Abstract
Latissimus dorsi transfer is a reasonable treatment option for massive posterosuperior rotator cuff tears that can substantially improve chronically painful and dysfunctional shoulders. This report and accompanying video describe the treatment of an active 43-year-old man with severe pain and weakness in the right shoulder after 3 failed rotator cuff repairs. Preoperative imaging showed a massive posterosuperior rotator cuff tear retracted to the glenoid as well as a hypermobile os acromiale likely causing dynamic impingement and recurrent rotator cuff tears. After diagnostic arthroscopy, the latissimus tendon is harvested and augmented with a 3-mm human acellular dermal patch (ArthroFlex; Arthrex, Naples, FL). The native rotator cuff tissue is repaired as much as possible, and the latissimus tendon is passed underneath the deltoid and posterior to the teres minor. The patch-augmented tendon is then integrated into a double-row SpeedBridge repair of eight 4.75-mm BioComposite SwiveLock anchors (Arthrex). The bony surface of the os acromiale is prepared and then fixed to the acromion with 2 cannulated partially threaded screws and additional tension-band wiring. Postoperative rehabilitation initially focuses on early passive range of motion, followed by active and active-assisted motion and a biofeedback program starting at 6 weeks postoperatively.
Massive rotator cuff tears usually occur as anterosuperior tears (involving the subscapularis and supraspinatus tendons) or, more commonly, posterosuperior tears (involving the infraspinatus and supraspinatus tendons and sometimes the teres minor tendon). In the absence of glenohumeral osteoarthritis, latissimus dorsi transfer is a treatment option for massive posterosuperior rotator cuff tears that can substantially improve chronically painful, dysfunctional shoulders.1, 2, 3 As a modification, arthroscopically assisted latissimus dorsi transfer can avoid a deltoid-splitting incision, thereby preserving the deltoid muscle, which may lead to a better clinical outcome.2
This report and Video 1 describe the treatment of an active 43-year-old man with severe pain and weakness in the right shoulder after 3 failed rotator cuff repairs elsewhere (2 arthroscopic and, most recently, 1 open). He presented with pain and weakness that resulted in a significant functional deficit. On physical examination, he had a positive external rotation lag sign and a positive drop-arm sign.
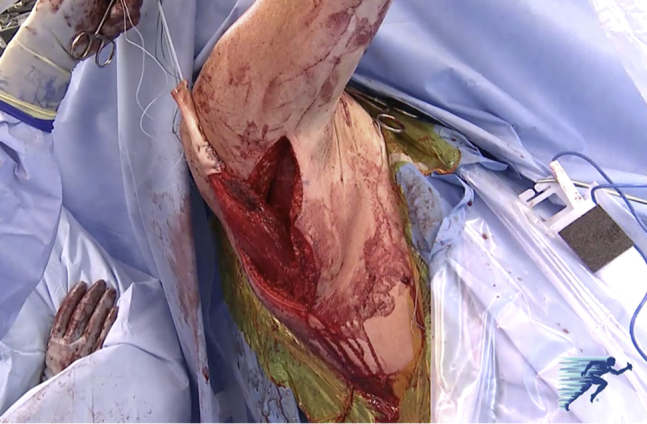
Preoperative imaging showed a massive posterosuperior rotator cuff tear retracted to the glenoid (Fig 1) with no obvious lesion of the subscapularis, as well as a hypermobile os acromiale and tenodesis of the long head of the biceps tendon. Given the patient's young age and good medical condition, as well as the absence of joint space narrowing, he was considered too young for reverse total shoulder replacement. The treatment options included partial rotator cuff repair,4 bridging rotator cuff reconstruction with a graft,5 superior capsular reconstruction,6 or latissimus dorsi tendon transfer. Furthermore, open reduction–internal fixation of the os acromiale was planned because it was considered to be unstable and likely causing dynamic impingement and recurrent rotator cuff tears. Therefore an arthroscopically assisted latissimus approach was not suitable in this case, and an open approach was used; the key surgical risks and technical pearls summarized in Table 1.
