Abstract
Background
Many patients seek greater accessibility to healthcare. Meanwhile surgeons face increasing time constraints due to workforce shortages and elevated performance demands. Online postoperative care may improve patient access while increasing surgeon efficiency. We aimed to evaluate patient and surgeon acceptance of online postoperative care after elective general surgical operations.
Study Design
A prospective pilot study within an academic general surgery service compared online and in-person postoperative visits from May-December 2014. Included patients underwent elective laparoscopic cholecystectomy, laparoscopic ventral hernia repair, umbilical hernia repair, or inguinal hernia repair by one of five surgeons. Patients submitted symptom surveys and wound pictures, then corresponded with their surgeons using an online patient portal. The primary outcome was patient-reported acceptance of online visits in lieu of in-person visits. Secondary outcomes included detection of complications via online visits, surgeon-reported effectiveness, and visit times.
Results
Fifty patients completed both online and in-person visits. Online visits were acceptable to most patients as their only follow-up (76%). For 68% of patients, surgeons reported that both visit types were equally effective, while clinic visits were more effective in 24% and online visits in 8%. No complications were missed via online visits, which took significantly less time for patients (15 versus 103 minutes, p<0.01) and surgeons (5 versus 10 minutes, p<0.01).
Conclusions
In this population, online postoperative visits were accepted by patients and surgeons, took less time, and effectively identified patients who required further care. Further evaluation is needed to establish the safety and potential benefit of online postoperative visits in specific populations.
Keywords: online patient portal, telemedicine, store-and-forward, surgery, postoperative, smartphone
BACKGROUND
Many patients seek more convenient access to healthcare services. In traditional healthcare delivery models, this can put a strain on providers, who face increasing time constraints due to elevated performance demands, modified payment models, and workforce shortages.1,2 Now more than ever, providers and delivery systems are challenged to identify ways to optimize clinical outcomes and patient satisfaction while minimizing inefficiency.1 Many health systems and individual providers have responded to the Institute of Medicine’s proposed solution to “develop multiple ways to respond to patients’ needs beyond patient visits,”3 relying on web-based technology to extend the care environment both temporally and spatially beyond clinics, operating rooms, and inpatient wards.4–7
A cornerstone of this informatics-enriched approach to healthcare delivery is the online patient portal, which typically provides patients with the ability to access their medical records, review important health information, and engage in two way electronic messaging with care providers.8,9 Online portals have reoriented care around patients, offering them the opportunity to independently access health information and input their own health data into care conversations (and often into the medical record).8,10–14 An added benefit of online portals is asynchronous communication between patients and care teams, enabling patients and providers to address health care needs at times and locations that are convenient for them.15–18
Patients and providers are also realizing the benefits of sharing digital images asynchronously using electronic transmission. Classically known as “store-and-forward” telemedicine, this approach has been used successfully to provide clinical assessments and follow-up care in dermatology, plastic surgery, and burn care.19–25 Often, these images are captured by a clinician in one setting and shared with another clinician elsewhere. To date, there has been minimal incorporation of these new care delivery modalities into general surgical care, and patients have been less frequently relied upon to generate their own data in the form of digital images.26 However, much general surgical care, particularly in the postoperative setting, may be effectively managed using electronic messaging and sharing of patient-generated digital images for wound evaluation. This approach could increase patient access to convenient postoperative care, expedite decisions about management, and increase surgeon efficiency, making it a preferred method of follow-up for appropriate patients after operations. We hypothesized that in the majority of low risk elective general surgical cases, patients and surgeons would find online postoperative care acceptable for accomplishing the objectives of surgical follow-up.
METHODS
We conducted a prospective pilot study comparing online and in-person general surgery postoperative visits at Vanderbilt University Medical Center, an academic tertiary referral center in the Southeastern United States. Enrollment occurred from May through November 2014, and postoperative visits were completed from June through December 2014. All participants completed both online and traditional (in-person) visits with their surgeons during the one month interval after their operations. Online visits were performed in an asynchronous fashion, and included a secure symptom survey, surgeon review of wound pictures taken by patients, and correspondence using a secure online patient portal. The primary outcome was patient acceptance of online versus in-person care, measured by patient response to the question “Would you be okay with having your follow-up done as an online visit only (yes/no)?” Secondary outcomes included patient preferences for online versus in-person visits, surgeon comparisons of the efficacy of online versus in-person visits, amount of time required for patients and surgeons to complete each visit type, and agreement between findings on online versus in-person evaluations.
The study population included adult patients who underwent an elective general surgical operation by one of five participating surgeons. Operations included laparoscopic cholecystectomy, laparoscopic or open umbilical or epigastric hernia repair, laparoscopic or open inguinal hernia repair, and laparoscopic ventral hernia repair. Patients were excluded if they underwent an emergent operation or had an intraoperative or immediate postoperative complication (i.e. prior to surgical discharge). Patients scheduled for an eligible procedure were screened for participation at their preoperative clinic visit. Patients meeting the following criteria, either independently or with the assistance of a person they identified, were invited to participate by a member of the research team other than their surgeon: 1. Previous use or expressed desire to begin using the institution’s online patient portal; 2. Ability to access the internet; and 3. Ability to take and upload a digital picture to a secure site. Some patients were not approached due to unavailability of research personnel to conduct recruitment activities at the times of their preoperative visits. Patients who consented to participate reported basic demographic information including travel distances from their home of residence to the surgical clinic, current employment status, highest level of education completed, and whether they intended to receive assistance in completing online visit activities.
