Abstract
AIM
Obesity is a major cardiovascular (CV) risk factor. Bariatric surgery (BSx) is an approved therapeutic alternative for class II–III obesity but little evidence focuses on older adults. We assessed the effect of BSx on cardiometabolic variables and long-term CV risk in elders.
METHODS
We performed a population-based, observational study from 1990–2009, of 40 consecutive elderly (age≥60years) residents of Olmsted County, MN, with class II–III obesity treated with BSx at a University-based, academic health center. Data were obtained from the Rochester Epidemiology Project. Metabolic syndrome (MetS) was defined using AHA/NHLBI criteria (increased triglycerides, low high-density lipoprotein, increased blood pressure, increased glucose, and BMI as a modified measure of obesity instead of waist circumference). Change in CV risk factors, MetS prevalence, and impact on predicted CV risk using the Framingham risk score was ascertained at a year post-operatively and assessed statistically.
RESULTS
Mean age and BMI were 64.4±3.7 and 45.0±6.3kg/m2, resp., and 28/40 (70%) were female. One subject died during the 11month study period after BSx from respiratory complications related to BSx, and one subject at two years. %Excess weight loss decreased by 57.5% at a year. Prevalence one year after BSx decreased for diabetes (57.5 to 22.5%; p<0.03), hypertension 87.5% to 73.7% (p=0.003), dyslipidemia (80 to 42.5%; p<0.001), and sleep apnea (62.5 to 23.7; p<0.001). MetS prevalence decreased from 80 to 45% (p<0.002). Baseline risk was 14.1% which changed at follow-up at 8.2%.
CONCLUSIONS
In elders, BSx induces considerable weight loss, improves CV risk factors, decreases MetS prevalence, and is an effective treatment in this population.
Keywords: bariatric surgery, elderly, Framingham risk, metabolic risk
INTRODUCTION
The epidemic of obesity impacts ~35% of the population1 and impacts potentially severe cardiovascular risk factors, including hypertension, diabetes, dyslipidemia and sleep apnea2, 3. Long-term cardiovascular risk is affected4 which can lead to premature mortality5. An increase n the number of older adults due to the baby boomer population6, improved life expectancy7, and improved pharmacologic and cardiovascular care8 has led to a large proportion of obese elders impacted by this disease.
Effective treatments for management of obesity, including lifestyle modifications and pharmacotherapy, lead to limited degrees of weight loss9. In older adults, there are even fewer weight loss trials10, 11, and the short term impact on comorbidity has been established only inconsistantly. Bariatric surgery (BSx) in adults with weight-related co-morbidities is a well-recognized treatment modality that induces and maintains weight loss in adults with comorbidities and is endorsed and approved by the NIH12. However, conflicting data on the impact of BSx in older adults exists13–15, and very little long-term data on important geriatric outcomes, including quality of life and functional status have been published to date.
The aim of this study was to identify the changes in short-term cardiometabolic risk factors using a population-based study of older adults who had undergone BSx. This information is the first step needed to identify the natural course of outcomes post-surgery. We hypothesized that in older adults, Bsx was an effective modality in improving cardiovascular risk.
MATERIALS & METHODS
We identified all residents of Olmsted County, Minnesota who underwent Roux-en-Y gastric bypass (RYGB) between January 1st, 1990 and December 31st, 2009. All bariatric operations in Olmsted County were performed at one center at that time. Patients were identified using a centralized diagnostic index and the Rochester Epidemiology Project (REP), allowing us to perform a true population-based, retrospective cohort study. The REP is a record-linkage system, funded continuously since 1966 by the Federal government for its use in disease-related epidemiology. All county residents have their medical care indexed allowing complete case ascertainment. Olmsted County is relatively isolated in southeastern MN, with medical care provided by two medical centers. This population provides reasonable extrapolation to other parts of the United States16. The study was approved by local institutional review boards.
Using the Surgical index, we identified those with RYGB as the primary surgical indication, cross-referenced with the REP to identify Olmsted county residents, verifying primary place of residency using Olmsted County US Postal Service zip codes. All weight-loss procedures were performed at the main teaching hospital, a 1,157 bed tertiary care center. We identified 40 patients over the age of 60 years. All surgical patients received medical and dietetic care including extensive physical activity counseling as part of their program. All baseline variables were abstracted on the basis of information from the medical record from the time of surgery or earlier. The REP was utilized to ensure adequate and proper follow-up data. One-year follow-up was based on information in the medical record +/− 2 months from the 12 month surgical date. Height and weight were measured in standardized manners by trained nurses. BMI was calculated as weight (in kilograms) divided by height (in meters) squared. The method of Robinson et al was used to calculate ideal body weight17.