Fig 1.
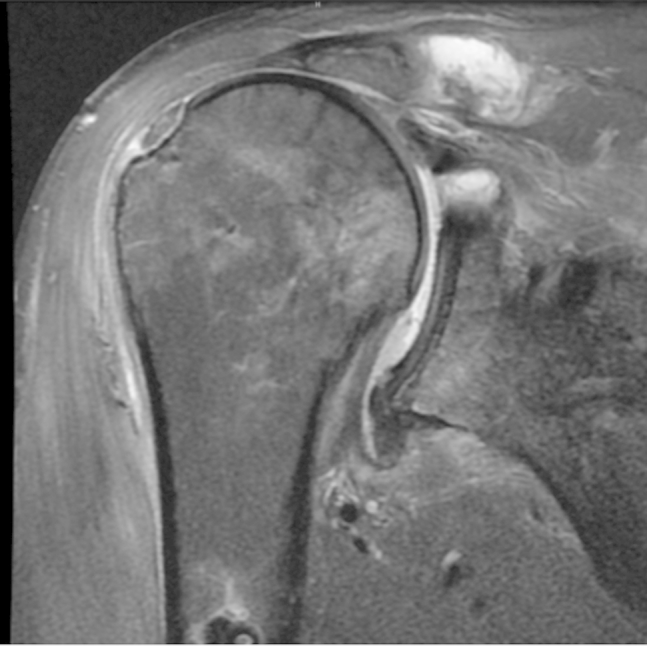
Preoperative magnetic resonance imaging scan (coronal view, T2) showing a massive posterosuperior rotator cuff tear retracted to the glenoid.
Table 1.
Summary of Surgical Risks and Technical Pearls
| Surgical Risks | Technical Pearls |
|---|---|
| Injury to neurovascular pedicle of latissimus dorsi | Sound knowledge of anatomy; meticulous dissection under moderate tension on the previously released latissimus dorsi tendon |
| Insufficient length of latissimus dorsi tendon; over-tensioning | Augmentation of tendon with 3-mm ArthroFlex patch |
| Tear of transferred latissimus dorsi tendon | ORIF of unstable os acromiale to avoid dynamic outlet impingement |
| Secondary dislocation or implant failure of os acromiale ORIF | Combination of cannulated screws and additional tension-band wiring |
| Postoperative weakness with forward flexion and external rotation | Biofeedback program teaching patient how to fire latissimus dorsi muscle for forward flexion and external rotation of shoulder |
ORIF, open reduction–internal fixation.
Surgical Technique
Surgery is performed with the patient under general anesthesia with an additional interscalene nerve catheter. The patient is placed in the modified beach-chair position with a pneumatic arm holder (T-Max Shoulder Positioner and Spider Positioner; Smith & Nephew, Andover, MA), and a fluoroscopic C-arm is draped into the surgical field (Fig 2).
Fig 2.
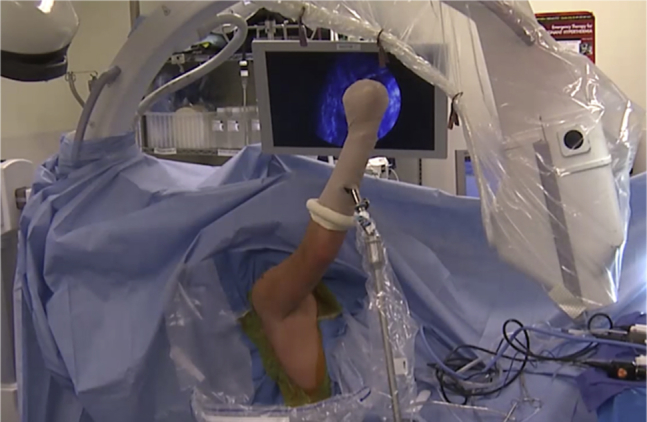
The patient is placed in the modified beach-chair position with a pneumatic arm holder, and a fluoroscopic C-arm is draped into the surgical field.
