All clinicians believe they provide quality care, yet most clinicians do not directly measure quality parameters in their practice to provide verifiable health care outcomes.1 Quality measures related to a chronic disease provide reportable and repeatable measures that can either document performance of quality care or identify gaps in care for future action/improvement. Disease-specific quality measures in neurology provide a framework that can assist clinicians in practice measurement and modification; these have the potential to benefit both subspecialist and generalist alike. Multiple sclerosis (MS) is a common, chronic, and ultimately disabling disease with multiple potential clinical intervention points during its course. It is therefore appropriate to have quality measures specific for this condition that span the course of the disease.
It is estimated that MS affects about 400,000 Americans.2 MS is a costly disease, and is the leading cause of disability among young adults.3,4 MS can culminate in irreversible functional disability with symptoms including visual or sensory disturbances, loss of strength, tremor, ambulatory problems, loss of bladder/bowel control, fatigue, spasticity, cognitive impairment, depression, and sexual dysfunction. The median time to death is around 30 years from disease onset, which represents a reduction in life expectancy of 5–10 years.5
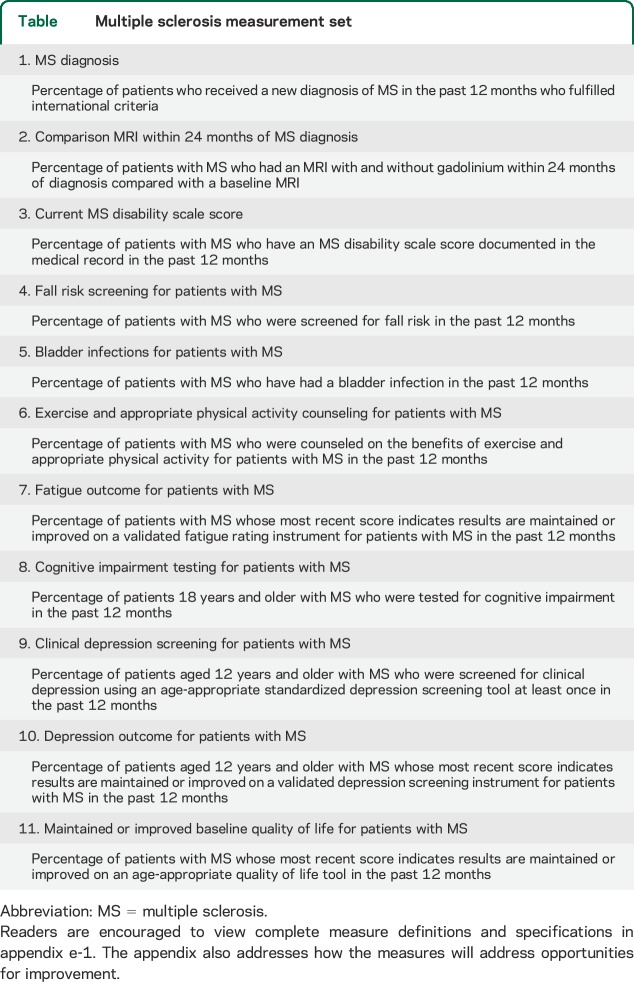
In 2014, the American Academy of Neurology (AAN) formed a multidisciplinary MS quality measurement set work group to identify and construct new quality measures aimed at improving the delivery of care and outcomes for patients with MS. In this executive summary, we report on the quality measurement set developed by the work group (table). The full measurement set, including specifications, is available in appendix e-1 on the Neurology® Web site at Neurology.org. The AAN Multiple Sclerosis Quality Measurement Set includes measures that can be used in quality improvement initiatives, public reporting, payment, and maintenance of certification performance in practice programs.
Table.