During their preoperative visit, consented participants were assisted in setting up an online portal account (if not already done) and participated in a demonstration by study personnel of how to complete the online survey on a digital tablet, including taking and uploading digital pictures into the online survey. Participants were instructed to take a “close up” picture of each wound, as well as a “zoomed out” picture encompassing all wounds when more than one was present (eg. laparoscopic cholecystectomy, laparoscopic hernia repairs). Postoperative clinic visits were scheduled for approximately four weeks after the planned operation. Online visits were scheduled for one week prior to the planned postoperative visit to allow time for completion of all online visit activities before the in-person visit.
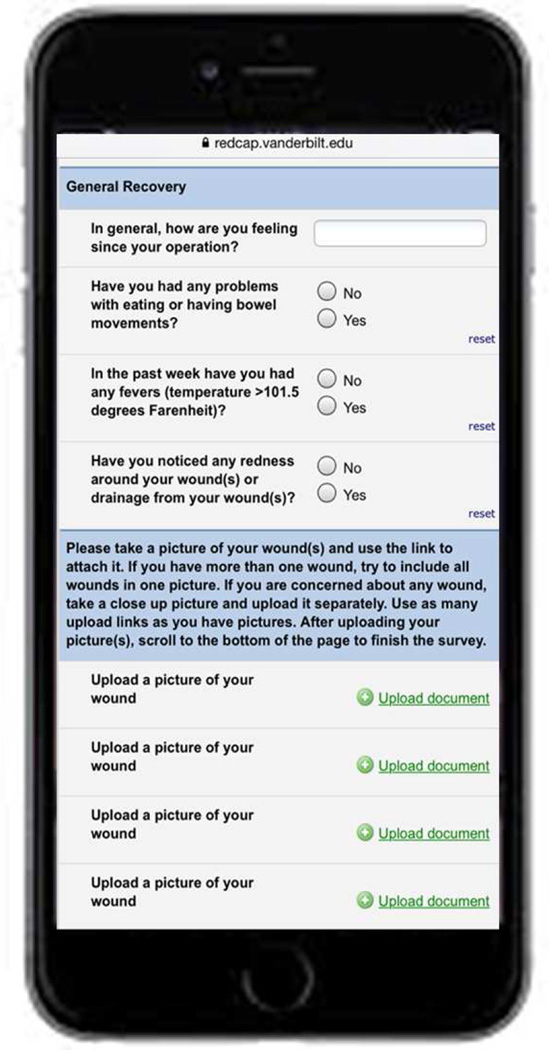
The online visit capitalized on existing informatics and research resources at Vanderbilt University Medical Center. Vanderbilt’s online patient portal, www.myhealthatvanderbilt.com (MHAV), provides a way for patients to access health data and communicate with their care providers in a secure setting outside of traditional clinic visits.27 On the date of the online visit, the patient portal was used to send patients a reminder with the web address for the online survey, which was developed by group discussion and consensus among the participating surgeons about necessary elements of postoperative assessment. The survey included symptom-based questions, image upload links, and free text boxes for participant comments (Figure 1). The survey was administered using Vanderbilt REDCap (Research Electronic Data Capture), a widely-used, HIPAA compliant tool for building and managing secure online surveys.28 Participants could use a personal smartphone, digital tablet, or computer and digital camera to complete the online visit. Surgeons responded to patients about their symptom reports and wound images in an asynchronous fashion (ie. at a different time) using the online portal, through which all patient-provider electronic conversations were automatically documented in the electronic medical record.27 Patients who did not access the reminder message or complete the survey within 48 hours were called by a member of the study team to remind them to complete their online visit.
Figure 1.
Patient symptom survey and image upload links. Patients provided information on postoperative recovery, pertinent symptoms, and wound images using a secure online survey. Symptom questions for which “yes” was selected branched to text box where they could provide an explanation. Additional free text boxes permitted extended responses and patient questions. Surgeons responded via the online patient portal.
Traditional in-person clinic visits were conducted by participating surgeons in the standard fashion. After participants completed both visits, they and their surgeons independently completed written assessments of the adequacy of the online visit relative to the in-person visit, estimated time to complete visit activities including travel and wait time, whether they would accept online visits as the sole mechanism for postoperative follow-up, and their preference for an online versus in-person visit.
One protocol change was made near the beginning of the pilot. Participants had initially been randomized to complete the online and in-person visits in one of two sequences: online visit then clinic visit (online-then-clinic) or clinic visit then online visit (clinic-then-online). Of the first seven participants in the clinic-then-online group, six did not complete the online visits. Participants stated that they did not see value in completing the online visit after they had already seen their surgeons, even for research purposes. Hence, the approach of visit sequencing was not believed to be feasible, and all subsequent participants were converted to the online-then-clinic sequence. The study was completed after 50 patients participated in both online and clinic visits, as the research team determined that the pilot had achieved its primary objective of evaluating patient acceptance of online care.