A standard arthroscopic posterior viewing portal is placed approximately 2 cm medial and 2 cm inferior to the posterolateral corner of the acromion. A standard 30° arthroscope is introduced, and a diagnostic arthroscopy is performed. An anterosuperior working portal is established through the rotator interval, and a low-profile 5-mm × 7-cm cannula (Arthrex, Naples, FL) is inserted to facilitate instrumentation.
An accessory lateral portal is created to mobilize the scarred rotator cuff. A 3.75-mm suction radiofrequency cautery device (Super TurboVac 90; ArthroCare, Austin, TX) is used to perform synovectomy, as well as to release adhesions of the rotator cuff. Because the torn cuff tendons cannot be completely mobilized to the footprint, surgery is extended to a latissimus dorsi tendon transfer with patch augmentation. A deltoid-splitting approach between the anterior and middle heads over the acromion is performed, and the native rotator cuff is tagged with No. 2 sutures (FiberWire; Arthrex) to allow for manipulation. The os acromiale is identified, which is highly unstable and likely causing dynamic outlet impingement.
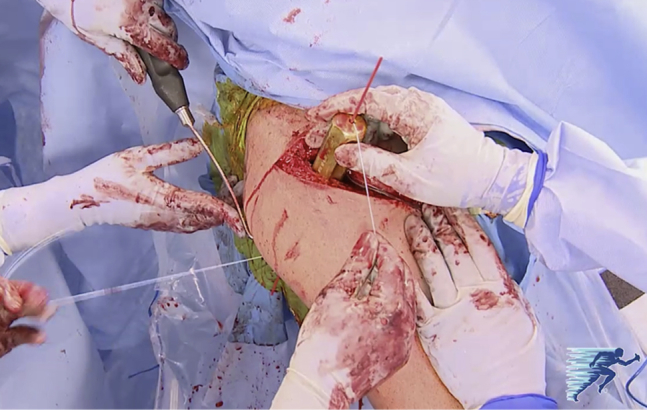
The arm is elevated using the pneumatic arm holder, and a curvilinear incision is made posteriorly and laterally (Fig 3). The latissimus tendon is harvested at its attachment site onto the humerus. The latissimus dorsi muscle belly is entirely freed, and the neurovascular pedicle is identified (Fig 4).
Fig 3.
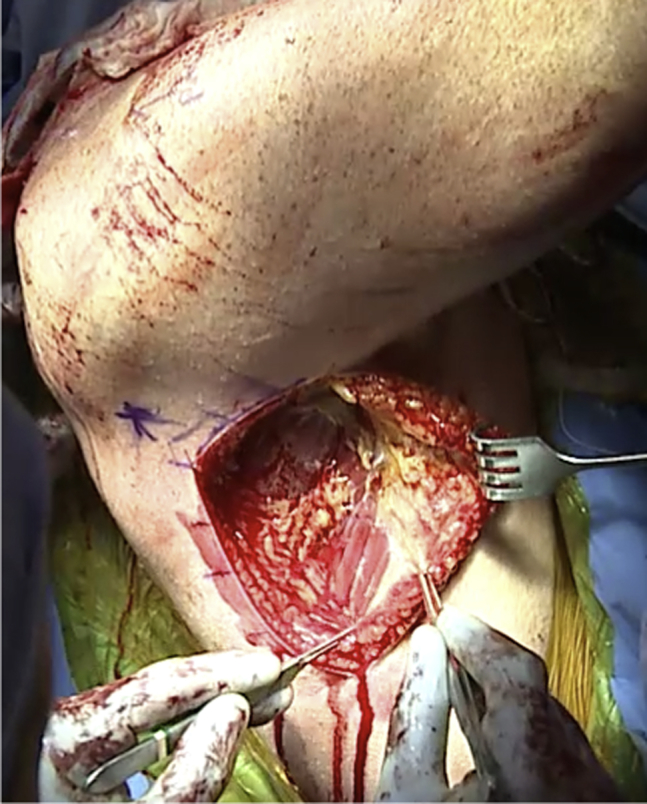
Lateral view of the right shoulder and chest wall. For the harvest of the latissimus dorsi muscle and tendon, the arm is elevated and a curvilinear incision is made posteriorly and laterally following the lateral border of the latissimus dorsi muscle belly.
