Abstract
Anterior cervical surgery is commonly used for cervical vertebral body lesions. However, the structure of blood vessels and nerve tissues along the route of anterior cervical surgery is complex. We aimed to measure the data of the longus colli, the sympathetic trunk and the cervical sympathetic trunk (CST) ganglia in Chinese cadaver specimens. A total of 32 adult cadavers were studied. We delineated the surgical anatomy of the CST. The superior and inferior/cervicothoracic ganglia of the sympathetic trunk consistently appeared. The middle ganglion was observed in 28.1% of the specimens and there were 2 cases of unilateral double middle cervical ganglia. The inferior ganglion was observed in 25.0% of the specimens and the cervicothoracic ganglion was observed in the remaining specimens. The distance between the CST gradually decreased from the top to the bottom, and the distance between the medial edges of the longus colli gradually broadened from the top down. The average angle between the bilateral CST and the midline of the vertebra was 11.2°±1.8° on the left side and 10.3°±1.4° on the right side. The average angle between the medial margins of longus colli of both sides was 11.1°±1.9°. The CST is at high risk when LC muscle is cut transversely or is dragged heavily, especially at the levels of C6 and C7. Awareness of the regional anatomy of the CST could help surgeons to identify and preserve it during anterior cervical surgeries.
Keywords: cervical sympathetic trunk, ganglion, Horner syndrome, longus colli, spinal surgery
Introduction
Discectomy from the anterior cervical spine and interbody bone graft fusion was first reported by Robinson and Smith[1], which provided an effective surgical procedure for cervical and intervertebral disc disease. Since then, various methods for improved surgery have been advanced. Anterior cervical surgery for the treatment of cervical vertebral body lesions, including tumor infection and trauma, has become very common. However, the structure of blood vessels and the nerve tissue along the route of anterior cervical surgery is complex, which increases surgical difficulty and risk. Sympathetic nerve injury, a complication of the surgery, has been studied[2,3]. In our work, we also found postoperative symptoms of injury to the sympathetic trunk. Bertalanffy and Eggert reported that the incidence of Horner's syndrome was 1.1% in a cohort of 450 cases undergoing anterior cervical surgery[4], which is similar to that reported by Cuatico and Dohn[5,6], but lower than that reported (4%) by Bruneau et al.[7]. Research into the cervical sympathetic trunk (CST) was also reported[8,9], but there have been no systemic anatomical studies of the sympathetic trunk and surrounding structures in Chinese subjects. This study aimed to measure the data of the longus colli (LC), sympathetic trunk and CST ganglia in Chinese subjects and to become more familiar with their anatomical characteristics, thereby providing a basis for avoiding injury in surgery.
Materials and methods
Cadavers
In our study, 32 adult cadavers (18 men and 14 women) with a mean age of 56 years old (ranged from 27 to 78 years) were obtained from the Department of Anatomy of the authors' affiliated institution. They were placed in the supine position and their necks in loose extension. Anterior skin and soft tissues of the neck and platysma muscles were removed. After the omohyoid muscle was transected, and the sternocleidomastoid muscle and the carotid sheath were retracted, the LC and the sympathetic trunk beneath the prevertebral fascia were exposed. Research was performed on the course of the cervical LC on both sides of and on the sympathetic trunk, as well as its corresponding relationship with the vertebral body. The study protocol was approved by the local institutional review board at the authors' affiliated institution and the study was carried out in accordance with the institutional and state guidelines regarding use of human cadavers.
Measurements
Measurements were obtained, including the dimensions of the superior cervical ganglion, the middle cervical ganglion, the inferior cervical/cervicothoracic ganglion and the vertebral ganglion, the distance between the ganglia, the medial part of the LC on both sides, the cervical and thoracic vertebral anterior midline, CST and cervical spine anterior midline, the angle between CST and cervical spine longitudinal axis, and the angle between the medial parts of the LC. The protractor used for angle measurement was sensitive to 1°, and the vernier calipers used for length measurements were sensitive to 0.1 mm. We examined the measurement data of both sides using a test and analysis of variance, respectively.
Statistical analysis
Data was expressed as x±s. Statistical analysis of distance between the two sides was performed using Student's t test, and the number of the ganglions between men and women was examined using χ2 test. P<0.05 was considered as significant.
Results
The CST, which is located on both sides of the cervical spine and is covered by the prevertebral fascia, was composed of the superior cervical ganglion, the middle cervical ganglion, the inferior cervical/cervicothoracic ganglion, the vertebral ganglion, and the internode branch. We observed that the superior cervical ganglion appeared in all cadavers, the middle cervical ganglion and inferior cervical/cervicothoracic ganglion were asymmetrically absent in some cadavers, and the middle cervical ganglion appeared on the left side in 8 (25%) cases and on the right side in 6 (18.8%) cases of 32 specimens at different times. The cervicothoracic ganglion or stellate ganglion, which is combined with cervical ganglion and the first thoracic ganglion, consistently appeared on both sides (with 8 cases on the left side and 8 cases of 32 specimens on the left side) in the absence of the inferior cervical ganglion at different times. The appearance rate of a vertebral ganglion was not high. A vertebral ganglion appeared asymmetrically on the left side in 5 (15.6%) cases and on the right side in 4 (12.5%) cases of 32 specimens (Table 1).