Patient and operative characteristics associated with patient acceptance of online postoperative care were compared using chi-squared tests for categorical variables and student’s t-test or Wilcoxon rank sum test for continuous variables with parametric and non-parametric distributions, respectively. Differences between visit times for patients and surgeons were compared using Wilcoxon rank sum tests. Qualitative feedback from patients and surgeons were analyzed to identify key factors and mechanisms associated with online visit acceptance.29
In sub-analyses, we compared demographic characteristics of patients who were eligible versus those who were ineligible. We also compared consented participants based on whether or not they completed the online visit. We used descriptive statistics, chi-squared tests for categorical variables, and Wilcoxon rank sum tests for continuous variables, which were nonparametric.
RESULTS
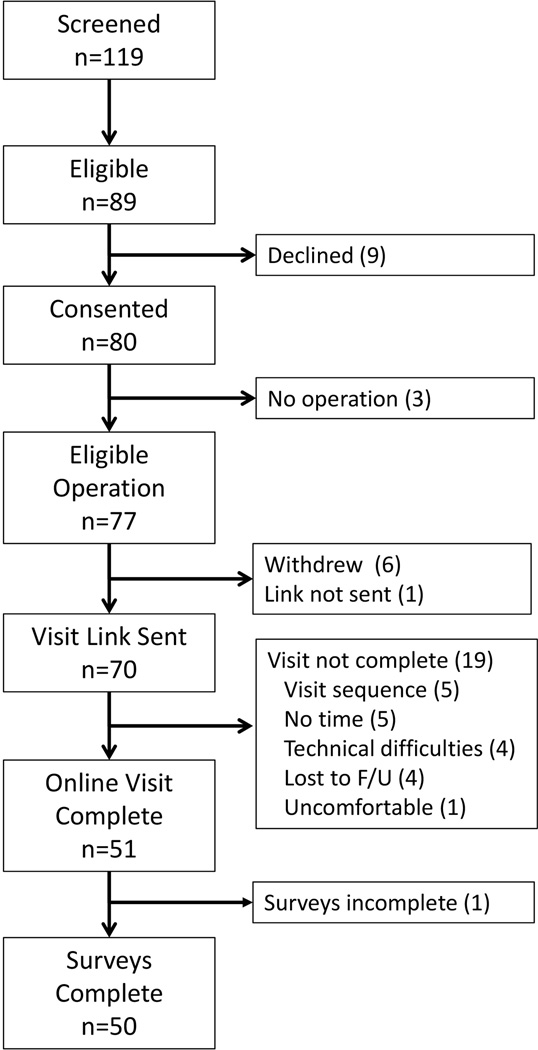
Of patients scheduled for included operations on study recruitment days, 94% were evaluated for eligibility. Of these, 75% (89/119) were eligible and 90% (80/89) consented to participate (Figure 2). Ten participants subsequently withdrew or became ineligible for the study (3 did not undergo the scheduled operation, 6 withdrew after giving consent but prior to the operation, 1 did not receive the online follow-up link). Among 70 participants to whom the online visit link was sent, 51 completed an online postoperative visit (73%). Excluding participants who did not complete clinic or online visits (4) and those who were initially randomized to the clinic-then-online visit sequence (6), 84% (51/61) of eligible patients completed the online visit. Complete data were available for 98% of participants (50/51, 1 participant did not complete the survey at study conclusion). Reasons for incomplete online visits included loss to follow-up (patients did not complete the online visit or attend the clinic visit), assignment to the clinic-then-online sequence, inadequate time to do the online visit in addition to the clinic visit, technical difficulties, and lack of comfort taking a picture of a sensitive site (Figure 2).
Figure 2.
Cohort flow. Potential participants screened, eligible, consented, and included in the study. Reasons for non-participation and study exclusion are listed (number of participants).
Participants were on average 49 years old (±15), and traveled a median of 24 miles from their homes to the surgical clinic (range 2–139) (Table 1). All participants had at least some high-school education, 60% had obtained a Bachelor’s degree or higher level of education, and 68% percent were employed. Half of participants (25/50) underwent inguinal hernia repair, while 26% (13/50) underwent laparoscopic cholecystectomy, 18% (9/50) umbilical or epigastric hernia repair, and 6% (3/50) laparoscopic ventral hernia repair (Table 2). Most participants were treated by a surgeon who had been in practice for 15 or more years (34/50, 68%). The majority used a smartphone to complete the online visit (28/50, 56%), while a minority used a tablet (14/50, 28%) or digital camera and computer (8/50, 16%).
Table 1.
Participant Characteristics
| Characteristic | Data, n=50 |
|---|---|
| Age, y, mean±SD | 49±15 |
| Travel distance, miles, median (range) | 24 (2–139) |
| Education, n (%) | |
| High School | 11 (22) |
| Associate’s degree | 9 (18) |
| Bachelor’s degree | 14 (28) |
| Masters/doctoral degree | 16 (32) |
| Employment, n (%) | |
| Employed | 34 (68) |
| Unemployed | 4 (8) |
| Student | 5 (10) |
| Retired | 7 (14) |
| Operation, n (%) | |
| Laparoscopic/open inguinal hernia repair | 25 (50) |
| Laparoscopic cholecystectomy | 13 (26) |
| Laparoscopic/open umbilical/epigastric hernia repair | 9 (18) |
| Laparoscopic ventral hernia repair | 3 (6) |
| Patients’ surgeons’ experience, n (%) | |
| < 15 y in practice | 16 (32) |
| ≥ 15 y in practice | 34 (68) |
Table 2.
