Abstract
High-flow nasal cannula (HFNC) therapy supports respiratory effort with a minimal elevation in airway pressure. We examined hemodynamic effects of HFNC therapy in a 10-year-old girl with Fontan circulation, in which positive airway pressure has deleterious hemodynamic effects. The HFNC therapy at 30 L/min improved oxygenation without an increase in central venous pressure. It also reduced heart rate, and systemic and pulmonary vascular resistance, and increased cardiac output. In addition, the HFNC therapy improved the cerebral circulation measured by near-infrared spectroscopy. Thus, HFNC therapy may be a potentially useful noninvasive ventilation modality, particularly for patients with Fontan circulation.
Keywords: fontan, ventilation
Introduction
Negative intrathoracic pressure produced by spontaneous breathing is an important driving force for pulmonary blood flow in the Fontan circulation, which is characterized by the lack of the pulmonary ventricle. Therefore, positive-pressure ventilation, including continuous positive airway pressure (CPAP) via the nasal cannula, and conventional mechanical ventilation are thought to be detrimental for the Fontan circulation, because they impede venous return and increase central venous pressure (CVP).
High-flow nasal cannula (HFNC) therapy is a relatively new mode of noninvasive ventilation that is as effective as and better tolerated than CPAP ventilation.1 More importantly, in contrast to CPAP ventilation, HFNC supports respiratory effort with a minimal elevation in airway pressure and, consequently, minimal elevation in intrathoracic pressure.1 This feature of HFNC may be of particular benefit for respiratory support in Fontan patients, in whom positive airway pressure exerts deleterious effects on hemodynamic events. In this case report, we present detailed data regarding the effects of HFNC therapy on Fontan hemodynamics. The patient’s guardian gave written consent for the publication of this report.
Clinical Summary
The patient was a 10-year-old girl (body weight, 34 kg) with tricuspid stenosis and regurgitation, atrial and ventricular septum defect, and patent ductus arteriosus. She underwent pulmonary artery banding at one month of age and subsequent bidirectional Glenn anastomosis at the age of seven months. Thereafter, she underwent Fontan operation at the age of two years. Hemodynamic changes were evaluated before and five minutes after HFNC therapy during follow-up catheterization. Written informed consent for all the procedures during catheterization was obtained from the parents of the patient. HFNC was applied using heated and humidified gas at the flow rate of 30 L/minute with a fraction of inspired oxygen of 0.21 and 0.3. As summarized in Table 1, after induction of HFNC, arterial oxygen saturation increased from 95% to 97% without a change in CVP. A reduction in the heart rate and pulmonary arterial and systemic arterial resistance, with an increase in cardiac output, was also observed. Thirty percent oxygen inhalation further amplified these favorable hemodynamic changes. Changes in the cerebral oxygenation status measured by near-infrared spectroscopy are shown in Figure 1. The tissue oxygenation index and oxygenated hemoglobin level increased after HFNC therapy, indicating improved oxygenation of the brain tissue. In addition, the deoxygenated hemoglobin level decreased, but the normalized tissue hemoglobin index did not alter, indicating an improved cerebral blood flow without congestion.
Table 1.
Hemodynamic changes before and after HFNC therapy.
| BEFORE HFNC | AFTER HFNC (FIO2 AT 21%) | AFTER HFNC (FIO2 AT 30%) | |
|---|---|---|---|
| SaO2 (%) | 95 | 97 | 99 |
| SvO2 (%) | 72 | 83 | 86 |
| Heart rate (bpm) | 85 | 75 | 70 |
| AoP (mmHg) | 146/90 | 145/87 | 138/82 |
| CVP (mmHg) | 11 | 11 | 11 |
| Cardiac index | 2.93 | 4.54 | 4.85 |
| PVR (units × m2) | 1.71 | 1.32 | 1.03 |
| SVR (units × m2) | 32.2 | 22.0 | 19.2 |
Abbreviations: HFNC, high-flow nasal cannula; FiO2, fraction of oxygen; SaO2, arterial oxygen saturation; SvO2, mixed venous oxygen saturation; AoP, aortic pressure; CVP, central venous pressure; PVR, pulmonary vascular resistance; SVR, systemic vascular resistance.
Figure 1.
