D. Differences in carbohydrate metabolism in Turner syndrome dependince on age and karyotype. Pediatrics. 1988;12:1072–1080. doi: 10.1007/BF00441818. [DOI] [PubMed] [Google Scholar]
- 10.Hjerrild B.E., Holst J.J., Juhl C.B., Christiansen J.S., Schmitz O., Gravholt C.H. Delayed beta-cell response and glucose intolerance in young women with Turner syndrome. BMC Endocr. Disord. 2011;11:6. doi: 10.1186/1472-6823-11-6. (2011/03/17 ed) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bakalov V.K., Cooley M.M., Quon M.J., Luo M.L., Yanovski J.a., Nelson L.M. Impaired insulin secretion in the Turner metabolic syndrome. J Clin Endocrinol Metab. Jul 2004;89(7):3516–3520. doi: 10.1210/jc.2004-0122. ([Internet]. 2004/07/09 ed. [cited 2014 Apr 24] Available from: http://www.ncbi.nlm.nih.gov/pubmed/15240640) [DOI] [PubMed] [Google Scholar]
- 12.Hjerrild B.E., Holst J.J., Juhl C.B., Christiansen J.S., Schmitz O., Gravholt C.H. 2011/03/17 ed. BioMed Central Ltd; Jan 2011. Delayed β-Cell Response and Glucose Intolerance in Young Women With Turner Syndrome; p. 6. (BMC Endocr Disord). ([Internet]. [cited 2014 Apr 29] Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3068952&tool=pmcentrez&rendertype=abstract) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Salgin B., Yuen K., Williams R., Dunger D.A.R., Salgin B., Amin R., Yuen K., Williams R.M., Murgatroyd P. Insulin resistance is an intrinsic defect independent of fat mass in women with Turner's syndrome. Horm. Res. 2006;65(2):69–75. doi: 10.1159/000090907. (2006/01/13 Ed.) [DOI] [PubMed] [Google Scholar]
- 14.Gravholt C.H., Naeraa R.W., Nyholm B., Gerdes L.U., Christiansen E., Schmitz O. Glucose metabolism, lipid metabolism and cardiovascular risk factors in adult Turner's Syndrome: the impact of sex hormone replacement. Diabetes Care. Jul 1998;21(7):1062–1070. doi: 10.2337/diacare.21.7.1062. ([Internet]. [cited 2014 Feb 21] Available from: http://www.ncbi.nlm.nih.gov/pubmed/9653596) [DOI] [PubMed] [Google Scholar]
- 15.Caprio S., Boulware S., Diamond M., Sherwin R.S., Carpenter T.O., Rubin K. Insulin resistance: an early metabolic defect of Turner's syndrome. J Clin Endocrinol Metab. 1991;72(4):832–836. doi: 10.1210/jcem-72-4-832. (1991/04/01 Ed.) [DOI] [PubMed] [Google Scholar]
- 16.O'Gorman C.S., Syme C., Lang J., Bradley T.J., Wells G.D., Hamilton J.K. An evaluation of early cardiometabolic risk factors in children and adolescents with Turner syndrome. Clin. Endocrinol. Jun 2013;78(6):907–913. doi: 10.1111/cen.12079. ([Internet]. [cited 2014 Apr 24] Available from: http://www.ncbi.nlm.nih.gov/pubmed/23106295) [DOI] [PubMed] [Google Scholar]
- 17.Bondy C.A. Care of girls and women with Tuner syndrome: a guideline of the Turner Syndrome Study Group. J Clin Endocrinol Metab. 2007;92(1):10–35. doi: 10.1210/jc.2006-1374. [DOI] [PubMed] [Google Scholar]
- 18.Donaldson M.D.C., Gault E.J., Tan K.W., Dunger D.B. Optimising management in Turner syndrome: from infancy to adult transfer. Arch. Dis. Child. Jun 2006;91(6):513–520. doi: 10.1136/adc.2003.035907. ([Internet]. [cited 2014 Apr 9] Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=2082783&tool=pmcentrez&rendertype=abstract) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ryan S.A., Sullivan S.S.O. 2010. Process Review. [Google Scholar]
- 20.Calcaterra V., Brambilla P., Maffè G.C., Klersy C., Albertini R., Introzzi F. Metabolic syndrome in Turner syndrome and relation between body composition and clinical, genetic, and ultrasonographic characteristics. Metab. Syndr. Relat. Disord. Apr 2014;12(3):159–164. doi: 10.1089/met.2013.0075. ([Internet]. [cited 2014 Apr 29] Available from: http://www.ncbi.nlm.nih.gov/pubmed/24447068) [DOI] [PubMed] [Google Scholar]
- 21.Giordano R., Forno D., Lanfranco F., Manieri C., Ghizzoni L., Ghigo E. Metabolic and cardiovascular outcomes in a group of adult patients with Turner's syndrome under hormonal replacement therapy. Eur. J. Endocrinol. May 2011;164(5):819–826. doi: 10.1530/EJE-11-0002. ([Internet]. [cited 2014 Apr 24] Available from: http://www.ncbi.nlm.nih.gov/pubmed/21378088) [DOI] [PubMed] [Google Scholar]