Factors Associated with Patient Acceptance of Online Postoperative Care
| Patient and operative characteristics | Accept online care, n=38 |
Do not accept online care, n=12 |
p Value |
|---|---|---|---|
| Age, y, mean±SD | 49±14 | 52±18 | 0.45 |
| Travel distance, miles, median (IQR) | 27 (15–45) | 15 (10–27) | 0.09 |
| Education, n (%) | 0.64 | ||
| High school | 7 (18) | 4 (33) | |
| Associate’s degree | 7 (18) | 2 (17) | |
| Bachelor’s degree | 12 (32) | 2 (17) | |
| Masters/doctoral degree | 12 (32) | 4 (33) | |
| Employment, n (%) | 0.68 | ||
| Employed | 25 (66) | 9 (75) | |
| Unemployed | 4 (11) | 0 (0) | |
| Student | 5 (13) | 2 (17) | |
| Retired | 4 (11) | 1 (8) | |
| Operation, n (%) | 0.45 | ||
| Laparoscopic/open inguinal hernia repair | 17 (45) | 8 (67) | |
| Laparoscopic cholecystectomy | 10 (26) | 3 (25) | |
| Laparoscopic/open umbilical/epigastric hernia repair | 8 (21) | 1 (8) | |
| Laparoscopic ventral hernia repair | 3 (8) | 0 (0) | |
| Patients’ surgeons’ experience, n (%) | 0.55 | ||
| Less than 15 years in practice | 13 (34) | 3 (25) | |
| 15 or more years in practice | 25 (66) | 9 (75) | |
| Device used, n (%) | 0.42 | ||
| Smartphone | 22 (58) | 6 (50) | |
| Tablet | 9 (24) | 5 (42) | |
| Computer/digital camera | 7 (18) | 1 (8) | |
| Required assistance, n (%) | 0.04 | ||
| No | 28 (74) | 5 (42) | |
| Yes | 10 (26) | 7 (58) | |
| Difference in patient time for online versus clinic visit, min, median (IQR) | 90 (60–130) | 53 (23–73) | <0.01 |
IQR, interquartile range; SD, standard deviation.
Seventy-six percent of patients (38/50) reported that they would be okay with only having an online visit for their postoperative care. Patients who accepted online care were less likely to require assistance with visit activities (58 vs. 26%, p=0.04) and reported a greater difference between times required to complete online versus in-person visit activities (90 vs. 53 minutes, p<0.01) (Table 2). Most participants either preferred the online visit over the clinic visit or expressed no preference (34% preferred online, 34% no preference, 32% preferred clinic). Including travel time, clinic visits took a median of 103 minutes for patients (interquartile range (IQR) 60–130), compared with 15 minutes (IQR 10–30) for online visits (p<0.01). For surgeons, clinic visits took a median of 10 minutes (IQR 5–10) versus 5 minutes (IQR 3–5) for online visits (p<0.01) (Table 3).
Table 3.
Patient- and Surgeon-Reported Visit Times for Online vs Clinic Visits
| Visit times, min | Online visit, n=50 |
Clinic visit, n=50 |
p Value |
|---|---|---|---|
| Patient time, median (IQR)* | 15 (10–30) | 103 (60–130) | <0.01 |
| Surgeon time, median (IQR) | 5 (3–5) | 10 (5–10) | <0.01 |
Patient-reported visit times include travel.
IQR, interquartile range.
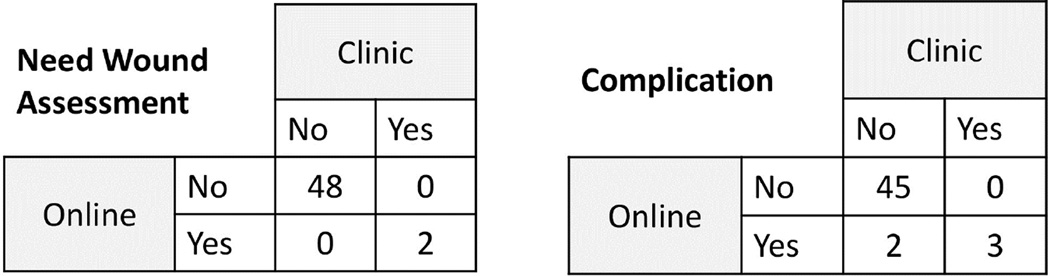
Surgeons reported that online and clinic visits were equally effective for 68% (34/50) of patients, while the clinic visit was more effective for 24% (12/50) and the online visit more effective for 8% (4/50). Evaluative findings on online versus clinic visits were generally in agreement (Figure 3). Considering the clinic visit as the gold standard, there were three true positive and two false positive findings on online visits. For three participants with true positive findings, the online visit revealed postoperative complications that were confirmed upon clinic visit (two wound infections, one case of postoperative urinary incontinence). For the two participants with false positive findings, the online visit suggested a postoperative complication that was not found at the time of clinic visit (both were participants whose symptom surveys suggested concern for early hernia recurrence, which was not present on physical exam).
Figure 3.
