Abstract
Rift Valley fever virus (RVFV) is an arbovirus circulating between ruminants and mosquitoes to maintain its enzootic cycle. Humans are infected with RVFV through mosquito bites or direct contact with materials of infected animals. The virus causes Rift Valley fever, which was first recognized in the Great Rift Valley of Kenya in 1931. RVFV is characterized by a febrile illness resulting in a high rate of abortions in ruminants and an acute febrile illness, followed by fatal hemorrhagic fever and encephalitis in humans. Initially, the virus was restricted to the eastern region of Africa, but the disease has now spread to southern and western Africa, as well as outside of the African continent, e.g., Madagascar, Saudi Arabia and Yemen. There is a serious concern that the virus may spread to other areas, such as North America and Europe. As vaccination is an effective tool to control RVFV epidemics, formalin-inactivated vaccines and live-attenuated RVFV vaccines have been used in endemic areas. The formalin-inactivated vaccines require boosters for effective protection, whereas the live-attenuated vaccines enable the induction of protective immunity by a single vaccination. However, the use of live-attenuated RVFV vaccines for large human populations having a varied health status is of concern, because of these vaccines’ residual neuro-invasiveness and neurovirulence. Recently, novel vaccine candidates have been developed using replication-defective RVFV that can undergo only a single round of replication in infected cells. The single-cycle replicable RVFV does not cause systemic infection in immunized hosts, but enables the conferring of protective immunity. This review summarizes the properties of various RVFV vaccines and recent progress on the development of the single-cycle replicable RVFV vaccines.
Keywords: Rift Valley fever , vaccines , single-cycle replication , safety , membrane fusion
1. Introduction
Rift Valley fever virus (RVFV), an arbovirus, is the causative agent of Rift Valley fever (RVF), characterized by a febrile illness, resulting in a high rate of abortions in ruminants. In humans, RVFV causes an acute febrile illness followed by fatal hemorrhagic fever, encephalitis, or ocular diseases (Ikegami and Makino, 2011). RVF was first recognized in the Great Rift Valley of Kenya in 1931 (Daubney et al., 1931) after the deaths of lambs and ewes. Initially, the virus was restricted to the eastern region of Africa, but today it has spread to southern and western Africa and also outside of Africa, including Madagascar, Saudi Arabia and Yemen (Bird et al., 2009). The virus periodically causes major epidemics in these countries. Young animals are generally susceptible to the virus infection and show high mortality rates (Bird et al., 2009). Virus infection causes a very high rate of abortions called “abortion storms” in pregnant ruminants, as well as the death of newborns. In the 2007 RVF outbreak in Kenya and Tanzania, approximately 49,000 cattle, goats, and sheep died (Himeidan et al., 2014). RVFV outbreaks have had a significant economic impact due to loss of livestock and the need to curtail livestock trade following outbreaks (Himeidan et al., 2014). Human RVFV infections generally manifest as self-limiting and nonfatal illnesses (Ikegami and Makino, 2011). However, a small number of cases progress to more severe diseases, such as acute hepatitis and delayed-onset encephalitis. In the case of human infection, case fatality rates have varied from 12% to 31% in recent outbreaks (Himeidan et al., 2014). The virus is transmitted by mosquito bites and direct contact with materials from infected animals. Farmers, farm workers, veterinarians, and other health care workers are at high risk for infection, as they handle RVFV-infected animals, e.g., aborted fetal material and body fluids from infected humans. Warm weather, heavy rainfall, and flooding promote breeding of mosquitoes and are often connected to outbreaks (Himeidan et al., 2014). Introduction of RVFV into non-endemic countries, including the U.S., potentially occurs by the movement of infected travelers, animals and, most likely, insect vectors, including mosquitoes (Rolin et al., 2013). RVFV has wide range of vector species, over 30, including mosquito species existing in the U.S. (Turell et al., 2010; Turell et al., 2008). Hence, there is a serious concern that RVFV may be introduced into non-endemic areas and establish infection cycles with resident mosquitoes and domestic animals. The intentional spread of RVFV is also of serious national biosecurity concern. Currently, RVFV is classified as a select agent and belongs to the NIAID Category A list pathogens and the CDC list of potential bioterrorism agents. RVF outbreaks in the non-endemic areas, including the U.S., would cause serious public health, agricultural, and economic problems.
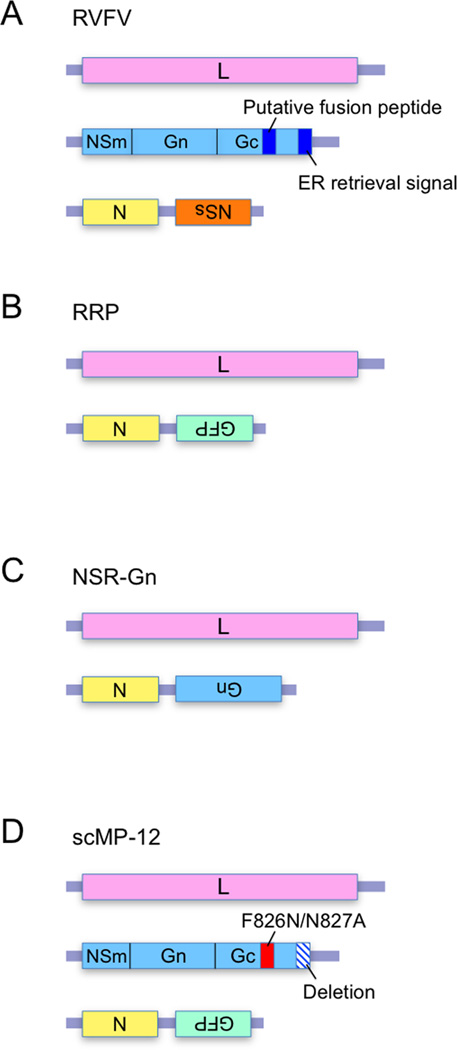
RVFV is a member of the genus Phlebovirus, family Bunyaviridae, and carries negative-stranded, tripartite RNA genomes, comprised of L, M, and S RNA segments (Walter and Barr, 2011). The anti-genomic sense of L RNA encodes RNA-dependent RNA polymerase (L protein). The anti-genomic sense of M RNA carries 5 in-frame start codons, each of which is used for the expression of 78-kDa protein, the nonstructural proteins NSm and NSm’ (Kreher, 2014), and the major glycoproteins Gn and Gc. S RNA uses an ambisense strategy to express nucleocapsid (N) protein and nonstructural protein NSs (Fig. 1A). The RVFV particle consists of the segmented viral RNA genomes, L, N and envelope glycoproteins, and several host proteins (Nuss et al., 2014). The glycoproteins, Gn and Gc, are co-translationally cleaved from a precursor polypeptide and form heterodimers which are arranged into an icosahedral lattice with T=12 symmetry (Freiberg et al., 2008). The virus utilizes DC-SIGN or/and heparin sulfate as one of its entry receptors and gets into the cells via caveola-mediated endocytosis (de Boer et al., 2012a; Harmon et al., 2012; Lozach et al., 2011). RVFV L and N proteins are essential for the viral RNA replication and transcription (Accardi et al., 2001; Ikegami et al., 2005; Lopez et al., 1995). NSs, NSm and 78-kDa proteins are not required for RVFV replication in cultured cells (Gerrard et al., 2007; Ikegami et al., 2006; Won et al., 2006), but play important roles in controlling virus virulence and dissemination in infected hosts (Bird et al., 2007; Kreher, 2014; Muller et al., 1995).
Fig. 1. Schematic diagrams of the anti-genomic sense genomic RNAs of RVFV (A), RRP (B), NSR-Gn (C) and scMP-12 (D).
(A) The putative fusion peptide and the ER retrieval signal in M segment are marked in dark blue. (D) The M RNA segment of scMP-12 has F826N and N827A mutations (red box) and a deletion of the C-terminal ER retrieval signal (a box with diagonal lines).
Although RVFV spread can be prevented by effective vaccination of animals and humans, there are no licensed RVFV vaccines to immunize general citizens in the U.S. and many other countries. There is a substantial body of literature demonstrating that humoral immunity is necessary and sufficient for protection against RVFV (Anderson et al., 1987; Besselaar and Blackburn, 1991; Harrington et al., 1980; Niklasson et al., 1984; Pittman et al., 1999; Peters et al., 1988; Peters et al., 1986; Spik et al., 2006; Schmaljohn et al., 1989; Spik et al., 2006). Also, RVFV is considered to be serologically monotypic (Besselaar et al., 1991; Shope et al., 1980; Tesh et al., 1982). Hence, RVFV vaccines that elicit strong humoral immune responses will be invaluable candidates that are able to induce rapid immune responses against any strain of RVFV. Several different types of RVF vaccine candidates have been developed and tested for their efficacies in protection. This review provides a brief description of attenuated live RVF vaccines, recombinant vaccines based on other viral vectors, and non-replicable RVFV vaccines, including formalin-inactivated RVFV, DNA vaccine, subunit vaccine, and virus-like particle (VLP)-based vaccine. In addition, recent progress in the development of single-cycle replicable RVFV vaccine candidates is highlighted.
2. Live attenuated vaccine candidates
A live-attenuated Smithburn vaccine has been used to control RVF in endemic areas (Bird et al., 2009). The vaccine was developed by serial passages of a wt RVFV, isolated from mosquitoes in Uganda, in mouse brains (Smithburn, 1949). Smithburn vaccine does not cause lethal infection in mice after inoculation via the intraperitoneal (i.p) route (Smithburn, 1949), whereas it has caused hepatocyte necrosis in young and adult goats and abortions in pregnant goats (Kamal, 2009). Abortions were also reported in European-bred ruminants vaccinated with Smithburn vaccine (Botros et al., 2006). These studies implied that Smithburn vaccine is still virulent in ruminants and therefore, is not recommended for use in non-endemic areas.
