Abstract
Tenosynovitis of the flexor hallucis longus tendon is a condition typically found in ballet dancers and sometimes in soccer players and is related to chronic overuse. It mostly involves the portion of the tendon behind the ankle joint. However, the portion of the tendon under the sustentaculum tali can also be involved. Open synovectomy requires extensive dissection. We report the technique of arthroscopic synovectomy of the deep portion of the flexor hallucis longus.
The flexor hallucis longus (FHL) is a muscle of the deep posterior compartment of the leg. It arises from the lower two-thirds of the posterior surface of the fibula and the adjacent interosseous membrane. Fibers pass obliquely downward and medially to form the tendon. The tendon passes distally between the lateral and medial tubercles of the talus. Beyond the talus, the tendon enters a fibro-osseous tunnel under the sustentaculum tali.1
Tenosynovitis of the FHL tendon is a condition typically found in ballet dancers and sometimes in soccer players and is related to chronic overuse. A traumatic cause for this situation, such as an ankle sprain, is considered rare.2 The condition commonly involves the portion of the FHL tendon behind the ankle.1, 3, 4, 5 However, the portion of the tendon under the sustentaculum tali can also be involved. In case of failure of conservative treatment, synovectomy is indicated, which is usually performed as an open procedure.2 Open synovectomy requires extensive dissection. We report the technique of arthroscopic synovectomy of the deep portion of the FHL that will minimize the soft-tissue dissection and surgical trauma.
Technique
The patient is prone, and a thigh tourniquet was applied. No arthroscopic pump is used. Posterior ankle endoscopy is performed with the posterolateral and posteromedial portals.6 The posterolateral portal is on the lateral side of the Achilles tendon just above the posterosuperior calcaneal tubercle. The posteromedial portal is at the junction point between the medial edge of the Achilles tendon and the line joining the plantar edge of the first metatarsal and the sustentaculum tali. The portion of the flexor hallucis tendon at the posterior ankle (zone 1) is examined.6, 7 Any inflamed synovium is debrided. The arthroscopic instruments are kept on the lateral side of the FHL tendon, and the ankle is slightly flexed to reduce the risk of neurovascular injury.6, 8 After completion of synovectomy of the posterior ankle, the fibro-osseous orifice between the posterior talar tubercles is identified. A Wissinger rod is inserted through the orifice and enters the fibro-osseous sheath under the sustentaculum tali through the posteromedial portal. If there is constriction at the orifice, a release of the fibrous sheath orifice is needed before insertion of the rod. There should not be any significant resistance during advancement of the rod until the plantar aponeurosis is reached. Excessive force should be avoided when advancing the rod to minimize the risk of injury to the tendons and neurovascular structures of the sole. The rod penetrates the plantar aponeurosis, and the plantar portal is made. The arthroscopic cannula is inserted along the rod. The rod should be held such that accidental dropping of the rod is avoided after the cannula passes through both portals.
The rod is removed, and a 4.0-mm 30° arthroscope (Dyonics; Smith & Nephew, Andover, MA) is inserted. The arthroscopic instrument is introduced through the plantar portal under arthroscopic guidance as the arthroscope is withdrawn from the plantar portal. The instrument will pass through the flexor digitorum brevis muscle and the fascial layer deep to the muscle before the FHL tendon is reached. No debridement should be performed at the fascial layer because the medial plantar nerve lies in this layer.9, 10 The portion of the FHL tendon sheath under the sustentaculum tali (zone 2A) is then reached, and arthroscopic synovectomy can be performed.7, 9, 10 Complete synovectomy of the fibro-osseous tendon sheath, including the medial calcaneal wall and the undersurface of the sustentaculum tali, as well as the plantar medial fibrous sheath, should be performed with an arthroscopic shaver (Smith & Nephew) (Video 1). Postoperatively, the patient is advised on active ankle and foot mobilization and weight-bearing walking as tolerated based on the level of pain.