Comparison of findings: online versus clinic visits. Evaluative findings from online and clinic visits were compared based on need for wound assessment/care and any postoperative complication. On online visits in “Wound Assessment” there were 2 true positives (both surgical site infections) and in “Complication” there were 3 true positives (2 surgical site infections, 1 case of urinary retention) and 2 false positives (patient concern for hernia recurrence).
Qualitative analysis of unstructured comments from patient participants who preferred online visits revealed convenience and decreased travel as important factors in their preference, while those who preferred clinic visits cited preference for face-to-face communication and uncertainty regarding online assessment or their ability to perform self-assessment (Table 4). Surgeons emphasized benefits to patients in terms of time and travel distance in situations when the online visit was equally or more effective, while they reported need for physical exam, poor photography, or improved communication in situations when the clinic visit was favored (Table 4).
Table 4.
Reasons for Patients’ and Surgeons’ Preferences for Clinic and Online Visits
| Prefer Clinic | Prefer Online |
|---|---|
| Patient | |
| Communication “prefer personal conversations” “easier to communicate, ask follow-up questions” “I like face-to-face” |
Convenience “didn’t miss work” “quick and easy, perfect for busy people” “easy, less time consuming, and questions were addressed” |
| Confidence in self/online assessment “don’t trust myself to provide all the pertinent info, I don’t know what to look for” “I have more confidence with [my surgeon] eyeballing my wound than the ‘selfie’” |
Decreased travel “less travel” “saves trip and time” |
| Surgeon | |
| Exam needed “exam was necessary to address patient concern for recurrent hernia” “large seroma – needed counseling based on physical exam” |
Perceived benefits to patient “patient lives 2 hours away and could have avoided postop visit” “excellent patient for online follow-up as she lives about 2 hours away” |
| Image quality “photo too magnified, did not give accurate representation of the situation” “photography was poor” |
Image quality “good pictures” |
| Communication “in-person better for interpersonal communication, the patient appreciates interaction” “I made her laugh and feel better – that may be helpful for rapport later if she develops infection, recurrence, etc.” |
Clinic logistics “my appointments were running late – patient had to leave then come back – very disruptive to his schedule – all could have been avoided with online visit” |
Comparing eligible versus ineligible patients, eligible patients were younger (median 50 years (interquartile range (IQR) 40–63) versus 63 years (47–73), p<0.01), but there were no differences with respect to gender, race, or insurance status. Among consented participants who maintained study eligibility, whites were more likely than non-whites to complete the online visit (90 versus 67%, p<0.01). There were no differences in online visit completion rates with respect to age, gender, or insurance status.
DISCUSSION
This study involved the novel use of an online patient portal and secure online survey with a digital image upload feature to provide postoperative care for general surgical patients. Online visits were accepted by the majority of patients. Surgeons reported that online visits were equally or more effective than in-person visits in most cases. Further, online visits took significantly less time for both patients and surgeons.
The concept of providing healthcare remotely is well-established in non-surgical specialties and has been traditionally viewed as a means to increase rural patients’ access to care.30 As technology improves and smartphone use becomes ubiquitous, patients are now seeking remote care for other reasons, including 24/7 access and convenience.15–18 This is evidenced by widespread adoption of online patient portals.9,10,31 In light of these changes in how healthcare is delivered, some surgeons have begun to re-consider the essential elements of perioperative care and to re-define how care is delivered.
A retrospective review of postoperative visits after cholecystectomies and appendectomies found that only 14% of patients received any intervention (including wound or drain management, medication prescriptions, imaging, readmission from clinic, or scheduling an additional follow-up appointment), with only 9% requiring “hands-on” interventions.32 Accordingly, some surgeons have removed “hands-on” assessments, conducting perioperative visits using secure two-way interactive video.33–37 Still others have eliminated both “hands-on” and visual assessments, using telephone to follow-up adults after laparoscopic cholecystectomy and inguinal hernia repair as well as a variety of minor pediatric general surgical procedures.38–40 Both video and telephone-based care are limited in that they must be performed in a synchronous fashion, with both patient and surgeon available concurrently to participate in follow-up. Telephone assessments are further limited in their inability to visually assess the surgical site. Our online tool may be advantageous in that it facilitates visual assessment and can be completed and viewed at different times that are more convenient for patients and surgeons.
The use of wound images for assessment is an example of store-and-forward telemedicine, which has been employed in multiple areas of care provision including dermatology, plastic surgery, and burn care, but has traditionally relied upon a trained clinician as photographer.19–24,26 As a result of smartphone-based digital cameras, most people now have basic familiarity with image capture and sharing.41 Prior survey-based work suggested that most patients would be willing to use smartphones for wound surveillance after vascular surgery procedures.42 Our pilot study applied this finding by asking general surgery patients to submit wound pictures for postoperative assessment, and found similar patient acceptance. We demonstrated that in the majority of cases, online visits incorporating images taken by patients were perceived by surgeons as effective for postoperative assessment. These findings suggest that online wound assessment in conjunction with a symptom survey and patient-surgeon electronic communication could potentially substitute for, rather than augment, in-person postoperative care. However, before this concept can be adopted widely, there is a need to establish standards for image quality and confidentiality of data transmission, as well as to train surgeons to discern when patient-generated data are sufficient for clinical assessment.43
An intrinsic feature of the online visit was automatic documentation of patient-surgeon communications in patient electronic medical records. Because data are generated by the patient, this documentation may be regarded as more accurate and descriptive than a traditional clinic note written by a surgeon, which is limited to the surgeon’s perception and written evaluation of the patient’s symptoms and physical findings. Further, it could substitute for traditional visit documentation, which requires significant surgeon time.