Clone 13, a naturally occurring attenuated strain isolated by plaque cloning of the RVFV 74HB59 strain, lacks 69% of the NSs gene (Muller et al., 1995). Although the NSs protein is not essential for RVFV replication in cell culture (Billecocq et al., 2008; Habjan et al., 2008; Ikegami et al., 2006), it is a major virulence factor of the virus (Bouloy et al., 2001). NSs suppresses host innate immune functions by inhibiting host RNA synthesis (Le May et al., 2004), including IFNβ mRNA (Le May et al., 2008), and by promoting the degradation of double-stranded RNA-dependent protein kinase (PKR), which mediates the host antiviral responses (Habjan et al., 2009b; Ikegami et al., 2009). Due to large deletions in the NSs gene, clone 13 is highly attenuated in mice (Muller et al., 1995). Vaccination of clone 13 in ruminants did not cause clinical signs, including abortions, and protected the animals from virulent RVFV challenge, suggesting that clone 13 is safe and effective in ruminants (Dungu et al., 2010; von Teichman et al., 2011).
Another attenuated strain, MP-12, was generated by the serial passage of virulent RVFV strain ZH548 in the presence of chemical mutagen, 5-fluorouracil (Caplen et al., 1985). MP-12 encodes a total of 23 mutations (9 amino acid substitutions) (Lokugamage et al., 2012) and is highly attenuated in animals. When viruses, created by reassortment between a virulent RVFV strain and MP-12, were analyzed, it was found that mutations in the M and L segments primarily contributed to attenuation of MP-12 (Billecocq et al., 2008; Saluzzo and Smith, 1990). Vaccination of MP-12 in mice and ruminants demonstrated that MP-12 is safe and elicits high titers of virus-neutralizing antibodies, which are sufficient for protection against virulent RVFV challenge (Bird et al., 2009). Due to the low virulence of MP-12, it is currently the only RVFV strain that can be used in a BSL-2 laboratory, whereas wt RVFV and other RVFV mutants need to be handled in BSL-4 or enhanced BSL-3 labs.
By using reverse genetics systems, several recombinant RVFV mutants were created and tested for their potential as live attenuated vaccines. MP-12-clone 13 is an MP-12-based mutant carrying a clone 13-type large deletion in the NSs gene (Lihoradova et al., 2012). Although MP-12-clone 13 has lower virulence than its parental strain MP-12, its immunogenicity was lower than that of MP-12 (Lihoradova et al., 2012). Lihoradova et al. also generated an MP-12 mutant, rMP12-mPKRN167, carrying a dominant negative form of PKR in place of the NSs gene. The rMP12-mPKRN167 undergoes efficient virus replication by inactivating PKR, but does not suppress host transcription, including IFNβ mRNA synthesis (Lihoradova et al., 2012). rMP12-mPKRN167 showed good protection efficacy from wt RVFV challenge in mice. A recombinant virus, lacking the NSm and NSs genes of the virulent RVFV ZH501 strain, was safe in pregnant ewes and fully protected them from viremia and abortions caused by virulent RVFV challenge (Bird et al., 2011). rMP12-mPKRN167 and ZH501 lacking NSm and NSs genes are ideal for application of the concept of DIVA (Differentiating Infected from Vaccinated Animals), because they lack a specific viral protein(s). Generation of a new type of 35/74 strain-derived virus, RVFV-4s, carrying an L RNA segment, S RNA segment, and 2 separated M segments, one expressing NSm and Gn proteins and the other expressing Gc protein, has been reported (Wichgers Schreur et al., 2014). RVFV-4s had attenuated virulence in mice due to inefficient dissemination, but was highly immunogenic and protected all of the immunized mice from virulent RVFV challenge.
An ideal RVF vaccine should be safe for individuals of all ages and physiological status. Furthermore, concerns about residual virulence and reversion of live attenuated RVFV vaccine candidates should be negligible. MP-12 has not been found to kill 5-week-old mice after i.p. inoculation, but it often invades the CNS and replicates efficiently in the brain in younger mice after i.p. inoculation, resulting in the deaths of the infected mice (unpublished data). Furthermore, MP-12 and even attenuated MP-12 lacking NSs causes lethal infections in mice with impaired immune responses after i.p. inoculation (Gommet et al., 2011; Papin et al., 2011). These data indicate the possibility that current, live attenuated RVF vaccine candidates may cause an efficient systemic infection and neurological diseases by invasion into the CNS in genetically predisposed or immunocompromised individuals and/or young children, whose immune systems have not fully developed.
3. RVF vaccines based on other viral platforms
Several recombinant RVFV vaccines have been generated by using other viruses as platforms. Immunization of mice and baboons with a vaccinia virus (VACV)-based vaccine, vCOGnGc expressing Gn and Gc of the wt RVFV ZH501 strain, elicited anti-RVFV neutralizing antibodies (Papin et al., 2011). Importantly, most of the mice, vaccinated with two doses of vCOGnGc, were protected from wt RVFV challenge. vCOGnGcγ expressing human IFN-γ gene and RVFV glycoproteins was constructed to enhance safety, but expression of the human IFN-γ gene appeared to reduce the immune response of the mice to the vCOGnGcγ. Although both rVACVs were deemed safe and induced neutralizing antibodies against RVF, a booster immunization was needed to elicit high levels of neutralizing antibodies and protection against RVFV challenge. A recombinant modified vaccinia virus Ankara (rMVA) was also used for the expression of RVFV Gn/Gc (rMVA-Gn/Gc) and N protein (rMVA-N) (Lopez-Gil et al., 2013). A single dose of the rMVA-Gn/Gc vaccine in mice induced RVFV-neutralizing antibodies and glycoprotein-specific CD8+ T cell responses that completely protected the immunized mice against challenge with RVFV. Prime-boost regimen using rMVA-N vaccine elicited an antibody response against RVFV nucleocapsid protein and partially protected the immunized mice from RVFV challenge. Immunization with rMVA-Gn/Gc did not protect mice lacking the type I IFN receptor, indicating the importance of innate immune responses in providing protection against RVFV infection.
RVFV vaccines based on Newcastle disease virus (NDV) expressing Gn and Gc proteins of M35/74 strain have been reported (Kortekaas et al., 2010). A single immunization of lambs with the NDV-based vaccine was sufficient to induce anti-RVFV- neutralizing antibodies, whereas a prime-booster immunization protocol was needed to elicit neutralizing antibodies in mice and calves. Mice challenged with a lethal dose of RVFV were protected 100% after a homologous prime-boost vaccination regimen.
An adenovirus vector (CAdVax) was used to generate CAdVax-RVF which expresses Gn and Gc proteins of the RVFV ZH548 strain as separate, recombinant proteins (Holman et al., 2009). Although CAdVax-RVF induced high levels of antibodies against RVFV after a single vaccination, antibody titers began to decline after 10 weeks post vaccination. Nevertheless, all immunized mice survived from a lethal dose of wt RVFV challenge. In mice, a prime-boost vaccination with CAdVax-RVF offered long-term protection against lethal RVFV infection. Mice with a pre-existing adenovirus vector immunity were immunized with CAdVax-RVF and then challenged with RVFV. An increase in vaccine dosage seemed to overcome the limitation of a pre-existing immunity to CAdVax in mice. A replication-deficient Chimpanzee adenovirus vector, ChAdOx1, was also tested as an RVFV vaccine candidate (Warimwe et al., 2013). Because the serotype of ChAdOx1 is distinct from that of human adenovirus type 5 (HAdV5), the ChAdOx1 vaccine response is not affected by a pre-existing immune response against HAdV5. Although ChAdOx1 encoding RVFV Gn and Gc glycoproteins was less immunogenic than HAdV5-GnGc encoding the same glycoproteins in BALB/c mice, a single vaccination of mice with each virus elicited neutralizing antibody and a robust CD8+ T cell response and conferred protection from clinical disease and mortality following challenge with wild type RVFV.
Alphavirus-replicon-derived RVF vaccine candidates which express Nsm, Gn and Gc proteins of RVFV ZH501 strain were developed from mosquito and human isolates of Sindbis virus (Heise et al., 2009). A prime-boost vaccination of mice with both vaccine candidates produced anti-RVFV neutralizing antibodies and elicited a protective immune response against RVFV challenge. Although the prime-boost vaccination of sheep also induced neutralizing antibody production, it is unknown if antibody levels are sufficient to protect the immunized sheep from RVFV challenge.
Although many of these vaccine candidates have been shown to elicit protective levels of neutralizing antibodies against RVFV and protection against RVFV challenge, they often require prime-boost vaccinations to offer 100% protection. A pre-existing vector immunity may limit the efficacy of some RVFV vaccines that are based on other viral vectors.
4. Non-replicable RVFV vaccine candidates
4.1. Formalin-inactivated vaccines
A formalin-inactivated vaccine, NDBR 103, was manufactured based on the RVFV Entebbe strain, which was originally isolated from mosquitoes in Uganda (Randall et al., 1962). NDBR 103 was used for immunization of more than 500 human volunteers and was proven safe and immunogenic after three doses of vaccination (Niklasson et al., 1985; Niklasson, 1982). Another formalin-inactivated vaccine, TSI-GSD-200, was produced based on the Entebbe strain for human use, especially for those with a high occupational risk of exposure to the virus (Pittman et al., 1999). Inactivated RVFV vaccines need a booster with a several-months interval to keep good neutralizing antibody titers for maximum protection (Niklasson et al., 1985; Pittman et al., 1999).
4.2. Subunit and DNA vaccines
Humoral immunity, particularly neutralizing antibodies, is known to play a central role in protection against RVFV. As Gn and Gc envelope proteins carry neutralizing epitopes, DNA and subunit vaccines primarily target these envelope proteins to elicit high titers of neutralizing antibodies.