We ascertained common comorbidities associated with obesity in the medical record. Hypertension was defined as a blood pressure ≥140/90 or if subjects were on medications for this indication. Diabetes was defined as having a fasting blood glucose ≥126mg/dL or on medications for diabetes (hypoglycemic agents or insulin). Dyslipidemia consisted on patients on any medications including statins, fibrate, nicotinic acid, or if the LDL≥160mg/dL. Patients using devices for obstructive sleep apnea were considered to have obstructive sleep apnea. Lastly, patients with a documented diagnosis of depression on medications for this indication were considered to have depression. These definitions were applied both at baseline and at follow-up.
Metabolic Syndrome (MetS) was characterized using the AHA/NHLBI criteria18. As waist circumference is not documented routinely in the medical record, a BMI≥30kg/m2 was considered to fulfill criteria for this component. Patients taking fibrates or nicotinic acid or whose serum TG were ≥150mg/dL fulfilled criteria for hypertriglyceridemia. Serum HDL-C was considered low if it was <50mg/dL in females, or <40mg/dL in males, or taking nicotinic acid or fibrates for this disorder based on review of the medical chart. Patients fulfilled criteria for hypertension if their blood pressure ≥135/85mmHg or taking medications for this indication. A fasting blood glucose ≥100mg/dL without the diagnosis of DM or those taking oral hypoglycemic agents or insulin fulfilled this criterion for the MetS; MetS was classified if ≥3 criteria were fulfilled. As performed in a previous analysis, we determined the effect on the prevalence of MetS defined as ≥2 components without obesity as a diagnostic criterion. Cause of death was identified using medical record review.
Statistical Analysis
Continuous data are presented as mean ± SD and categorical data as number and percentage. A two-sided, paired–t-test, and Wilcoxon signed rank test for continuous variables and McNemar test for categorical variables tested baseline vs. follow-up data. Logarithmic transformation due to the skewness of TGs was assessed. Our primary outcome was the determination of the prevalence of common comorbidities, including prevalence of MetS after surgery. We calculated the Framingham Risk Score based on the formula by Wilson et al19. Each outcome was assessed at baseline and follow-up and comparisons were subsequently made. A p-value <0.05 is considered statistically significant. All analyses were performed using JMP for SAS (V10.0, Cary, NC).
RESULTS
Baseline characteristics are shown in Table 1. Mean age was 64.4 ± 3.7 years, with the majority being females (70%), and 52.5% had a laparoscopic RYGB procedure. Mean BMI was 45.0±6.3kg/m2, and mean % excess weight was 105.8%. Other baseline metabolic variables are represented in the table. Two patients died within the 1st year – the first from respiratory failure and the second from sepsis. Figure 1 highlights the baseline and one-year co-morbidity data. There were significant decreases (p<0.05 each) in the prevalence of hypertension, diabetes, obstructive sleep apnea and hyperlipidemia, but not depression. The number of individual components of the MetS are represented in Figure 2. All components of the MetS dropped significantly at follow-up. There were 15 (39.5%) patients who had resolution of their MetS, 21 (55.3) who had no change, and 2 (5.3%) who had worsened components. Overall, the prevalence of MetS decreased from 80.0% to 44.7%, representing a 44.1% decrease (p=0.002). Using 4 components (in lieu of 5) of MetS led to a change in prevalence from 79.5% to 50%, a 37.5% decrease (p=0.005). Lastly, the FRS decreased from 14.1% at baseline to 8.2% at follow-up (p<.001).
TABLE 1.
