Abstract
Background
There is a paucity of research on the profile of cancers among displaced populations, specifically Afghan refugees in Iran. This study illustrates the pattern of cancers in this population, and highlights the challenges of cancer care in displaced people with the intent that this data will facilitate appropriate allocation of resources to improve care in this population.
Material/Methods
This was a retrospective cross-sectional study, in which we collected the demographics and profile of cancers among Afghan refugees from 2005 to 2010 from referrals to the United Nations High Commissioner for Refugees (UNHCR) offices in Iran. Accrued evidence by other studies published between January 1993 and July 2014 pertaining to cancer diagnoses in refugees from Afghanistan, Tibet, Syria, Jordan, and Iraq was reviewed.
Results
Cancer diagnoses accounted for 3083 of 23 152 total referrals, with 49% female and 51% male cases; 23.3% were 0–17 years of age, 61.2% were 18–59, and 15.5% were above 60. The most common health referral for females and males (0–17) was malignant neoplasms of lymphatic and hematopoietic tissue, accounting for 34.2%. In the age groups 18–59 and above 60 for both male and females it was malignant neoplasm of the digestive system, occurring in 26.3% and 48.7%, respectively.
Conclusions
In the setting of humanitarian crises especially war, cancer diagnoses among refugees is a major health burden both on the host countries and the international community with serious implications considering the recent growing trend in the Middle Eastern countries. The prevalence of certain cancer diagnoses among refugees, like gastrointestinal, respiratory, breast, and genitourinary cancers necessitates a multidirectional approach, primarily aimed at prevention and early detection. International partnerships are essential for improvement in cancer surveillance service availability, and delivery of the standard of care, in an overall effort to reduce the human cost, monetary, and resource associated burdens of cancer.
Recommendations to implement effective prevention and management goals as well as improved record keeping in the refugee setting and the acquisition of secure and sustainable funding sources should be implemented in collaboration with global humanitarian agencies like UNHCR.
MeSH Keywords: Breast Neoplasms, Cancer Care Facilities, Gastrointestinal Neoplasms, Minority Health, Refugees, United Nations
Background
As per the United Nations High Commissioner for Refugees (UNHCR), the term refugee refers to “persons who are outside their country and cannot return owing to a well-founded fear of persecution because of their race, religion, nationality, political opinion, or membership of a particular group” [1]. According to UNHCR records, a total of 35.8 million people were displaced in 2012, including 10.5 million refugees along with several million others seeking asylum internationally [2].
Non-communicable diseases (NCDs) represent 43% of the burden of disease worldwide and by 2020 NCDs are expected to be responsible for 60% of the disease burden and 73% of all deaths. This anticipated increase in prevalence can primarily be attributed to emerging epidemics of NCDs in developing countries [3]. Despite the overwhelming statistics, NCDs generally have not been receiving adequate attention [4,5]. Not only are lower socioeconomic individuals disproportionately affected, due in part to more likely exposure to risk factors, they are also less equipped to deal with long-term management of their conditions. Furthermore, many NCDs, especially diabetes and cancer, weaken social consistency through stigma and discrimination [6]. In the refugee population afflicted with such diseases, challenges specific to their situation hinder appropriate follow-up and treatment. Low income, older age, unfamiliarity with the host country’s medical system, multiple comorbidities, and low healthcare literacy are among the factors that limit effectual disease prevention and management [7]. In the case of patients with chronic disorders (e.g., hypertension, diabetes, and cancers), exacerbations may occur if disease is not well controlled or treatment is suddenly disrupted.
There is a paucity of data regarding the cancer profile of refugee populations [8]. Epidemiological investigations related to cancer have not been undertaken in a significant number of host countries serving refugees, thus there is sparse data evaluating cancer as an important NCD in the setting of this at risk population. In the study herein, we have compiled available data from over a 6-year period of various cancer types in refugees in Iran, with the intention of highlighting the challenges and patterns of cancer care in displaced peoples and the overall goal to improve outcomes during humanitarian emergencies. Accrued studies include peer-reviewed articles published between January 1993 to July 2014 pertaining to cancer diagnoses in refugees from Afghanistan, Tibet, Syria, Jordan and Iraq (Table 1).
Table 1.
