Abstract
Background
Patient reported outcomes (PRO) have been increasingly emphasized; however determining clinically valuable PRO has been problematic and investigation limited. This study examines the association of a previously described PRO – readiness for discharge – with patient satisfaction and readmission.
Study Design
Data from adult patients admitted to our institution from 2009 to 2012 who completed both the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) and the Press Ganey (PG) surveys post-discharge were extracted from an existing database of patients (comprised of 220 patients admitted for small bowel obstruction (SBO) and 98 patients with hospital stays ≥21 days). Using the survey question, “Did you feel ready for discharge?” (RFD), 2 groups were constructed, those RFD and those with lesser degrees of readiness (LRFD – less ready for discharge) using topbox methodology. Outcomes, readmission rates, and satisfaction were compared between those RFD and those LRFD.
Results
Three hundred and eighteen patients met the inclusion criteria; 45% were female and 94% were Caucasian. Median age was 62.3 years (interquartile range [IQR] 52.5-70.8 years). Median length of stay was 10 days (IQR 6.0-24.0 days) and 69.2% were admitted with SBO. The 30-day readmission rate was 14.3%; and 55% indicated they were RFD. Those RFD and LRFD had similar demographics, comorbidity scores, and rates of surgery. Those RFD had higher overall hospital satisfaction (87.3% RFD vs. 62.4% LRFD, p<0.001), higher physician communication scores (median 3.0 RFD vs 2.0 LRFD, p<0.001), and higher nursing communication scores (median 3.0 RFD vs. 2.0 LRFD, p<0.001). Readmission rates were similar between the groups (11.4% RFD vs 18.2% LRFD; p=0.09).
Conclusions
Readiness for discharge appears to be a clinically useful patient-reported metric, as those RFD have higher satisfaction with the hospital and physicians. Prospective investigation into variables affecting patient satisfaction in those LRFD is needed.
Introduction
During the last decade, many aspects of clinical care and medical research have been impacted by the focus on patient-centered care. This concept was given prominence in 2001 with the publication of Crossing the Quality Chasm by the Institute of Medicine.1 Therein, they defined 1 of the 6 priority areas for collective action as the provision of patient-centered care, which is customized according to the patient's needs and values. As a consequence, there was rapid expansion in the field of patient-reported outcomes (PRO).2 Patient-reported outcomes are defined as the report of the status of a patient's health that comes directly from the patient.3 Because the impact of medical care can best be assessed by those who actually experience it, the appropriate use of PRO is central to the transformation of healthcare into a more patient-centered enterprise.4
Concurrent with the emphasis on the delivery of patient-centered health care, regulations requiring the use of a variety of healthcare quality metrics have been rapidly increasing and impacting healthcare delivery.5-7 The Affordable Care Act's establishment of the Hospital Readmissions Reduction Program is one such regulatory program, which is having profound effects on the clinical care delivered in hospital settings. Another critical regulation having significant impact is the institution of Hospital Value-Based Purchasing, which links Medicare and Medicaid reimbursement to patient satisfaction, as measured by the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey.8,9
One relatively understudied area at present is the relationship between patient-reported outcomes and quality metrics. The aim of this study was therefore to determine the relationship between a previously studied patient-reported outcome (readiness for discharge) and 2 quality metrics (readmission rates and patient satisfaction).
Methods
Patient Sample
An existing database of patients with complete patient satisfaction data was used for this study. This database was constructed from hospital records and included only patients who returned satisfaction surveys over the defined interval. This dataset of 318 patients was comprised of 2 distinct subgroups and had been collected for earlier studies. It included patients admitted for small bowel obstruction (SBO) (n=220 or 69.2% of the total sample) and patients with hospital stays longer than 21 days (n=98 or 30.8% of the total sample). All patients with a diagnosis of SBO were included. The most recent 100 patients (98 of whom were included in this sample) with hospital stays ≥21 days (from a larger group of 278 patients) who had detailed clinical data extracted for a earlier study were included. This resulted in a patient population that was diverse and included both medical and surgical patients. In addition, there was variety in the acuity of the hospital course, including both routine and complex admissions, as well as emergent and elective admissions. All patients had completed both the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) and the institutional Press Ganey (PG) surveys between 2009 and 2012. For the overall group (n= 318) patient accrual by year was as follows: 5% (n=15) in 2009, 8% (n=27) in 2010, 46% (n=147) in 2011, and 41% (n=129) in 2012. For each subgroup patient accrual by year followed a similar pattern. For the SBO group, accrual by year was 5% (n= 12) in 2009, 9% (n= 19) in 2010, 43% (n=95) in 2011, and 43% (n= 94) in 2012. For patients with hospital stays longer than 21 days group, the accrual was 3% (n=3) in 2009, 8% (n=8) in 2010, 53% (n=52) in 2011, and 36% (n=35) in 2012. Those who completed only one of these surveys were not included in our sample. Standard HCAHPS exclusions applied (e.g. those who were aged younger than 18 years, psychiatric or rehabilitation admissions, discharge to nursing facilities, admitted as observation status, those already surveyed within previous 90 days). At our facility, > 85% of patients are eligible to be surveyed and all of those eligible are sent surveys through a third party vendor. All patients from the database were included, with the exception of 2 patients who had missing data for the central variable – readiness for discharge. Patients had previously undergone detailed retrospective chart reviews. Variables collected included demographic (e.g. age, gender), clinical (e.g. comorbidities, admitting diagnosis), and structural data related to inpatient hospital admission (e.g. admitting service, route of admission). Primary diagnosis was determined by clinical chart review, including review of admitting notes, daily notes, discharge summaries, imaging studies, and relevant laboratory studies. Billing records were not used for this study. The distance that patients traveled from home to the hospital facility was calculated using the patient's home address and standard mapping programs. Comorbidities were defined by the standard definitions within the Charlson comorbidity index scoring system.10
Surveys
Surveys were distributed as part of the processes for standard care by the institution's chosen vendor (Press Ganey). Surveys were mailed between 48 hours and 6 weeks after discharge, the standard HCAHPS recommended time frame. Mean± SD time in our sample between discharge and a resulted survey was 37± 12.1 days Because the date that surveys are sent was not available and the resulted date included all aspects of records submission to the vendor (which is only done on a weekly basis and includes processing time), this is only an estimate of the true time period for survey completion by patients. Institutional Review Board (IRB) approval was obtained prior to study inception.