Fig 4.
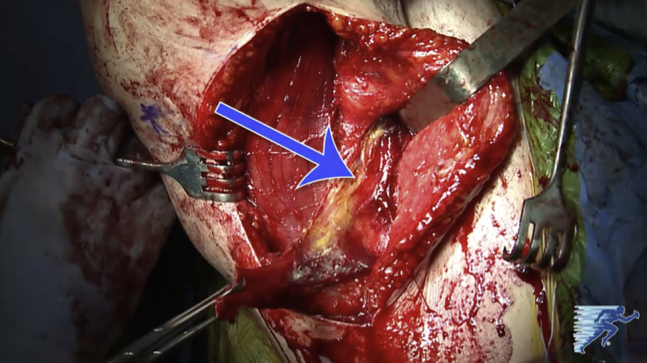
Lateral view of the curvilinear incision for the latissimus dorsi muscle-tendon harvest site on the inferior right shoulder. The arrow indicates the neurovascular pedicle of the latissimus dorsi. To avoid injury to the neurovascular pedicle, sound knowledge of anatomy is crucial. Meticulous dissection of the muscle belly is best performed with slight tension on the previously released tendon.
The latissimus tendon is then augmented with a 3-mm ArthroFlex patch (Arthrex). Locking No. 2 FiberWire sutures are sewn in place, and the patch is oriented to extend medially to allow sewing of it into the native rotator cuff tendon (Fig 5). The muscle-tendon unit is mobilized until the tendon can reach the acromion (Fig 6).
Fig 5.

The latissimus tendon is augmented with a 3-mm ArthroFlex patch. Locking No. 2 FiberWire sutures are sewn in place, and the patch is oriented to extend medially to allow sewing of it into the native rotator cuff tendon.
Fig 6.
The muscle-tendon unit is mobilized until the tendon can reach the acromion to avoid over-tensioning.
A soft-tissue tunnel underneath the deltoid and posterior to the teres minor is created and dilated. This will allow for the latissimus dorsi muscle-tendon unit to pass into the subacromial space and function as an active muscle-tendon unit. A passing suture is placed through the dilator (Fig 7). The graft and latissimus are passed into the subacromial space.
Fig 7.
A passing suture is placed through the dilator to allow for passage of the muscle-tendon unit through a soft-tissue tunnel underneath the deltoid and posterior to the teres minor.
The native rotator cuff tissue is repaired as much as possible with four 4.75-mm BioComposite SwiveLock anchors (Arthrex) loaded with FiberTape (Arthrex) medially. The latissimus graft is tensioned laterally with a second row of cinch sutures and placed onto the lateral aspect of the greater tuberosity. The ArthroFlex patch is then incorporated into the 8-anchor SpeedBridge repair (Arthrex) according to the technique described by van der Meijden et al.,7 passing 8 strands of FiberTape through the patch and the latissimus tendon. The graft is then secured to the native rotator cuff tendons including the teres minor posteriorly and the subscapularis anteriorly with No. 2 FiberWire sutures. The FiberTapes are incorporated into a lateral row of 4.75-mm BioComposite SwiveLock anchors compressing the patch onto the prepared footprint of the greater tuberosity. The final repair shows complete closure of the rotator cuff and complete reattachment of the latissimus to the greater tuberosity (Fig 8).
Fig 8.