Purified RVFV Gn and/or Gc proteins produced in E.coli, drosophila and baculovirus-based expression systems were tested as subunit vaccines. All mice inoculated with Gn protein or a soluble form of Gn protein by a prime-boost immunization regimen survived after wt RVFV challenge (de Boer et al., 2010; Schmaljohn et al., 1989; Wallace et al., 2006), demonstrating that Gn or a soluble form of Gn alone was sufficient for eliciting neutralization antibodies for protection. However, a single immunization of Gn subunit RVFV vaccine candidates did not achieve 100% protection in mice. DNA constructs encoding the soluble form of Gn protected 80% of mice against lethal RVFV challenge after three doses of the vaccination by gene gun, while expression of murine C3d, a molecular adjuvant, fused with the Gn increased survival rates up to 100%, indicating that C3d improved the protective efficacy of the DNA vaccine (Bhardwaj et al., 2010). Multiple immunizations of DNA or subunit vaccines expressing both Gn and Gc resulted in full protection of mice after virulent RVFV challenge (Lorenzo et al., 2010; Spik et al., 2006). Schmaljohn et al. reported that immunization of mice with subunit vaccine containing both Gn and Gc proteins induced neutralizing antibody titers, which were significantly higher than in mice immunized with Gn subunit vaccine, indicating that Gn and Gc expressed as polyproteins were better immunogens than Gn alone (Schmaljohn et al., 1989). The Gn/Gc subunit vaccine protected all immunized animals from wt RVFV after single-dose immunization (Schmaljohn et al., 1989). Immunogenicity of DNA or subunit vaccines expressing both Gn and Gc proteins varied depending on the selection of which initiation codons to use for expression of M gene products. DNA vaccines which expressed glycoproteins from the 1st or 2nd AUG resulted in lower immunogenicity compared to the vaccine expressing proteins from the 4th AUG (Lorenzo et al., 2010; Spik et al., 2006). On the other hand, expressing proteins from a 2nd AUG by a baculovirus expression system significantly improved the immunogenicity of the vaccine.
In addition to viral envelope proteins, effects of immunity against RVFV N protein for protective efficacy have been tested. Multi-dose (two to four times) immunization with purified N protein or DNA construct encoding N protein elicited antibodies against N protein and partially protected the immunized mice from death or disease caused by virulent RVFV challenge (Boshra et al., 2011; Jansen van Vuren et al., 2010; Lorenzo et al., 2010; Lagerqvist et al., 2009; Wallace et al., 2006), demonstrating that immunization of N protein alone conferred protection. N protein carries epitopes recognized by human CD8+ T cell and elicits memory responses (Xu et al., 2013). Immune responses induced by a vaccine consisting of N protein or a DNA vaccine encoding only N protein generally conferred lower levels of protection from wt RVFV challenge than did those induced by vaccines carrying or expressing Gn/Gc glycoproteins (Jansen van Vuren et al., 2010; Lorenzo et al., 2010; Lagerqvist et al., 2009). Co-immunization of mice with two DNA vaccines, one encoding N protein and the other encoding Gn/Gc proteins, showed that expression of N protein with Gn/Gc proteins did not improve the protective efficacy (Lorenzo et al., 2010).
Overall, in the case of RVF DNA and subunit vaccines, multiple doses of immunization and/or presence of an adjuvant are often required for full protection from wt RVFV challenge, although they are safe vaccine candidates.
4.3. VLP-based vaccine candidates
RVF VLPs carry all or some virus structural proteins and are morphologically similar to infectious RVFV particles; however, they are unable to replicate due to the absence of viral genomes that are required for virus replication. Liu et al. generated RVF VLPs by expressing N, Gn and Gc proteins by using a baculovirus-based expression system. The produced particles, which were 90-120 nm in diameter with a spiky outer layer, were morphologically similar to authentic RVFV particles (Liu et al., 2008). Other groups demonstrated that expression of Gn and Gc proteins by using mammalian expression plasmids resulted in production of VLPs, which were morphologically similar to RVFV particles (de Boer et al., 2010; Mandell et al., 2010). These results showed that N protein was not necessary for the generation of VLP. Expression of viral minigenome RNA, along with N, Gn and Gc proteins, did not affect VLP yields and the abundance of N protein in the VLP (Mandell et al., 2010). In contrast, Piper et al. reported that the expression of S segment-based minigenome containing a Renilla luciferase gene increased VLP yield (Piper et al., 2011). Habjan et al. generated VLP carrying minigenome RNA consisting of Renilla Luciferase flanked by M segment UTRs. Luciferase activity was observed in VLP-inoculated indicator cells expressing L and N proteins, indicating that the minigenome RNA was incorporated into the VLP (Habjan et al., 2009a).
Immunization of mice via the i.p. route with three doses of VLP consisting of RVFV structural proteins and mini genome RNA resulted in neutralizing antibody titers that ranged from 1:250 to 1:1250, and 92% of the immunized mice were protected from wt RVFV challenge (Naslund et al., 2009). To improve immunogenicity, another VLP, named N-VLP, was generated by the co-expression of a RVFV RNA carrying the N gene flanked by the M segment UTR and other viral structural proteins (Pichlmair et al., 2010). A single immunization of N-VLP did not cause any disease in mice and protected the animals from a lethal dose of RVFV. Because low levels of N protein expression occur in VLP-infected cells, these data imply that N protein expression in VLP-infected cells enhanced the immunogenicity. Additionally, the immunogenicity of VLPs produced in a Drosophila cell expression system was also tested in mice (de Boer et al., 2010). Prime-boost, i.p. immunization induced high titers of neutralizing antibodies and protected 100% of the immunized mice from lethal RVFV challenge. Neutralizing antibody titers of the mice immunized with these VLPs were statistically higher than those of mice immunized with a soluble form of Gn, indicating that Gn and Gc expressed as polyproteins were better immunogens than Gn alone. Mandel et al. reported the generation of chimeric VLP containing Gn, Gc and gag protein of Moloney murine leukemia virus and tested for its efficacy as a vaccine (Mandell et al., 2010). Three subcutaneous (s.c.) immunization of mice with chimeric VLP elicited neutralizing antibody titers above 1:640. Although the chimeric VLP carrying Gn/Gc, N and gag proteins and authentic RVFV VLP carrying Gn/Gc and N proteins induced similar neutralizing antibody titers, the chimeric VLP showed better protective efficacy than did the RVFV VLP, indicating that including a gag protein in the chimeric VLP enhanced immunogenicity. The authors also showed that the presence of N protein in the chimeric VLP did not affect neutralizing antibody titers but enhanced protection efficacy from wt RVFV challenge, demonstrating the importance of N protein for the VLP vaccine efficacy. The protective efficacies of these VLPs and single-cycle replicable vaccine candidates are summarized in Table 1.
Table 1.
Protective efficacy of VLP and single-cycle replicable RVFV vaccines in mice
| Reference | Vaccine component |
RVFV strain | Mouse strain | Immunization |
Peak neutralizing antibody titer |
% Protective efficacya |
|||
|---|---|---|---|---|---|---|---|---|---|
| Viral proteins | Viral RNAs | Dosage (number) | Route | Adjuvant | |||||
| VLP-based | |||||||||
| de Boer et al., 2010 | Gn/Gc | M35/74 | BALB/c | 10μg (2) | I.P. | No | 1000b | 100 | |
| Yes | 5000b | 100 | |||||||
| Mandell et al., 2010 | Gn/Gc, gag | MP-12 | BALB/cC | 6μg (3) | S.C. | Yes | >640 | 68 | |
| Gn/Gc | Yes | >640 | 19 | ||||||
| Gn/Gc, N | Yes | >640 | 56 | ||||||
| Naslund et al., 2009 | 78/NSm/Gn/Gc, L, N |
M-UTR with rLuc ORF |
ZH548 | C57BL/6 | 105 particles (3) | I.P. | No | 250 | 50 |
| 106 particles (3) | No | >1250 | 92 | ||||||
| Pichlmair et al., 2010 | 78/NSm/Gn/Gc, L, N |
M-UTR with N protein-ORF |
ZH548 | C57BL/6 | 106 particles (1) | I.P. | No | NT | 100 |
| Single-cycle replicable | |||||||||
| Kortekaas et al., 2011 | 78/NSm/Gn/Gc, L, N |
L, S-GFP | 35/74 | BALB/c | 106 TCID50 (1) | S.C | No | NT | 60 |
| I.M. | NT | 100 | |||||||
| Oreshkova et al., 2013 | 78/NSm/Gn/Gc, L, N |
L, S-Gn | 35/74 | BALB/cAnCrl | 5×105 TCID50 (1) | I.M. | No | 2500b | NT |
| L, S-GFP | BDb | NT | |||||||
| Dodd et al., 2012 | Gn/Gc, L, N | L, S-GFP | ZH501 | C57BL/6 | 104 TCID50 (1) | S.C | No | 320 | 100 |
| L, S-GFP (irradiated) |
40 | 20 | |||||||
| Murakami et al., 2014 | 78/NSm/Gn/Gc, L, N |
L, M with mutation, S-GFP |
MP-12 | CD-1 | 105 pfu (1) | I.M. | No | 1280 (238c) | 89 |
| L, S-GFP | 160 (38c) | 45 | |||||||
Percentage of surviving mice
Estimated titer (read from the graph in the reference)
Mean titer
NT: not tested
BD: below detection limit
5. Single-cycle replicable vaccine candidates
5.1. RVFV replicon particles (RRP)
In contrast to RVFV VLPs that do not carry out viral RNA replication in VLP-infected cells, RVFV replicon particles (RRP, also called non-spreading RVFV [NSR] or virus replicon particle [VRP]) carry viral RNAs that undergo transcription and RNA replication in RRP-infected cells. RRP carries L RNA and S RNA encoding N protein and GFP in place of the NSs gene (S-GFP RNA) (Fig.1B). In RRP-infected cells, incoming L and N proteins initiate the transcription of L and S-GFP RNAs, resulting in the synthesis of L and N proteins, both of which exert viral RNA synthesis. Subsequently, newly synthesized L and N proteins drive further replication and transcription of the viral RNAs, resulting in the efficient accumulation of L and N proteins and GFP. RRP lacks an M RNA segment for envelope protein expression and is unable to produce virus particles from infected cells, resulting in single-cycle replication.