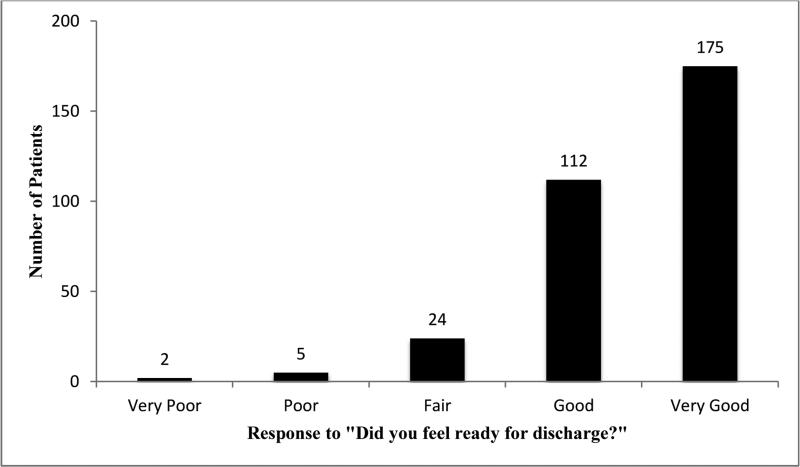
A question from the institutional Press Ganey survey was used to determine readiness for discharge: “Did you feel ready for discharge?” This question had 5 possible responses: very poor, poor, fair, good, and very good (Figure 1). Those who responded with the highest response (very good) were deemed “ready for discharge” (RFD). Patients with all other responses were combined and deemed “less ready for discharge” (LRFD). This categorization was chosen for a number of reasons. First, the psychometric properties of the survey as designed by Press Ganey allowed for either a mean score or a topbox methodology to analyze results on the institutional level.11 The topbox methodology to categorize patients dichotomously was chosen for a number of reasons. Foremost was the principle that survey respondents who respond with the highest response have been shown to be distinct from those who choose all other responses in a variety of settings (e.g. automobile and airline industries, business settings, entertainment parks).12,13 Second, the CAHPS consortium has created a standard practice of using the topbox response as the response to which all other responses are compared.9 Third, to further validate the topbox methodological approach, we also examined RFD as a continuous variable (as opposed to the dichotomous topbox methodology just described.) When correlation analysis was used to compare RFD as a continuous variable to physician communication and hospital satisfaction, similar results were obtained (see Results section). For these reasons, the results are reported here using the most recognizable and standard format of topbox response.5,7,14
Figure 1.
Distribution of responses to “Did you feel ready for discharge?” plot of the data from all patients studied; many of the points overlap.....”. Edit 2nd and 3rd sentences: Correct the grammar: it currently is inconsistent and missing words: Suggestion: “The values on the y-axis represent.... patient responses to...... The values on the x-axis represent ......”.
The HCAHPS survey was used to abstract the satisfaction data relevant to the study question. Specifically, satisfaction with physician communication was determined using the following HCAHPS questions: “During this hospital stay, how often did doctors treat you with courtesy and respect?”, “During this hospital stay, how often did doctors listen carefully to you?”, “During this hospital stay, how often did doctors explain things in a way you could understand?” All of these questions had the following possible responses: never, sometimes, usually, and always. These were analyzed by assigning each response a score from 1-4 (1 = never, 4 = always). A physician communication composite was then constructed from the responses to the 3 questions, with the composite score being the number of topbox responses for the 3 questions with the maximum score being 3 (or topbox response to all of the questions). This dichotomized variable (topbox or not topbox) was the primary communication composite domain. Additionally, to demonstrate the consistency of this approach, the physician communication composite was also examined as a continuous variable and calculated by determining the mean response (1-4), with the highest possible score being 4 (a response of 4 to all 3 questions). Hospital satisfaction was determined using the summary HCAHPS question: “Using any number from 0 to 10, where 0 is the worst hospital possible and 10 is the best hospital possible, what number would you use to rate this hospital during your stay?” Responses 9 and 10 were considered “topbox”, according to HCAHPS standard prescription.15
In addition, we evaluated differences in the discharge process between the groups using the questions: “During this hospital stay, did doctors, nurses or other hospital staff talk with you about whether you would have the help you needed when you left the hospital?” and “During this hospital stay, did you get information in writing about what symptoms or health problems to look out for after you left the hospital?” Finally, we calculated a nursing communication composite using the method described here. The included questions were: “During this hospital stay, how often did nurses treat you with courtesy and respect?”, “During this hospital stay, how often did nurses listen carefully to you?”, and “During this hospital stay, how often did nurses explain things in a way you could understand?”
Setting
All patients received care at a single tertiary care academic medical center. The discharge process involved a standardized workflow created and implemented by patient providers, a case manager, pharmacy, nursing, and therapy services. A written individualized summary was presented to patients at discharge, which included education for self-care, medications, future appointments, necessary therapies and equipment. In addition, a pharmacist performed medication teaching, including reasons for each new medication or changes to previous medications. Any drain or wound care education was performed primarily by nursing staff. This process was performed according to standard hospital policies and was without significant change over the study period.
Post Discharge Utilization
The 30-day readmission rate was determined from retrospective chart review and was defined as readmission to any hospital within 30 days of discharge. Inpatient and outpatient notes were reviewed in detail, and admission to outside hospitals was abstracted if noted in the medical record. Patients were not directly contacted, due to limitations imposed by human studies approval. HCAHPS satisfaction scores for overall hospital rating and the physician communication domain were the primary outcomes, and these were examined as a function of readiness for discharge. Secondary outcomes were communication with nurses, number of post-discharge clinic visits, number of emergency department (ED) visits, and number of readmissions. Hospital contacts were calculated by using the total of the number of ED visits, readmissions, and clinic visits. Urgent contacts were defined as unplanned readmissions and ED visits. Clinic visits to any provider for any reason were tabulated, as it was difficult to accurately discern planned follow-up visits from urgent visits to evaluate new symptoms.