Multiple sclerosis measurement set
OPPORTUNITIES FOR IMPROVEMENT
Review of the literature showed gaps in care and areas where quality measures might be used to drive improvement in the care of patients with MS. Several studies suggest that the misdiagnosis of MS is common and can lead to patient harm, such as psychological distress, socioeconomic disadvantage, and exposure to inappropriate treatments.6–9 Consensus statements suggest that MRI, the most sensitive method of detecting MS disease activity, is underutilized in monitoring MS disease activity in clinical practice.10,11 Furthermore, current standards in most practices do not include the use of scored disability ratings, despite the availability of a wide range of validated instruments including patient self-report instruments. The use of such instruments would allow for the more accurate tracking of disease progression and disability.12 Fall screening is also an opportunity for improvement: patients with MS have an increased risk of falls, do not spontaneously report falls to health care providers, and fall history has been shown to be a good predictor of future falls.13–16 Bladder infections are common in patients with MS and proper management can reduce the risk of infection, offering an opportunity for improvement.17 Despite the known benefits of exercise and physical activity, many persons with MS remain inactive, offering an opportunity for improvement.18,19 Fatigue occurs in about 80% of persons with MS and has an impact on physical activity and daily functioning.20 Behavioral strategies and medications can improve fatigue, offering an opportunity for improvement.21 Cognitive impairment is reported by 40%–70% of patients with MS, yet the most widely used screening tool for cognitive function, the Mini-Mental State Examination, is insensitive to the changes most commonly found in patients with MS.22–24 Cognitive rehabilitation has been shown to be beneficial in patients with MS, providing an opportunity for improvement if cognitive complaints are ascertained. Depression is common in patients with MS but is underdiagnosed and undertreated.25 Use of simple screening tools could increase the recognition of depression and thus the use of appropriate treatments. MS has a negative impact on quality of life that can be improved by the proper use of disease-modifying and symptomatic therapies.4 Monitoring quality of life provides a way to assess a patient's overall management.
METHODS
Project leadership for the MS quality measurement set was provided by the AAN, who has designed and coordinated several quality measurement sets, including headache, 2013 epilepsy update, and amyotrophic lateral sclerosis.26–28 Details of the full AAN measurement development process are available online.29
The AAN aimed to convene a cross-specialty and multidisciplinary expert work group, and therefore solicited a broad representation of key stakeholders by inviting nominations for expert panel members from physician and nonphysician associations, MS patient and caregiver advocacy organizations, health plans, and large group employers. The selected work group consisted of 23 members (a list of work group members and contributing organizations follows this article): 6 MS specialists, 3 patient organization representatives, 3 nurse practitioners, 2 rehabilitation specialists, 1 occupational therapist, 1 physical therapist, 1 psychiatrist, 1 neuropsychologist, 1 insurance plan representative, 1 patient representative, and 3 facilitators. All work group members are required to disclose potential conflict of interests and completed an application summarizing experiences and interest.
The co-chairs independently select members from the pool of qualified specialists and experts who respond to the nomination call. The selection was based on the nominee's experience in performance measures, quality improvement, and clinical activities. In addition, requests for nominations were sent to relevant physician organizations and patient advocacy groups. Large health care organizations or insurers were also invited to nominate individuals for the work group.
The work group followed the AAN measure development process, which requires completing an evidence-based literature search, drafting candidate measures and technical specifications, establishing a multidisciplinary work group adhering to the AAN conflict of interest policy, convening in person to review candidate measures, refining and discussing the candidate measures, soliciting public comments on approved measures during a 30-day period, refining the final measures according to input received during the public comment period and corresponding technical specifications, and obtaining approvals from the work group, AAN Quality and Safety Subcommittee, AAN Practice Committee, and AAN Institute Board of Directors.29
The work group sought to develop measures to support the delivery of high-quality care and to improve patient outcomes. A rigorous review of the evidence occurred. The co-chairs and facilitators, guided by a medical librarian, conducted a comprehensive search identifying over 557 abstracts and winnowing results to locate 13 guidelines and 1 consensus paper used as the evidence base for the measures developed.
The work group also strove to balance the burdens of measures on clinicians and patients against the benefit of these measures in guiding quality care. The AAN will update these measures on an ongoing basis every 3 years, and thus the measure set provides a working framework for measurement, rather than a long-term mandate.