Profile of cancer diseases among refugees, Review of the articles 1990–2014.
| Reference | Location of asylum | Refugee’s country of origin | Total number of Refugees | Total number of refugees with cancer | Demographic characteristic | Type of cancer studied | Years of observation | Most common cancers |
|---|---|---|---|---|---|---|---|---|
| Khan (1997) [11] | Pakistan | Afghanistan | 655 | 368 | Male (69%) Female (31%) |
All types | 1990–94 | Hematopoietic, CNS and eye |
| Khan (1997) [12] | Pakistan | Afghanistan | NA | 2988 | Male (59%) Female (41%) |
All types | 1990–94 | Hematopoietic, CNS and eye, Gastrointestinal |
| Bhitia (2002) [13] | India | Tibet | 65000 | NA | NA | NA | 1994–96 | NA |
| Mateen (2012) [8] | Jordan | Iraq | 7642 | 164 | Male (58%) Female (42%) |
All types | 2012 | Breast, Brain, Genitourinary |
| Otoukesh (2012) [3] | Iran | Afghanistan | 23158 | 3083 | Male (51%) Female (49%) |
All types | 2005–11 | Hematopoietic, CNS and eye, Gastrointestinal, Breast, Benign tumors |
| Doocy (2013) [10] | Jordan & Syria | Iraq | Jordan (3414) Syria (2342) |
Jordan (444) Syria (140) |
Jordan: NA Syria, 18–70 yr’s old: Male (51%) Female (49%) |
NA | 2008–09 | NA |
| Spiegel (2014) [9] | Jordan & Syria | Iraq | NA | Jordan (511) Syria (954) |
Jordan: Male (63%) Female (37%) Syria: Male (17%) Female (83%) |
All types | 2010–12 | Jordan: Breast, Soft tissue, Gastrointestinal Syria: Hematopoietic, Breast, Gastrointestinal, Endocrine tumors |
Material and Methods
This is a retrospective, cross-sectional study utilizing data from the UNHCR offices in Tehran and Mashhad cities in Iran. The data provided for this study, including 3083 referrals, is from a sample of 23 167 registered Afghan refugees who were referred to the two main offices from 2005 to 2011. The data collection was done by two separate teams; each including social workers with a minimum of three professional interviewers, one physician, and one general-purpose receptionist. The teams were based in the main UNHCR offices with an extended area of coverage over the central, northern, and eastern parts of Iran.
Individual cases approached or were referred to UNHCR by regional hospitals, welfare and charity societies, as well as by governmental and non-governmental organizations. For eligibility assessments these cases were screened and processed by the community and medical service teams. Community visits and interviews at UNHCR offices, homes and hospitals were different screening methods. A report of consented individuals was then recorded in the Community Integrated Social and Medical Assistance Program (CISAMAP) database. Records consist of all cases either accepted or rejected for assistance to ensure reliable data entry was conducted based on the list of the cancers presented as the referral cause. The CISAMAP physician was responsible for performing the medical assessments. SPSS (version 18) was used for data analysis initially where rejected cases were excluded from the analysis, while tables and graphs were prepared in Microsoft Word 2010.
Results
The total number of refugees included in the analysis was 23 152 with a 47.5% male and 52.5% female distribution. The second most frequent type of referral was for cancer accounting for 13.3% of diseases, with females constituting 49% of the cases and males constituting 51%. Among this referral group, 23.3% were 0–17 years of age (53% males and 47% females), 61.2% were 18–59 years of age (43.2% males and 56.8% females), and 15.5% were above the age of 60 (63.6% males and 34.4% females). The most commonly encountered cancer in males and females within the 0–17 year age group was malignant neoplasms of lymphatic and hematopoietic tissue, corresponding to 34.2% of this population. In the 18–59 year age group, the most common cause of referrals for both males and females was malignant neoplasm of the digestive system, occurring in 26.3% (51.8% and 48.2%, respectively). Similarly, malignant neoplasm of the digestive system was the most common cause of referral in both males and females in the above 60 year age group, with an incidence of 48.7%.