Statistical Analysis
Statistical analysis was performed using the chi-square test, Student's T-test, and Mann-Whitney U test as applicable using SPSS statistical software version 21.0, released 2012, IBM Corp). Additionally, correlations between the various measures were calculated using Spearman's rank correlation (rs) analyses.
Results
The analysis sample consisted of a total of 318 patients. Of these, 45% were female and 94% were Caucasian. Median age was 62.3 years (interquartile range 52.5 to 70.8), and median body mass index (BMI) was 26.9 kg/m2 (interquartile range 23.2 to 31.0 kg/m2). median length of stay (LOS) was 10.0 days (interquartile range 6.0 to 24.0 days), and 62.6% of patients had an operative procedure during their admission. Primary admission diagnoses included gastrointestinal diagnoses (48.4%), hematologic diagnoses (10.0%), injury-related admissions (6.3%), and other assorted diagnoses (11.9%) (consisting largely of urologic or gynecologic malignancies). The remaining 23.4% of patients were admitted for various other primary conditions (including pulmonary, cardiac, and neurologic conditions.) The overall 30-day readmission rate was 14.5%.
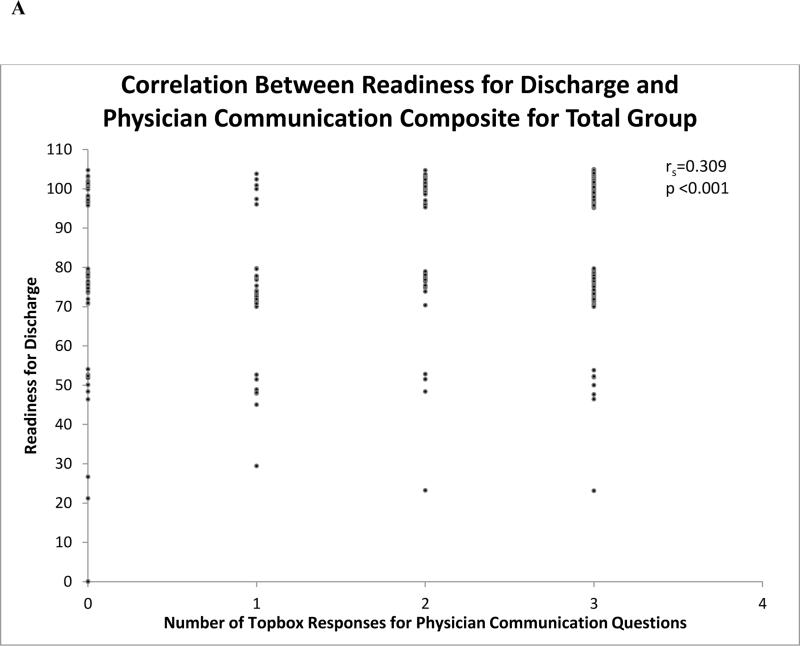
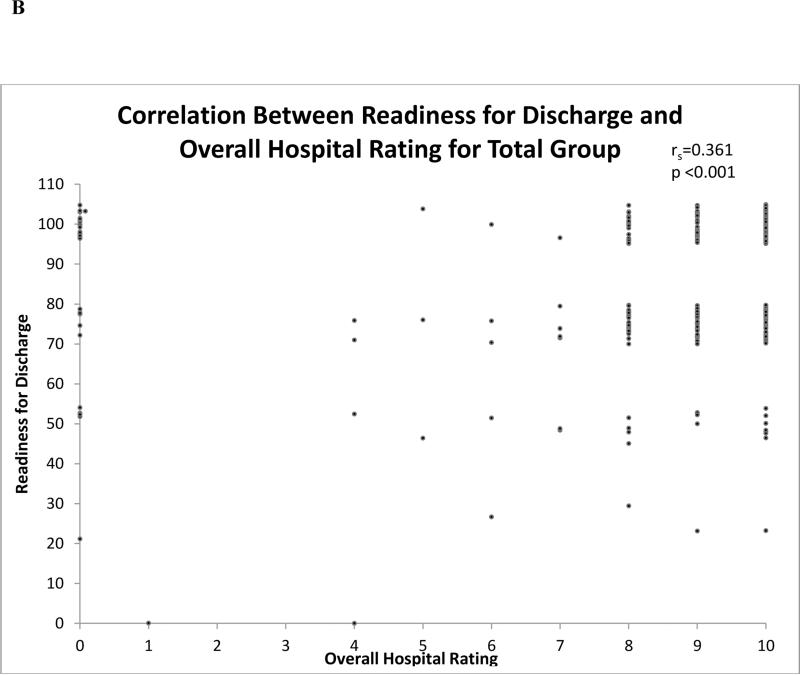
To examine the relationship between the predictor variable, readiness for discharge, and the primary outcomes, a correlation analysis was first performed. A significant correlation between readiness for discharge (as a continuous variable) and the physician communication composite domain was found (rs= 0.309; p < 0.001; Figure 2A). This was true with either method of calculating the physician communication composite. In addition, the 2 methods for calculating the physician communication composite had a very strong correlation with one another (rs = 0.997; p < 0.001). When comparing readiness for discharge as a continuous variable to the overall hospital rating, there was a significant correlation as well (rs = 0.361; p < 0.001; Figure 2B). These strong correlations between readiness for discharge and satisfaction held true in both subgroups – those admitted for SBO and those with prolonged hospital stays. (We also conducted a sensitivity analysis by comparing those who responded to the readiness for discharge question with the topbox response (i.e. “very good”)) to those who responded with the next best response (i.e. “good”). We found no change in our results with a continued significant difference between groups for all outcome variables (physician communication, nursing communication, hospital satisfaction, and information giving about care after discharge) (Supplemental Table 1, available online). Given these results, patients were classified as RFD using the dichotomized topbox method.