Discussion
The FHL tendon can be divided into 3 zones.7, 9, 10 Zone 1 is behind the ankle. Zone 2 is from the opening between the talar tubercles to the master knot of Henry. It is subdivided into zone 2A (fibro-osseous tendon sheath under the sustentaculum tali) and zone 2B (fascial tendon sheath distal to the sustentaculum tali). Zone 3 is distal to the master knot of Henry down to the phalangeal insertion. Symptoms associated with FHL pathology can manifest themselves anywhere along its length from the posterior leg to the plantar foot and the hallux.11 The prevalence of FHL tenosynovitis may be higher than previously reported, and this condition should always be considered in the differential diagnosis of posteromedial ankle pain.3 Most reports have focused on zone 1 FHL tenosynovitis. Zone 2 FHL synovitis is an uncommon entity, and magnetic resonance imaging is a useful diagnostic tool (Fig 1). However, clinical correlation is an important factor in interpreting the magnetic resonance imaging scan.12
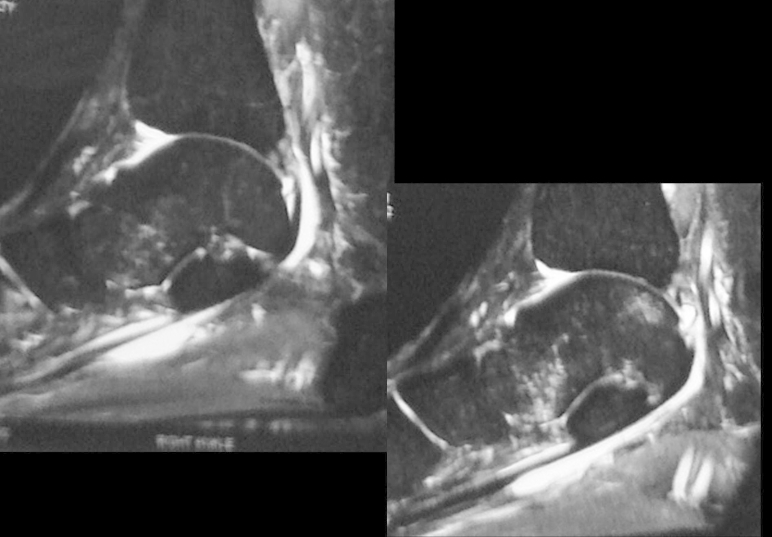
Fig 1.
Magnetic resonance imaging showed extensive tenosynovitis involving both zone 1 and zone 2 of flexor hallucis longus tendon.
Conservative treatment of FHL tenosynovitis includes an FHL stretching program, short-term immobilization, and nonsteroidal anti-inflammatory drugs. Operative decompression and synovectomy are indicated for patients in whom nonoperative treatment has failed.11 Posterior ankle endoscopy is gaining popularity in treating zone 1 FHL tenosynovitis and has proved to be an effective and safe approach.2, 12, 13 It is a minimally invasive surgical procedure that allows good visualization of the involved structures and yields good results.2 This report shows that FHL tendoscopy can be used for arthroscopic synovectomy of a zone 2 FHL tendon sheath. This technique can avoid the extensive soft-tissue dissection that is usually required in an open approach. Zone 2 FHL tendoscopy is a valid approach for synovectomy of the FHL tendon sheath under the sustentaculum tali (Table 1).
Table 1.
Pearls of Arthroscopic Synovectomy for Zone 2 FHL Tenosynovitis
| Both preoperative clinical examination and MRI are important for making the diagnosis. |
| The instruments should be on the lateral side of the FHL tendon during debridement of zone 1 of the FHL tendon. |
| No debridement should be performed at the fascial layer deep to the flexor digitorum brevis muscle. |
| Debridement at the zone 2A FHL tendon sheath is safe because the medial plantar nerve is protected by the fibrous tendon sheath. |
FHL, flexor hallucis longus; MRI, magnetic resonance imaging.
Footnotes
The author reports that he has no conflicts of interest in the authorship and publication of this article.
Supplementary Data
Arthroscopic synovectomy of zone 1 and zone 2 of flexor hallucis longus (FHL) tendon. Zone 1 FHL tendoscopy is performed through the posteromedial and posterolateral portals. Zone 2 FHL tendoscopy is performed through the posteromedial and plantar portals. After the completion of debridement of the posterior ankle, a Wissinger rod is inserted through the zone 2 tendon sheath through the posteromedial portal. The plantar portal is made at the exit point of the rod at the sole. The arthroscopic shaver is inserted into the zone 2 FHL tendon sheath through the plantar portal under arthroscopic guidance.