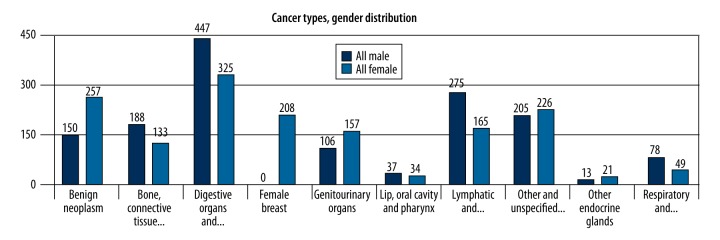
Table 2 summarizes the cause of referral among the different age groups. Cancers reported in the 0–17 year age group include: malignant neoplasms of lymphatic and hematopoietic tissue (34.2%), malignant neoplasms of other and unspecified sites including brain and eye (24.7%), benign neoplasms (14.2%), and malignant neoplasms of bone, connective tissue, and skin (10.7), comprising 83.8% of referrals in this group. In the 15–59 year old category, malignant neoplasms of the digestive system and peritoneum; benign neoplasms; malignant neoplasms of other and unspecified sites including brain and eye; malignant neoplasms of bone, connective tissue, and skin; and breast cancer were the most common reason for referrals, accounting for a total of 72.7% (26.3%, 14.3%, 11.6%, 10.3%, and 10.2% respectively, in descending order of frequency). Malignant neoplasms of the digestive system and peritoneum; malignant neoplasms of bone, connective tissue and skin; malignant neoplasms of the genitourinary system; and benign neoplasms constituted 76.5% of referrals in the above 60 age group (48.8%, 10.5%, 9.9%, and 7.3%, respectively, in descending order of frequency). Stratifying by gender, cancers reported in males and females included: malignant neoplasms of the digestive system and peritoneum (58% and 42%, respectively); malignant neoplasms of lymphatic and hematopoietic tissue (62.5% and 37.5%, respectively); malignant neoplasms of other and unspecified sites including brain and eye (47.6% and 52.4%, respectively); and benign neoplasms (37% and 63%, respectively) (Figure 1).
Table 2.
Types of cancer referrals by age and gender distribution.
| Cancer diagnoses | 0–17 yrs | 18–59 yrs | 60+ yrs | Total | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| M | F | All | M | F | All | M | F | All | |||
| Benign neoplasms | Count | 48 | 54 | 102 | 81 | 189 | 270 | 21 | 14 | 35 | 407 |
| % | 12.60 | 16.00 | 14.17 | 9.90 | 17.63 | 14.31 | 6.70 | 8.54 | 7.35 | 13.20 | |
| Malignant neoplasm of bone, connective tissue, skin | Count | 40 | 37 | 77 | 108 | 86 | 194 | 40 | 10 | 50 | 321 |
| % | 10.50 | 10.90 | 10.69 | 13.30 | 8.02 | 10.28 | 12.82 | 6.10 | 10.50 | 10.41 | |
| Malignant neoplasm of digestive organs and peritoneum | Count | 25 | 19 | 44 | 257 | 239 | 496 | 165 | 67 | 232 | 772 |
| % | 6.50 | 5.60 | 6.11 | 31.50 | 22.30 | 26.29 | 52.90 | 40.90 | 48.74 | 25.04 | |
| Malignant neoplasm of female breast | Count | 0 | 7 | 7 | 0 | 192 | 192 | 0 | 9 | 9 | 208 |
| % | 0.00 | 2.07 | 0.97 | 0.00 | 17.91 | 10.17 | 0.00 | 5.49 | 1.89 | 6.75 | |
| Malignant neoplasm of genitourinary organs | Count | 24 | 20 | 44 | 54 | 118 | 172 | 28 | 19 | 47 | 263 |
| % | 6.30 | 5.90 | 6.11 | 6.60 | 11.00 | 9.11 | 9.00 | 11.60 | 9.87 | 8.53 | |
| Malignant neoplasm of lip, oral cavity and pharynx | Count | 6 | 5 | 11 | 25 | 21 | 46 | 6 | 8 | 14 | 71 |
| % | 1.60 | 1.50 | 1.53 | 3.10 | 2.00 | 2.44 | 1.90 | 4.90 | 2.94 | 2.30 | |
| Malignant neoplasm of lymphatic and hematopoietic tissue | Count | 153 | 93 | 246 | 101 | 67 | 168 | 21 | 5 | 26 | 440 |
| % | 40.10 | 27.50 | 34.17 | 12.40 | 6.30 | 8.90 | 6.70 | 3.00 | 5.46 | 14.27 | |
| Malignant neoplasm of other and unspecified sites (brain, eye) | Count | 77 | 101 | 178 | 112 | 107 | 219 | 16 | 18 | 34 | 431 |
| % | 20.20 | 29.90 | 24.72 | 13.70 | 10.00 | 11.61 | 5.10 | 11.00 | 7.14 | 13.98 | |
| malignant neoplasm of other endocrine glands | Count | 0 | 0 | 0 | 10 | 16 | 26 | 3 | 5 | 8 | 34 |
| % | 0.00 | 0.00 | 0.00 | 1.20 | 1.50 | 1.38 | 1.00 | 3.00 | 1.68 | 1.10 | |
| Malignant neoplasm of respiratory and intrathoracic organs | Count | 9 | 2 | 11 | 66 | 38 | 104 | 12 | 9 | 21 | 136 |
| % | 2.40 | 0.60 | 1.53 | 8.10 | 3.50 | 5.51 | 3.80 | 5.50 | 4.41 | 4.41 | |
| Total | Count | 382 | 338 | 720 | 815 | 1072 | 1887 | 312 | 164 | 476 | 3083 |
| % | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 | |
| % within Total | 12.39 | 10.96 | 23.35 | 26.44 | 34.77 | 61.21 | 10.12 | 5.32 | 15.44 | 100.00 | |
Figure 1.