- 22.Gravholt C.H., Hjerrild B.E., Mosekilde L. Body composition is distinctly altered in Turner syndrome: relations to glucose metabolism, circulating adipokines, and endothelial adhesion molecules. Eur. J. Endocrinol. 2006;155:583–592. doi: 10.1530/eje.1.02267. [DOI] [PubMed] [Google Scholar]
- 23.Ostberg J.E., Thomas E.L., Hamilton G., Attar M.J.H., Bell J.D., Conway G.S. Excess visceral and hepatic adipose tissue in Turner syndrome determined by magnetic resonance imaging: estrogen deficiency associated with hepatic adipose content. J Clin Endocrinol Metab. May 2005;90(5):2631–2635. doi: 10.1210/jc.2004-1939. ([Internet]. [cited 2014 Apr 24] Available from: http://www.ncbi.nlm.nih.gov/pubmed/15713713) [DOI] [PubMed] [Google Scholar]
- 24.Garden A.S., Diver M.J., Fraser W.D. Undiagnosed morbidity in adult women with Turner's syndrome. Clin. Endocrinol. Nov 1996;45(5):589–593. doi: 10.1046/j.1365-2265.1996.00849.x. ([Internet]. [cited 2014 Jun 16] Available from: http://www.ncbi.nlm.nih.gov/pubmed/8977756) [DOI] [PubMed] [Google Scholar]
- 25.Van P.L., Bakalov V.K., Bondy C.A. Monosomy for the X-chromosome is associated with an atherogenic lipid profile. J Clin Endocrinol Metab. Aug 2006;91(8):2867–2870. doi: 10.1210/jc.2006-0503. (Available from: http://www.ncbi.nlm.nih.gov/pubmed/16705071) [DOI] [PubMed] [Google Scholar]
- 26.De Armani M.C.A., Baldin A.D., Lemos-Marini S.H.V., Baptista M.T.M., Maciel-Guerra A.T., Guerra-Junior G. Evaluation of insulin resistance and lipid profile in Turner syndrome. Arq Bras Endocrinol Metab. Apr 2005;49(2):278–285. doi: 10.1590/s0004-27302005000200015. ([Internet]. 2005/09/27 ed. [cited 2014 Apr 29] Available from: http://www.ncbi.nlm.nih.gov/pubmed/16184257) [DOI] [PubMed] [Google Scholar]
- 27.Elsheikh M., Conway G.S. The impact of obesity on cardiovascular risk factors in Turner's syndrome. Clin. Endocrinol. Oct 1998;49(4):447–450. doi: 10.1046/j.1365-2265.1998.00552.x. ([Internet]. [cited 2014 Apr 29] Available from: http://www.ncbi.nlm.nih.gov/pubmed/9876341) [DOI] [PubMed] [Google Scholar]
- 28.O'Gorman C.S., Syme C., Lang J., Bradley T., Wells G., Hamilton J. An evaluation of early cardiometabolic risk factors in children and adolescents with Turner syndrome. Clin. Endocrinol. 2012 doi: 10.1111/cen.12079. ([Internet]. 2012/10/31 ed. Available from: http://onlinelibrary.wiley.com/doi/10.1111/cen.12079/abstract?systemMessage=Wiley+Online+Library+will+be+disrupted+on+15+December+from+10:00-13:00+GMT+(05:00-08:00+EST)+for+essential+maintenance) [DOI] [PubMed] [Google Scholar]
- 29.O'Gorman C.S., Syme C., Bradley T., Hamilton J., Mahmud F.H. 2012/04/05 ed. BioMed Central Ltd; Jan 2012. Impaired Endothelial Function in Pediatric Patients With Turner Syndrome and Healthy Controls: A Case–Control Study; p. 5. (Int J Pediatr Endocrinol). ([Internet]. [cited 2014 Apr 24] Available from: http://www.ijpeonline.com/content/pdf/1687-9856-2012-5.pdf) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Baldin A.D., Siviero-Miachon A.A., Fabbri T., de Lemos-Marini S.H.V., Spinola-Castro A.M., Baptista M.T.M. Turner syndrome and metabolic derangements: another example of fetal programming. Early Hum. Dev. Feb 2012;88(2):99–102. doi: 10.1016/j.earlhumdev.2011.07.014. ([Internet]. 2011/08/02 ed [cited 2014 Apr 24] Available from: http://www.ncbi.nlm.nih.gov/pubmed/21802870) [DOI] [PubMed] [Google Scholar]
- 31.Elsheikh M., Casadei B., Conway G.S., Wass J.A. Hypertension is a major risk factor for aortic root dilatation in women with Turner's syndrome. Clin. Endocrinol. Jan 2001;54(1):69–73. doi: 10.1046/j.1365-2265.2001.01154.x. ([Internet]. 2001/02/13 ed [cited 2014 Apr 29] Available from: http://www.ncbi.nlm.nih.gov/pubmed/11167928) [DOI] [PubMed] [Google Scholar]
- 32.Turner — know your body!