Figure 2.
Correlation between readiness for discharge and satisfaction measures for total group. (A) Plot of the total patient population; since many of the points overlapped secondary to the same responses to both questions, a very small random number was added or subtracted to the response to improve the visual depiction of the data. The values y-axis represents the actual patient response to the readiness for discharge question. The value on the x-axis represents the number of topbox responses to the physician communication composite questions. (B) Plot of the total patient population; since many of the points overlapped secondary to the same responses to both questions, a very small random number was added or subtracted to the response to improve the visual depiction of the data. The values y-axis represents the actual patient response to the readiness for discharge question. The value on the x-axis represents the response to the overall hospital rating question.
To further examine the relationship between readiness for discharge and satisfaction, patients were grouped into RFD and those with lesser degrees of readiness for discharge (LRFD). More than half (n=175 [55%]) of patients indicated they were RFD (Figure 1). Those RFD were then compared with those LRFD with respect to basic demographic and clinical variables (Table 1). There were no significant differences in terms of age, gender, race, BMI or comorbidities. A similar fraction had operative procedures during the admission (61.7% RFD vs 63.6% LRFD). The distance traveled to the hospital from home was similar between groups (Table 1). Those patients LRFD had longer hospital stays (median 14.0 days LRFD vs 8.0 days RFD, p=0.003) than those patients RFD.
Table 1.
Characteristics of Patients by Readiness for Discharge
| Characteristic | Ready for discharge (n=175) | Less ready for discharge (n=143) | p Value |
|---|---|---|---|
| Age, y median, (IQR) | 64.2 (54.4-71.0) | 60.6 (51.0-70.4) | 0.26 |
| Female, n (%) | 83 (47.4) | 60 (42.0) | 0.37 |
| Caucasian, n (%) | 165 (94.2) | 133 (93.0) | 0.64 |
| Distance from hospital, median miles (IQR) | 56.3 (11.6-82.3) | 54.3 (23.0-104.0) | 0.33 |
| BMI, kg/m2, median (IQR) | 27.4 (23.4-31.4) | 26.6 (23.0-30.4) | 0.15 |
| Charlson Comorbidity Index, median (IQR) | 2.0 (0.0-2.0) | 1.0 (0.0-3.0) | 0.71 |
| Length of stay, d, median (IQR) | 8.0 (5.0-20.0) | 14.0 (6.0-29.0) | 0.003 |
| Surgery during admission, n (%) | 108 (61.7) | 91 (63.6) | 0.73 |
| Diagnosis, n (%) | 0.10 | ||
| Gastrointestinal | 91 (52.0) | 63 (44.1) | |
| Urologic/gynecologic malignancies | 22 (12.6) | 16 (11.2) | |
| Hematologic | 22 (12.6) | 10 (7.0) | |
| Injury related | 9 (5.1) | 11 (7.6) | |
| Infectious | 4 (2.3) | 12 (8.4) | |
| Neurologic | 4 (2.3) | 7 (4.9) | |
| Other | 23 (13.1) | 24 (16.7) |
IQR, interquartile range
When patients RFD were compared to those LRFD, significant differences in satisfaction were seen (Table 2). Most importantly, patients RFD had significantly higher satisfaction scores for the physician communication composite (median 3.0 RFD vs 2.0 LRFD, p<0.001) and the nursing communication composite (median 3.0 RFD vs. 2.0 LRFD, p<0.001). Calculating the physician composite using the alternate method of average response for the questions also demonstrated a similar result (p<0.001; data not shown). Those who reported feeling RFD also had significantly higher overall satisfaction with the hospital (87.3% RFD vs. 62.4% LRFD, p<0.001). Finally, both HCAHPS questions related to discharge preparation (i.e. post-discharge hospital needs and written instructions) were similarly strongly related to readiness for discharge (Table 2).
Table 2.
Comparison of Quality Metrics as a Function of Readiness for Discharge
| Variable | Ready for discharge (n=175) | Less ready for discharge (n=143) | p Value |
|---|---|---|---|
| Composite score for physician communication n, median (IQR) of topbox responses* | 3.0 (2.0-3.0) | 2.0 (1.0-3.0) | <0.001 |
| Composite score for nursing communication (median no., IQR of topbox responses)* | 3.0 (2.0-3.0) | 2.0 (1.0-3.0) | <0.001 |
| Overall satisfaction with hospital, n (%) topbox of question respondents | 138/159 (87.3) | 83/133 (62.4) | <0.001 |
| During this hospital stay, did doctors, nurses or other hospital staff talk with you about whether you would have the help you needed when you left the hospital? n (%) topbox of composite questions respondents | 135/142 (95.1) | 87/104 (83.7) | 0.003 |
| During this hospital stay, did you get information in writing about what symptoms or health problems to look out for after you left the hospital? n (%) topbox of composite questions respondents | 134/139 (96.4) | 88/104 (84.6) | 0.001 |
IQR, interquartile range.
Composite communication score represents the mean number of topbox responses for the questions. The maximum score is 3 (topbox response to all three questions).
When these same outcome measures as a function of readiness for discharge were examined in the subgroup of patients admitted with SBO, significant differences persisted for all outcome variables (Supplemental Table 2, available online). When examined in the subgroup of those with prolonged hospital stays, similar patterns were seen (Supplemental Table 3, available online), but not all reached statistical significance, likely due to the smaller sample size in this subgroup.
The 3 separate questions regarding physician communication that comprise the composite score were also examined individually for the entire cohort. Each showed a similar and significant relationship to readiness for discharge (Table 3).
Table 3.
Comparison of Responses for Individual Physician Communication Questions by Readiness for Discharge
| Variable | Ready for discharge (n=175) n/n % |
Less ready for discharge (n=143) n/n % |
p Value |
|---|---|---|---|
| Treat you with courtesy and respect? | 152/163 (93.3) | 95/134 (70.9) | <0.001 |
| Listen carefully to you? | 140/163 (85.9) | 74/132 (56.1) | <0.001 |
| Explain things in a way you could understand? | 130/163 (79.8) | 70/132 (53.0) | <0.001 |
Answers to all 3 questions are used to create the physician communication composite.