RESULTS
The work group met on June 30, 2014, discussing and voting to approve 13 candidate measures for public comment. Following public comment, the measurement set was revised and the work group ultimately approved 11 measures for inclusion in the AAN 2015 Multiple Sclerosis Quality Measurement Set (table).
It is impossible for one quality measurement set to address all quality of care issues in MS. The measures developed reflect consensus decisions about how gaps in care could be improved and where clinical evidence exists to support the measures. The measures primarily are intended for use in quality improvement efforts. The final measures span the natural history of MS from diagnosis to later disability. Two measures explicitly were not recommended for use in accountability programs (Multiple Sclerosis Diagnosis and Comparison MRI Within 24 Months of MS Diagnosis) due to the potential burden of locating information via chart review.
Four measures are intended to be applied at the system or accountable care organization level, and these include measures to address bladder infections, fatigue, depression, and quality of life. Use of these measures to compare individual providers or practices would require the application of a valid risk adjustment methodology, which does not yet exist for MS or any other disease populations. These measures may be used for accountability at the system or accountable care organization level if the MS populations being compared are similar in demographics, socioeconomic status, and the prevalence of comorbid conditions. These measures may also be used for internal, non–publicly reported quality improvement for a patient population that is not subject to significant change, as risk adjustment or stratification would not be required. The work group determined the Cognitive Impairment Testing for Patients with MS should also apply only to the system or health plan level of care for use in accountability programs. The AAN encourages a minimum sample size of 20 for use in public reporting programs to further reduce likelihood of error. The number 20 reflects current CMS sample requirements for Hospital Compare public reporting.
At the beginning of this project, the work group determined the scope would be limited to MS, meaning that neuromyelitis optica and clinically isolated syndrome were excluded. The work group considered several other important constructs in care for people with MS, including MS relapse, spasticity, mobility, visual deficits, and disease-modifying therapy (DMT) use. Development of a relapse measure was deemed to be of high importance given the fact that reduction in the number of relapses is considered to be one of the most important desired outcomes for a patient with MS. However, potential measure drafts were noted to be potentially difficult or impossible to measure, difficult or impossible for a practitioner to act upon, and cost-inefficient. Development of a measure related to DMT was evaluated, but there was lack of published data supporting a treatment gap in care. There were also concerns that a denominator could be accurately identified using administrative data with limitations in ICD coding (i.e., specifically to relapsing-remitting MS vs progressive MS). The work group began to develop measure concepts to address mobility and visual deficits, but these did not receive high enough priority for further development following the in-person meeting.
The work group announced and accepted public comments on the draft measurement set during August and September 2014. During the public comment period, 87 individuals provided over 600 comments on the draft measurement set. As a result of public comments and concern, the proposed measures on “pain assessment” and “fall follow-up plan” candidate measures were withdrawn from the final set the work group approved for public comment. The pain assessment measure was withdrawn due to concern that it unnecessarily duplicated existing measures. In its place, the work group encourages individuals to consider National Quality Forum–endorsed measure 0420 (adopted into the Physician Quality Reporting System measure 131) to address patient pain concerns. The fall follow-up measure was withdrawn due to potential difficulty locating follow-up plan documentation, which would potentially require burdensome chart review, as the information would not be easily accessed in an electronic health record.
The full measurement set specifications are available in appendix e-1.
DISCUSSION
Improving the quality of health care is essential in the practice of medicine. Fundamental to these efforts to improve quality is the ability to measure care because we cannot improve what we do not measure. These measures are intended to be used by stakeholders to quantify the quality of care provided to patients with MS. There are several statewide, national, and private and public payer efforts to hold health care providers formally accountable for the quality of their care. AAN-developed measures may be considered for use in these programs as well as other public reporting programs; these measures are based on existing guidelines and in part are intended to help focus providers on these standards of care.
Just as the work on guidelines is never complete, there will always be ongoing work on a measurement set. As the medical literature is updated, guidelines will be updated, and subsequently, quality measures will be updated as well. In addition to re-reviewing the clinical content of a measure, further validation research will be needed to measure the process–outcome link, which consists of using these measures and determining whether they lead to better health. Finally, if future studies show that there is little to no gap in care, that measure may be retired even if it has strong medical evidence to justify doing it.