- 33.Nathwani N.C., Unwin R., Brook C.G., Hindmarsh P.C. Blood pressure and Turner syndrome. Clin. Endocrinol. Mar 2000;52(3):371–377. doi: 10.1046/j.1365-2265.2000.00961.x. ([Internet]. 2000/03/16 ed [cited 2014 Apr 29] Available from: http://www.ncbi.nlm.nih.gov/pubmed/10718835) [DOI] [PubMed] [Google Scholar]
- 34.Nathwani N.C., Unwin R., Brook C.G., Hindmarsh P.C. The influence of renal and cardiovascular abnormalities on blood pressure in Turner syndrome. Clin. Endocrinol. 2000;52(3):371–377. doi: 10.1046/j.1365-2265.2000.00961.x. (2000/03/16 ed) [DOI] [PubMed] [Google Scholar]
- 35.Fudge E.B., Constantacos C., Fudge J.C., Davenport M. Improving detection of hypertension in girls with Turner syndrome using ambulatory blood pressure monitoring. Horm Res pædiatrics. Jan 2014;81(1):25–31. doi: 10.1159/000355510. ([Internet]. [cited 2014 Jun 4] Available from: http://www.ncbi.nlm.nih.gov/pubmed/24281046) [DOI] [PubMed] [Google Scholar]
- 36.Akyürek N., Atabek M.E., Eklioglu B.S., Alp H. Ambulatory blood pressure and subclinical cardiovascular disease in children with turner syndrome. Pediatr. Cardiol. Jan 23 2014;35(1):57–62. doi: 10.1007/s00246-013-0740-2. ([Internet]. [cited 2013 Sep 7] Available from: http://www.ncbi.nlm.nih.gov/pubmed/23794013) [DOI] [PubMed] [Google Scholar]
- 37.Elsheikh M., Conway G.S. The impact of obesity on cardiovascular risk factors in Turner’ s syndrome. 2000;44(1998):447–450. doi: 10.1046/j.1365-2265.1998.00552.x. [DOI] [PubMed] [Google Scholar]
- 38.Baguet J.-P.P., Douchin S., Pierre H., a-MM R., Bost M., J-MM M. Structural and functional abnormalities of large arteries in the Turner syndrome. Heart. Nov 2005;91(11):1442–1446. doi: 10.1136/hrt.2004.048371. ([Internet]. 2005/03/12 ed. [cited 2014 Apr 24] Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1769156&tool=pmcentrez&rendertype=abstract) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Weiss R., Bremer A.a., Lustig R.H. What is metabolic syndrome, and why are children getting it? Ann. N. Y. Acad. Sci. Apr 2013;1281:123–140. doi: 10.1111/nyas.12030. ([Internet]. [cited 2014 Jan 27] Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3715098&tool=pmcentrez&rendertype=abstract) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gravholt C.H., Naeraa R.W., Brixen K., Kastrup K.W., Mosekilde L., Jorgensen J.O. Short-term growth hormone treatment in girls with Turner syndrome decreases fat mass and insulin sensitivity: a randomized, double-blind, placebo-controlled, crossover study. Pediatrics. 2002;110(5):889–896. doi: 10.1542/peds.110.5.889. (2002/11/05 ed) [DOI] [PubMed] [Google Scholar]
- 41.Sas T.C., de Muinck Keizer-Schrama S.M., Stijnen T., Aanstoot H.J., Drop S.L. Carbohydrate metabolism during long-term growth hormone (GH) treatment and after discontinuation of GH treatment in girls with Turner syndrome participating in a randomized dose–response study. Dutch Advisory Group on Growth Hormone. J Clin Endocrinol Metab. Mar 2000;85(2):769–775. doi: 10.1210/jcem.85.2.6334. ([Internet]. 2000/02/26 ed [cited 2014 Apr 30] Available from: http://www.ncbi.nlm.nih.gov/pubmed/10690889) [DOI] [PubMed] [Google Scholar]
- 42.Sas T., de Muinck K.-S.S., Aanstoot H.J., Stijnen T., Drop S. Carbohydrate metabolism during growth hormone treatment and after discontinuation of growth hormone treatment in girls with Turner syndrome treated with once or twice daily growth hormone injections. Clin. Endocrinol. 2000;52(6):741–747. doi: 10.1046/j.1365-2265.2000.01007.x. (2000/06/10 ed) [DOI] [PubMed] [Google Scholar]