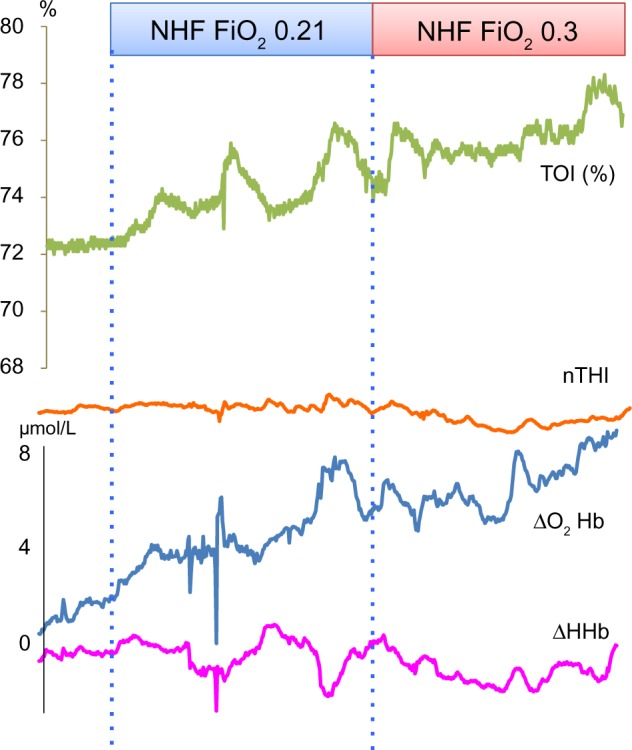
Changes in the cerebral oxygenation measured by near-infrared spectroscopy.
Abbreviations: NHF, nasal high flow; TOI, total oxygen index; nTHI, normalized tissue hemoglobin index; ΔO2Hb, amount of oxygenated hemoglobin change; ΔHHb, amount of deoxygenated hemoglobin change.
Discussion
Several recent studies have reported that HFNC therapy improves oxygenation and provides dyspnea relief and comfort in patients with hypoxemia caused by various conditions.2 However, little information is available regarding the hemodynamic effects of HFNC. HFNC supports respiration through direct delivery of gas at high flow rates into the nasopharynx to create a reservoir of fresh gas and to reduce dead space, rather than through an increase in the end-expiratory pressure to increase lung volumes, and therefore, its effect on CVP should be minimum.1 Both pressure and volume requirements to support gas exchange were lower in HFNC than in conventional mechanical ventilation. In addition, HFNC may be a useful clinical adjunct to respiratory management and may cause minimal damage to Fontan circulation. In our Fontan patient, HFNC at 30 L/minute indeed improved oxygenation without an increase in CVP. It also reduced the heart rate, systemic vascular resistance, and pulmonary vascular resistance and increased the cardiac output. In addition, HFNC improved cerebral circulation, measured by near-infrared spectroscopy.
In the management immediately after the Fontan surgery, early establishment of spontaneous breathing is thought to be beneficial for the enhancement of hemodynamic performance of Fontan circulation through the generation of a negative intrathoracic pressure with inspiration.3 However, in clinical practice, not all patients can achieve extubation immediately after the surgery; furthermore, a rather unstable respiratory condition caused by early extubation exerts untoward effects on the Fontan circulation. As observed in the case of our patient, because HFNC could support respiration with a minimum increase in CVP, it may contribute to the establishment of favorable Fontan circulation immediately after the operation through early extubation. Similarly, HFNC therapy may play a role in the prevention of intubation in Fontan patients who show respiratory failure caused by unexpected events, such as respiratory infection and pleural effusion. Minimum effects of HFNC on CVP may also be beneficial for Fontan cerebral circulation (Fig. 1), because increased CVP in Fontan patients appears to confer increased outflow resistance to the cerebral circulation and thereby impairs cerebral perfusion, as previously reported by Kurishima et al.4 and Saiki et al.5 In addition, increased cardiac output with a reduction in the heart rate, systemic vascular resistance, and pulmonary vascular resistance strongly suggests that HFNC suppresses sympathetic nerve activity, probably through the secondary effects of improved oxygenation.
Other potential advantages of HFNC over other ventilatory modalities are summarized in Table 2. HFNC can be safely and easily applied to individuals belonging to various age groups, ranging from newborns to adults. As compared to CPAP, HFNC rarely causes abdominal distension. In children, sedation may be needed during the application of CPAP and mechanical ventilation, but not during the application of HFNC. During HFNC, patients are able to speak, eat, and receive medications. Nonetheless, several potential disadvantages of HFNC therapy should be acknowledged. HFNC therapy may not be effective in patients with postoperative diaphragmatic paralysis. In the case of patients who show poor response to HFNC, positive-pressure ventilation should be used without any delay in intubation. HFNC allows delivery of up to 60 L/minute of heated and humidified gas; the optimal flow rate needs to be adjusted in a patient-specific manner. Higher flow rates are more effective in improving the oxygenation. In contrast, higher flow rates can cause discomfort to patients and may affect the intrathoracic pressure. Therefore, the optimal flow rate should be adjusted by balancing the abovementioned factors.