Table 1. The number of ganglia on the right and left side in men and women.
| Male (%) | Female (%) | |||
| Ganglion | Left | Right | Left | Right |
| SG | 18 (100.0) | 18 (100.0) | 14 (100.0) | 14 (100.0) |
| MG | 5 (27.8) | 3 (16.7) | 3 (21.4) | 3 (21.4) |
| IG | 5 (27.8) | 4 (22.2) | 3 (21.4) | 4 (28.6) |
| CTG | 13 (72.2) | 14 (77.8) | 11 (78.6) | 10 (71.4) |
| VG | 3 (16.7) | 2 (11.1) | 2 (14.3) | 2 (14.3) |
SG, superior ganglion; MG, middle ganglion; IG, inferior ganglion; CTG, cervicothoracic ganglion; VG, vertebral ganglion. There was no statistical differences between men and women and the two sides (p>0.05).
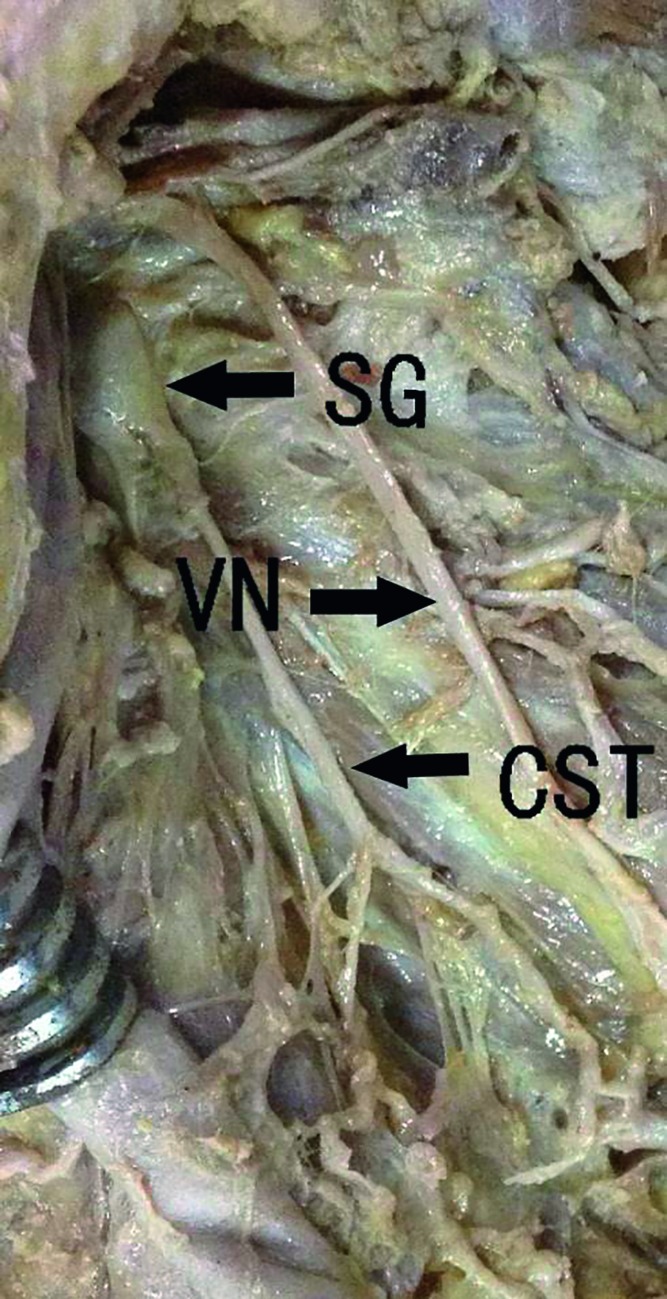
Superior cervical ganglion
The superior cervical ganglion was detected in all 32 specimens on both sides, in the front of the transverse process at C2-C3. The average length of the superior cervical ganglion was 31.9±5.3 mm and 32.2±5.0 mm on the left and right side, respectively. The average width was 7.0±1.2 mm and 7.2±1.1 mm on the left and right side, respectively. The average thickness was 2.7±0.3 mm and 2.7±0.3 mm on the left and right side, respectively. No significant differences were found between the left and right side (P>0.05) (Fig. 1).
Fig. 1. The position and adjacent tissue of the superior ganglion.
SG: superior ganglion; CST: cervical sym-pathetic trunk; VN: nervi vagus.