Reimbursement for non-face-to-face care remains problematic under traditional fee-for-service payment models, many of which do not yet pay for online care. As a result, hospital systems with alternate payment models, including capitation and accountable care organizations, have more readily adopted online care.18 Currently, postoperative care provided within 90 days of an operation is included in a global payment for the operation regardless of the number or type of interactions required. As such, surgeons are incentivized to use modalities of care provision that maximize quality and efficiency. Visits that can be accomplished online may free up surgeon and clinic resources, which can be used to care for other patients.
Online visits were initiated by a reminder message from a member of the research team who was not involved in the patient’s clinical care. When implemented in routine practice, this responsibility could be undertaken by a surgeon, surgeon-extender, or other clinic staff member, such as a nurse. In some settings, including our clinic, nurses routinely address basic telephone and online portal communications with patients, serving an important triage role for providers.31 Clinic nurses could function in a similar role with respect to initiation of online visits, although training needs and implications for staff workload will need to be further evaluated.
There are several limitations to this study. As a small pilot study in a single academic general surgery practice, it is not certain whether our findings could be applied in other settings. We used a locally developed online patient portal with unique policies and procedures, but the basic functionality of our portal mirrors that of widely-used commercial products, so this application likely does represent a generalizable tool for online postoperative care.8 Further, our use of online REDCap surveys for patient submission of symptom data and wound images can be replicated by providers in various settings and can be customized to accommodate various operation types, which further increases the generalizability of this tool.28
While we are reassured that all postoperative complications were detected via online visits and subsequently validated by in-person assessment, we must acknowledge that the study was not adequately powered to detect these differences given the low incidence of complications in this population of patients undergoing low risk, elective operations.
An additional limitation relates to the fact that patients completed sequential online and in-person visits. We cannot predict the potential impact of online-only visits on patient acceptance of online care or time required to complete postoperative care. Because patients knew that they would see their surgeon for a second encounter after the online visit, they may have been less motivated to address all questions and concerns during the online visit. It is possible that patients may have required greater reassurance and/or more follow-up communication if the online visit had been their only visit. The impact of this on patient acceptance of online care and surgeon workflow are yet to be determined, but could modify patient impressions of online care and negate surgeon efficiency as an observed benefit of online postoperative care. Given the large difference in time to complete visit activities for patients, we suspect that even if more online communication had been required, patients would still have experienced a decrease in visit times for online versus in-person care.
The proportion of online visits completed among eligible participants was reasonable, but loss to follow up was slightly higher than with traditional clinic visits in this cohort. Loss to follow-up due to missed online visits is a potential concern that will need to be studied in a future cohort receiving only online care. We also acknowledge that the study sample was limited to patients undergoing relatively low risk general surgical operations and those patients who had adequate technological experience to complete an online visit, including the ability to use the internet, take digital images of their wound(s), and upload the images into an online survey. While our recruitment efforts did target a representative sample of patients undergoing included operations, we found that younger patients were more likely to be eligible for the study based on technological requirements. We also found that consented participants who were non-white were less likely to complete the online visit. Moving forward, it will be important to understand these differences in uptake and use of online visit tools, which may be used to tailor instructions and interventions to maximize accessibility to diverse populations. Additionally, further research is needed to define the range of operations for which online care is appropriate.
CONCLUSIONS
Online postoperative care can be accomplished using an online patient portal and data submitted by patients including symptom reports and wound images. This study demonstrated the utility of online postoperative visits as a triage tool for identifying patients who require in-person surgeon assessment. The data revealed potential advantages of online postoperative care, including convenient access for patients, decreased patient travel times, and surgeon efficiency gains; however, these must be carefully weighed against potential detriments of using patient-generated data to provide clinical assessment, including concerns about liability, provider work burden, and modified patient-provider relationships. Further research and ongoing discussions are needed to understand appropriate indications for and outcomes of online postoperative care, as well as implications for care quality, patient satisfaction, and efficiency of care delivery.
ACKNOWLEDGMENT
The authors wish to thank Dr Gretchen Jackson Purcell for her thoughtful review and feedback on the manuscript.
Disclosures outside the scope of this work: Dr. Poulose receives research support from Bard-Davol and is a paid consultant to Ariste Medical.
Support: This material is based upon work supported by the Office of Academic Affiliations (OAA), Department of Veterans Affairs, VA National Quality Scholars Program and with use of facilities at VA Tennessee Valley Healthcare System, Nashville, TN. The project was also supported by the National Center for Research Resources, Grant UL1RR024975-01, and is now at the National Center for Advancing Translational Sciences, Grant 2UL1 TR000445-06. The content is soley the responsibility of the authors and does not necessarily represent the official views of the VA or NIH.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure Information: Nothing to disclose.
Presented at the American College of Surgeons 101st Annual Clinical Congress, Scientific Forum, Chicago, IL, October 2015.