Types of cancer by gender distribution.
Discussion
Non Communicable Diseases (NCDs), which notably encompass the spectrum of cancers, are viewed with urgency in undeveloped and developing countries [4,5] and can pose enormous challenges in the setting of humanitarian efforts. The prevalence of all NCDs, including cancer, have generally been found to be higher in middle-income in comparison to lower-income populations [7]. The long-term consequences of neglecting to address these diseases are various and involve reduction in quality of life, monetary productivity, and treatment expenditure.
This study provides basic demographic and clinical data for the cancer profile of refugees in Iran, mainly of Afghan origin, between the years 2005 to 2011, and serves as a comparison for related studies in the field. Our study reinforces the evidence that cancer is an important public health problem in the refugee setting, and becomes more prominent with respect to the scarce data existing for the refugee population afflicted with cancer [3,8–13]. Reported cancers were categorized by age groups and gender, and comprised of referrals made to the UNHCR on the basis of required, extended monetary support for acquisition of treatment. The assessment of incidence and prevalence of cancer in refugees is limited by displacement status, limited access to regular healthcare, and lack of a universal registry system in this population. A PubMed search of peer-reviewed articles published from January 1993 to July 2014 of cancer diagnoses in refugees identified 7 articles reporting cancers in Afghan, Tibetan, Syrian, Jordanian, and Iraqi refugees (Table 1).
The dearth of health data as a whole is a general challenge in Afghanistan. According to the Afghan Ministry of Public Health in 2011, minimal data exists on the current health status of the Afghani population and on resource allocations in the healthcare sector [14]. The World Health Organization (WHO) has stated that Afghanistan is a country where there is limited knowledge on most causes of mortality and morbidity [15]. Lack of knowledge about cancer treatments, fear of exorbitant treatment expenditure, and lack of familial and social support systems promotes the UNHCR as the only resource for assistance in the country of asylum for many refugees. Hence, the number of reported cancers documented in this study, and presumably other studies, may over-represent the baseline cancer incidence and prevalence in the population in the respective country of origin.
It is well established that refugee populations are typically uninsured and unable to adequately afford the cost of medical expenses, further encumbered by limited access to regular medical follow up. Middle Eastern countries have welcomed millions of refugees in exile, first Afghanis, followed by Iraqis, and now Syrians. As a matter of fact, most of these countries are not participants of the 1951 Refugee Convention. The massive entry of refugees to these countries has posed a substantial burden on the respective host national healthcare systems. Conversely, unfamiliarity with the healthcare system of the host country, inability to seek medical attention due to financial issues or conflicting priorities, and fear of persecution for having an illegal status in the host country are compounding factors leading to significant delays in seeking medical attention, which in turn is responsible for these patients presenting at advanced stages of disease in comparison to national populations. Loss of medical records in the expatriation process further impedes timely management of disease, and often necessitates additional diagnostic studies.
Based on our observations and related findings presented in Table 1, the common cancers reported in the refugee population in Iran were gastrointestinal, genitourinary, hematologic, breast, CNS and eye, and other benign neoplasms. While many cancers could be related to environmental conditions and exposures during war and humanitarian crises, noted by the prevalence of malignant neoplasms of the digestive systems (25%) and lympatic and blood cancers (14%), many cancers were deemed to be preventable or had the potential to be detected at an early stage with routine screening methods such as colonoscopy, fecal occult blood testing, mammography, and pap smears. Tobacco use is rampant among refugees, as is consumption of high fat diets and lifestyle habits not frequently associated with regular exercise, enhancing the risk of many NCDs such as cancers, diabetes, hypertension, and cardiovascular and respiratory diseases [16–19]. Modification of lifestyle habits, expansion of screening health programs in host country medical systems, and incorporation of one-on-one counseling by community outreach workers and healthcare providers are more feasible interventions that should be considered. Further investigations concerning the cost-effectiveness of prevention, follow up methods, and treatment of NCDs are necessary to better evaluate such interventions. Finally, the need for palliative care in refugees in the setting of cancer and other chronic, disabling diseases should be considered.