Baseline Characteristics of 40 Older Bariatric Surgery Patients in Olmsted County
| Baseline N=40 |
Follow-up N=38 |
p-value | |
|---|---|---|---|
| Age, years | 64.4 ± 3.7 | 65.5 ± 3.9 | --- |
| Female sex | 28 (70) | --- | --- |
| Employment Status | |||
| Employed | 10 (25) | --- | |
| Unemployed | 7 (17.5) | --- | --- |
| Retired | 23 (57.5) | --- | |
| Insurance Status | |||
| Private | 29 (72.5) | --- | --- |
| Medicare | 11 (27.5) | --- | |
| Type of Procedure | |||
| Open | 19 (47.5) | --- | --- |
| Laparoscopic | 21 (52.5) | --- | |
| Body Mass Index, kg/m2 | 45.0 ± 6.3 | 31.6 ± 5.5 | <0.001 |
| Change in BMI, % | −29.5% | ||
| Weight, kg | 124.8 ± 25.5 | 86.9 ± 19.3 | <0.001 |
| IBW | 60.5 ± 8.3 | 60.1 ± 8.3 | <0.001 |
| % Excess Weight | 105.8 ± 28.7 | 44.7 ± 25.4 | <0.001 |
| % Excess Weight Loss | 57.5% | ||
| Ever Smoker | 20 (50.0) | --- | |
| Systolic Blood Pressure, mmHg | 130.4 ± 15.4 | 125.3 ± 18.5 | 0.66 |
| Diastolic Blood Pressure, mmHg | 68.7 ± 10.8 | 68.4 ± 11.7 | 0.93 |
| Glucose, mg/dL | 128.1 ± 36.6 | 99.3 ± 16.8 | 0.03 |
| Total Cholesterol, mg/dL | 179.2 ± 40.1 | 157.1 ± 37.8 | 0.03 |
| Triglycerides, mg/dL | 163.4 ± 101.7 | 104.4 ± 42.4 | 0.003 |
| Low Density Lipoprotein, mg/dL | 95.2 ± 28.7 | 81.0 ± 27.5 | 0.17 |
| Comorbidities | |||
| Hypertension | 35 (87.5) | 28 (73.7) | 0.003 |
| Diabetes | 23(57.5) | 9 (22.5) | 0.03 |
| Hyperlipidemia | 32 (80.0) | 17 (42.5) | 0.04 |
| OSA | 25 (62.5) | 9 (23.7) | <0.001 |
| Depression | 16 (40.0) | 16 (42.1) | 0.99 |
| Metabolic Syndrome (%) | 32 (80.0) | 17 (44.7) | <0.001 |
Continuous variables are represented as mean ± standard deviation and categorical variables are represented as counts (%).
Abbrevations: BMI – body mass index; IBW – ideal body weight; OSA – obstructive sleep apnea
Figure 1. Cardiac Risk Factors.
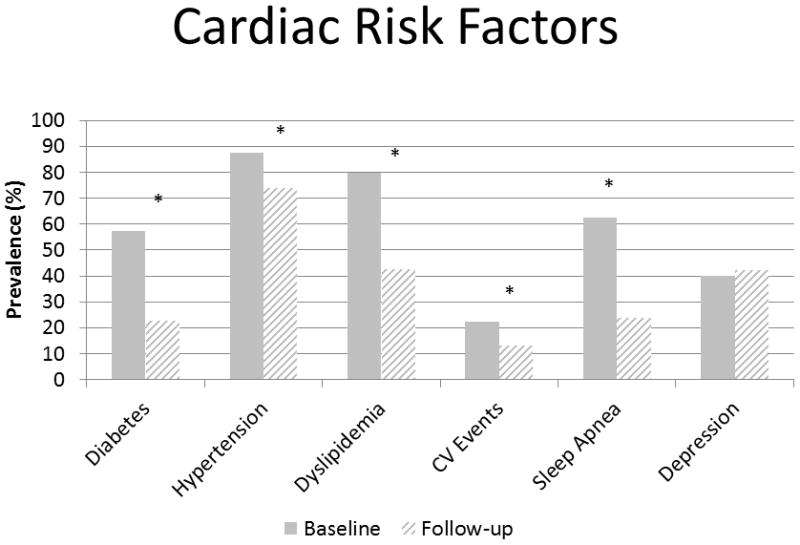
Prevalence of cardiometabolic risk factors at baseline and one-year post Roux-en-Y gastric bypass. CV - Cardiovascular
*- represents p<0.05
Figure 2. Metabolic Syndrome Criteria.