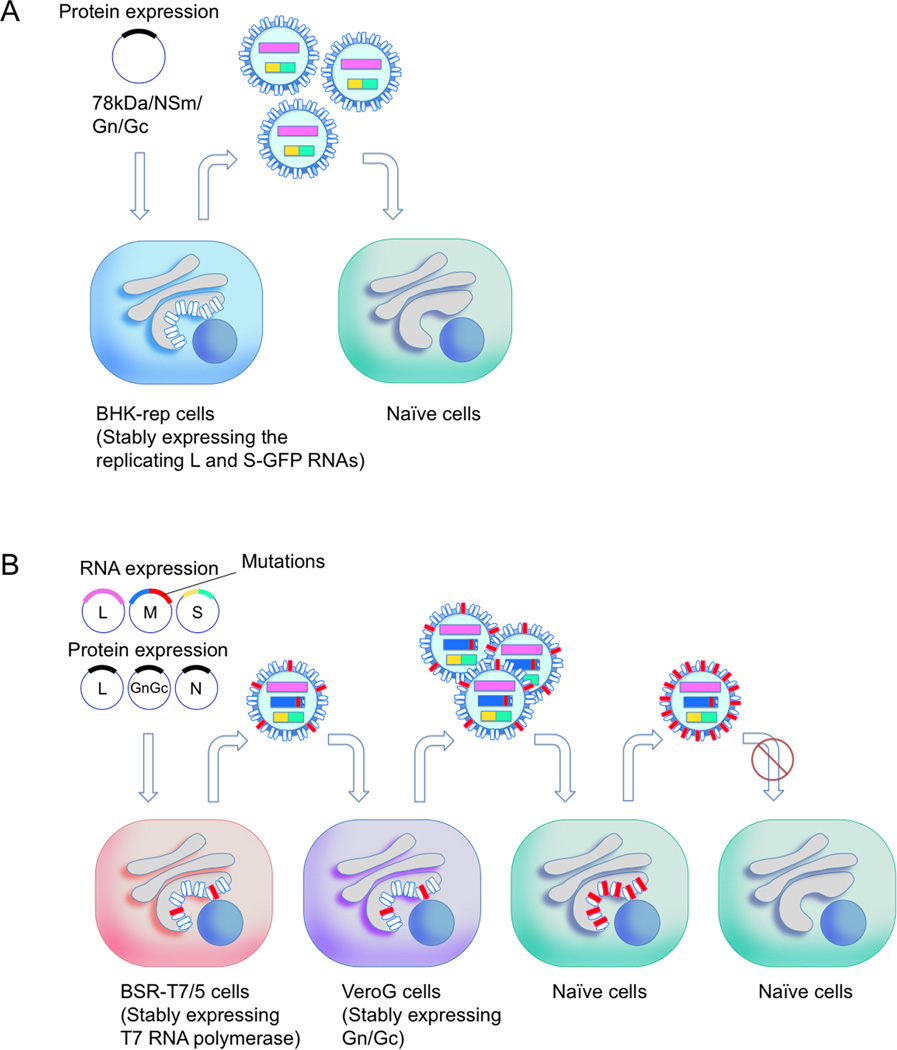
Kortekaas et al. reported the generation and characterization of RRP (Kortekaas et al., 2011). They generated BHK-rep cells stably supporting replication of L and S-GFP RNAs derived from an RVFV virulent strain 35/74 (Fig. 1B). Transfection of the BHK-rep cells with plasmid encoding 78kDa, NSm, Gn and Gc proteins resulted in efficient production of RRPs (Fig. 2A). All of the mice vaccinated with a single dose (106 TCID50) of RRP via the intramuscular (i.m.) route survived the wt RVFV challenge. In addition, vaccination of sheep with RRP elicited the highest neutralizing antibody titers among other vaccine candidates, including inactivated and Gn subunit vaccines and Newcastle disease virus-based recombinant vaccine, which expresses Gn and Gc. The RRP-immunized sheep were protected from diseases caused by wt RVFV challenge (Kortekaas et al., 2012).
Fig. 2. Schematic diagram of RRP (A) and scMP-12 systems (B).
(A) RRP is produced by transfecting plasmid encoding 78kDa/NSm/Gn/Gc proteins into BHK-rep cells stably supporting the replication of L RNA and S-GFP RNA. Inoculation of RRP into naïve cells results in transcription/replication of L and S-GFP RNA and expression of L, N, and GFP proteins. (B) scMP-12 is generated in BSR-T7/5 cells stably expressing T7 polymerase by co-transfection of plasmids, each encoding L, N, and Gn/Gc proteins, L RNA, S RNA and M RNA encoding Gc mutant. Released scMP-12 contains viral RNAs and is competent for initiation of infection, as it carries wt Gn/Gc derived from the protein expression plasmid. scMP-12 is further amplified in Vero-G cells stably expressing wt Gn/Gc. Inoculation of scMP-12 into naïve cells results in viral RNA synthesis, expression of viral proteins, and production of non-infectious VLPs.
The same group generated an improved RRP (NSR-Gn), which carries L RNA and S-Gn RNA encoding N and Gn proteins (Fig. 1C) (Oreshkova et al., 2013). Mice immunized with NSR-Gn elicited significantly higher neutralizing antibody titers than did those immunized with the original RRP, which indicated that Gn protein expression promoted the production of virus-neutralizing antibodies. In lambs immunized with a single dose of NSR-Gn (106.3 TCID50), no virus RNA was detected from liver, brain and plasma samples after wt RVFV challenge, demonstrating that the NSR-Gn conferred sterile immunity in immunized lambs.
Dodd et al. also generated high titers of RRP, which they termed VRP, by co-transfecting T7 promoter-driven plasmids, each expressing Gn/Gc protein, L RNA and S-GFP RNA into BSR-T7/5 cells stably expressing T7 RNA polymerase, and examined VRP’s immunogenicity and protective efficacy (Dodd et al., 2012). Intracranial inoculation of VRP into newborn suckling mice did not cause disease or death, demonstrating its safety. Immunization of mice s.c. with a single dose of VRP (104 TCID50) elicited neutralizing antibody titers of 1:40 to 1:320 and protected 100% of the mice from the wt RVFV challenge, whereas immunization of mice with irradiated VRP (104 TCID50) elicited neutralizing antibody titers from under detection levels to 1:40 and showed 20% protection. These results indicated that replication of viral RNA and viral protein expression in immunized hosts significantly enhanced the protective efficacy of the VRP.
5.2. MP-12-based single-cycle replicable particle (scMP-12)
To improve the safety of MP-12, we have developed an MP-12-based, single-cycle replicable particle, scMP-12, which undergoes single-cycle replication in infected cells and immunized hosts (Murakami et al., 2014). Unlike RRP, scMP-12 carries three viral RNA segments, L RNA, M RNA carrying a mutation in Gc, and S-GFP RNA encoding N protein and GFP (Fig. 1D). The introduced mutation in Gc of scMP-12 abolishes membrane fusion activity, which is essential for the viral genomes to be delivered to the cytoplasm of infected cells, and prevents multiple cycles of scMP-12 replication in infected hosts.
Structural and computational analyses of RVFV glycoproteins predict the presence of a fusion peptide in Gc protein (Dessau and Modis, 2013; Garry and Garry, 2004). It has been hypothesized that acid-triggered conformational change of the Gc protein initiates insertion of the fusion peptide into a host membrane and leads to the fusion of the viral envelope and vesicle membrane. We developed a fusion assay to identify amino acid residue(s) within the putative fusion peptide region that are responsible for the fusion activity. RVFV Gn/Gc proteins accumulate mainly in the Golgi apparatus when they are expressed as a polyprotein in mammalian cells because Gn contains a Golgi targeting signal, and the C-terminal region of Gc has an endodomain carrying a di-lysine-based ER retrieval signal, which most probably prevents the translocation of Gn/Gc to the plasma membrane. The phlebovirus glycoprotein-induced virus-cell membrane fusion requires a low pH environment (Filone et al., 2006). However, exposure of cells expressing Gn/Gc to a low pH condition does not induce cell-to-cell fusion due to the absence of Gn/Gc at the plasma membrane. Removal of the ER retrieval signal in the Gc protein of Uukuniemi virus (a Phlebovirus) results in the accumulation of expressed Gn/Gc at the Golgi apparatus and the plasma membrane (Overby et al., 2007). Accordingly, we targeted Gn/Gc proteins to the plasma membrane by deleting the ER retrieval signal in Gc protein and screened for fusion-incompetent Gn/Gc heterodimers by using a cell-to-cell membrane fusion assay under low pH conditions. Treatment of BSR-T7/5 cells transiently expressing Gn protein, Gc protein lacking the C-terminal ER retrieval signal, and Venus protein with low pH medium induced membrane fusion (Murakami et al., 2014). To estimate the effects of introduced mutations in the fusion peptide on the structural alteration of Gn/Gc proteins, we also performed immunofluorescent staining of the cells expressing Gn and Gc mutants by using an anti-Gn monoclonal antibody and anti-Gc-monoclonal antibody. We identified 6 amino-acid residues that are important for the fusion activity of Gc, while some mutants were not recognized by the anti Gc monoclonal antibody, implying that a mutation altered the conformation of the Gc (Murakami et al., 2014). For subsequent studies, we used a Gc mutant carrying a deletion of the C-terminal ER retrieval signal and F826N and N827A mutations, which abolished membrane fusion and were recognized by anti-Gc and anti-Gn monoclonal antibodies.
An outline of the generation of scMP-12 is shown in Fig. 2B. scMP-12 was rescued by using a modified MP-12 reverse genetics system (Ikegami et al., 2006). Briefly, BSR-T7/5 cells were co-transfected with three RNA-expression plasmids expressing the L RNA, a mutant M RNA encoding F826N and N827A mutations and a deletion of the C-terminal ER retrieval signal, and an S-GFP RNA, as well as three protein expression plasmids encoding the L, N, and wt Gn/Gc proteins. The scMP-12 produced from transfected cells was infectious due to the presence of wt Gn/Gc. Inoculation of the released scMP-12 into Vero-G cells stably expressing wt Gn/Gc resulted in amplification of scMP-12. In naïve cells infected with scMP-12, the expression of L protein, N protein, GFP and the fusion-defective Gn/Gc from the replicating viral RNAs resulted in the production of noninfectious VLPs containing the fusion-defective Gn/Gc. In immunized hosts, scMP-12 particles in the inoculum, viral proteins accumulated in scMP-12-infected cells, and the noninfectious VLPs released from scMP-12-infected cells served as immunogens to elicit immune responses. Due to its characteristic single-cycle replication, the scMP-12 did not cause systemic infection and did invade the CNS of immunized hosts.
Virological characterization of scMP-12 in cultured cells demonstrated that scMP-12 did not undergo multiple cycles of replication in naïve cells, but viral proteins and RNAs were expressed in these scMP-12-infected naïve cells. scMP-12 formed plaques in Vero-G cells, but not in Vero cells. The introduced mutations in the Gc gene of scMP-12 were retained even after 10 passages in Vero-G cells, indicating that scMP-12 was genetically stable. In Vero-G cells, the maximum titer of scMP-12 was ~100 times lower than that of MP-12, implying that scMP-12 particle production was less efficient than MP-12.