References
- 1.Purushothaman R., Karuppal R., Valsalan R. Hallux saltans due to flexor hallucis longus entrapment at a previously unreported site in an unskilled manual laborer: A case report. J Foot Ankle Surg. 2012;51:334–336. doi: 10.1053/j.jfas.2012.02.014. [DOI] [PubMed] [Google Scholar]
- 2.Corte-Real N.M., Moreira R.M., Guerra-Pinto F. Arthroscopic treatment of tenosynovitis of the flexor hallucis longus tendon. Foot Ankle Int. 2012;33:1108–1112. doi: 10.3113/FAI.2012.1108. [DOI] [PubMed] [Google Scholar]
- 3.Ogut T., Ayhan E., Irgit K., Sarikaya A.I. Endoscopic treatment of posterior ankle pain. Knee Surg Sports Traumatol Arthrosc. 2011;19:1355–1361. doi: 10.1007/s00167-011-1428-x. [DOI] [PubMed] [Google Scholar]
- 4.Ogut T., Ayhan E. Hindfoot endoscopy for accessory flexor digitorum longus and flexor hallucis longus tenosynovitis. Foot Ankle Surg. 2011;17:e7–e9. doi: 10.1016/j.fas.2010.07.001. [DOI] [PubMed] [Google Scholar]
- 5.Hamilton W.G., Geppert M.J., Thompson F.M. Pain in the posterior aspect of the ankle in dancers. J Bone Joint Surg Am. 1996;78:1491–1500. doi: 10.2106/00004623-199610000-00006. [DOI] [PubMed] [Google Scholar]
- 6.van Dijk C.N., Scholten P.E., Krips R.A. 2-portal endoscopic approach for diagnosis and treatment of posterior ankle pathology. Arthroscopy. 2000;16:871–876. doi: 10.1053/jars.2000.19430. [DOI] [PubMed] [Google Scholar]
- 7.Lui T.H. Flexor hallucis longus tendoscopy: A technical note. Knee Surg Sports Traumatol Arthrosc. 2009;17:107–110. doi: 10.1007/s00167-008-0623-x. [DOI] [PubMed] [Google Scholar]
- 8.Lui T.H. Lateral plantar nerve neuropraxia after FHL tendoscopy: Case report and anatomic evaluation. Foot Ankle Int. 2010;31:828–831. doi: 10.3113/FAI.2010.0828. [DOI] [PubMed] [Google Scholar]
- 9.Lui T.H., Chan K.B., Chan L.K. Zone 2 flexor hallucis longus tendoscopy: A cadaveric study. Foot Ankle Int. 2009;30:447–451. doi: 10.3113/FAI-2009-0447. [DOI] [PubMed] [Google Scholar]
- 10.Lui T.H., Chan K.B., Chan L.K. Cadaveric study of zone 2 flexor hallucis longus tendon sheath. Arthroscopy. 2010;26:808–812. doi: 10.1016/j.arthro.2009.11.007. [DOI] [PubMed] [Google Scholar]
- 11.Michelson J., Dunn L. Tenosynovitis of the flexor hallucis longus: A clinical study of the spectrum of presentation and treatment. Foot Ankle Int. 2005;26:291–303. doi: 10.1177/107110070502600405. [DOI] [PubMed] [Google Scholar]
- 12.Sammarco G.J., Cooper P.S. Flexor hallucis longus tendon injury in dancers and nondancers. Foot Ankle Int. 1998;19:356–362. doi: 10.1177/107110079801900603. [DOI] [PubMed] [Google Scholar]
- 13.Gasparetto F., Collo G., Pisanu G. Posterior ankle and subtalar arthroscopy: Indications, technique, and results. Curr Rev Musculoskelet Med. 2012;5:164–170. doi: 10.1007/s12178-012-9118-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Arthroscopic synovectomy of zone 1 and zone 2 of flexor hallucis longus (FHL) tendon. Zone 1 FHL tendoscopy is performed through the posteromedial and posterolateral portals. Zone 2 FHL tendoscopy is performed through the posteromedial and plantar portals. After the completion of debridement of the posterior ankle, a Wissinger rod is inserted through the zone 2 tendon sheath through the posteromedial portal. The plantar portal is made at the exit point of the rod at the sole. The arthroscopic shaver is inserted into the zone 2 FHL tendon sheath through the plantar portal under arthroscopic guidance.