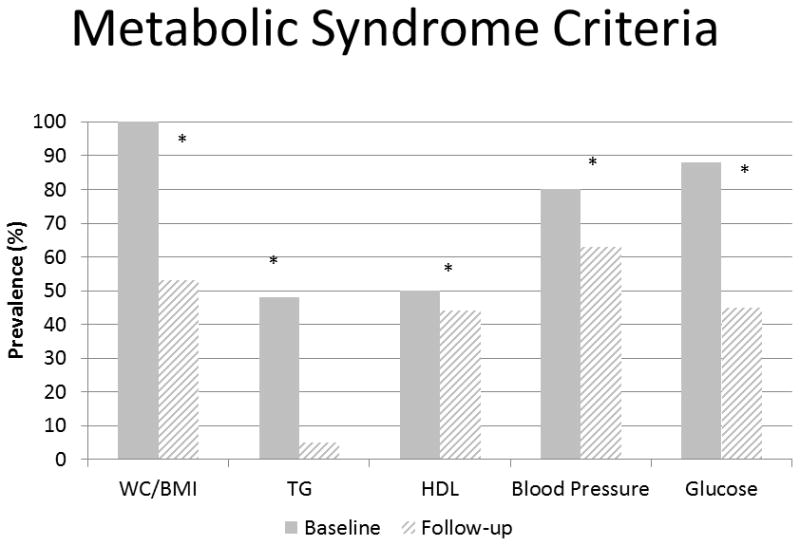
Proportion of individuals with each metabolic syndrome components at baseline (n=40) and one-year post Roux-en-Y gastric bypass (n=38). BMI – body mass index; HDL – high density lipoprotein; TG – triglycerides; WC – Waist circumference
*- represents p<0.05
DISCUSSION
Our results prove that BSx may be effective in decreasing cardiometabolic risk and reversing MetS, even in older adults. These results cannot understate the importance of bariatric surgery as a possible option in the elderly to decrease the prevalence of MetS which may lead to improved long-term quality of life, morbidity, and mortality18, 20.
Identification of MetS is important in adults undergoing Bsx, and relatively few studies have used this entity as an outcome after surgery21. To our knowledge, this is the first that demonstrates the marked reductions in prevalence and number of components in an elderly population. The decrease in MetS is associated with decreases in cardiac risk in this specific population. While models such as the Framingham risk score are limited to those younger than age 75, none of our patients exceeded this age and hence proves the associated improvement in risk. Additionally, the results of the FRS score may in fact underestimate overall cardiac risk, as this cardiac risk index does not include obesity or BMI as part of its equation22.
Other studies have demonstrated the decrease of cardiovascular risk after bariatric surgery in different populations4, 23. These risk assessments correlate well with studies of bariatric surgery that identify actual number of events24. While our study does not examine the longitudinal nature of change, it does provide emerging evidence that the trajectory of change may be similar to that observed in other, younger populations. While improvement of comorbidity is important in older adults undergoing BSx, the decision to undergo bariatric surgery needs to be weighed cautiously by patients, the surgeon, and the medical team. Older adults have different goals than younger middle-aged adults. Often, the goal is improvement in quality of life25, 26, decrease in disability27 and prevention of institutionalization28. Obesity impacts each of these three elements. Few studies have examined these outcomes specifically in an older adult population undergoing bariatric surgery. In the carefully selected elder patient, Bsx should be considered, although criteria are based on expert opinion rather than studies at this time. An urgent need to perform such studies is needed to determine whether there indeed is a cost-benefit relationship between surgery and important long-term geriatric outcomes.
For younger adults, the importance of co-morbidity resolution has been described consistently in both longitudinal and randomized controlled studies. For instance in the Swedish Obesity Study29, the changes observed with surgery with mortality are clear (HR 0.71), and marked long-term improvements in co-morbidity, including diabetes in randomized controlled trials have been observed30–32. Yet, one cannot extrapolate such data to older populations. Our study provides evidence of such. In fact, the upper limit for surgery has actually been recommended to be eliminated by the European Society for the Study for Obesity and that the overall primary surgical goal should also be to slow the functional decline trajectory. Identifying the appropriate surgical candidate aside from using strict age criteria is needed. Identification of physiologic, rather than chronologic age is needed33.
Of the 40 candidates, two died (5%) – one within the first year after Bsx and the other within 2 years. Both had similar improvements in co-morbidities but neither was clinically believed to be due to surgery-related causes. The authors fully recognize that this rate is unacceptably high and could dissuade medical and surgical teams from recommending surgery in an aging population. However, none of these patients died because of complications of the RYGB. Both patients had open RYGB, which is known to carry greater morbidity that laparoscopic, particularly in older adults34. Whether profound degrees of weight are a contributing factor is unclear as well. Previous studies have excluded such lower risk candidates13. Furthermore, there may have been other factors influencing their death, outside the standard 90-day surgical outcome window period. A previous series at Mayo Clinic suggested that 30-d hospital mortality was <1% and 5-year mortality was 5% in older adults suggesting the safety and efficacy of the procedure at a high-volume center at the extreme of age35. While there is no information to standardize the current approach to selecting patients, similar metabolic criteria to younger patients should be considered, and the focus of the assessment should revolve around psychosocial and functional status, with a life-expectancy >10 years should be mandatory. The goals of surgery should be to improve quality of life and improved function.