Several issues in the improvement of refugee cancer care and treatment remain unresolved and merit further elaboration. Expansion of healthcare resources with the capacity to cover treatment expenditures, which led to establishment of UNHCR’s referral guidelines for country offices worldwide [20], as well as the initiation of similar health insurance programs in countries such as Iran should be viewed as revolutionary, considering the substantial burden of NCDs among Afghani refugees in this country [3,21]. Moreover, it is imperative to achieve a balance between addressing primary or emergency situations and secondary or tertiary concerns, the idea being that measures focusing at the primary care level will eventually correspond to a decrease in incidence and progression of cancer, with resultant decreases in treatment costs. Integration of routine screening methods such as colonoscopy, fecal occult blood testing, mammography, and pap smears; in addition to counseling for lifestyle modifications and ancillary services emphasizing increased cancer awareness have important roles in the public health national programs of host countries. Finally, the value of data stratification and appropriate documentation via cancer registry methods should not be underestimated, as this information is limited in the majority of host counties [22] and could greatly improve cancer surveillance and subsequent follow up. Ideally, these registries would be connected between countries to facilitate continuity of care in migrants and forcibly displaced individuals when feasible. Successful implementation of the aforementioned discussions rests upon the ability to secure a constant source of financing to ensure long-term maintenance of care, which otherwise would prove difficult in planning healthcare and prevention programs remaining sustainable beyond 1 year.
Conclusions
The extent of care entailed in cancer diagnoses in the setting of humanitarian crises points to a growing trend towards more costly management of chronic disease, necessitating a multidirectional approach. International partnerships are essential for improvement in cancer surveillance and prevention, service availability, and delivery of the standard of care, in an overall effort to reduce monetary and resource associated burdens. Recommendations to implement effective prevention and management goals in the refugee setting include the evolution of healthcare systems to encompass standard operating procedures, while incorporating innovative financing schemes; balancing primary and emergency needs with expensive secondary and tertiary referral care; development of electronic cancer registries; and the acquisition of secure and sustainable funding sources.
Limitations
As is the case with most retrospective studies, the current study design may be considered inferior to prospective study models. A detailed reporting system regarding mortality and morbidity rates, stages of disease, and the specific type of treatments are not available in the UNHCR database, as this program was not initially designed with intention of research purposes. However, these data provide the first assessment of the largest number of cancer reports in a refugee population thus far.
It is of note that the scarcity of health data for Afghanis in exile renders data collected by UNHCR over the reported 6 years of significant value. Most retrospective studies rely on the accuracy of records or recall of individuals; similarly, the current study relies on accuracy of data entry by the interviewers. Inconsistencies in record keeping in other UNHCR offices did not allow data compilation for the whole country. Equal access of all Afghani refugees and homogeneous distribution of their age in the country were assumptions, based on which referral rates were calculated. There are currently estimated to be more than 2 million unregistered foreigners in Iran [23], mostly of Afghan background, but also inclusive of Iraqi nationals, who were excluded from this study.
Acknowledgments
The authors would like to thank UNHCR Iran and its representative, Sivanka Dhanapala.
The views stated by the authors do not necessarily represent those of their organization.
This manuscript was supported by division of Hematology and Oncology at Texas Tech University of Health Sciences Center, El Paso, TX.
Footnotes
Source of support: This manuscript was supported by division of Hematology and Oncology at Texas Tech University of Health Sciences Center, El Paso, TX
Conflict of interest statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- 1.UNHCR. Background Note on Afghan Refugees in Iran. 2011. [Google Scholar]
- 2.UNHCR. UNHCR global trends 2012. 2012. http://www.unhcr.org/51bacb0f9.html.