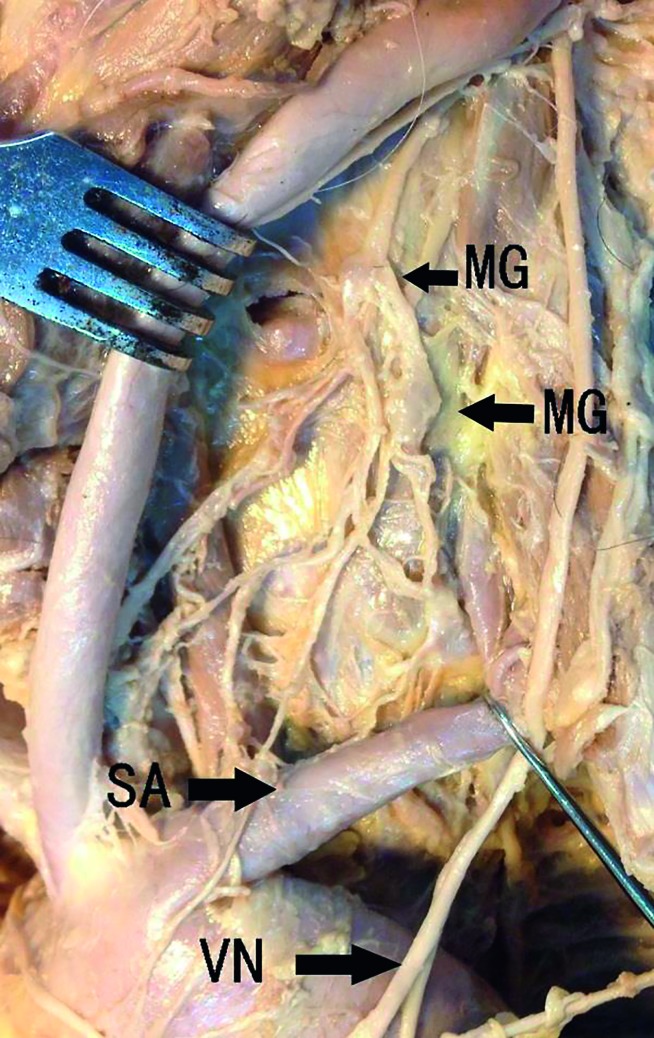
Middle cervical ganglion
We observed that the middle cervical ganglion was on the left in 8 cases and on the right in 6 cases, among which 5 cases of bilateral symmetry appeared (Fig. 2). The middle cervical ganglion was located in the front of C6 transverse process; the average length was 6.6±1.5 mm and 6.3±1.5 mm on the left and right side, respectively. The average width was 3.9±0.8 mm and 3.8±0.8 mm on the left and right side, respectively. The average thickness was 2.0±0.5 mm and 1.7±0.3 mm on the left and right side, respectively. No significant differences were found between the left and right side (P>0.05) (Fig. 3).
Fig. 2. The double middle cervical ganglia are observed.
MG: middle ganglion; SA: subclavian artery; VN: nervi vagus.
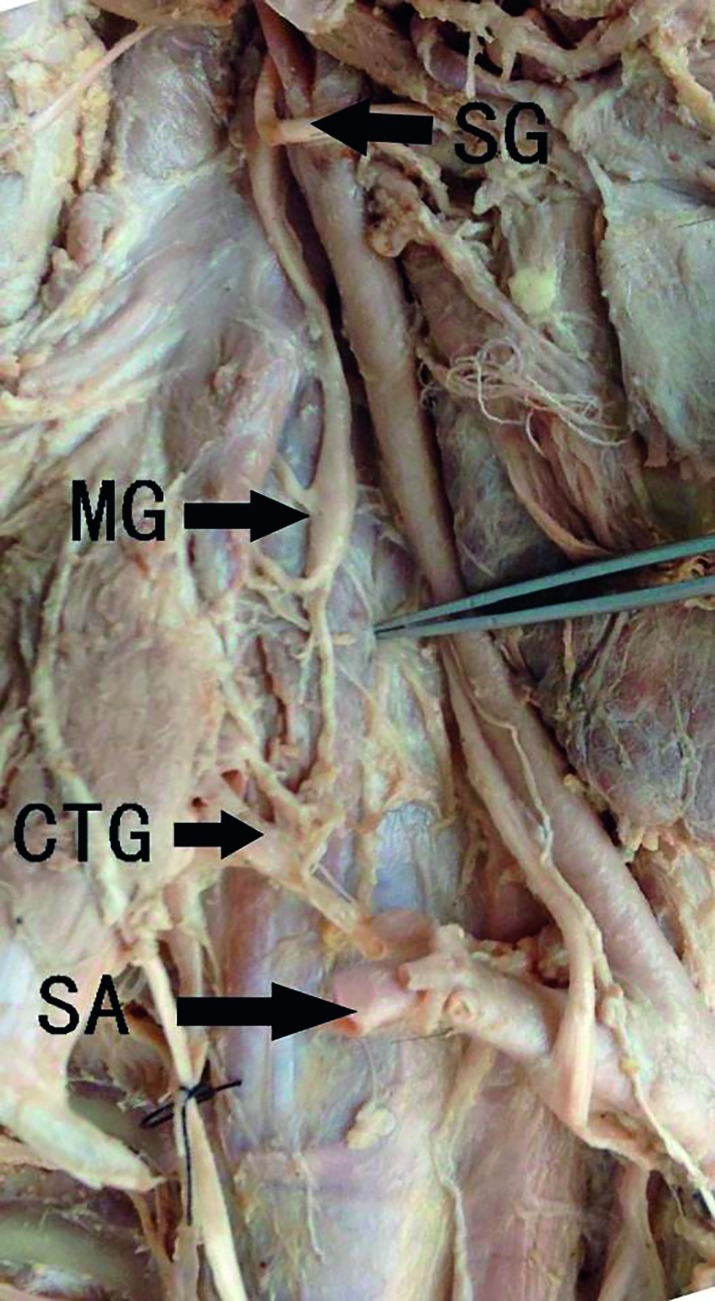
Fig. 3. The position and adjacent tissue of the sympathetic trunk.