To our knowledge, our study is the first community-based study examining changes in one-year prevalence of MetS and changes in cardiovascular risk, specifically in an older adult population after bariatric surgery. We also deliberately incorporated the use of medications in our definitions of such risk factors. The geographically circumscribed area encompasses all patients undergoing bariatric surgery meeting inclusion criteria, and minimizing selection and referral bias. This is the first study consisting of only RYGB patients and the first identifying changes in cardiovascular risk specifically in older adults.
There are a number of study limitations including: its retrospective nature, the decision to undergo bariatric surgery was not random, and we had no control over ordering laboratory data or clinical follow-up. Additionally, this is an ethnically homogenous population, and extrapolation to other groups should be made with caution. Weight loss often occurs nonlinearly in the first year and often rebounds subsequently. We caution readers that further long-term data are needed to determine whether the metabolic effects of BSx are maintained in this population.
Lastly, our results do not account for nor do they describe the changes observed in body composition. Changes in lean mass can range between 10–25% and are often negatively correlated with weight loss. Such changes in fat-free mass may impact disability, function and frailty36, 37. Reduced muscle mass impairs the usual improvement in insulin sensitivity induced by bariatric surgery induced fat loss38. Additionally, bone loss occurs as early as three months post-surgery, and can be persistent up to 18 months, leading to bone fragility and impaired cross-linkage39. Increased fracture risk likely can ensues40. These issues are heightened in an older adult population and can possibly be mitigated with structured resistance exercise programs but require further investigation11, 41.
Short-term outcomes in older adults after bariatric surgery are very favorable and appear to decrease projected long-term cardiovascular risk. Future studies should examine long-term changes in functional status and quality of life in older adults undergoing bariatric surgery.
Acknowledgments
JAB – received American Geriatrics Society/Merck New Investigator Award; Northern New England Geriatric Education Center. Health Resources and Services Administration Grant #D31HP-08813; Dartmouth Centers for Health and Aging and the Department of Medicine Junior Faculty Career Development Award
This study was made possible by the Rochester Epidemiology Project (Grant #R01-AR30582 from the National Institute of Arthritis and Musculoskeletal and Skin Diseases
ABBREVIATIONS
- BSx
Bariatric surgery
- FRS
Framingham Risk Score
- MetS
Metabolic syndrome
- REP
Rochester Epidemiology Project
- RYGB
Roux-en-Y gastric bypass
Footnotes
Disclosures:
No Conflicts of Interests pertinent to this study were disclosed
Work presented at the 2012 The Obesity Society Conference, San Antonio, TX, September 2012
References
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311:806–14. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gami AS, Caples SM, Somers VK. Obesity and obstructive sleep apnea. Endocrinol Metab Clin North Am. 2003;32:869–94. doi: 10.1016/s0889-8529(03)00069-0. [DOI] [PubMed] [Google Scholar]
- 3.Gregg EW, Cheng YJ, Cadwell BL, et al. Secular trends in cardiovascular disease risk factors according to body mass index in US adults. JAMA. 2005;293:1868–74. doi: 10.1001/jama.293.15.1868. [DOI] [PubMed] [Google Scholar]
- 4.Batsis JA, Romero-Corral A, Collazo-Clavell ML, et al. Effect of weight loss on predicted cardiovascular risk: change in cardiac risk after bariatric surgery. Obesity (Silver Spring) 2007;15:772–84. doi: 10.1038/oby.2007.589. [DOI] [PubMed] [Google Scholar]
- 5.Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA. 2013;309:71–82. doi: 10.1001/jama.2012.113905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Government US. Census Bureau Statistics. 2012. [Google Scholar]
