Abstract
Evaluation of articular cartilage and subchondral bone is essential in the diagnosis of joint diseases and injuries. Interobserver and intraobserver reproducibilities of arthroscopic grading are only poor to moderate. Thus, for quantitative and objective evaluation of cartilage and subchondral bone, ultrasound arthroscopy (UA) has been introduced to clarify this dilemma. Assessment of the clinical feasibility of high-frequency ultrasonography (US) during 6 knee arthroscopies was conducted, and the surgical technique is presented. US imaging was conducted with a flexible 9-MHz US catheter inserted into the joint through conventional portals. US and arthroscopy videos were synchronously recorded, and US parameters for cartilage and subchondral bone characteristics were measured. Arthroscopy and US imaging were combined to perform cartilage grading. UA produced quantitative data on lesion size, as well as cartilage quality, and showed subchondral bone changes. Visualization of an osteochondritis dissecans lesion not detected by conventional arthroscopy and US-guided retrograde drilling were possible with UA. To conclude, UA proved to be clinically feasible and aided in the diagnosis when assessing knee osteochondral lesions.
Evaluation of articular cartilage and subchondral bone is essential in the diagnosis of joint diseases and injuries. Currently, diagnosis is based on clinical history, examination findings, radiographic imaging, and magnetic resonance imaging. Diagnosis of cartilage lesions should be immediate, sensitive, and reproducible to optimize treatment and prevent trauma-initiated osteoarthritis. Unfortunately, chondral lesions can sometimes be overlooked by magnetic resonance imaging because of suboptimal resolution, sensitivity, and accuracy.1 Nonetheless, nontraumatic joint diseases such as osteochondritis dissecans (OCD) are reported to cause major knee-related morbidity, especially among adolescents and young adults.
Numerous surgical techniques have been described for repair of chondral lesions.2 Accurate evaluation, grading, and delineation of a chondral lesion relative to subchondral bone are essential when selecting the appropriate cartilage repair technique.
Arthroscopic assessment of chondral injuries and stability of OCD is challenging,3 and the interobserver and intraobserver reproducibilities of grading of cartilage lesions have been reported to be poor, especially in the differentiation of intact International Cartilage Repair Society (ICRS) grade 0 cartilage from softened ICRS grade 1 cartilage, as well as the differentiation of ICRS grade 2 lesions from ICRS grade 3 lesions.4 An apparent need for more objective and quantitative arthroscopic methods has been identified.5
Several cartilage measurement instruments, such as external ultrasonography (US), arthroscopic indentation techniques, and optical coherence tomography, have been introduced. Quantitative US is reported to detect an increase in articular cartilage surface roughness, degradation of superficial collagen, changes in subchondral bone mineralization, and cartilage healing after surgical repair.6 Importantly, this technique has already been applied in human knee arthroscopies.7, 8 Ultrasound arthroscopy (UA) is a quantitative imaging technique that enables simultaneous visualization of cartilage and subchondral bone. The US device applied in our previous and present studies is approved by the Food and Drug Administration for human cardiographic imaging. Assessment of the clinical feasibility of high-frequency US during 6 knee arthroscopies (Table 1) was conducted, and the surgical technique is presented.
Table 1.