- 43.Radetti G., Pasquino B., Gottardi E., Boscolo Contadin I., Aimaretti G., Rigon F. Insulin sensitivity in Turner's syndrome: influence of GH treatment. Eur. J. Endocrinol. 2004;151(3):351–354. doi: 10.1530/eje.0.1510351. (2004/09/15 ed) [DOI] [PubMed] [Google Scholar]
- 44.Mazzanti L., Bergamaschi R., Castiglioni L., Zappulla F., Pirazzoli P., Cicognani A. Turner syndrome, insulin sensitivity and growth hormone treatment. Horm. Res. 2005;64(Suppl. 3):51–57. doi: 10.1159/000089318. (2006/01/28 ed) [DOI] [PubMed] [Google Scholar]
- 45.Bridges N. What is the value of growth hormone therapy in Prader Willi syndrome? Arch. Dis. Child. Feb 2014;99(2):166–170. doi: 10.1136/archdischild-2013-303760. ([Internet]. [cited 2014 Jun 26] Available from: http://www.ncbi.nlm.nih.gov/pubmed/24162007) [DOI] [PubMed] [Google Scholar]
- 46.Wooten N., Bakalov V.K., Hill S., Bondy C.A. Reduced abdominal adiposity and improved glucose tolerance in growth hormone-treated girls with Turner syndrome. J Clin Endocrinol Metab. Jun 2008;93(6):2109–2114. doi: 10.1210/jc.2007-2266. ([Internet]. 2008/03/20 ed [cited 2014 Apr 24] Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=2435647&tool=pmcentrez&rendertype=abstract) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ari M., Bakalov V.K., Hill S., Bondy C.a. The effects of growth hormone treatment on bone mineral density and body composition in girls with Turner syndrome. J Clin Endocrinol Metab. Nov 2006;91(11):4302–4305. doi: 10.1210/jc.2006-1351. ([Internet] [cited 2014 Apr 24] Available from: http://www.ncbi.nlm.nih.gov/pubmed/16940444) [DOI] [PubMed] [Google Scholar]
- 48.Kohno H., Igarashi Y., Ozono K., Ohyama K., Ogawa M., Osada H. Favorable impact of growth hormone treatment on cholesterol levels in Turner syndrome. Clin Pediatr Endocrinol case reports Clin Investig Off J Japanese Soc Pediatr Endocrinol. Apr 2012;21(2):29–34. doi: 10.1297/cpe.21.29. ([Internet] [cited 2014 Apr 30] Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3698903&tool=pmcentrez&rendertype=abstract) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bannink E.M., van der Palen R.L., Mulder P.G., de Muinck Keizer-Schrama S.M. Long-term follow-up of GH-treated girls with Turner syndrome: BMI, blood pressure, body proportions. Horm. Res. 2009;71(6):336–342. doi: 10.1159/000223418. (2009/06/10 ed) [DOI] [PubMed] [Google Scholar]
- 50.Sas T.C., Cromme-Dijkhuis A.H., de Muinck Keizer-Schrama S.M., Stijnen T., van Teunenbroek A., Drop S.L. The effects of long-term growth hormone treatment on cardiac left ventricular dimensions and blood pressure in girls with Turner's syndrome. Dutch Working Group on Growth Hormone. J. Pediatr. Oct 1999;135(4):470–476. doi: 10.1016/s0022-3476(99)70170-8. ([Internet] [cited 2014 Apr 30] Available from: http://www.ncbi.nlm.nih.gov/pubmed/10518081) [DOI] [PubMed] [Google Scholar]
- 51.Bondy C.A. Care of girls and women with Turner syndrome: a guideline of the Turner Syndrome Study Group. J Clin Endocrinol Metab. Jan 2007;92(1):10–25. doi: 10.1210/jc.2006-1374. ([Internet] [cited 2014 Mar 23 ] Available from: http://www.ncbi.nlm.nih.gov/pubmed/17047017) [DOI] [PubMed] [Google Scholar]
- 52.Ross J.L., Feuillan P., Long L.M., Kowal K., Kushner H., Cutler G.B. Lipid Abnormalities in Turner Syndrome. J. Pediatr. 1995;126(2):242–245. doi: 10.1016/s0022-3476(95)70551-1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Transparency documents.