- 7.Lubitz J, Cai L, Kramarow E, Lentzner H. Health, life expectancy, and health care spending among the elderly. N Engl J Med. 2003;349:1048–55. doi: 10.1056/NEJMsa020614. [DOI] [PubMed] [Google Scholar]
- 8.Ford ES, Ajani UA, Croft JB, et al. Explaining the decrease in U.S. deaths from coronary disease, 1980–2000. N Engl J Med. 2007;356:2388–98. doi: 10.1056/NEJMsa053935. [DOI] [PubMed] [Google Scholar]
- 9.Look ARG. Eight-year weight losses with an intensive lifestyle intervention: the look AHEAD study. Obesity (Silver Spring) 2014;22:5–13. doi: 10.1002/oby.20662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Messier SP, Mihalko SL, Legault C, et al. Effects of intensive diet and exercise on knee joint loads, inflammation, and clinical outcomes among overweight and obese adults with knee osteoarthritis: the IDEA randomized clinical trial. JAMA. 2013;310:1263–73. doi: 10.1001/jama.2013.277669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Villareal DT, Chode S, Parimi N, et al. Weight loss, exercise, or both and physical function in obese older adults. N Engl J Med. 2011;364:1218–29. doi: 10.1056/NEJMoa1008234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gastrointestinal surgery for severe obesity. Am J Clin Nutr; Proceedings of a National Institutes of Health Consensus Development Conference; March 25–27, 1991; Bethesda, MD . 1992. pp. 487S–619S. [DOI] [PubMed] [Google Scholar]
- 13.Flum DR, Salem L, Elrod JA, Dellinger EP, Cheadle A, Chan L. Early mortality among Medicare beneficiaries undergoing bariatric surgical procedures. JAMA. 2005;294:1903–8. doi: 10.1001/jama.294.15.1903. [DOI] [PubMed] [Google Scholar]
- 14.Livingston EH, Langert J. The impact of age and Medicare status on bariatric surgical outcomes. Arch Surg. 2006;141:1115–20. doi: 10.1001/archsurg.141.11.1115. discussion 21. [DOI] [PubMed] [Google Scholar]
- 15.Nelson LG, Lopez PP, Haines K, et al. Outcomes of bariatric surgery in patients > or =65 years. Surg Obes Relat Dis. 2006;2:384–8. doi: 10.1016/j.soard.2006.02.012. [DOI] [PubMed] [Google Scholar]
- 16.Melton LJ., 3rd History of the Rochester Epidemiology Project. Mayo Clin Proc. 1996;71:266–74. doi: 10.4065/71.3.266. [DOI] [PubMed] [Google Scholar]
- 17.Robinson JD, Lupkiewicz SM, Palenik L, Lopez LM, Ariet M. Determination of ideal body weight for drug dosage calculations. Am J Hosp Pharm. 1983;40:1016–9. [PubMed] [Google Scholar]
- 18.Batsis JA, Nieto-Martinez RE, Lopez-Jimenez F. Metabolic syndrome: from global epidemiology to individualized medicine. Clin Pharmacol Ther. 2007;82:509–24. doi: 10.1038/sj.clpt.6100355. [DOI] [PubMed] [Google Scholar]
- 19.Wilson PW, D’Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97:1837–47. doi: 10.1161/01.cir.97.18.1837. [DOI] [PubMed] [Google Scholar]
- 20.Gami AS, Witt BJ, Howard DE, et al. Metabolic syndrome and risk of incident cardiovascular events and death: a systematic review and meta-analysis of longitudinal studies. J Am Coll Cardiol. 2007;49:403–14. doi: 10.1016/j.jacc.2006.09.032. [DOI] [PubMed] [Google Scholar]
- 21.Batsis JA, Romero-Corral A, Collazo-Clavell ML, Sarr MG, Somers VK, Lopez-Jimenez F. Effect of bariatric surgery on the metabolic syndrome: a population-based, long-term controlled study. Mayo Clin Proc. 2008;83:897–907. doi: 10.4065/83.8.897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Batsis JA, Lopez-Jimenez F. Cardiovascular risk assessment--from individual risk prediction to estimation of global risk and change in risk in the population. BMC Med. 2010;8:29. doi: 10.1186/1741-7015-8-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Batsis JA, Sarr MG, Collazo-Clavell ML, et al. Cardiovascular risk after bariatric surgery for obesity. Am J Cardiol. 2008;102:930–7. doi: 10.1016/j.amjcard.2008.05.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sjostrom L, Narbro K, Sjostrom CD, et al. Effects of bariatric surgery on mortality in Swedish obese subjects. The New England journal of medicine. 2007;357:741–52. doi: 10.1056/NEJMoa066254. [DOI] [PubMed] [Google Scholar]