SG: superior ganglion; MG: middle ganglion; CTG: cervicothoracic ganglion; SA: subclavian artery.
Inferior cervical ganglion
The inferior cervical ganglion, which is located in C7 transverse process forward, was found in 8 cadavers on the left side and in 8 cadavers on the right side. There were 7 cases of bilateral symmetry. The average length of the inferior cervical ganglion was 8.6±1.6 mm and 8.2±1.5 mm on the left and right side, respectively. The average width was 4.5±0.6 mm and 4.4±0.5 mm on the left and right side, respectively. The average thickness was 4.4±0.5 mm and 3.9±0.3 mm on the left and right side, respectively. No significant differences were found between the left and right side (P>0.05).
Cervicothoracic ganglion
The cervicothoracic ganglion, which lies in front of the first rib neck, was detected on the left side in 32 specimens of 24 cases, and in 24 cases, it was located on the right side, but there was no symmetry. There were 23 cases of bilateral symmetry. The average length of the cervicothoracic ganglion was 18.7±2.0 mm and 18.9±1.6 mm on the left and right side, respectively. The average width was 7.0±1.0 mm and 6.7±0.9 mm on the left and right side, respectively. The average thickness was 2.5±0.4 mm and 2.3±0.3 mm on the left and right side, respectively. No significant differences were found between the left and right side (P>0.05) (Fig. 4).
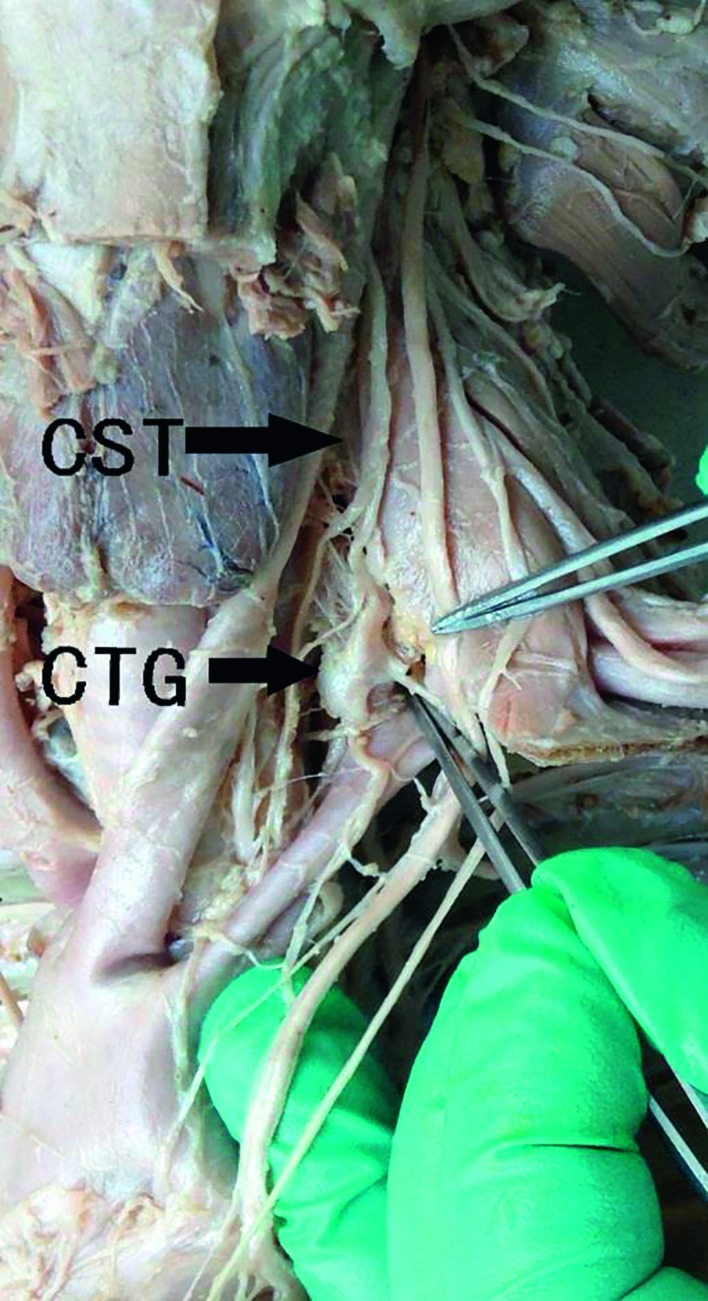
Fig. 4. The position and adjacent tissue of the sympathetic trunk.
CTG: cervicothoracic ganglion; CST: cervical sympathetic trunk.