We subsequently tested scMP-12 for safety and protective efficacy. All newborn suckling mice survived after an intracranial inoculation with scMP-12, whereas all died after MP-12 inoculation, demonstrating the lack of neurovirulence of scMP-12. Immunization of 5-week-old mice with a single, i.m. dose (105 PFU) of scMP-12 elicited neutralizing antibodies, whose titers were higher than those obtained from mice immunized with the same titer of MP-12- based RRP carrying L RNA and S-GFP RNA. After virulent RVFV challenge, 89% of the mice immunized with scMP-12 survived, whereas 45% of the mice immunized with MP-12-based RRP survived. Overall, immunization of 105 PFU of scMP-12 resulted in an immunogenicity and protective efficacy similar to that seen following administration of 104 PFU of MP-12 to 5-week-old mice. These data demonstrated that scMP-12 was less immunogenic than MP-12, whereas scMP-12 was clearly safer than MP-12 in mouse model systems.
5.3. An approach for improving the production of scMP-12 virus particles
The immunogenicity of scMP-12 was higher than that conferred by MP-12-based RRP, but was lower than MP-12 (Murakami et al., 2014). scMP-12 carrying Gc with F826N and N827A mutations and a deletion of the C-terminal ER retrieval signal produced very low levels of non-infectious particles from infected naïve cells. As non-infectious particles also serve as immunogens in immunized hosts, one approach for improving scMP-12’s immunogenicity would be to enhance the non-infectious particle production from infected naïve cells. We found that F826N mutation and deletion of the C-terminal ER retrieval signal in Gc were detrimental for efficient production of non-infectious virus (unpublished data), and hence, the ER retrieval signal should be retained to improve the production of scMP-12 virus particles.
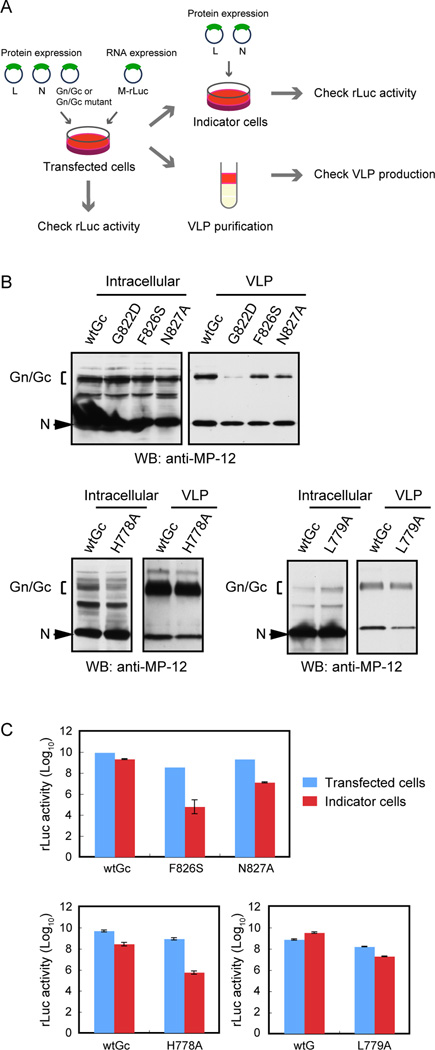
To obtain scMP-12 variants that lack membrane fusion function and are capable of producing large amounts of noninfectious virus particles from infected cells, we generated a series of Gc mutants, each of which carries a single amino-acid substitution within the putative fusion peptide. Because the crystal structure of Gc suggested the possible involvement of L779, which is located outside of the putative fusion peptide, in membrane fusion (Dessau and Modis, 2013), we also generated a Gc mutant carrying an L779A substitution. In addition, we generated several Gc mutants, each carrying a substitution of histidine to alanine mutation at specific sites in Gc, as the importance of several histidine residues of Gc in membrane fusion has been reported (de Boer et al., 2012b). We performed our membrane fusion assay by using plasmids, each of which expresses Gn and Gc mutants having one amino-acid substitution and a deletion of the ER retrieval signal. To know whether the introduced mutation induced a substantial conformational change in the Gc, we also stained expressed Gc mutants by using an anti-Gc monoclonal antibody. Gc mutants, that were defective for membrane fusion and recognized by the anti-Gc monoclonal antibody, were further examined for their VLP production activities (Fig. 3A). To purify VLPs, culture fluid from BSR-T7/5 cells expressing N protein, Gn protein and Gc protein carrying the ER retrieval signal and a specific mutation were collected and subjected to sucrose gradient centrifugation. The purified VLPs were examined by Western blot analysis that used an anti-MP-12 antibody (Fig. 3B). As demonstrated previously (Kortekaas et al., 2011), N protein, which is not associated with VLPs, is released into culture fluid and segmented to fractions containing VLPs in sucrose gradient centrifugation. Therefore, levels of VLP production were evaluated based on the abundance of Gn/Gc proteins in the purified VLPs. The results of these experiments are summarized in Table 2. We identified four Gc mutants having F826S, N827A, H778A, or L779A substitution that had the desired biological properties; they were defective for membrane fusion, recognized by the anti-Gc monoclonal antibody, and competent for efficient VLP production.
Fig. 3. Characterization of VLPs carrying membrane fusion-deficient Gc protein.
(A) An outline of the procedure for examining the infectivity of VLPs. BSR-T7/5 cells were transfected with protein expression plasmids encoding N protein, Gn protein and wt Gc (wtGc) or Gc carrying a specific amino acid substitution and RNA expression plasmid expressing M RNA encoding Renilla luciferase. VLPs released from the transfected cells were purified by sucrose gradient centrifugation or inoculated into indicator cells transiently expressing L and N proteins. Cell lysates of transfected cells and the purified VLPs were subjected to Western blot analysis. Reporter activities in plasmid-transfected cells and in indicator cells were examined at 3 days post transfection and at 24 h post VLP inoculation, respectively. (B) Experiments were performed as described in (A) and purified VLPs, and cell lysates were examined by Western blot analysis by using anti-MP-12 antibody. (C) BSR-T7/5 cells were transfected with plasmids as described in (A). Cell culture medium was collected at day 3 post transfection and inoculated into BSR-T7/5 cells expressing N and L proteins (indicator cells). Luciferase activities in transfected cells at 3 days post translation and in indicator cells at 24 h post VLP-inoculation are shown.
Table 2.
Gn mutants: fusion competence and efficiency of VLP production
| Amino acid sequence (820 to 837) | Fusion competence | Gc mAb recognition |
VLP production | |
|---|---|---|---|---|
| wtGc | GWGCGCFNVNPSCLFVHT | Competent | Positive | ++ |
| G820N | NWGCGCFNVNPSCLFVHT | Competent | NT | NT |
| G820S | SWGCGCFNVNPSCLFVHT | Competent | NT | NT |
| W821N | GNGCGCFNVNPSCLFVHT | Defective | Negative | NT |
| W821R | GRGCGCFNVNPSCLFVHT | Defective | Negative | NT |
| W821S | GSGCGCFNVNPSCLFVHT | Competent | Negative | NT |
| W821D | GDGCGCFNVNPSCLFVHT | Defective | Negative | NT |
| G822S | GWSCGCFNVNPSCLFVHT | Competent | NT | NT |
| G822D | GWDCGCFNVNPSCLFVHT | Defective | Positive | + |
| G822N | GWNCGCFNVNPSCLFVHT | Defective | NT | − |
| C823A | GWGAGCFNVNPSCLFVHT | Defective | Positive | − |
| C823N | GWGNGCFNVNPSCLFVHT | Defective | Positive | − |
| G824D | GWGCDCFNVNPSCLFVHT | Competent | NT | NT |
| C825A | GWGCGAFNVNPSCLFVHT | Defective | Negative | NT |
| F826N | GWGCGCNNVNPSCLFVHT | Defective | Positive | − |
| F826L | GWGCGCLNVNPSCLFVHT | Competent | NT | NT |
| F826S | GWGCGCSNVNPSCLFVHT | Defective | Positive | ++ |
| N827A | GWGCGCFAVNPSCLFVHT | Defective | Positive | ++ |
| V828N | GWGCGCFNNNPSCLFVHT | Competent | Positive | NT |
| P830N | GWGCGCFNVNNSCLFVHT | Competent | Positive | NT |
| H778A | Defective | Positive | ++ | |
| L779A | Defective | Positive | ++ | |
| H857A | NT | NT | − | |
| H857R | Defective | Positive | − | |
| H1087A | NT | NT | + | |
| H1087R | Competent | Positive | NT |
NT : Not tested
− : Under detactable level
We next tested the infectivity of VLP carrying these Gc mutants by using a reporter assay (Fig. 3C). BSR-T7/5 cells transiently expressing viral structural proteins, N, L, Gn and mutant Gc, and the M RNA-based minigenome reporter RNA encoding Renilla luciferase gene. Culture fluids containing VLPs carrying a reporter minigenome were collected at 3 days post-transfection and inoculated into indicator cells expressing L and N proteins. We measured reporter activities in plasmid-transfected cells at 3 days post transfection and in indicator cells at 24 h p.i. (Fig. 3C). In plasmid-transfected cells, the wt sample (wtGc) showed higher reporter activity than did the mutants, which could be due to the ability of the released VLPs in the wt sample to efficiently re-infect cells, resulting in the amplification of the reporter activity. All the Gc mutants were competent for VLP production but showed very low reporter activities in indicator cells (Fig. 3B). We normalized the percentage reporter activity in VLP-inoculated cells to the percentage reporter activity in plasmid-transfected cells and calculated the relative infectivity of the VLP carrying the mutations. The relative infectivity of VLPs carrying single amino acid substitution in Gc, including F826S, N827A, H778A and L779A, were 0.08%, 2.6%, 1% and 3% of the wt sample, respectively. These data indicated the severely impaired fusion activity of these Gc mutants.
These studies identified Gc mutants that were deficient in membrane fusion and competent for VLP production. Testing biological properties, genetic stability, immunogenicity and safety of scMP-12 variants carrying different combinations of these Gc mutations would be valuable for improvement of scMP-12 immunogenicity.