Demographic Data of Knee Ultrasound Arthroscopy Patients
| Gender | Age at Diagnosis, yr | Age at Surgery, yr | Preoperative Lysholm Knee Score | Affected Knee | Open Growth Plates | Extent of Lesion on MRI, cm2 | Location of Lesion | Diagnosis | MRI Grade | Ultrasound Arthroscopy Grade |
|---|---|---|---|---|---|---|---|---|---|---|
| Female | 25 | 25.2 | — | Right | No | 0.76 | LFC | OCD | ICRS OCD grade 4 | ICRS OCD grade 4 |
| Male | 16.4 | 28.1 | 80 | Right | No | 3.30 | MFC | OCD | ICRS OCD grade 3 | ICRS OCD grade 3 |
| Male | 24.1 | 24.4 | 71 | Left | No | 0.17 | MFC | Post-traumatic OA, meniscus defect | ICRS grade 3 | ICRS grade 3 |
| Male | 37.9 | 38 | 72 | Right | No | 0.43 | Patella | Patellofemoral OA | ICRS grade 1 | ICRS grade 2 |
| Male | 12.8 | 16.3 | 45 | Right | Yes | 1.79 | LFC | OCD | ICRS OCD grade 2 | ICRS OCD grade 2 |
| Male | 10.7 | 11.4 | 51 | Left | Yes | 0.40 | Both condyles | OCD | ICRS OCD grade 2 | ICRS OCD grade 2 |
ICRS, International Cartilage Repair Society; LFC, lateral femoral condyle; MFC, medial femoral condyle; MRI, magnetic resonance imaging; OA, osteoarthritis; OCD, osteochondritis dissecans.
Surgical Technique
A standard knee arthroscopy setup is used. The patient is placed supine with the hip flexed at about 50° and knee flexed at about 100°. A thigh tourniquet is recommended but not mandatory. We prefer a straight operating table with a side post and footrest. Both spinal and general anesthesia can be used. In addition, a US imaging device with a separate monitor, placed near the arthroscopy monitor, is needed, making it possible to follow both monitors. Conventional portals (anterolateral and anteromedial) are prepared in the usual way. The arthroscope is inserted through the anterolateral portal, and diagnostic arthroscopy is performed. Additional portal placement (superolateral, superomedial, posterolateral, or posteromedial) can be used when needed for the UA. Encountered osteochondral pathology is classified according to the ICRS guidelines.1, 8 A sterile US imaging catheter is prepared for injection of sterile saline solution with a needle into the tip of the 2.8-mm-diameter flexible 9-MHz US catheter (Boston Scientific, Marlborough, MA). The US device is activated and inserted into the knee joint manually through the arthroscopy portal and guided within the joint by an arthroscopic half-pipe instrument (Fig 1). The narrow and flexible catheter can be guided to reach every region in the knee joint. Because of the brittle construction of the US catheter, forceful manipulation or pushing toward an area of resistance needs to be avoided. Similarly, excessive bending of the catheter can cause disturbances in the US imaging. US and arthroscopy can be synchronously recorded. To optimize visualization, the US reflection is maximized by manually adjusting the probe perpendicular to the lesion surface. In addition to high-resolution real-time imaging, the US reflection coefficient (R), integrated reflection coefficient (IRC), and ultrasound roughness index (URI) are recorded for the cartilage and subchondral bone in normal and pathologic sites of the knee (Fig 1, Fig 2, Fig 3, Fig 4). Treatment modalities for each defect are chosen by combining data from visual inspection, mechanical probing, and US characteristics.
Fig 1.
(A, B) The characteristic subchondral separation (oval) encountered in osteochondritis dissecans lesions can be visualized with ultrasound arthroscopy as gaps of otherwise intact subchondral bone signal. (C, D) Furthermore, if ultrasound arthroscopy shows fluid beneath the cartilage surface, an unstable osteochondritis dissecans can be suspected. (f, fluid; F, femur; IRC, integrated reflection coefficient [decibels]; m, meniscus; R, ultrasound reflection coefficient [percent]; s, arthroscope artifact; sb, subchondral bone; Ti, tibia; URI, ultrasound roughness index [micrometers]).