- 3.Otoukesh S, Mojtahedzadeh M, Sherzai D, et al. A retrospective study of demographic parameters and major health referrals among Afghan refugees in Iran. Int J Equity Health. 2012;11:82. doi: 10.1186/1475-9276-11-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alleyne G, Binagwaho A, Haines A, et al. the Lancet NCD Action Group. Embedding non-communicable diseases in the post-2015 development agenda. Lancet. 2013;381:566–74. doi: 10.1016/S0140-6736(12)61806-6. [DOI] [PubMed] [Google Scholar]
- 5.Assembly UG. Political declaration of the High-level Meeting of the General Assembly on the Prevention and Control of Non-communicable Diseases; 2011. [Google Scholar]
- 6.Chapple A, Ziebland S, McPherson A. Stigma, shame, and blame experienced by patients with lung cancer: a qualitative study. BMJ. 2004;328(7454):1470. doi: 10.1136/bmj.38111.639734.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mowafi H, Spiegel P. The Iraqi refugee crisis: familiar problems and new challenges. JAMA. 2008;299:1713–15. doi: 10.1001/jama.299.14.1713. [DOI] [PubMed] [Google Scholar]
- 8.Mateen FJ, Carone M, Al-Saedy H, et al. Cancer diagnoses in Iraqi refugees. Acta Oncol. 2012;51:950–51. doi: 10.3109/0284186X.2012.667148. [DOI] [PubMed] [Google Scholar]
- 9.Spiegel P, Khalifa A, Mateen FJ. Cancer in refugees in Jordan and Syria between 2009 and 2012: challenges and the way forward in humanitarian emergencies. Lancet. 2014;15(7):e290–97. doi: 10.1016/S1470-2045(14)70067-1. [DOI] [PubMed] [Google Scholar]
- 10.Doocy S, Sirois A, Tileva M. Chronic disease and disability among Iraqi populations displaced in Jordan and Syria. Int J Health Plann Manage. 2013;28:e1–12. doi: 10.1002/hpm.2119. [DOI] [PubMed] [Google Scholar]
- 11.Khan SM, Gillani J, Nasreen S, Zai S. Pediatric tumors in north west Pakistan and Afghan refugees. Pediatr Hematol Oncol. 1997;14:267–72. doi: 10.3109/08880019709009496. [DOI] [PubMed] [Google Scholar]
- 12.Khan SM, Gillani J, Nasreen S, Zai S. Cancer in north west Pakistan and Afghan refugees. J Pak Med Assoc. 1997;47:122–24. [PubMed] [Google Scholar]
- 13.Bhatia S1, Dranyi T, Rowley D. A social and demographic study of Tibetan refugees in India. Soc Sci Med. 2002;54:411–22. doi: 10.1016/s0277-9536(01)00040-5. [DOI] [PubMed] [Google Scholar]
- 14.Carvalho N, Salehi AS, Goldie SJ. National and sub-national analysis of the health benefits and cost-effectiveness of strategies to reduce maternal mortality in Afghanistan. Health Policy Plan. 2013;28(1):62–74. doi: 10.1093/heapol/czs026. [DOI] [PubMed] [Google Scholar]
- 15.World Health Organization. D.o.M.a.H.I., Global Burden of Disease. WHO; http://www.who.int/entity/healthinfo/global_burden_disease/gbd/en/index.html. [Google Scholar]
- 16.McClellan WM, Flanders WD. Risk factors for progressive chronic kidney disease. J Am Soc Nephrol. 2003;14(7 Suppl 2):65–70. doi: 10.1097/01.asn.0000070147.10399.9e. [DOI] [PubMed] [Google Scholar]
- 17.McClellan WM. Epidemiology and risk factors for chronic kidney disease. Med Clin North Am. 2005;89(3):419–45. doi: 10.1016/j.mcna.2004.11.006. [DOI] [PubMed] [Google Scholar]
- 18.Halimi JM. The emerging concept of chronic kidney disease without clinical proteinuria in diabetic patients. Diabetes Metab. 2012;38(4):291–97. doi: 10.1016/j.diabet.2012.04.001. [DOI] [PubMed] [Google Scholar]
- 19.Merkin SS, Coresh J, Roux A, et al. Area socioeconomic status and progressive CKD: the Atherosclerosis Risk in Communities (ARIC) Study. Am J Kidney Dis. 2005;46(2):203–13. doi: 10.1053/j.ajkd.2005.04.033. [DOI] [PubMed] [Google Scholar]
- 20.UNHCR. UNHCR’s principles and guidance for referral health care for refugees and other persons of concern. 2009. http://www.unhcr.org/4b4c4fca9.html.
- 21.UNHCR. A guidance note on health insurance schemes for refugees and other persons of concern to UNHCR. 2012. http://www.unhcr.org/4f7d4cb1342.pdf.
- 22.WHO. Cancer registries. 2013. http://www.emro.who.int/noncommunicable-diseases/information-resources/cancer-registration.html.
- 23.Citizenship, D.o.I.a., Country Guidance Note, Iran. 2013. http://www.immi.gov.au/media/publications/pdf/cgn-iran.pdf.