REFERENCES
- 1.Porter M. The strategy that will fix healthcare. Harvard Bus Rev. 2013 Oct [Google Scholar]
- 2.Detsky AS. What patients really want from health care. JAMA. 2011;306:2500–2501. doi: 10.1001/jama.2011.1819. [DOI] [PubMed] [Google Scholar]
- 3.Institute of Medicine. Crossing the Quality Chasm. Washington, DC: National Academy Press; 2001. [Google Scholar]
- 4.Kaplan B, Brennan PF. Consumer informatics supporting patients as co-producers of quality. J Am Med Inform Assoc. 2001;8:309–316. doi: 10.1136/jamia.2001.0080309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.de Jongh T, Gurol-Urganci I, Vodopivec-Jamsek V, et al. Mobile phone messaging for facilitating self-management of long-term illnesses. Cochrane Database Syst Rev. 2012;12 doi: 10.1002/14651858.CD007459.pub2. CD007459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mosa AS, Yoo I, Sheets L. A systematic review of healthcare applications for smartphones. BMC Med Inform Decis Mak. 2012;12:67. doi: 10.1186/1472-6947-12-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Umefjord G, Petersson G, Hamberg K. Reasons for consulting a doctor on the Internet: Web survey of users of an Ask the Doctor service. J Med Internet Res. 2003;5:e26. doi: 10.2196/jmir.5.4.e26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Goldzweig CL, Orshansky G, Paige NM, et al. Electronic patient portals: evidence on health outcomes, satisfaction, efficiency, and attitudes: a systematic review. Ann Intern Med. 2013;159:677–687. doi: 10.7326/0003-4819-159-10-201311190-00006. [DOI] [PubMed] [Google Scholar]
- 9.Goldzweig CL, Towfigh AA, Paige NM, et al. Systematic Review: Secure Messaging Between Providers and Patients, and Patients' Access to Their Own Medical Record: Evidence on Health Outcomes, Satisfaction, Efficiency and Attitudes. Washington (DC): 2012. [PubMed] [Google Scholar]
- 10.Ammenwerth E, Schnell-Inderst P, Hoerbst A. The impact of electronic patient portals on patient care: a systematic review of controlled trials. J Med Internet Res. 2012;14:e162. doi: 10.2196/jmir.2238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gann B. Giving patients choice and control: health informatics on the patient journey. Yearb Med Inform. 2012;7:70–73. [PubMed] [Google Scholar]
- 12.Cimino JJ, Patel VL, Kushniruk AW. The patient clinical information system (PatCIS): technical solutions for and experience with giving patients access to their electronic medical records. Int J Med Inform. 2002;68:113–127. doi: 10.1016/s1386-5056(02)00070-9. [DOI] [PubMed] [Google Scholar]
- 13.Earnest MA, Ross SE, Wittevrongel L, et al. Use of a patient-accessible electronic medical record in a practice for congestive heart failure: patient and physician experiences. J Am Med Inform Assoc. 2004;11:410–417. doi: 10.1197/jamia.M1479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ross SE, Moore LA, Earnest MA, et al. Providing a web-based online medical record with electronic communication capabilities to patients with congestive heart failure: randomized trial. J Med Internet Res. 2004;6:e12. doi: 10.2196/jmir.6.2.e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Umefjord G, Sandstrom H, Malker H, Petersson G. Medical text-based consultations on the Internet: a 4-year study. Int J Med Inform. 2008;77:114–121. doi: 10.1016/j.ijmedinf.2007.01.009. [DOI] [PubMed] [Google Scholar]
- 16.Umefjord G, Hamberg K, Malker H, Petersson G. The use of an Internet-based Ask the Doctor Service involving family physicians: evaluation by a web survey. Family Practice. 2006;23:159–166. doi: 10.1093/fampra/cmi117. [DOI] [PubMed] [Google Scholar]
- 17.Otte-Trojel T, de Bont A, Rundall TG, van de Klundert J. How outcomes are achieved through patient portals: a realist review. J Am Med Inform Assoc. 2014;21:751–757. doi: 10.1136/amiajnl-2013-002501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bishop TF, Press MJ, Mendelsohn JL, Casalino LP. Electronic communication improves access, but barriers to its widespread adoption remain. Health Affairs. 2013;32:1361–1367. doi: 10.1377/hlthaff.2012.1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Whited JD, Hall RP, Foy ME, et al. Teledermatology's impact on time to intervention among referrals to a dermatology consult service. Telemed J E Health. 2002;8:313–321. doi: 10.1089/15305620260353207. [DOI] [PubMed] [Google Scholar]
- 20.Hsiao JL, Oh DH. The impact of store-and-forward teledermatology on skin cancer diagnosis and treatment. J Am Acad Dermatol. 2008;59:260–267. doi: 10.1016/j.jaad.2008.04.011. [DOI] [PubMed] [Google Scholar]
- 21.Barbieri JS, Nelson CA, James WD, et al. The reliability of teledermatology to triage inpatient dermatology consultations. JAMA Dermatol. 2014;150:419–424. doi: 10.1001/jamadermatol.2013.9517. [DOI] [PubMed] [Google Scholar]