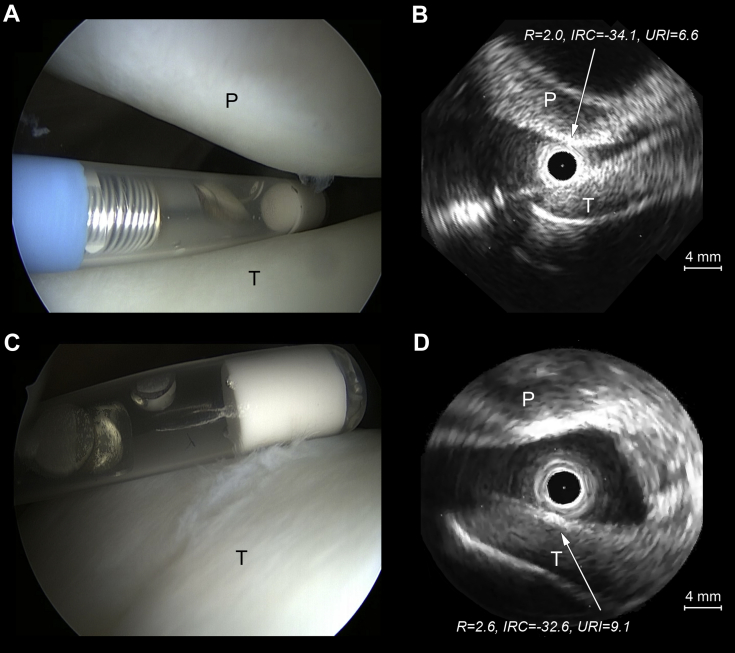
Fig 2.
Still ultrasound arthroscopy images showing (A, B) normal International Cartilage Repair Society (ICRS) grade 0 cartilage and (C, D) nearly normal ICRS grade 1 cartilage. Both surfaces produce similar ultrasound reflection (ultrasound reflection coefficient [R], as a percent). However, the ultrasound roughness index (URI) (in micrometers) is elevated for ICRS grade 1 compared with ICRS grade 0 articular cartilage, as clearly seen in the (A, C) corresponding arthroscopy images. (IRC, integrated reflection coefficient [decibels]; P, patella; T, trochlea.)
Fig 3.
Still ultrasound arthroscopy images showing a decrease in ultrasound reflection (ultrasound reflection coefficient [R], as a percent, and integrated reflection coefficient [IRC], in decibels) and a respective increase in ultrasound roughness index (URI) (in micrometers) with progressive cartilage degradation, as seen in (A, B) abnormal patellar International Cartilage Repair Society grade 2 and (C, D) severely abnormal femoral International Cartilage Repair Society grade 3 lesions compared with normal cartilage (Fig 2). (D) Concomitant meniscus pathology (encircled in red) can be visualized by ultrasound. (F, femur; m, meniscus; P, patella; T, trochlea; Ti, tibia.)
Fig 4.
(A, B) Ultrasound arthroscopy shows high reflection and intermediate roughness values for exposed sclerotic subchondral bone. (C, D) Other subchondral bone changes such as microfracture picking holes (mf) can also be visualized by ultrasound arthroscopy. (F, femur; IRC, integrated reflection coefficient [decibels]; R, ultrasound reflection coefficient [percent], sb, subchondral bone; Ti, tibia; URI, ultrasound roughness index [micrometers].)
UA enables quantitative measurement of cartilage lesion depth relative to cartilage thickness, offering more information for the ICRS grading (Fig 1, Fig 2, Fig 3, Fig 4). Normal (ICRS grade 0) and nearly normal (ICRS grade 1) cartilage showed similar reflection values (R and IRC), providing no additional information for the ICRS grading. However, the URI was elevated in ICRS grade 1 cartilage (Fig 2). A decrease in US reflection (R) was noted between abnormal (ICRS grade 2) and severely abnormal (ICRS grade 3) cartilage (Fig 3). On the other hand, the URI was increased in abnormal cartilage (ICRS grade 2 to 3) compared with normal or mildly deteriorated (ICRS grade 0 to 1) cartilage. High US reflection (R) was seen in ICRS OCD grade 4 lesions with exposed sclerotic bone on the bottom of the defect. After debridement and microfracture treatment, picking holes could be visualized by US (Fig 4). Moreover, UA enables detection of osteochondral lesions as well as measurement of their dimensions. UA is able to detect an OCD lesion with intact articular cartilage (patients 5 and 6) (Fig 1, Video 1). In addition, UA can show fluid between the bone-cartilage interface, indicating an unstable OCD lesion necessitating surgical intervention (Fig 1, Video 1). Even with a breached and lacerated cartilage surface, US allows simultaneous visualization of deeper structures reaching the subchondral bone. Furthermore, UA enables the evaluation of meniscal pathology (Fig 3). US-guided retrograde drilling of ICRS OCD grade 2 lesions is also possible (Video 1). US enables accurate evaluation of depth and progression of the drilling, avoiding cartilage surface perforation. The use of fluoroscopy can be minimized.