With respect to readmission, patients who felt less ready for discharge had a nonsignificant trend toward higher rates of readmission when compared to those who were RFD (18.2% LRFD vs 11.4% RFD; p=0.09; Table 4). Similarly, there was a nonsignificant result towards an increased number of urgent post-discharge visits in patients who felt less ready for discharge (22.3% LRFD vs 15.4% RFD, p=0.11; Table 4). There were no differences between groups in the percentage of patients undergoing ED evaluations, total number of clinic visits, or total number of encounters (Table 4). When those patients admitted for prolonged hospital stays and for SBO were examined as subgroups, similar patterns can be seen in post-discharge use (Supplemental Tables 4 and 5, available online). Not surprisingly, those admitted for prolonged stays, had higher rates of readmission and number of urgent visits when compared to those in the SBO group.
Table 4.
Post-Discharge Utilization Comparison
| Variable | Ready for discharge (n=175) | Less ready for discharge (n=143) | p Value |
|---|---|---|---|
| Readmission, n (%) | 20 (11.4) | 26 (18.2) | 0.09 |
| Emergency department visit, n (%) | 8 (4.6) | 12 (8.4) | 0.16 |
| Clinic visits, median (IQR) | 1.0 (1.0-3.0) | 1.0 (0.0-2.0) | 0.55 |
| Urgent visits, n (%) | 27 (15.4) | 32 (22.3) | 0.11 |
| Total encounters, median (IQR)* | 2.0 (1.0-3.0) | 2.0 (1.0-3.0) | 0.91 |
IQR, interquartile range.
Total encounters = number of readmisisons + number of emergency department visits + number of clinic visits.
Because this sample was diverse and included distinct subgroups, several secondary analyses of the primary outcomes were also performed (Table 5). When only patients admitted for bowel obstruction were considered, those RFD had significantly higher scores for physician communication (median 3.0 RFD vs. 2.0 LRFD; p<0.001) and hospital satisfaction (84.2% RFD vs. 61.5% LRFD; p<0.001). Similar findings were seen among the smaller subgroup of those admitted with prolonged LOS. When patients were examined as a function of admitting service (medical vs. surgical service), RFD again was significantly associated with higher physician communication scores and better overall satisfaction with the hospital in both subgroups.
Table 5.
Analysis of Satisfaction and Length of Stay by Diagnostic Group and by Admitting Service
| Variable | Ready for discharge | Less ready for discharge | p Value |
|---|---|---|---|
| Admitted for bowel obstruction | |||
| n | 133 | 87 | |
| Composite score for physician communication, n, median, (IQR) | 3.0 (2.0-3.0) | 2.0 (1.0-3.0) | <0.001 |
| Overall satisfaction with hospital n (%) topbox of question respondents | 101/120 (84.2) | 48/78 (61.5) | <0.001 |
| Length of stay, d (median, IQR) | 7.0 (4.0-11.0) | 7.0 (4.5-10.5) | 0.78 |
| Prolonged length of stay | |||
| n | 42 | 56 | |
| Composite score for physician communication, n, median, (IQR) | 3.0 (2.0-3.0) | 2.0 (1.0-3.0) | 0.12 |
| Overall satisfaction with hospital n (%) topbox of question respondents | 37/39 (94.9) | 35/55 (63.6) | 0.001 |
| Length of stay, d, median (IQR) | 26.0 (23.0-33.3) | 33.0 (26.3-44.5) | 0.003 |
| Admitted to surgical service | |||
| n | 129 | 94 | |
| Composite score for physician communication, n, median, (IQR) | 3.0 (3.0-3.0) | 2.0 (1.0-3.0) | <0.001 |
| Overall satisfaction with hospital n (%) topbox | 102/116 (87.9) | 60/90 (66.7) | <0.001 |
| Length of stay, d, median (IQR) | 8.0 (5.0-13.5) | 11.0 (6.0-28.3) | 0.001 |
| Admitted to medical service | |||
| n | 46 | 49 | |
| Composite score for physician communication, n, median, IQR) | 3.0 (2.0-3.0) | 2.0 (0.8-3.0) | 0.01 |
| Overall satisfaction with hospital n (%) topbox | 36/43 (83.7) | 23/43 (53.5) | 0.003 |
| Length of stay, d, median (IQR) | 22.0 (6.0-28.0) | 22.0 (5.0-30.5) | 0.85 |
IQR, interquartile range.
[C.E. Please query author about last row, 25.0 (24.0) because it seems to be inconsistent with other median (IQR) entries.]