6. Concluding remarks
Since RVFV was first recognized in Kenya in 1931 (Daubney et al., 1931), the virus has been spreading to many countries in the African continent and Arabian Peninsula and has caused death of a substantial number of animals and humans. Recent climate changes and rapid development of global transport network systems will potentially affect the behavior and distribution of insect vectors. As a result, RVFV-free countries will be exposed to a risk of an RVFV outbreak. As summarized above, substantial research efforts have been spent in developing vaccines to control RVFV outbreaks. These efforts contributed to an understanding of not only the mechanism of protection against RVFV but also to the basic knowledge in the field of RVFV virology.
RVFV vaccine candidates, including DNA vaccine, subunit vaccine, and recombinant vaccine based on other viral vectors, achieved protection of animals from lethal RVFV challenge. VLP vaccine, which could be considered efficient forms of subunit vaccines, also elicits protective immunity against RVFV. However, these vaccines often require a booster(s) for full protection against virulent RVFV and for long term immunity, as they do not contain full-set of virus genomes and unable to replicate in vaccinated hosts as infectious RVFV does. Live attenuated viruses, which undergo multiple cycles of replication in immunized hosts, can provoke efficient protective immunity that lasts long term. Hence, attenuated RVFV strains, e.g., MP-12, are promising vaccine candidates; however there are some safety concerns for using them for the general public, including children and immunocompromised individuals.
RRPs can be considered as an intermediate vaccine type between subunit vaccines and live attenuated vaccines in terms of immunogenicity and safety. Their immunogenicity and protective efficacy were significantly better than those of subunit vaccines, and thus, they have excellent potential for becoming immunogenic and safe vaccines for humans and domestic animals. Unlike that for live attenuated virus vaccine, the current production procedure for RRPs requires the transfection of plasmid expressing viral proteins. Hence, the mass production of RRP under current protocols would be expensive and highly labor intensive. Also RRPs produced from cell lines stably supporting L and S-GFP RNAs may have high levels of genetic variations; vaccines carrying highly variable genomes may not be suitable for human use.
Single-cycle, replicable scMP-12 had better immunogenicity and protective efficacy than did MP-12-based RRP. However, there is a possibility that some scMP-12 preparations may carry revertant or pseudorevertant viruses, which undergo multiple cycles of infection in immunized hosts, whereas the production of infectious viruses does not occur in the RRP system. scMP-12 can be easily amplified in Vero-G cells or equivalent cells stably expressing envelope proteins, and yet the titers of scMP-12 replicated in Vero-G cells were lower than MP-12. Modifications to improve the amount of titers of scMP-12 would be needed for its mass production. Additionally, further studies are necessary to improve single-cycle replicable RVFV as a safe and immunogenic vaccine for human and domestic animals.
Highlights.
An overview of the safety and immunogenicity of live attenuated and non-replicable Rift Valley fever virus (RVFV) vaccines
A summary of recent progress in the development of single-cycle replicable RVFV vaccine candidates
An approach towards improving the efficacy of single-cycle replicable RVFV vaccine
Acknowledgments
This work was supported by Public Health Service grant AI101772 from the NIH and a John Sealy Memorial Endowment Fund Research grant from The University of Texas Medical Branch. BRT was supported by NIH Post-Baccalaureate Research Education Program.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Accardi L, Prehaud C, Di Bonito P, Mochi S, Bouloy M, Giorgi C. Activity of Toscana and Rift Valley fever virus transcription complexes on heterologous templates. J. Gen. Virol. 2001;82(Pt 4):781–785. doi: 10.1099/0022-1317-82-4-781. [DOI] [PubMed] [Google Scholar]
- Anderson GW, Jr, Slone TW, Jr, Peters CJ. Pathogenesis of Rift Valley fever virus (RVFV) in inbred rats. Microb. Pathog. 1987;2(4):283–293. doi: 10.1016/0882-4010(87)90126-4. [DOI] [PubMed] [Google Scholar]
- Besselaar TG, Blackburn NK. Topological mapping of antigenic sites on the Rift Valley fever virus envelope glycoproteins using monoclonal antibodies. Arch. Virol. 1991;121(1–4):111–124. doi: 10.1007/BF01316748. [DOI] [PubMed] [Google Scholar]
- Besselaar TG, Blackburn NK, Meenehan GM. Antigenic analysis of Rift Valley fever virus isolates: monoclonal antibodies distinguish between wild-type and neurotropic virus strains. Res. Virol. 1991;142(6):469–474. doi: 10.1016/0923-2516(91)90069-f. [DOI] [PubMed] [Google Scholar]
- Bhardwaj N, Heise MT, Ross TM. Vaccination with DNA plasmids expressing Gn coupled to C3d or alphavirus replicons expressing gn protects mice against Rift Valley fever virus. PLoS Negl Trop Dis. 2010;4(6):e725. doi: 10.1371/journal.pntd.0000725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Billecocq A, Gauliard N, Le May N, Elliott RM, Flick R, Bouloy M. RNA polymerase I-mediated expression of viral RNA for the rescue of infectious virulent and avirulent Rift Valley fever viruses. Virology. 2008;378(2):377–384. doi: 10.1016/j.virol.2008.05.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bird BH, Albarino CG, Nichol ST. Rift Valley fever virus lacking NSm proteins retains high virulence in vivo and may provide a model of human delayed onset neurologic disease. Virology. 2007;362(1):10–15. doi: 10.1016/j.virol.2007.01.046. [DOI] [PubMed] [Google Scholar]
- Bird BH, Ksiazek TG, Nichol ST, Maclachlan NJ. Rift Valley fever virus. J. Am. Vet. Med. Assoc. 2009;234(7):883–893. doi: 10.2460/javma.234.7.883. [DOI] [PubMed] [Google Scholar]
- Bird BH, Maartens LH, Campbell S, Erasmus BJ, Erickson BR, Dodd KA, Spiropoulou CF, Cannon D, Drew CP, Knust B, McElroy AK, Khristova ML, Albarino CG, Nichol ST. Rift Valley fever virus vaccine lacking the NSs and NSm genes is safe, nonteratogenic, and confers protection from viremia, pyrexia, and abortion following challenge in adult and pregnant sheep. J. Virol. 2011;85(24):12901–12909. doi: 10.1128/JVI.06046-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boshra H, Lorenzo G, Rodriguez F, Brun A. A DNA vaccine encoding ubiquitinated Rift Valley fever virus nucleoprotein provides consistent immunity and protects IFNAR−/−) mice upon lethal virus challenge. Vaccine. 2011;29(27):4469–4475. doi: 10.1016/j.vaccine.2011.04.043. [DOI] [PubMed] [Google Scholar]
- Botros B, Omar A, Elian K, Mohamed G, Soliman A, Salib A, Salman D, Saad M, Earhart K. Adverse response of non-indigenous cattle of European breeds to live attenuated Smithburn Rift Valley fever vaccine. J. Med. Virol. 2006;78(6):787–791. doi: 10.1002/jmv.20624. [DOI] [PubMed] [Google Scholar]
- Bouloy M, Janzen C, Vialat P, Khun H, Pavlovic J, Huerre M, Haller O. Genetic evidence for an interferon-antagonistic function of rift valley fever virus nonstructural protein NSs. J. Virol. 2001;75(3):1371–1377. doi: 10.1128/JVI.75.3.1371-1377.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caplen H, Peters CJ, Bishop DH. Mutagen-directed attenuation of Rift Valley fever virus as a method for vaccine development. J. Gen. Virol. 1985;66(Pt 10):2271–2277. doi: 10.1099/0022-1317-66-10-2271. [DOI] [PubMed] [Google Scholar]
- Daubney R, Hudson JR, Garnham PC. Enzootic hepatitis or Rift Valley fever. An undescribed virus disease of sheep cattle and man from East Africa. J. Pathol. Bacteriol. 1931;34:545–579. [Google Scholar]
- de Boer SM, Kortekaas J, Antonis AF, Kant J, van Oploo JL, Rottier PJ, Moormann RJ, Bosch BJ. Rift Valley fever virus subunit vaccines confer complete protection against a lethal virus challenge. Vaccine. 2010;28(11):2330–2339. doi: 10.1016/j.vaccine.2009.12.062. [DOI] [PubMed] [Google Scholar]
- de Boer SM, Kortekaas J, de Haan CA, Rottier PJ, Moormann RJ, Bosch BJ. Heparan sulfate facilitates Rift Valley fever virus entry into the cell. J. Virol. 2012a;86(24):13767–13771. doi: 10.1128/JVI.01364-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Boer SM, Kortekaas J, Spel L, Rottier PJ, Moormann RJ, Bosch BJ. Acid-activated structural reorganization of the Rift Valley fever virus Gc fusion protein. J. Virol. 2012b;86(24):13642–13652. doi: 10.1128/JVI.01973-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dessau M, Modis Y. Crystal structure of glycoprotein C from Rift Valley fever virus. Proc. Natl. Acad. Sci. U. S. A. 2013;110(5):1696–1701. doi: 10.1073/pnas.1217780110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dodd KA, Bird BH, Metcalfe MG, Nichol ST, Albarino CG. Single-dose immunization with virus replicon particles confers rapid robust protection against Rift Valley fever virus challenge. J. Virol. 2012;86(8):4204–4212. doi: 10.1128/JVI.07104-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dungu B, Louw I, Lubisi A, Hunter P, von Teichman BF, Bouloy M. Evaluation of the efficacy and safety of the Rift Valley Fever Clone 13 vaccine in sheep. Vaccine. 2010;28(29):4581–4587. doi: 10.1016/j.vaccine.2010.04.085. [DOI] [PubMed] [Google Scholar]