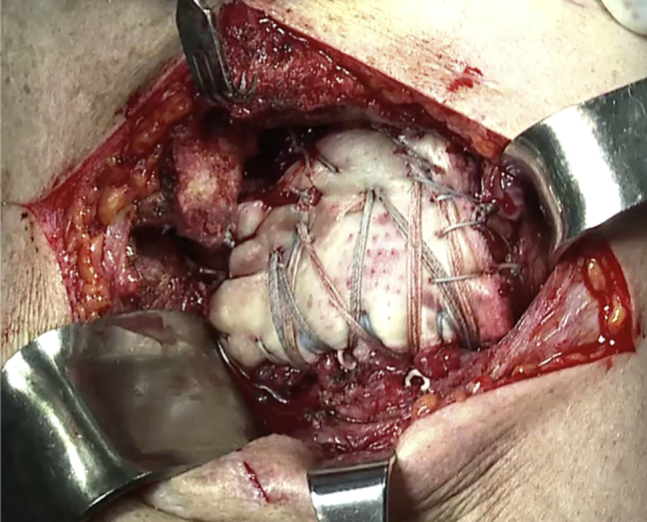
The final repair shows complete closure of the rotator cuff and complete reattachment of the latissimus to the greater tuberosity. The graft is also secured to the native rotator cuff tendons, including the teres minor posteriorly and the subscapularis anteriorly, with No. 2 FiberWire sutures. Stability of the construct is dynamically assessed through a range of motion.
The bony surface on the acromion is prepared, and hypertrophic bone is removed. The os acromiale is then reduced using 2 double-ended K-wires. The pins are overdrilled, and two 3.5-mm cannulated partially threaded screws (Synthes, West Chester, PA) are inserted. Two 18-gauge wires are passed through the screws and over the top of the acromion to resist the inferior bending moment applied by the deltoid. Intraoperative fluoroscopy is used at this point with anteroposterior and oblique views of the acromion.8 Stability of the repair and subcortical placement of hardware are confirmed with digital palpation on the undersurface of the acromion (Fig 9).
Fig 9.

Fluoroscopic anteroposterior view of repair of unstable os acromiale in a right shoulder. A combination of two 3.5-mm cannulated partially threaded screws and additional tension-band wiring with two 18-gauge wires is applied to resist the inferior bending moment applied by the deltoid. The combination of cannulated screws and additional tension-band wiring has shown superior biomechanical results compared with cannulated screws alone.
Postoperatively, the patient starts early passive range of motion with limitations to 30° of external rotation, 90° of abduction, and 120° of forward flexion. At 6 weeks, active and active-assisted motion is begun. A biofeedback program is initiated, teaching the patient how to fire the latissimus dorsi muscle for forward flexion and external rotation of the shoulder.
Discussion
Warner and Parsons1 reported a 73% overall satisfaction rate after latissimus dorsi transfer, with a rerupture rate of 27%. They emphasized that the results of latissimus dorsi transfer as a salvage procedure after failed rotator cuff repair were significantly worse than those of primary procedures.
Similarly, Iannotti et al.9 reported satisfactory results in 64% of patients with irreparable posterosuperior rotator cuff tears. In women, patients with poor shoulder function, and patients with generalized muscle weakness before surgery, less satisfactory clinical results were found postoperatively. Iannotti et al. also emphasized that none of the patients with a poor clinical result showed electrical activity of the latissimus dorsi with active forward flexion or external rotation of the shoulder, showing the importance of appropriate postoperative rehabilitation and biofeedback.
Birmingham and Neviaser10 reported on 18 patients with massive, irreparable rotator cuff tears that were treated with a latissimus dorsi tendon transfer as revisions for failed, previously attempted rotator cuff repairs. The mean American Shoulder and Elbow Surgeons (ASES) score increased from 43 preoperatively to 61 postoperatively (P = .05). This postoperative ASES score is not remarkably good, and the improvement was not significant. Active elevation and active external rotation improved significantly (P < .001), and the average pain level as determined by a visual analog scale significantly decreased from 5.9 points preoperatively to 2.2 points postoperatively (P = .001). The authors concluded that in patients after failed rotator cuff repairs, latissimus transfer as a salvage procedure allowed for a significant return of active elevation and function with minimal postoperative pain. A recently published study conducted by El-Azab et al.11 reported the outcomes of latissimus dorsi transfer in 115 shoulders with a mean duration of follow-up of 9.3 years. At final follow-up, the mean Constant score, ASES score, and pain score on a visual analog scale had all improved. Furthermore, the rate of clinical failure of latissimus dorsi transfer was 10%, and the rate of progression to shoulder replacement after latissimus transfer was 4%. These results suggest that latissimus dorsi transfer is a durable procedure with good long-term outcomes.