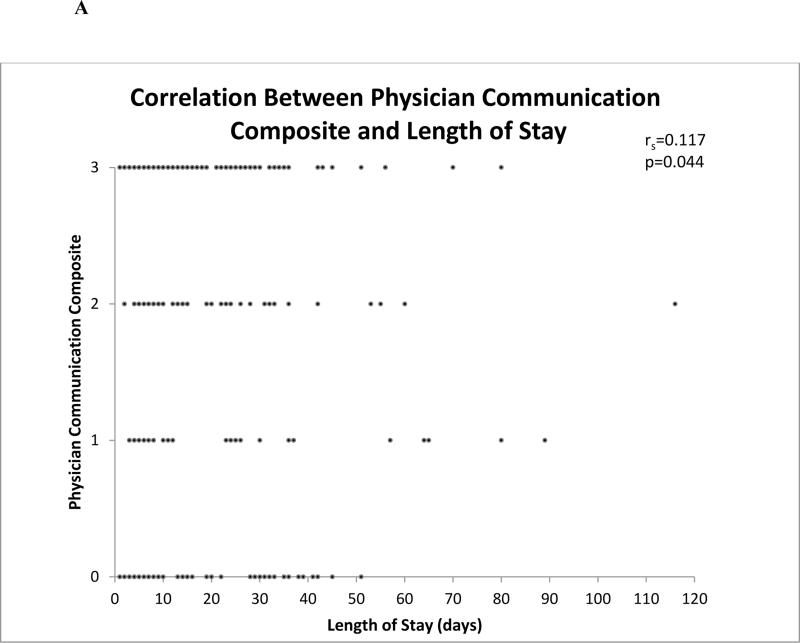
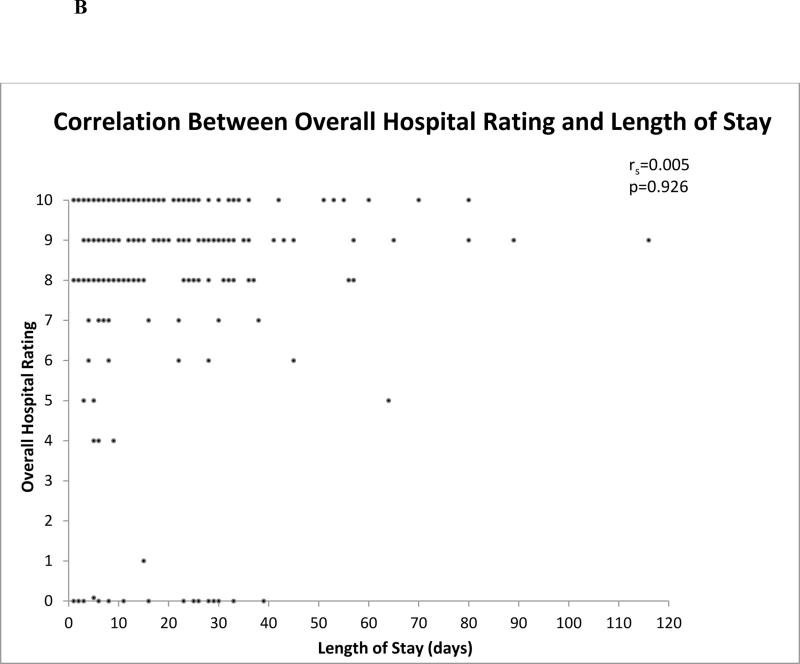
Finally, correlation analyses between length of hospital stay and satisfaction were performed in the overall sample (Figure 3A and 3B). There was no evidence of correlation between LOS and overall score for satisfaction with the hospital, but there was a very weak (rs=−0.117) negative correlation between LOS and physician communication. Similar patterns persisted for both the patient subgroups examined. For those with SBO as an admitting diagnosis, LOS was not significantly correlated with either the overall hospital rating (rs =0.131, p=0.07) or physician communication scores (rs=0.025, p=.72). For those with prolonged hospital stays, LOS has a weak negative correlation with physician communication scores (rs =−0.252, p=0.014) and no correlation with overall hospital score (rs =−0.152, p=0.145).
Figure 3.
(A) Correlations of patient length of stay and physician communication scores. Plot of the total patient population; many of the points overlap secondary to the same responses to both questions. The value on the y-axis represents the number of topbox responses to the physician communication composite questions. The values x-axis represents length of stay in days. (B) Correlations of patient length of stay and overall hospital satisfaction scores. Plot of the total patient population; some of the points overlap secondary to the same responses to both questions. The value on the y-axis represents the response to the overall hospital rating question. The values x-axis represents length of stay in days.
To further evaluate the potential confounding effect of LOS in this study, the subgroup of patients admitted for SBO was examined. Among these 220 patients, there was no difference in median LOS between those RFD and LRFD (7.0 RFD vs. 7.0 LRFD; p=0.78), but the differences in scores for physician communication persisted and remained highly significant (Table 5). Similarly, when only patients admitted to the medical service were considered, there was no difference in median LOS between those RFD and LRFD and satisfaction scores remained significantly different between groups.
Discussion
The major finding in this study is the association of PRO with an important quality metric. Specifically, we demonstrate a strong and significant association between patient-reported readiness for discharge and patient satisfaction. This association holds for satisfaction across multiple domains, namely physician communication, nursing communication, and overall hospital experience. This is a novel finding that, to our knowledge, has not been previously investigated, but is consistent with a previous report demonstrating an association between global patient satisfaction and patient satisfaction with discharge planning as measured by HCAHPS surveys.16
Underlying Mechanism of Associations
Although intriguing, the directionality and mechanism of the relationship between patient-reported readiness for discharge and patient satisfaction have not been elucidated by this study. The most basic explanation is that a patient's satisfaction might be directly and negatively impacted by being discharged from the hospital before the patient felt ready. Although patients might meet specific discharge criteria and no longer require inpatient care, they still might believe they are prepared to continue their convalescence outside the hospital. This type of situation is one for which PRO might be ideal, as its use would add a new dimension to the typical clinical data used to direct discharge teaching and processes. An alternative mechanism is that these variables might be related by way of a third variable, such as discharge teaching. In this scenario, effective discharge teaching might lead to a patient's feeling ready for discharge and to higher levels of satisfaction. This latter postulate is supported by earlier findings suggesting that patient satisfaction scores capture effective patient and provider communications.2,16 However, even if the relationship between readiness for discharge and satisfaction is not causal or direct, that does not imply that it is not useful. In fact, because a third variable, such as effective discharge teaching, would be best assessed by patients, use of a PRO would still be required and might be best represented by a more readily reported surrogate, such as readiness for discharge.
The relationship between readiness for discharge and readmission has been previously studied with mixed findings.17-19 Weiss and colleagues19 examined both patient-reported and nurse-perceived readiness for discharge using a novel Readiness for Hospital Discharge Scale. Using this tool, they demonstrated that a standardized nursing assessment of a patient's readiness for discharge is highly predictive of readmission risk, but their findings have been conflicting.17,19 In one study patient report of readiness for discharge was predictive of readmission risk (2007)19, and in a later study (2010), it was not.17 Our findings demonstrated at most a relatively weak association of patient-reported readiness for discharge with readmission and post-discharge use. Taken together, these data suggest that a weak association between the two might exist, raising the possibility of a mediating variable. Examining our data, it is possible that readiness for discharge is only related to readmission in so much as it is predictive of patient satisfaction. Patients who felt most ready for discharge might be highly satisfied as a result, making them less likely to return to the hospital within 30 days. Patient satisfaction and readmission have previously been shown to be negatively and significantly correlated.16 Conversely, the causal relationship might be either in the opposite direction or bidirectional. Stated differently, could low levels of patient-reported readiness for discharge actually be leading to readmission? Patients who felt ill prepared for discharge might be returning to the hospital for readmission as a result of believing that they were not ready to leave initially. The intricate relationships here are avenues ripe for future research.