- Filone CM, Heise M, Doms RW, Bertolotti-Ciarlet A. Development and characterization of a Rift Valley fever virus cell-cell fusion assay using alphavirus replicon vectors. Virology. 2006;356(1–2):155–164. doi: 10.1016/j.virol.2006.07.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freiberg AN, Sherman MB, Morais MC, Holbrook MR, Watowich SJ. Three-dimensional organization of Rift Valley fever virus revealed by cryoelectron tomography. J. Virol. 2008;82(21):10341–10348. doi: 10.1128/JVI.01191-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garry CE, Garry RF. Proteomics computational analyses suggest that the carboxyl terminal glycoproteins of Bunyaviruses are class II viral fusion protein (beta-penetrenes) Theor Biol Med Model. 2004;1:10. doi: 10.1186/1742-4682-1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerrard SR, Bird BH, Albarino CG, Nichol ST. The NSm proteins of Rift Valley fever virus are dispensable for maturation, replication and infection. Virology. 2007;359(2):459–465. doi: 10.1016/j.virol.2006.09.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gommet C, Billecocq A, Jouvion G, Hasan M, Zaverucha do Valle T, Guillemot L, Blanchet C, van Rooijen N, Montagutelli X, Bouloy M, Panthier JJ. Tissue tropism and target cells of NSs-deleted rift valley fever virus in live immunodeficient mice. PLoS Negl Trop Dis. 2011;5(12):e1421. doi: 10.1371/journal.pntd.0001421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Habjan M, Penski N, Spiegel M, Weber F. T7 RNA polymerase-dependent and -independent systems for cDNA-based rescue of Rift Valley fever virus. J. Gen. Virol. 2008;89(Pt 9):2157–2166. doi: 10.1099/vir.0.2008/002097-0. [DOI] [PubMed] [Google Scholar]
- Habjan M, Penski N, Wagner V, Spiegel M, Overby AK, Kochs G, Huiskonen JT, Weber F. Efficient production of Rift Valley fever virus-like particles: The antiviral protein MxA can inhibit primary transcription of bunyaviruses. Virology. 2009a;385(2):400–408. doi: 10.1016/j.virol.2008.12.011. [DOI] [PubMed] [Google Scholar]
- Habjan M, Pichlmair A, Elliott RM, Overby AK, Glatter T, Gstaiger M, Superti-Furga G, Unger H, Weber F. NSs protein of rift valley fever virus induces the specific degradation of the double-stranded RNA-dependent protein kinase. J. Virol. 2009b;83(9):4365–4375. doi: 10.1128/JVI.02148-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harmon B, Schudel BR, Maar D, Kozina C, Ikegami T, Tseng CT, Negrete OA. Rift Valley fever virus strain MP-12 enters mammalian host cells via caveola-mediated endocytosis. J. Virol. 2012;86(23):12954–12970. doi: 10.1128/JVI.02242-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrington DG, Lupton HW, Crabbs CL, Peters CJ, Reynolds JA, Slone TW., Jr Evaluation of a formalin-inactivated Rift Valley fever vaccine in sheep. Am. J. Vet. Res. 1980;41(10):1559–1564. [PubMed] [Google Scholar]
- Heise MT, Whitmore A, Thompson J, Parsons M, Grobbelaar AA, Kemp A, Paweska JT, Madric K, White LJ, Swanepoel R, Burt FJ. An alphavirus replicon-derived candidate vaccine against Rift Valley fever virus. Epidemiol. Infect. 2009;137(9):1309–1318. doi: 10.1017/S0950268808001696. [DOI] [PubMed] [Google Scholar]
- Himeidan YE, Kweka EJ, Mahgoub MM, El Rayah el A, Ouma JO. Recent outbreaks of rift valley Fever in East Africa and the middle East. Front Public Health. 2014;2:169. doi: 10.3389/fpubh.2014.00169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holman DH, Penn-Nicholson A, Wang D, Woraratanadharm J, Harr MK, Luo M, Maher EM, Holbrook MR, Dong JY. A complex adenovirus-vectored vaccine against Rift Valley fever virus protects mice against lethal infection in the presence of preexisting vector immunity. Clin Vaccine Immunol. 2009;16(11):1624–1632. doi: 10.1128/CVI.00182-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ikegami T, Makino S. The Pathogenesis of Rift Valley Fever. Viruses. 2011;3(5):493–519. doi: 10.3390/v3050493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ikegami T, Narayanan K, Won S, Kamitani W, Peters CJ, Makino S. Rift Valley fever virus NSs protein promotes post-transcriptional downregulation of protein kinase PKR and inhibits eIF2alpha phosphorylation. PLoS Pathog. 2009;5(2):e1000287. doi: 10.1371/journal.ppat.1000287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ikegami T, Peters CJ, Makino S. Rift valley fever virus nonstructural protein NSs promotes viral RNA replication and transcription in a minigenome system. J. Virol. 2005;79(9):5606–5615. doi: 10.1128/JVI.79.9.5606-5615.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ikegami T, Won S, Peters CJ, Makino S. Rescue of infectious rift valley fever virus entirely from cDNA, analysis of virus lacking the NSs gene, and expression of a foreign gene. J. Virol. 2006;80(6):2933–2940. doi: 10.1128/JVI.80.6.2933-2940.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jansen van Vuren P, Tiemessen CT, Paweska JT. Evaluation of a Recombinant Rift Valley Fever Virus Subunit Nucleocapsid Protein as an Immunogen in Mice and Sheep. The Open Vaccine Journal. 2010;3:114–126. [Google Scholar]
- Kamal SA. Pathological studies on postvaccinal reactions of Rift Valley fever in goats. Virol J. 2009;6:94. doi: 10.1186/1743-422X-6-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kortekaas J, Antonis AF, Kant J, Vloet RP, Vogel A, Oreshkova N, de Boer SM, Bosch BJ, Moormann RJ. Efficacy of three candidate Rift Valley fever vaccines in sheep. Vaccine. 2012;30(23):3423–3429. doi: 10.1016/j.vaccine.2012.03.027. [DOI] [PubMed] [Google Scholar]
- Kortekaas J, de Boer SM, Kant J, Vloet RP, Antonis AF, Moormann RJ. Rift Valley fever virus immunity provided by a paramyxovirus vaccine vector. Vaccine. 2010;28(27):4394–4401. doi: 10.1016/j.vaccine.2010.04.048. [DOI] [PubMed] [Google Scholar]
- Kortekaas J, Oreshkova N, Cobos-Jimenez V, Vloet RP, Potgieter CA, Moormann RJ. Creation of a nonspreading Rift Valley fever virus. J. Virol. 2011;85(23):12622–12630. doi: 10.1128/JVI.00841-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kreher F. The Rift Valley fever accessory proteins NSm and P78/NSm-GN are distinct determinants of virus propagation in vertebrate and invertebrate hosts. Emerg Microbes Infect. 2014;(3):e71. doi: 10.1038/emi.2014.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lagerqvist N, Naslund J, Lundkvist A, Bouloy M, Ahlm C, Bucht G. Characterisation of immune responses and protective efficacy in mice after immunisation with Rift Valley Fever virus cDNA constructs. Virol J. 2009;6:6. doi: 10.1186/1743-422X-6-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le May N, Dubaele S, Proietti De Santis L, Billecocq A, Bouloy M, Egly JM. TFIIH transcription factor, a target for the Rift Valley hemorrhagic fever virus. Cell. 2004;116(4):541–550. doi: 10.1016/s0092-8674(04)00132-1. [DOI] [PubMed] [Google Scholar]
- Le May N, Mansuroglu Z, Leger P, Josse T, Blot G, Billecocq A, Flick R, Jacob Y, Bonnefoy E, Bouloy M. A SAP30 complex inhibits IFN-beta expression in Rift Valley fever virus infected cells. PLoS Pathog. 2008;4(1):e13. doi: 10.1371/journal.ppat.0040013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lihoradova O, Kalveram B, Indran SV, Lokugamage N, Juelich TL, Hill TE, Tseng CT, Gong B, Fukushi S, Morikawa S, Freiberg AN, Ikegami T. The dominant-negative inhibition of double-stranded RNA-dependent protein kinase PKR increases the efficacy of Rift Valley fever virus MP-12 vaccine. J. Virol. 2012;86(14):7650–7661. doi: 10.1128/JVI.00778-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu L, Celma CC, Roy P. Rift Valley fever virus structural proteins: expression, characterization and assembly of recombinant proteins. Virol J. 2008;5:82. doi: 10.1186/1743-422X-5-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lokugamage N, Freiberg AN, Morrill JC, Ikegami T. Genetic subpopulations of Rift Valley fever virus strains ZH548 and MP-12 and recombinant MP-12 strains. J. Virol. 2012;86(24):13566–13575. doi: 10.1128/JVI.02081-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez-Gil E, Lorenzo G, Hevia E, Borrego B, Eiden M, Groschup M, Gilbert SC, Brun A. A single immunization with MVA expressing GnGc glycoproteins promotes epitope-specific CD8+-T cell activation and protects immune-competent mice against a lethal RVFV infection. PLoS Negl Trop Dis. 2013;7(7):e2309. doi: 10.1371/journal.pntd.0002309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez N, Muller R, Prehaud C, Bouloy M. The L protein of Rift Valley fever virus can rescue viral ribonucleoproteins and transcribe synthetic genome-like RNA molecules. J. Virol. 1995;69(7):3972–3979. doi: 10.1128/jvi.69.7.3972-3979.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorenzo G, Martin-Folgar R, Hevia E, Boshra H, Brun A. Protection against lethal Rift Valley fever virus (RVFV) infection in transgenic IFNAR−/−) mice induced by different DNA vaccination regimens. Vaccine. 2010;28(17):2937–2944. doi: 10.1016/j.vaccine.2010.02.018. [DOI] [PubMed] [Google Scholar]
- Lozach PY, Kuhbacher A, Meier R, Mancini R, Bitto D, Bouloy M, Helenius A. DC-SIGN as a receptor for phleboviruses. Cell Host Microbe. 2011;10(1):75–88. doi: 10.1016/j.chom.2011.06.007. [DOI] [PubMed] [Google Scholar]