- 25.Batsis J, Zbehlik A, Barre L, Bynum J, Bartels S. Impact of Waist Circumference on Quality of Life and Function: The Osteoarthritis Initiative. 2013. [Submitted] [Google Scholar]
- 26.Rosemann T, Grol R, Herman K, Wensing M, Szecsenyi J. Association between obesity, quality of life, physical activity and health service utilization in primary care patients with osteoarthritis. Int J Behav Nutr Phys Act. 2008;5:4. doi: 10.1186/1479-5868-5-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schaap LA, Koster A, Visser M. Adiposity, Muscle Mass, and Muscle Strength in Relation to Functional Decline in Older Persons. Epidemiol Rev. 2012 doi: 10.1093/epirev/mxs006. [DOI] [PubMed] [Google Scholar]
- 28.Zizza CA, Herring A, Stevens J, Popkin BM. Obesity affects nursing-care facility admission among whites but not blacks. Obes Res. 2002;10:816–23. doi: 10.1038/oby.2002.110. [DOI] [PubMed] [Google Scholar]
- 29.Sjostrom L, Narbro K, Sjostrom CD, et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med. 2007;357:741–52. doi: 10.1056/NEJMoa066254. [DOI] [PubMed] [Google Scholar]
- 30.Mingrone G, Panunzi S, De Gaetano A, et al. Bariatric surgery versus conventional medical therapy for type 2 diabetes. N Engl J Med. 2012;366:1577–85. doi: 10.1056/NEJMoa1200111. [DOI] [PubMed] [Google Scholar]
- 31.Schauer PR, Bhatt DL, Kirwan JP, et al. Bariatric surgery versus intensive medical therapy for diabetes--3-year outcomes. N Engl J Med. 2014;370:2002–13. doi: 10.1056/NEJMoa1401329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schauer PR, Kashyap SR, Wolski K, et al. Bariatric surgery versus intensive medical therapy in obese patients with diabetes. N Engl J Med. 2012;366:1567–76. doi: 10.1056/NEJMoa1200225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Batsis JA, Dolkart KM. Evaluation of older Adults with obesity for bariatric surgery: Geriatricians’ perspective. Journal of Clinical Gerontology and Geriatrics. 2015 [Google Scholar]
- 34.Webber KH, Tate DF, Quintiliani LM. Motivational interviewing in internet groups: a pilot study for weight loss. J Am Diet Assoc. 2008;108:1029–32. doi: 10.1016/j.jada.2008.03.005. [DOI] [PubMed] [Google Scholar]
- 35.Fatima J, Houghton SG, Iqbal CW, et al. Bariatric surgery at the extremes of age. J Gastrointest Surg. 2006;10:1392–6. doi: 10.1016/j.gassur.2006.08.014. [DOI] [PubMed] [Google Scholar]
- 36.Amatruda JM, Statt MC, Welle SL. Total and resting energy expenditure in obese women reduced to ideal body weight. J Clin Invest. 1993;92:1236–42. doi: 10.1172/JCI116695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Guida B, Belfiore A, Angrisani L, et al. Laparoscopic gastric banding and body composition in morbid obesity. Nutr Metab Cardiovasc Dis. 2005;15:198–203. doi: 10.1016/j.numecd.2004.10.001. [DOI] [PubMed] [Google Scholar]
- 38.Wadstrom C, Backman L, Forsberg AM, et al. Body composition and muscle constituents during weight loss: studies in obese patients following gastroplasty. Obes Surg. 2000;10:203–13. doi: 10.1381/096089200321643313. [DOI] [PubMed] [Google Scholar]
- 39.Fleischer J, Stein EM, Bessler M, et al. The decline in hip bone density after gastric bypass surgery is associated with extent of weight loss. J Clin Endocrinol Metab. 2008;93:3735–40. doi: 10.1210/jc.2008-0481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lalmohamed A, de Vries F, Bazelier MT, et al. Risk of fracture after bariatric surgery in the United Kingdom: population based, retrospective cohort study. BMJ. 2012;345:e5085. doi: 10.1136/bmj.e5085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pahor M, Guralnik JM, Ambrosius WT, et al. Effect of structured physical activity on prevention of major mobility disability in older adults: the LIFE study randomized clinical trial. JAMA. 2014;311:2387–96. doi: 10.1001/jama.2014.5616. [DOI] [PMC free article] [PubMed] [Google Scholar]