Table 2.
Comparison of HFNC with other modalities for ventilatory support.
| NON-INVASIVE | INVASIVE | ||||
|---|---|---|---|---|---|
| HFNC | FM | CPAP | NEEP | CMV | |
| Max FiO2 | 1.0 | 0.5–0.6 | 1.0 | 0.5–0.6 | 1.0 |
| Ventilation effect | DV↓ | – | TV↑ | TV↑ | TV↑ |
| ITP | → ~ ↑ | → | ↑ | → ~ ↓ | ↑ |
| Application | Easy | Easy | Easy | Not easy | Not easy |
| Oral intake | Possible | Possible | Impossible | Impossible | Impossible |
| Discomfort | – | – | + | ++ | +++ |
Abbreviations: HFNC, high-flow nasal cannula; FM, face mask; CPAP, continuous positive airway pressure; NEEP, negative extrathoracic end-expiratory pressure; CMV, conventional mechanical ventilation; Max FiO2, maximum possible fraction of oxygen; ITP, intrathoracic pressure; DV, dead-space volume; TV, tidal volume.
In conclusion, HFNC may be potentially useful, noninvasive ventilation, particularly for patients with Fontan circulation. Further studies in a large number of patients are warranted.
Footnotes
ACADEMIC EDITOR: Thomas E. Vanhecke, Editor in Chief
PEER REVIEW: Five peer reviewers contributed to the peer review report. Reviewers’ reports totaled 570 words, excluding any confidential comments to the academic editor.
FUNDING: Authors disclose no funding sources.
COMPETING INTERESTS: Authors disclose no potential conflicts of interest.
Paper subject to independent expert blind peer review. All editorial decisions made by independent academic editor. Upon submission manuscript was subject to anti-plagiarism scanning. Prior to publication all authors have given signed confirmation of agreement to article publication and compliance with all applicable ethical and legal requirements, including the accuracy of author and contributor information, disclosure of competing interests and funding sources, compliance with ethical requirements relating to human and animal study participants, and compliance with any copyright requirements of third parties. This journal is a member of the Committee on Publication Ethics (COPE).
Author Contributions
Conceived and designed the experiments: SK, JK, H.Senzaki. Analyzed the data: SK, CK, JK, YI. Wrote the first draft of the manuscript: SK. Contributed to the writing of the manuscript: H.Senzaki. Agree with manuscript results and conclusions: SK, CK, JK, YI, H.Saiki, HI, SM, H.Senzaki. Jointly developed the structure and arguments for the paper: SK, CK, JK, YI, H.Saiki, HI, SM, H.Senzaki. Made critical revisions and approved final version: H.Senzaki. All authors reviewed and approved of the final manuscript.
REFERENCES
- 1.Kevin D, Thomas LM, Marla RW, Thomas HS. Research in high flow therapy: mechanisms of action. Respir Med. 2009;103:1400–5. doi: 10.1016/j.rmed.2009.04.007. [DOI] [PubMed] [Google Scholar]
- 2.Roca O, Pérez-Terán P, Masclans JR, et al. Patients with New York Heart Association class III heart failure may benefit with high flow nasal cannula supportive therapy: high flow nasal cannula in heart failure. J Crit Care. 2013;28:741–6. doi: 10.1016/j.jcrc.2013.02.007. [DOI] [PubMed] [Google Scholar]
- 3.Lofland GK. The enhancement of hemodynamic performance in Fontan circulation using pain free spontaneous ventilation. Eur J Cardiothorac Surg. 2001;20:114–8. doi: 10.1016/s1010-7940(01)00757-6. [DOI] [PubMed] [Google Scholar]
- 4.Kurishima C, Tsuda M, Shiima Y, et al. Coupling of central venous pressure and intracranial pressure in a 6-year-old patient with Fontan circulation and intracranial hemorrhage. Ann Thorac Surg. 2011;91:1611–3. doi: 10.1016/j.athoracsur.2010.09.068. [DOI] [PubMed] [Google Scholar]
- 5.Saiki H, Kurishima C, Masutani S, Senzaki H. Cerebral circulation in patients with Fontan circulation: assessment by carotid arterial wave intensity and stiffness. Ann Thorac Surg. 2014;97:1394–9. doi: 10.1016/j.athoracsur.2013.10.079. [DOI] [PubMed] [Google Scholar]