- Mandell RB, Koukuntla R, Mogler LJ, Carzoli AK, Freiberg AN, Holbrook MR, Martin BK, Staplin WR, Vahanian NN, Link CJ, Flick R. A replication-incompetent Rift Valley fever vaccine: chimeric virus-like particles protect mice and rats against lethal challenge. Virology. 2010;397(1):187–198. doi: 10.1016/j.virol.2009.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muller R, Saluzzo JF, Lopez N, Dreier T, Turell M, Smith J, Bouloy M. Characterization of clone 13, a naturally attenuated avirulent isolate of Rift Valley fever virus, which is altered in the small segment. Am. J. Trop. Med. Hyg. 1995;53(4):405–411. doi: 10.4269/ajtmh.1995.53.405. [DOI] [PubMed] [Google Scholar]
- Murakami S, Terasaki K, Ramirez SI, Morrill JC, Makino S. Development of a novel, single-cycle replicable rift valley Fever vaccine. PLoS Negl Trop Dis. 2014;8(3):e2746. doi: 10.1371/journal.pntd.0002746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naslund J, Lagerqvist N, Habjan M, Lundkvist A, Evander M, Ahlm C, Weber F, Bucht G. Vaccination with virus-like particles protects mice from lethal infection of Rift Valley Fever Virus. Virology. 2009;385(2):409–415. doi: 10.1016/j.virol.2008.12.012. [DOI] [PubMed] [Google Scholar]
- Niklasson B. Rift Valley fever virus vaccine trial: study of side-effects in humans. Scand J. Infect. Dis. 1982;14(2):105–109. doi: 10.3109/inf.1982.14.issue-2.06. [DOI] [PubMed] [Google Scholar]
- Niklasson B, Peters CJ, Bengtsson E, Norrby E. Rift Valley fever virus vaccine trial: study of neutralizing antibody response in humans. Vaccine. 1985;3(2):123–127. doi: 10.1016/0264-410x(85)90061-1. [DOI] [PubMed] [Google Scholar]
- Niklasson BS, Meadors GF, Peters CJ. Active and passive immunization against Rift Valley fever virus infection in Syrian hamsters. Acta Pathol Microbiol Immunol Scand C. 1984;92(4):197–200. doi: 10.1111/j.1699-0463.1984.tb00074.x. [DOI] [PubMed] [Google Scholar]
- Nuss JE, Kehn-Hall K, Benedict A, Costantino J, Ward M, Peyser BD, Retterer CJ, Tressler LE, Wanner LM, McGovern HF, Zaidi A, Anthony SM, Kota KP, Bavari S, Hakami RM. Multi-faceted proteomic characterization of host protein complement of Rift Valley fever virus virions and identification of specific heat shock proteins, including HSP90, as important viral host factors. PLoS One. 2014;9(5):e93483. doi: 10.1371/journal.pone.0093483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oreshkova N, van Keulen L, Kant J, Moormann RJ, Kortekaas J. A single vaccination with an improved nonspreading Rift Valley fever virus vaccine provides sterile immunity in lambs. PLoS One. 2013;8(10):e77461. doi: 10.1371/journal.pone.0077461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Overby AK, Pettersson RF, Neve EP. The glycoprotein cytoplasmic tail of Uukuniemi virus (Bunyaviridae) interacts with ribonucleoproteins and is critical for genome packaging. J. Virol. 2007;81(7):3198–3205. doi: 10.1128/JVI.02655-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papin JF, Verardi PH, Jones LA, Monge-Navarro F, Brault AC, Holbrook MR, Worthy MN, Freiberg AN, Yilma TD. Recombinant Rift Valley fever vaccines induce protective levels of antibody in baboons and resistance to lethal challenge in mice. Proc. Natl. Acad. Sci. U.S.A. 2011;108(36):14926–14931. doi: 10.1073/pnas.1112149108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters CJ, Jones D, Trotter R, Donaldson J, White J, Stephen E, Slone TW., Jr Experimental Rift Valley fever in rhesus macaques. Arch. Virol. 1988;99(1–2):31–44. doi: 10.1007/BF01311021. [DOI] [PubMed] [Google Scholar]
- Peters CJ, Reynolds JA, Slone TW, Jones DE, Stephen EL. Prophylaxis of Rift Valley fever with antiviral drugs, immune serum, an interferon inducer, and a macrophage activator. Antiviral Res. 1986;6(5):285–297. doi: 10.1016/0166-3542(86)90024-0. [DOI] [PubMed] [Google Scholar]
- Pichlmair A, Habjan M, Unger H, Weber F. Virus-like particles expressing the nucleocapsid gene as an efficient vaccine against Rift Valley fever virus. Vector Borne Zoonotic Dis. 2010;10(7):701–703. doi: 10.1089/vbz.2009.0248. [DOI] [PubMed] [Google Scholar]
- Piper ME, Sorenson DR, Gerrard SR. Efficient cellular release of Rift Valley fever virus requires genomic RNA. PLoS One. 2011;6(3):e18070. doi: 10.1371/journal.pone.0018070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pittman PR, Liu CT, Cannon TL, Makuch RS, Mangiafico JA, Gibbs PH, Peters CJ. Immunogenicity of an inactivated Rift Valley fever vaccine in humans: a 12-year experience. Vaccine. 1999;18(1–2):181–189. doi: 10.1016/s0264-410x(99)00218-2. [DOI] [PubMed] [Google Scholar]
- Randall R, Gibbs CJ, Jr, Aulisio CG, Binn LN, Harrison VR. The development of a formalin-killed Rift Valley fever virus vaccine for use in man. J. Immunol. 1962;89:660–671. [PubMed] [Google Scholar]
- Rolin AI, Berrang-Ford L, Kulkarni MA. The risk of Rift Valley fever virus introduction and establishment in the United States and European Union. Emerg. Micro. and Inf. 2013;2:e81. doi: 10.1038/emi.2013.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saluzzo JF, Smith JF. Use of reassortant viruses to map attenuating and temperature-sensitive mutations of the Rift Valley fever virus MP-12 vaccine. Vaccine. 1990;8(4):369–375. doi: 10.1016/0264-410x(90)90096-5. [DOI] [PubMed] [Google Scholar]
- Schmaljohn CS, Parker MD, Ennis WH, Dalrymple JM, Collett MS, Suzich JA, Schmaljohn AL. Baculovirus expression of the M genome segment of Rift Valley fever virus and examination of antigenic and immunogenic properties of the expressed proteins. Virology. 1989;170(1):184–192. doi: 10.1016/0042-6822(89)90365-6. [DOI] [PubMed] [Google Scholar]
- Shope RE, Peters CJ, Walker JS. Serological relation between Rift Valley fever virus and viruses of phlebotomus fever serogroup. Lancet. 1980;1(8173):886–887. doi: 10.1016/s0140-6736(80)91395-1. [DOI] [PubMed] [Google Scholar]
- Smithburn KC. Rift Valley fever; the neurotropic adaptation of the virus and the experimental use of this modified virus as a vaccine. Br. J. Exp. Pathol. 1949;30(1):1–16. [PMC free article] [PubMed] [Google Scholar]
- Spik K, Shurtleff A, McElroy AK, Guttieri MC, Hooper JW, SchmalJohn C. Immunogenicity of combination DNA vaccines for Rift Valley fever virus, tick-borne encephalitis virus, Hantaan virus, and Crimean Congo hemorrhagic fever virus. Vaccine. 2006;24(21):4657–4666. doi: 10.1016/j.vaccine.2005.08.034. [DOI] [PubMed] [Google Scholar]
- Tesh RB, Peters CJ, Meegan JM. Studies on the antigenic relationship among phleboviruses. Am. J. Trop. Med. Hyg. 1982;31(1):149–155. doi: 10.4269/ajtmh.1982.31.149. [DOI] [PubMed] [Google Scholar]
- Turell MJ, Dohm DJ, Mores CN, Terracina L, Wallette DL, Jr, Hribar LJ, Pecor JE, Blow JA. Potential for North American mosquitoes to transmit Rift Valley fever virus. J. Am. Mosq. Control Assoc. 2008;24(4):502–507. doi: 10.2987/08-5791.1. [DOI] [PubMed] [Google Scholar]
- Turell MJ, Wilson WC, Bennett KE. Potential for North American mosquitoes (Diptera: Culicidae) to transmit rift valley fever virus. J. Med. Entomol. 2010;47(5):884–889. doi: 10.1603/me10007. [DOI] [PubMed] [Google Scholar]
- von Teichman B, Engelbrecht A, Zulu G, Dungu B, Pardini A, Bouloy M. Safety and efficacy of Rift Valley fever Smithburn and Clone 13 vaccines in calves. Vaccine. 2011;29(34):5771–5777. doi: 10.1016/j.vaccine.2011.05.055. [DOI] [PubMed] [Google Scholar]
- Wallace DB, Ellis CE, Espach A, Smith SJ, Greyling RR, Viljoen GJ. Protective immune responses induced by different recombinant vaccine regimes to Rift Valley fever. Vaccine. 2006;24(49–50):7181–7189. doi: 10.1016/j.vaccine.2006.06.041. [DOI] [PubMed] [Google Scholar]
- Walter CT, Barr JN. Recent advances in the molecular and cellular biology of bunyaviruses. J. Gen. Virol. 2011;92(Pt 11):2467–2484. doi: 10.1099/vir.0.035105-0. [DOI] [PubMed] [Google Scholar]
- Warimwe GM, Lorenzo G, Lopez-Gil E, Reyes-Sandoval A, Cottingham MG, Spencer AJ, Collins KA, Dicks MD, Milicic A, Lall A, Furze J, Turner AV, Hill AV, Brun A, Gilbert SC. Immunogenicity and efficacy of a chimpanzee adenovirus-vectored Rift Valley fever vaccine in mice. Virol J. 2013;10:349. doi: 10.1186/1743-422X-10-349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wichgers Schreur PJ, Oreshkova N, Moormann RJ, Kortekaas J. Creation of Rift Valley fever viruses with four-segmented genomes reveals flexibility in bunyavirus genome packaging. J. Virol. 2014;88(18):10883–10893. doi: 10.1128/JVI.00961-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Won S, Ikegami T, Peters CJ, Makino S. NSm and 78-kilodalton proteins of Rift Valley fever virus are nonessential for viral replication in cell culture. J. Virol. 2006;80(16):8274–8278. doi: 10.1128/JVI.00476-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu W, Watts DM, Costanzo MC, Tang X, Venegas LA, Jiao F, Sette A, Sidney J, Sewell AK, Wooldridge L, Makino S, Morrill JC, Peters CJ, Kan-Mitchell J. The nucleocapsid protein of Rift Valley fever virus is a potent human CD8+ T cell antigen and elicits memory responses. PLoS One. 2013;8(3):e59210. doi: 10.1371/journal.pone.0059210. [DOI] [PMC free article] [PubMed] [Google Scholar]