Vertebral ganglion
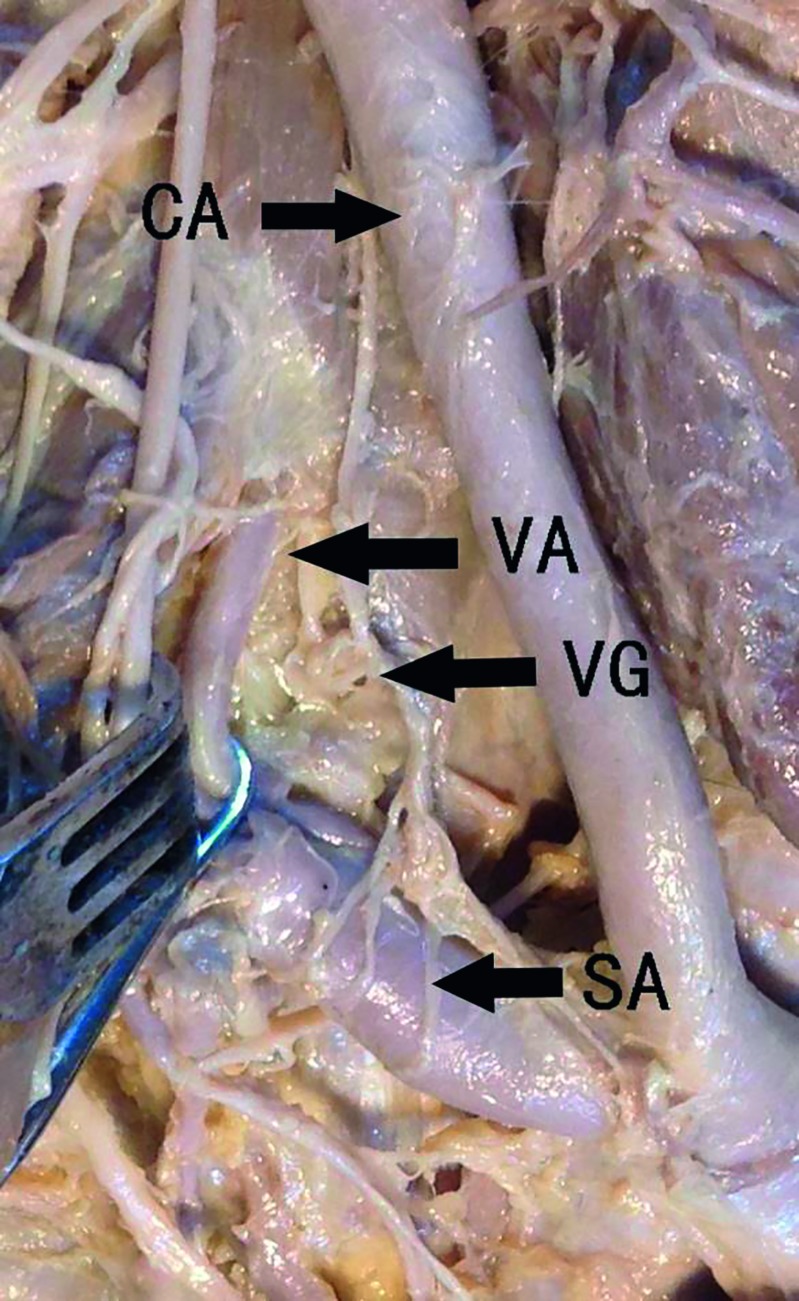
Bilaterally symmetrical vertebral ganglia were detected in 4 cases of 32 specimens, and 1 case was unilateral (Fig. 5). The average length of the vertebral ganglion was 4.7±0.9 mm and 4.8±0.5 mm on the left and right side, respectively. The average width was 3.6±0.6 mm and 3.3±0.4 mm on the left and right side, respectively. The average thickness was 2.5±0.3 mm and 2.7±0.1 mm on the left and right side, respectively. No significant differences were found between the left and right side (P>0.05) (Table 2).
Fig. 5. The position and adjacent tissue of the vertebral ganglion.
VG: vertebral ganglion; CA: cephalic artery; VA: vertebral artery; SA: subclavian artery.
Table 2. The sizes of ganglia.
| Left (mm) | Right (mm) | |||||
| Ganglion | Length | Width | Thickness | Length | Width | Thickness |
| SG | 31.9±5.3 | 7.0±1.2 | 2.7±0.3 | 32.2±5.0 | 7.2±1.1 | 2.7±0.3 |
| MG | 6.6±1.5 | 3.9±0.8 | 2.0±0.5 | 6.3±1.5 | 3.8±0.8 | 1.7±0.3 |
| IG | 8.6±1.6 | 4.5±0.6 | 4.4±0.5 | 8.2±1.5 | 4.4±0.5 | 3.9±0.3 |
| CTG | 18.7±2.0 | 7.0±1.0 | 2.5±0.4 | 18.9±1.6 | 6.7±0.9 | 2.3±0.3 |
| VG | 4.7±0.9 | 3.6±0.6 | 2.5±0.3 | 4.8±0.5 | 3.3±0.4 | 2.7±0.1 |
SG: superior ganglion; MG: middle ganglion; IG: inferior ganglion; CTG: cervicothoracic ganglion; VG: vertebral ganglion. There was no statistical differences between two sides (P>0.05).