Spiegl et al.8 recently compared different techniques of repair for an unstable os acromiale in a biomechanical study, reporting that a combination of cannulated screws and additional tension-band wiring showed significantly higher repair strength compared with cannulated screws alone. Therefore the os acromiale in our patient was repaired accordingly.
In this technical review, we describe a patch-augmented latissimus dorsi transfer and open reduction–internal fixation of an unstable os acromiale for the treatment of an irreparable massive posterosuperior rotator cuff tear. This technique is a more reasonable treatment option than reverse total shoulder arthroplasty in this young individual. The primary benefits of patch-augmented latissimus dorsi transfer include improved biomechanical stability of the repair and muscle transfer, coverage of the rotator cuff defect (Fig 10), and stability to the os acromiale.
Fig 10.
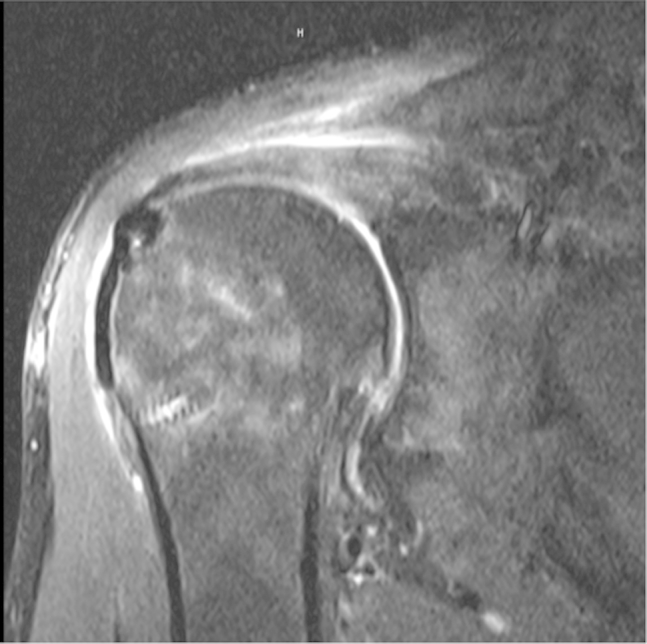
Postoperative magnetic resonance imaging scan (coronal view, T2) showing complete closure of the rotator cuff.
Footnotes
The authors report the following potential conflict of interest or source of funding: M.P., J.A.G., S.B., and P.J.M. receive support from Steadman Philippon Research Institute (SPRI). SPRI receives corporate support from Smith & Nephew, Ossur, Siemens, and Arthrex. M.P. has had his research position at SPRI funded by Arthrex. P.J.M. is a paid consultant for Arthrex and Myos, receives royalties from Arthrex, and has stock or stock options in GameReady and VuMedi.
Supplementary Data
Surgical procedure of patch-augmented latissimus dorsi transfer for a massive irreparable posterosuperior rotator cuff tear in the right shoulder of a 43-year-old man after 3 failed rotator cuff repairs. The patient also had a highly unstable os acromiale, which might have caused dynamic outlet impingement, and therefore also underwent open reduction–internal fixation by combined osteosynthesis with cannulated screws and tension-band wiring.