- 22.Trovato MJ, Scholer AJ, Vallejo E, et al. eConsultation in plastic and reconstructive surgery. Eplasty. 2011;11:e48. [PMC free article] [PubMed] [Google Scholar]
- 23.Wallace DL, Jones SM, Milroy C, Pickford MA. Telemedicine for acute plastic surgical trauma and burns. J Plast Reconstr Aesthet Surg. 2008;61:31–36. doi: 10.1016/j.bjps.2006.03.045. [DOI] [PubMed] [Google Scholar]
- 24.Chen CH, Young TH, Huang CH, et al. Patient-centered wound teleconsultation for cutaneous wounds: a feasibility study. Ann Plast Surg. 2014;72:220–224. doi: 10.1097/SAP.0000000000000031. [DOI] [PubMed] [Google Scholar]
- 25.Boccara D, Chaouat M, Uzan C, et al. Retrospective analysis of photographic evaluation of burn depth. Burns. 2011;37:69–73. doi: 10.1016/j.burns.2010.05.017. [DOI] [PubMed] [Google Scholar]
- 26.Mora F, Cone S, Rodas E, Merrell RC. Telemedicine and electronic health information for clinical continuity in a mobile surgery program. World J Surg. 2006;30:1128–1134. doi: 10.1007/s00268-005-0204-9. [DOI] [PubMed] [Google Scholar]
- 27.Osborn CY, Rosenbloom ST, Stenner SP, et al. My Health At Vanderbilt: policies and procedures governing patient portal functionality. J Am Med Inform Assoc. 2011;18:i18–i23. doi: 10.1136/amiajnl-2011-000184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Glaser BG, Strauss AL. The discovery of grounded theory; strategies for qualitative research. Chicago: Aldine Pub. Co.; 1967. [Google Scholar]
- 30.Currell R, Urquhart C, Wainwright P, Lewis R. Telemedicine versus face to face patient care: effects on professional practice and health care outcomes. Nurs Times. 2001;97:35. [PubMed] [Google Scholar]
- 31.Cronin RM, Davis SE, Shenson JA, et al. Growth of secure messaging through a patient portal as a form of outpatient interaction across medical specialties. Appl Clin Inform. 2015;6:288–304. doi: 10.4338/ACI-2014-12-RA-0117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chen DW, Davis RW, Balentine CJ, et al. Utility of routine postoperative visit after appendectomy and cholecystectomy with evaluation of mobile technology access in an urban safety net population. J Surg Res. 2014;190:478–483. doi: 10.1016/j.jss.2014.04.028. [DOI] [PubMed] [Google Scholar]
- 33.Wallace P, Haines A, Harrison R, et al. Joint teleconsultations (virtual outreach) versus standard outpatient appointments for patients referred by their general practitioner for a specialist opinion: a randomised trial. Lancet. 2002;359:1961–1968. doi: 10.1016/s0140-6736(02)08828-1. [DOI] [PubMed] [Google Scholar]
- 34.Harrison R, Clayton W, Wallace P. Virtual outreach: a telemedicine pilot study using a cluster-randomized controlled design. J Telemed Telecare. 1999;5:126–130. doi: 10.1258/1357633991933440. [DOI] [PubMed] [Google Scholar]
- 35.Augestad KM, Lindsetmo RO. Overcoming distance: video-conferencing as a clinical and educational tool among surgeons. World J Surg. 2009;33:1356–1365. doi: 10.1007/s00268-009-0036-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Harno K, Arajarvi E, Paavola T, et al. Clinical effectiveness and cost analysis of patient referral by videoconferencing in orthopaedics. J Telemed Telecare. 2001;7:219–225. doi: 10.1258/1357633011936435. [DOI] [PubMed] [Google Scholar]
- 37.Haukipuro K, Ohinmaa A, Winblad I, et al. The feasibility of telemedicine for orthopaedic outpatient clinics--a randomized controlled trial. J Telemed Telecare. 2000;6:193–198. doi: 10.1258/1357633001935347. [DOI] [PubMed] [Google Scholar]
- 38.Hwa K, Wren SM. Telehealth follow-up in lieu of postoperative clinic visit for ambulatory surgery: results of a pilot program. JAMA Surg. 2013;148:823–827. doi: 10.1001/jamasurg.2013.2672. [DOI] [PubMed] [Google Scholar]
- 39.Eisenberg D, Hwa K, Wren SM. Telephone follow-up by a midlevel provider after laparoscopic inguinal hernia repair instead of face-to-face clinic visit. JSLS. 2015;19 doi: 10.4293/JSLS.2014.00205. e2014 00205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.McVay MR, Kelley KR, Mathews DL, et al. Postoperative follow-up: is a phone call enough? J Pediatr Surg. 2008;43:83–86. doi: 10.1016/j.jpedsurg.2007.09.025. [DOI] [PubMed] [Google Scholar]
- 41.Pew Research Center. The Smartphone Difference. [Accessed April 21, 2015];2015 Apr; http://www.pewinternet.org/2015/04/01/us-smartphone-use-in-2015/. 2015. [Google Scholar]
- 42.Wiseman JT, Fernandes-Taylor S, Barnes ML, et al. Conceptualizing smartphone use in outpatient wound assessment: patients' and caregivers' willingness to use technology. J Surg Res. 2015 May 14; doi: 10.1016/j.jss.2015.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Stanberry B. Legal ethical and risk issues in telemedicine. Comput Methods Programs Biomed. 2001;64:225–233. doi: 10.1016/s0169-2607(00)00142-5. [DOI] [PubMed] [Google Scholar]