The AAN is monitoring the field of quality measurement, and there are major changes under way. Some of these trends include thinking about outcomes of care in addition to process of care, focusing on patient-centered instead of clinician-centered measures, considering overuse measures in addition to underuse measures, including costs of care into the measures, and thinking about measures that can be more easily incorporated within electronic health records. None of these features was highlighted in the first AAN measures published only 5 years ago, demonstrating the speed of change in this arena. These attributes are being incorporated in AAN guidelines, and as such, the AAN Quality Measurement Subcommittee will be incorporating them in future measures.
Supplementary Material
ACKNOWLEDGMENT
The authors thank the Multiple Sclerosis Quality Measurement Set Work Group members for their dedication, time, energy, contributions, and work that supported the development of this article: Christopher Bever, MD, MBA, FAAN (American Academy of Neurology); Alexander Rae-Grant, MD, FRCP(C) (American Academy of Neurology); Barbara Giesser, MD, FAAN (American Academy of Neurology); Douglas Jeffery, MD, PhD (American Academy of Neurology); Mitch Wallin, MD, MPH (American Academy of Neurology); Mary Alissa Willis, MD (American Academy of Neurology); K. Rao Poduri, MD, FAAPMR (American Academy of Physical Medicine and Rehabilitation); Patricia Pagnotta, MSN, ARNP, CNRN, MSCN (American Association of Neuroscience Nurses); Carrie Sammarco, DrNP, FNP-C, MSCN (American Academy of Nurse Practitioners); Virgil Mathiowetz, PhD, OTR/L, FAOTA (American Occupational Therapy Association); Amy Yorke, PT, PhD, NCS (American Physical Therapy Association); Melanie Schwarz, MD (American Psychiatric Association); Victor Mark, MD (American Society of Neurorehabilitation); Ronald Koenig, MD, FAAN (Anthem); John DeLuca, PhD (National Academy of Neuropsychology); June Halper, MSN, APN-C, MSCN, FAAN (Consortium of Multiple Sclerosis Centers); Cindy Richman (Multiple Sclerosis Association of America); Annette Okai, MD (Multiple Sclerosis Foundation); Nicholas LaRocca, PhD (National Multiple Sclerosis Society); William MacNally, MHA, FACHE (National Multiple Sclerosis Society–Midwest Chapter); Eric Cheng, MD, MS, FAAN (American Academy of Neurology Facilitator); Michael Phipps, MD, MHS (American Academy of Neurology Facilitator); Amy E. Sanders, MD, MS (American Academy of Neurology Facilitator); Amy Bennett, JD (American Academy of Neurology staff); Gina Gjorvad (American Academy of Neurology staff); Erin Hagen (American Academy of Neurology staff); Becky Schierman, MPH (American Academy of Neurology staff).
GLOSSARY
- AAN
American Academy of Neurology
- DMT
disease-modifying therapy
- ICD
International Classification of Diseases
- MS
multiple sclerosis
Footnotes
Supplemental data at Neurology.org
AUTHOR CONTRIBUTIONS
Dr. Rae-Grant contributed to study concept and design, acquisition of data, analysis or interpretation of data, drafting/revising the manuscript, critical revision of the manuscript for important intellectual content, and study supervision. A. Bennett contributed to study concept and design, acquisition of data, analysis or interpretation of data, drafting/revising the manuscript, critical revision of the manuscript for important intellectual content, and study supervision. Dr. Sanders contributed to study concept and design, acquisition of data, analysis or interpretation of data, drafting/revising the manuscript, critical revision of the manuscript for important intellectual content, and study supervision. Dr. Phipps contributed to study concept and design, acquisition of data, analysis or interpretation of data, drafting/revising the manuscript, critical revision of the manuscript for important intellectual content, and study supervision. Dr. Cheng contributed to study concept and design, acquisition of data, analysis or interpretation of data, drafting/revising the manuscript, critical revision of the manuscript for important intellectual content, and study supervision. Dr. Bever contributed to study concept and design, acquisition of data, analysis or interpretation of data, drafting/revising the manuscript, critical revision of the manuscript for important intellectual content, and study supervision.