Distance among the superior, middle, and inferior cervical ganglia
Distance between the superior and middle cervical ganglia on the same side corresponded to the lower edge of the superior cervical ganglion and the upper edge of the middle cervical ganglion. Distance between the middle cervical ganglion and inferior cervical/cervicothoracic ganglion on the ipsilateral side corresponded to the lower edge of the middle cervical ganglion and upper edge of the inferior cervical/cervicothoracic ganglion. Distance between the superior cervical ganglion and the cervical/cervicothoracic ganglion on the ipsilateral side corresponded to the lower edge of the superior cervical ganglion and upper edge of the cervical/cervicothoracic ganglion. In our study, there were 2 cases of double middle cervical ganglia. Distance between the superior and middle cervical ganglia corresponded to the lower edge of the superior cervical ganglion and upper edge of the double middle cervical ganglion. Distance between the middle double cervical ganglion and inferior cervical/cervicothoracic ganglion on the ipsilateral side corresponded to the lower edge of the double middle cervical ganglion and upper edge of the inferior cervical/cervicothoracic ganglion. On the left side, the average distance between the superior and middle ganglia was 44.2±4.9 mm, while on the right side, the average was 46.8±4.6 mm, and no significant differences were found between the left and right side. The mean distance on the left side between the middle cervical ganglion and inferior cervical/cervicothoracic ganglion was 18.9±2.9 mm, and on the right side, 18.0±1.5 mm, and no significant differences were found between the left and right side. The average distance on the left side between the superior cervical ganglion and cervical/cervicothoracic ganglion was 71.5±6.0 mm, and on the right side, 73.1±5.3 mm, and no significant differences were found between the left and right side (Table 3).
Table 3. The distances among the ganglia.
| SG-MG (mm) | MG-IG/CTG (mm) | SG-IG/CTG (mm) | |||||||
| Min. | Max. | Mean | Min. | Max. | Mean | Min. | Max. | Mean | |
| Left | 37.2 | 53.2 | 44.2±4.9 | 12.3 | 23.8 | 18.9±2.9 | 50.1 | 86.4 | 71.5±6.0 |
| Right | 39.6 | 59.7 | 46.8±4.6 | 15.2 | 21.8 | 18.0±1.5 | 48.3 | 89.6 | 73.1±5.3 |
SG: superior ganglion; MG: middle ganglion; IG: inferior ganglion; CTG: cervicothoracic ganglion; Min: minimum; Max: maximum. There was no statistical differences between two sides (P>0.05).
Sympathetic trunk
The average angle between CST and midline of the vertebral body on the left and right side was 11.2°±1.8° and 10.3°±1.4°, respectively. No significant differences were found between the left and right sides (P>0.05). The average distance between the medial margin of CST and midline of the vertebral body on the left side was 26.7±2.6 mm at C3, 25.5±2.3 mm at C4, 24.1±2.1 mm at C5, 22.5±1.9 mm at C6 and 20.8±1.6 mm at C7; on the right side, it was 26.5±2.7 mm at C3, 25.0±2.4 mm at C4, 23.5±2.0 mm at C5, 22.1±1.8 mm at C6 and 20.4±1.5 mm at C7.
In addition, 22 cases of 32 cadavers (68.8%) had white tendon tissues under the thoracic spine, and 10 cases of 32 cadavers (31.2%) had muscle tissues or a mixture of muscle and tendon tissues to inside of the anterior longitudinal ligament.
The LC from the cephalic end to caudal end has a tendency to converge. The average angle between the medial margins of LC on both sides was 11.1°±1.9°. Distance between the medial margin of LC and the anterior midline of the cervicothoracic spine from the top to the bottom gradually broadened. The average distance on the left was 4.0±0.6 mm at C3, 4.8±0.8 mm at C4, 5.9±0.9 mm at C5, 6.9±0.9 mm at C6, 7.8±0.8 mm at C7, 8.9±0.9 mm at T1 and 10.5±1.3 mm at T2; and on the right, it was 4.1±0.6 mm at C3, 5.0±0.7 mm at C4, 6.0±0.7 mm at C5, 7.1±0.8 mm at C6, 8.0±0.8 mm at C7, 9.2±1.0 mm at T1, 10.6±1.2 mm at T2 (Table 4).
Table 4. The distances between the CST and the midline and the distances between the LC and the midline at the level of the vertebrae.
| CST-Midline (mm) | LC-Midline (mm) | |||||
| Level | Left | Right | Mean | Left | Right | Mean |
| C3 | 26.7±2.6 | 26.5±2.7 | 26.6±2.7 | 4.0±0.6 | 4.1±0.6 | 4.0±0.6 |
| C4 | 25.5±2.3 | 25.0±2.4 | 25.2±2.3 | 4.8±0.8 | 5.0±0.7 | 4.9±0.7 |
| C5 | 24.1±2.1 | 23.5±2.0 | 23.8±2.1 | 5.9±0.9 | 6.0±0.7 | 5.9±0.8 |
| C6 | 22.5±1.9 | 22.1±1.8 | 22.3±1.9 | 6.9±0.9 | 7.1±0.8 | 7.0±0.9 |
| C7 | 20.8±1.6 | 20.4±1.5 | 20.6±1.6 | 7.8±0.8 | 8.0±0.8 | 7.9±0.8 |
| T1 | – | 8.9±0.9 | 9.2±1.0 | 9.1±1.0 | ||
| T2 | – | 10.5±1.3 | 10.6±1.2 | 10.6±1.3 | ||
CST: cervical sympathetic trunk; LC: longus colli. There was no statistical differences between two sides (P>0.05).