Limitations
Although this study examines a large cohort of patients from a variety of clinical care settings, there are a number of limitations to consider. First, this is a single center study performed in a demographically homogeneous group of patients. To better understand the relationship between readiness for discharge and satisfaction, examination of these variables at other centers would be helpful. Because the HCAHPS survey does not have a question related to readiness for discharge, this question is not readily examinable on a national level, and will require institutions with data related to discharge readiness to examine their own data. A second limitation is that some of the survey data used here might have been completed by the patient in retrospect. Because the standard HCAHPS survey process is to send surveys anytime from 48 hours up to 6 weeks after discharge11, a patient might not complete the survey until after a readmission has occurred. This type of situation raises the concern for recall bias. Patients with intervening significant clinical events who complete their surveys in a more delayed fashion might base their responses on more than the initial hospital stay. This is an inherent limitation of any study using HCAHPS data. However, previous data have shown that a more delayed survey return has only minimal effect on the overall outcomes examined.20 This suggests that the effect of recall bias in a study such as ours is likely to be small, but this remains a limitation of our study. Completion of a PRO related to RFD at the time of discharge would be most helpful to our ability to understand the relationship of these components. In addition, although the potential effect of nonresponse bias should be considered for any survey results, this issue has been well studied for the HCAHPS survey and nonresponse weighting is not recommended20. A third potential limitation is that the extent to which other clinical events influenced our findings is unknown. Because this study includes both medical and surgical patients, it would be difficult to classify hospital complications similarly in those subsets. Also, the association of RFD and satisfaction remained significant in the subset of patients with hospital stays longer than 3 weeks (a surrogate for complicated hospital stays), suggesting that our findings are not merely the result of a difference in clinical outcomes. Fourth, as with any study examining readmission, accurately measuring readmission to all facilities is challenging. Depending on the patient population examined, readmission to nonindex hospitals ranges from 22% to 47% of total readmissions.21-23 Our readmission rate in both groups is therefore likely to be underestimated. In a large surgical patient population at our facility where all readmissions were captured by primary patient contact, the total readmission rate was 10.2% 24 compared to 14.5% seen in this study. However, because patients who were least satisfied with their initial hospital stay might be more likely to seek care at another hospital if readmission is required, this effect might be different between those RFD and LRFD and remains a limitation of our conclusions relative to readmission.
Although those RFD and LRFD overall were quite similar, the LRFD group had a significantly longer LOS compared with the group that was RFD. The relationship between hospital LOS and satisfaction has been previously examined and has shown inconsistent results.25-31 We have examined this relationship in our patient population and found no correlation between increasing LOS and decreasing satisfaction with the hospital. We did find a very small but significant correlation between longer LOS and decreasing satisfaction with physician communication. Because of both the very low correlation value and the fact that satisfaction differences remained highly significant in subgroups without a difference in LOS, the impact of the difference in LOS between those RFD and those LRFD is likely to have been minimal.
Future Directions
In practice, assessment of a patient's readiness for discharge in real time will likely help to improve patient satisfaction and better inform the discharge planning process. This could be easily and serially assessed on each hospital day and used to identify those patients in need of potential educational, social, or medical intervention. At our institution we have recently instituted a new discharge approach, that includes daily updates from the care team to the patient about the current plan for discharge day and time. Our data provide support for this approach, by demonstrating that readiness for discharge is associated with increased patient satisfaction. Our new process does not currently incorporate use of PRO, but this might well be an excellent metric to reexamine after the implementation of this discharge approach to determine its effect on patient-reported readiness for discharge.
Summary
In summary, this study has identified a strong and positive relationship between PRO, namely readiness for discharge, and an important quality metric, specifically patient satisfaction with hospital care. This is a novel finding and one in need of further study to understand how best to incorporate a patient's assessment of discharge readiness into the structural processes of transitions in care.
Supplementary Material
Acknowledgment
The authors thank the Wisconsin Surgical Outcomes Research Program (WiSOR) for manuscript review. No compensation was received from this group.
Support: Dr Schmocker was supported by NIH Grant 5T32CA090217-12.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure Information: Nothing to disclose.
References
- 1.Transforming healthcare: IOM panel discusses vision and reality after Crossing the Quality Chasm. Qual Lett Healthc Lead. 2004;16:9–12, 1. [PubMed] [Google Scholar]
- 2.Kotronoulas G, Kearney N, Maguire R, et al. What is the value of the routine use of patient-reported outcome measures toward improvement of patient outcomes, processes of care, and health service outcomes in cancer care? A systematic review of controlled trials. J Clin Oncol. 2014;32:1480–1501. doi: 10.1200/JCO.2013.53.5948. [DOI] [PubMed] [Google Scholar]
- 3.Patient Reported Outcomes (PRO) in Performace Measurement. National Quality Forum; Washington, DC: Jan 10, 2013. 2013. [Google Scholar]
- 4.Black N. Patient reported outcome measures could help transform healthcare. BMJ. 2013;346:f167. doi: 10.1136/bmj.f167. [DOI] [PubMed] [Google Scholar]
- 5.Jha AK, Orav EJ, Zheng J, Epstein AM. Patients' perception of hospital care in the United States. N Engl J Med. 2008;359:1921–1931. doi: 10.1056/NEJMsa0804116. [DOI] [PubMed] [Google Scholar]
- 6.Tsai TC, Jha AK. Surgical-readmission rates and quality of care. N Engl J Med. 2013;369:2460–2461. doi: 10.1056/NEJMc1313241. [DOI] [PubMed] [Google Scholar]
- 7.Tsai TC, Orav EJ, Jha AK. Patient satisfaction and quality of surgical care in US hospitals. Ann Surg. 2015;261:2–8. doi: 10.1097/SLA.0000000000000765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. [August 18, 2013];The Official Website for the Medicare Hospital Value-based Purchasing Program. 2013 (at http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/hospital-value-based-purchasing/index.html?redirect=/hospital-value-based-purchasing.)