STUDY FUNDING
No targeted funding reported.
DISCLOSURE
A. Rae-Grant reports receiving royalty fees from textbook publication with Demos Publishing and Wolters Kluwer and contracted editing with Dynamic Medical. A. Bennett and A. Sanders report no disclosures relevant to the manuscript. M. Phipps reports being on the clinical advisory board for Castlight Health. E. Cheng reports no disclosures relevant to the manuscript. C. Bever reports receiving center of excellence and research merit awards from the Department of Veterans Affairs, receiving a research grant from the National Multiple Sclerosis Society, and serving on the Quality and Safety Subcommittee and the Registry Workgroup of the American Academy of Neurology and on the program committees of the Consortium of MS Clinics, the Americas Committee for Treatment and Research in MS, and the Paralyzed Veterans of America. He is the coholder of a patent for the use of hematogenous stem cells in cell replacement and gene delivery therapy. Go to Neurology.org for full disclosures.
CONFLICT OF INTEREST
The American Academy of Neurology is committed to producing independent measurement sets. Significant efforts are made to minimize the potential for conflicts of interest to influence the finalized measures. Conflict of interest forms were obtained from all authors and reviewed by an oversight authority prior to project initiation. All potential conflicts of interest are resolved in accordance with the AAN's Policy on Conflicts of Interest and as described in the 2014 AAN Measurement Manual.29 The AAN forbids commercial participation in, or funding of, measure development and initial distribution.
REFERENCES
- 1.Centers for Medicare & Medicaid (CMS). 2012 Reporting Experience. Baltimore, MD: Centers for Medicare & Medicaid; 2014:67. [Google Scholar]
- 2.Kantarci O, Wingerchuk D. Epidemiology and natural history of multiple sclerosis: new insights. Curr Opin Neurol 2006;19:248–254. [DOI] [PubMed] [Google Scholar]
- 3.Adelman G, Rane SG, Villa KF. The cost burden of multiple sclerosis in the United States: a systematic review of the literature. J Med Econ 2013;16:639–647. [DOI] [PubMed] [Google Scholar]
- 4.Zwibel H, Smrtka J. Improving quality of life in MS: an unmet need. Am J Manag Care 2011;17:S139–S145. [PubMed] [Google Scholar]
- 5.Compston A, Coles A. Multiple sclerosis. Lancet 2008;372:1502–1517. [DOI] [PubMed] [Google Scholar]
- 6.Miller DH, Weinshenker BG, Filippi M, et al. Differential diagnosis of suspected multiple sclerosis: a consensus approach. Mult Scler 2008;14:1157–1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Solomon AJ, Weinshenker BG. Misdiagnosis of multiple sclerosis: frequency, causes, effects, and prevention. Curr Neurol Neurosci Rep 2013;13:403. [DOI] [PubMed] [Google Scholar]
- 8.Carmosino MJ, Brousseau KM, Arciniegas DB, et al. Initial evaluations for multiple sclerosis in a university multiple sclerosis center. Arch Neurol 2005;62:585–590. [DOI] [PubMed] [Google Scholar]
- 9.Bagnato F, Tancredi A, Richert N, et al. Contrast-enhanced magnetic resonance activity in relapsing-remitting multiple sclerosis. Mult Scler 2000;6:43–49. [DOI] [PubMed] [Google Scholar]
- 10.Consortium of Multiple Sclerosis Centers. Consortium of MS Centers MRI Protocol for the Diagnosis and Follow-up of MS: 2009. Revised Guidelines. Hackensack, NJ: Consortium of Multiple Sclerosis Centers; 2009. [Google Scholar]
- 11.Simon JH, Li D, Traboulsee A, et al. Standardized MR imaging protocol for multiple sclerosis: Consortium of MS Centers consensus guidelines. AJNR Am J Neuroradiol 2006;27:455–461. [PMC free article] [PubMed] [Google Scholar]
- 12.National Institute for Health and Care Excellence. Multiple Sclerosis: Management of Multiple Sclerosis in Primary and Secondary Care: NICE Clinical Guideline 186. London: National Institute for Health and Care Excellence; 2014. [PubMed] [Google Scholar]