Discussion
Horner's syndrome was first reported in 1929 by Swiss ophthalmologist Johann-Friedirch-Horne. The diagnostic criteria of the World Health Organization are listed as follows: decreased vision, miosis, endophthalmos, no sweat, and vascular dilatation at the lesion site [10]. Horner's syndrome can occur after CST injury. Diagnosis can be made according to clinical signs and laboratory results.
Under normal circumstances, CST contains 3-4 ganglia, including the superior, middle (double), inferior cervical/cervicothoracic and vertebral ganglia. In the 32 specimens in our study, the inferior and cervical/cervicothoracic ganglia consistently appeared, and their locations were relatively fixed in general. The lower rate of the middle cervical ganglion was approximately 28.1%. Two of the specimens had unilateral appearance of two cervical middle ganglia. Our study showed that the superior ganglion was the largest ganglion of the sympathetic trunk. The length and width of the superior ganglion were 12.5±1.5 and 5.3±0.6 mm, respectively, which was located at the C4 vertebral level in the study of Civelek et al.[11]. However, in our study, the length and width of the superior ganglion were 32.1±5.1 and 7.1±1.2 mm, respectively, which was located at the C2-3 vertebral level. Tubbs et al. indicated that the superior ganglion was approximately located at the C2-3 vertebral level and in the rear of the internal carotid artery[12], which is consistent with our study. This disagreement might depend on if the specimens were soaked in formalin, as well as the soaking time. However, the likelihood of injury to the superior ganglia of the sympathetic trunk is very small. The anterior tubercle of the transverse process of the lower cervical spine at C6 is an important anatomical landmark. Our study found that the middle cervical ganglion was mostly in C6 transverse process level, and in 28% of the specimens, we observed 2 cases of double ganglia. The length and width of the middle ganglion were 6.5±1.5 and 3.9±0.8 mm, respectively. In some samples, in the absence of the middle ganglion, the diameter of the CST was 2.5±0.3 mm on the left side, and 2.3±0.3 mm on the right side. Our measurements corresponded to those in Kıray et al.'s report[8], in which the diameter of the CST was 2.2±0.7 mm. The inferior cervical ganglion and the first thoracic ganglion fused into the cervicothoracic ganglion in most cases. If the inferior ganglion appeared, it was close to the first thoracic ganglion, and the distance was 5.5±1.6 mm on the left side, and 5.1±1.0 mm on the right side. The two ganglia sometimes intertwined. Most studies have indicated that the CST runs along the prevertebral fascia posteriorly and along LC anteriorly. However, Lyons et al. found that in 16.7% of the specimens, the CST ran along the posterior wall of the carotid sheath, which indicated the possibility of damaging the sympathetic trunk by stretching the carotid sheath during anterior cervical surgery[13]. The anatomical characteristics are very important for surgery of the lower cervical or anterior cervical thoracic spine. Surgeons should avoid excessive stretching of the carotid sheath during surgery.
The LC is made of muscle and tendon tissues and is located in front of the cervical and upper thoracic vertebral body, including external and internal parts. The external part begins at the C3-6 transverse process and stops at the anterior tubercle of the atlas. The internal part begins at the C5-7 and T1-3 vertebral bodies and stops at the anterior tubercle of transverse process at T2-4 and C5-7, which is similar to Lu et al.'s reports[14,15].
The distance between the medial edge of LC and the anterior midline of the lower cervical spine gradually broadened from the top down. The nearest point of the sympathetic trunk on both sides was located at the C6-7 level; therefore, surgeons should keep deviating from the centerline as far as possible during surgery and minimize the stripping of LC, especially at the C6-7 level. LC is formed by muscle and tendon tissues, and the demarcation point is located at the cervicothoracic junction. In front of the lower cervical spine were mostly muscle tissues, and in front of the thoracic spine were mostly tendon tissues. This point could be used as a marker for intraoperative positioning.
CST injury is mostly caused by excessive exposure of the outer surface of the bone in front of the lower cervical vertebral body, the hook vertebral joint or the transverse foramen, cutting off the CST in operation or stripping or excessively stretching the LC. Among the reasons above, exposure of the cervical anterior lateral part or the transverse foramen and consequent excessive stretching of the LC were the main reason that the CST was injured. Lu et al. indicated that any injury of the CST in front of the lower cervical spine could cause Horner syndrome. Therefore, during anterior lower cervical operations, hooks should not be placed above the LC, and there is no need to expose the sympathetic trunk; a little blunt dissection below the inner edge of the LC, placing the retractor under the LC and pulling carefully for the sake of avoiding sympathetic trunk injury, is sufficient. Sometimes, the position of the middle cervical ganglion must be identified during surgery. However, in our study, the middle cervical ganglion was absent in some samples. Identifying the stellate ganglion was important in such cases. This ganglion is consistently and generally located in front of the first rib neck. Understanding of these anatomical features is helpful for avoiding injury to the sympathetic trunk.