References
- 1.Warner J.J., Parsons I.M., IV Latissimus dorsi tendon transfer: A comparative analysis of primary and salvage reconstruction of massive, irreparable rotator cuff tears. J Shoulder Elbow Surg. 2001;10:514–521. doi: 10.1067/mse.2001.118629. [DOI] [PubMed] [Google Scholar]
- 2.Millett P.J., Yen Y.M., Huang M.J. Arthroscopically assisted latissimus dorsi transfer for irreparable rotator cuff tears. Tech Shoulder Elbow Surg. 2008;9:76–79. [Google Scholar]
- 3.Gerber C., Rahm S.A., Catanzaro S., Farshad M., Moor B.K. Latissimus dorsi tendon transfer for treatment of irreparable posterosuperior rotator cuff tears: Long-term results at a minimum follow-up of ten years. J Bone Joint Surg Am. 2013;95:1920–1926. doi: 10.2106/JBJS.M.00122. [DOI] [PubMed] [Google Scholar]
- 4.Kim S.J., Kim S.H., Lee S.K., Seo J.W., Chun Y.M. Arthroscopic repair of massive contracted rotator cuff tears: Aggressive release with anterior and posterior interval slides do not improve cuff healing and integrity. J Bone Joint Surg Am. 2013;95:1482–1488. doi: 10.2106/JBJS.L.01193. [DOI] [PubMed] [Google Scholar]
- 5.Gupta A.K., Hug K., Boggess B., Gavigan M., Toth A.P. Massive or 2-tendon rotator cuff tears in active patients with minimal glenohumeral arthritis: Clinical and radiographic outcomes of reconstruction using dermal tissue matrix xenograft. Am J Sports Med. 2013;41:872–879. doi: 10.1177/0363546512475204. [DOI] [PubMed] [Google Scholar]
- 6.Mihata T., Lee T.Q., Watanabe C. Clinical results of arthroscopic superior capsule reconstruction for irreparable rotator cuff tears. Arthroscopy. 2013;29:459–470. doi: 10.1016/j.arthro.2012.10.022. [DOI] [PubMed] [Google Scholar]
- 7.van der Meijden O.A., Wijdicks C.A., Gaskill T.R., Jansson K.S., Millett P.J. Biomechanical analysis of two-tendon posterosuperior rotator cuff tear repairs: Extended linked repairs and augmented repairs. Arthroscopy. 2013;29:37–45. doi: 10.1016/j.arthro.2012.07.012. [DOI] [PubMed] [Google Scholar]
- 8.Spiegl U.J., Smith S.D., Todd J.N., Wijdicks C.A., Millett P.J. Biomechanical evaluation of internal fixation techniques for unstable meso-type os acromiale. J Shoulder Elbow Surg. 2015;24:520–526. doi: 10.1016/j.jse.2014.09.040. [DOI] [PubMed] [Google Scholar]
- 9.Iannotti J.P., Hennigan S., Herzog R. Latissimus dorsi tendon transfer for irreparable posterosuperior rotator cuff tears. Factors affecting outcome. J Bone Joint Surg Am. 2006;88:342–348. doi: 10.2106/JBJS.D.02996. [DOI] [PubMed] [Google Scholar]
- 10.Birmingham P.M., Neviaser R.J. Outcome of latissimus dorsi transfer as a salvage procedure for failed rotator cuff repair with loss of elevation. J Shoulder Elbow Surg. 2008;17:871–874. doi: 10.1016/j.jse.2008.04.007. [DOI] [PubMed] [Google Scholar]
- 11.El-Azab H.M., Rott O., Irlenbusch U. Long-term follow-up after latissimus dorsi transfer for irreparable posterosuperior rotator cuff tears. J Bone Joint Surg Am. 2015;97:462–469. doi: 10.2106/JBJS.M.00235. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Surgical procedure of patch-augmented latissimus dorsi transfer for a massive irreparable posterosuperior rotator cuff tear in the right shoulder of a 43-year-old man after 3 failed rotator cuff repairs. The patient also had a highly unstable os acromiale, which might have caused dynamic outlet impingement, and therefore also underwent open reduction–internal fixation by combined osteosynthesis with cannulated screws and tension-band wiring.