- 13.Giannì C, Prosperini L, Jonsdottir J, Cattaneo D. A systematic review of factors associated with accidental falls in people with multiple sclerosis: a meta-analytic approach. Clin Rehabil 2014;28:704–716. [DOI] [PubMed] [Google Scholar]
- 14.Nilsagård Y, Gunn H, Freeman J, et al. Falls in people with MS: an individual data meta-analysis from studies from Australia, Sweden, United Kingdom and the United States. Mult Scler 2015;21:92–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Matusda PN, Shumway-Cook A, Bamer AM, et al. Falls in multiple sclerosis PM R 2011;3:624–632. [DOI] [PubMed] [Google Scholar]
- 16.Cameron MH, Thielman E, Mazumder R, et al. Predicting falls in people with multiple sclerosis: fall history is as accurate as more complex measures. Mult Scler Int 2013;2013:496325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Manach A, Motsko SP, Haag-Molkenteller C, et al. Epidemiology and healthcare utilization of neurogenic bladder patients in US claims database. Neurourol Urodyn 2011;30:395–401. [DOI] [PubMed] [Google Scholar]
- 18.Mayo NE, Bayley M, Duquette P, et al. The role of exercise in modifying outcomes for people with multiple sclerosis: a randomized trial. BMC Neurol 2013;13:69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Motl RW, McAuley E, Snook EM. Physical activity and multiple sclerosis: a meta-analysis. Mult Scler 2005;11:459–463. [DOI] [PubMed] [Google Scholar]
- 20.Meads DM, Doward LC, McKenna SP, et al. The development and validation of the Unidimensional Fatigue Impact Scale (U-FIS). Mult Sclerosis 2009;15:1228–1238. [DOI] [PubMed] [Google Scholar]
- 21.Blikman LJ, Huisstede BM, Kooijmans H, et al. Effectiveness of energy conservation treatment in reducing fatigue in multiple sclerosis: a systematic review and metaanalysis. Arch Phys Med Rehab 2013;94:1360–1376. [DOI] [PubMed] [Google Scholar]
- 22.Connick P, Kolappan M, Bak TH, et al. Verbal fluency as a rapid screening test for cognitive impairment in progressive multiple sclerosis. J Neurol Neurosurg Psychiatry 2012;83:346–347. [DOI] [PubMed] [Google Scholar]
- 23.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975;12:189–198. [DOI] [PubMed] [Google Scholar]
- 24.Beatty WW, Goodkin ED. Screening for cognitive impairment in multiple sclerosis: an evaluation of the Mini-Mental State Examination. Arch Neurol 1990;47:297–301. [DOI] [PubMed] [Google Scholar]
- 25.Fargoso YD, Adoni T, Anacleto A, et al. Recommendations on diagnosis and treatment of depression in patients with multiple sclerosis. Pract Neurol 2014;14:206–209. [DOI] [PubMed] [Google Scholar]
- 26.Ross S, Wall E, Schierman B, et al. Quality improvement in neurology: primary headache quality measures. Neurology 2015;84:200–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fountain N, Van Ness P, Bennett A, et al. Quality improvement in neurology: epilepsy update quality measurement set. Neurology 2015;84:1483–1487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Miller RG, Brooks BR, Swain-Eng RJ, et al. Quality improvement in neurology: amyotrophic lateral sclerosis quality measures: report of the Quality Measurement and Reporting Subcommittee of the American Academy of Neurology. Neurology 2013;81:2136–2140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Quality and Safety Subcommittee. American Academy of Neurology Quality Measurement Manual 2014 Update. Available at: https://www.aan.com/uploadedFiles/Website_Library_Assets/Documents/3.Practice_Management/2.Quality_Improvement/1.Quality_Measures/2.About_Quality_Measures/2015%2002%2011%20Process%20Manual%20Final.pdf. Accessed August 20, 2015. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.