Discussion
UA enables imaging and accurate measurements of chondral and osteochondral lesion size and depth, as well as quantitative acoustic morphology characteristics of cartilage (R, IRC, URI). Reaching every region in the knee joint is achievable by UA. Thus UA has proved to be a useful adjunct when assessing and treating knee osteochondral lesions.
Although US imaging was primarily used to confirm the grades obtained by conventional arthroscopy, UA led to a change in the ICRS grade in 1 of 6 patients, in whom an ICRS OCD grade 2 lesion would have been missed by conventional means. The ability of conventional arthroscopy to differentiate ICRS grade 0 from grade 1 lesions and ICRS grade 2 from grade 3 lesions can be challenging. Unfortunately, the obtained US parameters did not help in the differentiation between these ICRS grades. Nevertheless, the differentiation of these groups was possible based on the US images. This observation is supported by a recent report showing a significant effect of arthroscopic US imaging on clinical cartilage grading.8 However, the interpretation of the UA images was not blinded, which probably composes a potential bias in the interpretation of the UA images. No statistically significant variation in the measured US parameters between lesions of different severity was found. This is because of the limited number of patients with variable cartilage conditions.
Nonetheless, UA provides advantages compared with existing techniques used in knee cartilage evaluation and treatment (Table 2). Conventional arthroscopy enables an evaluation of the superficial cartilage by visual and probing characteristics but yields no quantitative data. Furthermore, external US of the knee is suitable only in limited areas, requiring an experienced examiner.9
Table 2.
Advantages, Limitations, and Risks of Ultrasound Arthroscopy
| Advantages |
| Comprehensive accessibility |
| Quantitative cartilage measurements (e.g., cartilage thickness, lesion depth and size, US characteristics) |
| Accurate cartilage lesion evaluation |
| Accurate osteochondral lesion evaluation (e.g., intraoperative OCD stability assessment) |
| Radiation-free intraoperative monitoring (e.g., cartilage, menisci, subchondral bone) |
| Possibility for US-guided procedures (e.g., retrograde OCD drilling) |
| Limitations and risks |
| Not yet validated for cartilage injury classification |
| Costs (US catheter, measurement device) |
| Marginally prolonged operating time (5-15 min) |
OCD, osteochondritis dissecans; US, ultrasonography.
To conclude, UA was found to be readily applicable and diagnostically valuable when evaluating the integrity of knee articular cartilage. Cartilage thickness and quality may be quantitatively assessed, providing objective information on the location and extent of lesions. Furthermore, the stability and characteristics of OCD lesions can be evaluated with UA. US visualization of retrograde drilling in OCD treatment is also possible, and thus the use of fluoroscopy can be minimized. However, further basic and clinical research on this topic is warranted. We expect that UA might be a useful adjunct for arthroscopic surgeons in the future.
Acknowledgment
The authors acknowledge Kari Vanamo, M.D., Ph.D., at Kuopio University Hospital.