- 9.Calculation of HCAHPS Scores: From Raw Data to Publicly Reported Results. Center for Medicare & Medicaid Services; 2012. [May 20, 2014]. (at http://www.hcahpsonline.org/Files/Calculation%20of%20HCAHPS%20Scores.pdf.) [Google Scholar]
- 10.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 11. [November 20, 2014];Guide to Interpreting. 2011 (at http://www.pressganey.com/Documents/pg_gti.pdf?viewFile.)
- 12.Jones TOS,WE. Why Satisfied Customers Defect. Harv Bus Rev. 1995;73:88–99. [Google Scholar]
- 13.Lee F. If Disney Ran Your Hospital: 9 1/2 Things You Would Do differently: Cultural Insights from a Hospital Executive Who Became a Disney Cast Member: Second River Healthcare. 2004 [Google Scholar]
- 14.Dahlke AR, Chung JW, Holl JL, et al. Evaluation of initial participation in public reporting of American College of Surgeons NSQIP surgical outcomes on Medicare's Hospital Compare website. J Am Coll Surg. 2014;218:374–380. 80, e1–5. doi: 10.1016/j.jamcollsurg.2013.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.HCAHPS Fact Sheet (CAHPS Hospital Survey) Centers for Medicare & Medicaid Services (CMS); 2013. [July 15, 2014]. (at http://www.hcahpsonline.org/files/August%202013%20HCAHPS%20Fact%20Sheet2.pdf.) [Google Scholar]
- 16.Boulding W, Glickman SW, Manary MP, et al. Relationship between patient satisfaction with inpatient care and hospital readmission within 30 days. Am J Manag Care. 2011;17:41–48. [PubMed] [Google Scholar]
- 17.Weiss M, Yakusheva O, Bobay K. Nurse and patient perceptions of discharge readiness in relation to postdischarge utilization. Med Care. 2010;48:482–486. doi: 10.1097/MLR.0b013e3181d5feae. [DOI] [PubMed] [Google Scholar]
- 18.Weiss ME, Costa LL, Yakusheva O, Bobay KL. Validation of patient and nurse short forms of the Readiness for Hospital Discharge Scale and their relationship to return to the hospital. Health Serv Res. 2014;49:304–317. doi: 10.1111/1475-6773.12092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Weiss ME, Piacentine LB, Lokken L, et al. Perceived readiness for hospital discharge in adult medical-surgical patients. Clin Nurse Spec. 2007;21:31–42. doi: 10.1097/00002800-200701000-00008. [DOI] [PubMed] [Google Scholar]
- 20.Elliott MN, Edwards C, Angeles J, et al. Patterns of unit and item nonresponse in the CAHPS (R) Hospital Survey. Health Serv Res. 2005;40:2096–2119. doi: 10.1111/j.1475-6773.2005.00476.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Saunders RS, Fernandes-Taylor S, Kind AJ, et al. Rehospitalization to primary versus different facilities following abdominal aortic aneurysm repair. J Vasc Surg. 2014;59:1502–1510. 10, e1–2. doi: 10.1016/j.jvs.2013.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yermilov I, Bentrem D, Sekeris E, et al. Readmissions following pancreaticoduodenectomy for pancreas cancer: a population-based appraisal. Ann Surg Oncol. 2009;16:554–561. doi: 10.1245/s10434-008-0178-6. [DOI] [PubMed] [Google Scholar]
- 23.Reddy DM, Townsend CM, Jr., Kuo YF, et al. Readmission after pancreatectomy for pancreatic cancer in Medicare patients. J Gastrointest Surg. 2009;13:1963–1974. doi: 10.1007/s11605-009-1006-4. discussion 1974-1975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tevis SE, Weber SM, Kent KC, Kennedy GD. Nomogram to predict postoperative readmission in patients who undergo general surgery. JAMA Surg. 2015 doi: 10.1001/jamasurg.2014.4043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schoenfelder T, Klewer J, Kugler J. Factors associated with patient satisfaction in surgery: the role of patients' perceptions of received care, visit characteristics, and demographic variables. J Surg Res. 2010;164:e53–59. doi: 10.1016/j.jss.2010.08.001. [DOI] [PubMed] [Google Scholar]
- 26.Nguyen Thi PL, Briancon S, Empereur F, Guillemin F. Factors determining inpatient satisfaction with care. Soc Sci Med. 2002;54:493–504. doi: 10.1016/s0277-9536(01)00045-4. [DOI] [PubMed] [Google Scholar]
- 27.Walsh M, Knott JC. Satisfaction with the emergency department environment decreases with length of stay. Emerg Med J. 2010;27:821–828. doi: 10.1136/emj.2009.079764. [DOI] [PubMed] [Google Scholar]
- 28.Boudreaux ED, Ary RD, Mandry CV, McCabe B. Determinants of patient satisfaction in a large, municipal ED: the role of demographic variables, visit characteristics, and patient perceptions. Am J Emerg Med. 2000;18:394–400. doi: 10.1053/ajem.2000.7316. [DOI] [PubMed] [Google Scholar]
- 29.Gares D. The relationship of acute inpatient hospital length of stay and patient satisfaction. Waring historical Library (MUSC): South Carolina medical University; 2011. [Google Scholar]
- 30.Quintana JM, Gonzalez N, Bilbao A, et al. Predictors of patient satisfaction with hospital health care. BMC Health Serv Res. 2006;6:102. doi: 10.1186/1472-6963-6-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tokunaga J, Imanaka Y. Influence of length of stay on patient satisfaction with hospital care in Japan. Int J Qual Health Care. 2002;14:493–502. doi: 10.1093/intqhc/14.6.493. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.