In conclusion, Horner's syndrome in cervicothoracic spine anterior surgical complications is not rare, causing some adverse effects in patients. The distance between the medial margin of the CST and midline of the vertebral body is nearest at the levels of C6 and C7, and the CST is at high risk when LC muscle is cut transversely or is dragged heavily, especially during operation of exposing the outer surface of the bone in front of the lower cervical vertebral body, the hook vertebral joint or the transverse foramen. Familiarity with the anatomical characteristics of the LC and CST could contribute to identifying the sympathetic trunk correctly during surgery and reducing the occurrence of surgical complications.
Acknowledgments
This work was supported by National Natural Science Foundation of China (Grant 81171694, 81371968, 81401791), and a project funded by the Priority Academic Program Development of Jiangsu Higher Education institution. The cadavers used in our study were provided by the Department of Anatomy, Nanjing Medical University. We gratefully acknowledge the support and assistance from all the teachers of the Department of Anatomy.
References
- [1].Robinson RA, Smith GW. Anterolateral cervical disc removal and interbody fusion for cervical disc syndrome[J] Bull Johns Hopkins Med Soc. 1955;96:223–224. [Google Scholar]
- [2].An HS, Vaccaro A, Cotler JM. Spinal disorders at the cervicothoracic junction[J] Spine. 1994;19:2557–2564. doi: 10.1097/00007632-199411001-00011. [DOI] [PubMed] [Google Scholar]
- [3].Johnston FG, Crockard A. One-stage internal fixation and anterior fusion in complex cervical spinal disorders[J] J Neurosurg. 1995;82:234–238. doi: 10.3171/jns.1995.82.2.0234. [DOI] [PubMed] [Google Scholar]
- [4].Bertalanffy H, Eggert HR. Complications of anterior cervical discectomy without fusion in 450 consecutive patients[J] Acta Neurochir (Wien) 1989;99:41–50. doi: 10.1007/BF01407775. [DOI] [PubMed] [Google Scholar]
- [5].Cuatico W. Anterior cervical discectomy without inter-body fusion: an analysis of 81 cases[J] Acta Neurochir (Wien) 1981;57:269–274. doi: 10.1007/BF01664843. [DOI] [PubMed] [Google Scholar]
- [6].Dohn DF. Anterior interbody fusion for treatment of cervical disc conditions[J] JAMA. 1966;197:897–900. [PubMed] [Google Scholar]
- [7].Bruneau M, Cornelius JF, George B. Microsurgical cervical nerve root decompression by anterolateral approach[J] Neurosurgery. 2006;58(1 Suppl):ONS108–ONS113. doi: 10.1227/01.NEU.0000193521.98836.C5. [DOI] [PubMed] [Google Scholar]
- [8].Kiray A, Arman C, Naderi S, et al. Surgical Anatomy of the Cervical Sympathetic Trunk[J] Clin Anat. 2005;18:179–185. doi: 10.1002/ca.20055. [DOI] [PubMed] [Google Scholar]
- [9].Saylam CY, Ozgiray E, Orhan M, et al. Neuroanatomy of Cervical Sympathetic Trunk: A Candaveic Study[J] Clin Anat. 2009;22(3):324–330. doi: 10.1002/ca.20764. [DOI] [PubMed] [Google Scholar]
- [10].Wlaton KA, Buono LM. Horner syndrome[J] Curr Opin Ophthalmol. 2003;14(6):357. doi: 10.1097/00055735-200312000-00007. [DOI] [PubMed] [Google Scholar]
- [11].Civelek E, Karasu A, Cansever T, et al. Surgical anatomy of the cervical sympathetic trunk during anterolateral approach to cervical spine[J] Eur Spine J. 2008;17(8):991–995. doi: 10.1007/s00586-008-0696-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Tubbs RS, Salter EG, Oakes WJ. Anatomic landmarks for nerves of the neck: a Vade Mecum for neurosurgeons[J] Oper Neurosurg. 2005;2(56):256–260. doi: 10.1227/01.neu.0000156541.78020.da. [DOI] [PubMed] [Google Scholar]
- [13].Lyons AJ, Mills CC. Anatomical variants of the cervical sympathetic chain to be considered during neck dissection[J] Br J Oral Maxillofac Surg. 1998;36:180–182. doi: 10.1016/s0266-4356(98)90493-4. [DOI] [PubMed] [Google Scholar]
- [14].Golffinos JG, Dickman CA. Repair of vertebral artery during anterior cervical decompression[J] J Spine. 1994;19(22):2552–2556. doi: 10.1097/00007632-199411001-00010. [DOI] [PubMed] [Google Scholar]
- [15].Lu J, Ebraheim NA, Nadim Y, et al. Anterior approach to the cervical spine: Surgical anatomy[J] Orthopedics. 2000;23(8):841–845. doi: 10.3928/0147-7447-20000801-19. [DOI] [PubMed] [Google Scholar]