Footnotes
The authors report the following potential conflict of interest or source of funding: P.P. receives support from a grant for Ph.D. thesis work from the Foundation for Pediatric Research. T.V., J.S.J., and J.T. receive support from strategic funding of the University of Eastern Finland, Kuopio University Hospital (EVO grants 5041723 and 5041716); Academy of Finland (project 132367 and 267551, University of Eastern Finland); and the Spear Head Research project (Interdisciplinary, Translational Research for Improved Diagnosis and Treatment of Musculoskeletal Diseases–Musculoskeletal Research Consortium).
Supplementary Data
The principle of arthroscopic ultrasound imaging and different cartilage lesions in the knee joint are shown on simultaneous arthroscopy and ultrasound views. Simultaneous ultrasound and arthroscopy videos present the noninvasive evaluation, retrograde drilling, and bone transplantation for 3 different osteochondritis dissecans lesions in the medial femoral condyle.
References
- 1.Reed M.E., Villacis D.C., Hatch G.F., III 3.0-Tesla MRI and arthroscopy for assessment of knee articular cartilage lesions. Orthopedics. 2013;36:e1060–e1064. doi: 10.3928/01477447-20130724-24. [DOI] [PubMed] [Google Scholar]
- 2.Harris J.D., Brophy R.H., Siston R.A., Flanigan D.C. Treatment of chondral defects in the athlete’s knee. Arthroscopy. 2010;26:841–852. doi: 10.1016/j.arthro.2009.12.030. [DOI] [PubMed] [Google Scholar]
- 3.Sugita T., Aizawa T., Uozumi H. Can the fragment stability of osteochondritis dissecans be interpreted by arthroscopic findings alone? Arthroscopy. 2011;27:1171–1172. doi: 10.1016/j.arthro.2011.06.039. [DOI] [PubMed] [Google Scholar]
- 4.Spahn G., Klinger H.M., Baums M., Pinkepank U., Hofmann G.O. Reliability in arthroscopic grading of cartilage lesions: Results of a prospective blinded study for evaluation of inter-observer reliability. Arch Orthop Trauma Surg. 2011;131:377–381. doi: 10.1007/s00402-011-1259-8. [DOI] [PubMed] [Google Scholar]
- 5.Spahn G., Klinger H.M., Hofmann G.O. How valid is the arthroscopic diagnosis of cartilage lesions? Results of an opinion survey among highly experienced arthroscopic surgeons. Arch Orthop Trauma Surg. 2009;129:1117–1121. doi: 10.1007/s00402-009-0868-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nieminen H.J., Zheng Y.P., Saarakkala S. Quantitative assessment of articular cartilage using high-frequency ultrasound: Research findings and diagnostic prospects. Crit Rev Biomed Eng. 2009;37:461–494. doi: 10.1615/critrevbiomedeng.v37.i6.20. [DOI] [PubMed] [Google Scholar]
- 7.Kaleva E., Virén T., Saarakkala S. Arthroscopic ultrasound assessment of articular cartilage in the human knee joint: A potential diagnostic method. Cartilage. 2010;2:246–253. doi: 10.1177/1947603510391781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liukkonen J., Lehenkari P., Hirvasniemi J. Ultrasound arthroscopy of human knee cartilage and subchondral bone in vivo. Ultrasound Med Biol. 2014;40:2039–2047. doi: 10.1016/j.ultrasmedbio.2014.04.001. [DOI] [PubMed] [Google Scholar]
- 9.Mathiesen O., Konradsen L., Torp-Pedersen S., Jørgensen U. Ultrasonography and articular cartilage defects in the knee: An in vitro evaluation of the accuracy of cartilage thickness and defect size assessment. Knee Surg Sports Traumatol Arthrosc. 2004;12:440–443. doi: 10.1007/s00167-003-0489-x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The principle of arthroscopic ultrasound imaging and different cartilage lesions in the knee joint are shown on simultaneous arthroscopy and ultrasound views. Simultaneous ultrasound and arthroscopy videos present the noninvasive evaluation, retrograde drilling, and bone transplantation for 3 different osteochondritis dissecans lesions in the medial femoral condyle.